On-Site Medical Management of Avalanche Victims—A Narrative Review
Abstract
1. Introduction and Epidemiology
2. Pathophysiology
3. On-Site Management
3.1. Guidelines for On-Site Management
3.2. Companion and Organized Rescue
3.3. Extrication, Initial Assessment and Monitoring
3.4. Trauma Management
3.5. Airway Management and Ventilation
3.6. Management of Moderate and Severe Hypothermia
3.7. Management of Patients in Cardiac Arrest
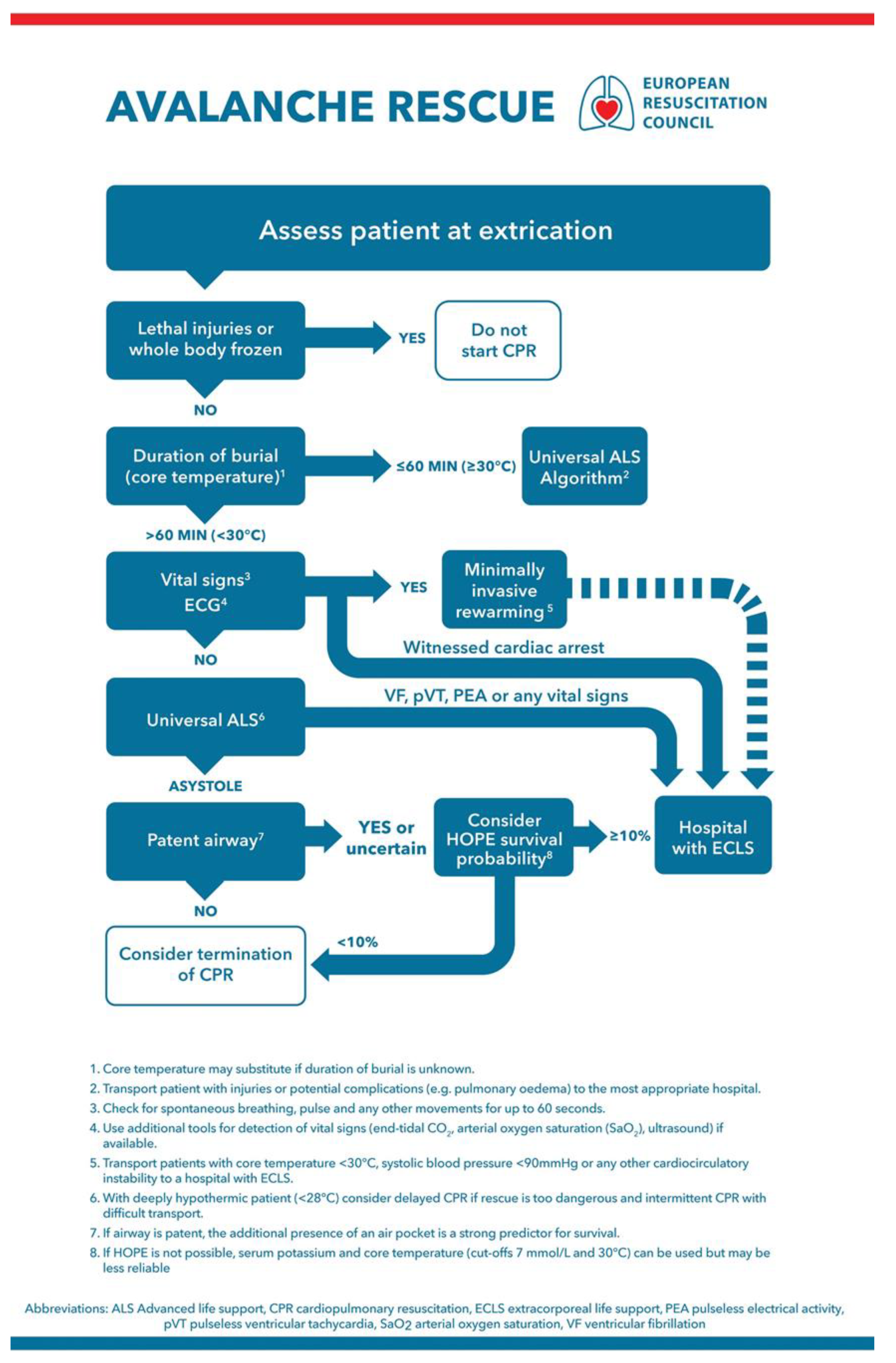
3.7.1. Management Algorithm
3.7.2. Intermittent CPR
3.7.3. Drugs and Defibrillation
3.7.4. Prognostication of Successful Rewarming
3.7.5. Training in Avalanche Rescue and the Avalanche Victim Resuscitation Checklist
3.7.6. Termination of CPR
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Techel, F.; Jarry, F.; Kronthaler, G.; Mitterer, S.; Nairz, P.; Pavšek, M.; Valt, M.; Darms, G. Avalanche fatalities in the European Alps: Long-term trends and statistics. Geogr. Helvetica 2016, 71, 147–159. [Google Scholar] [CrossRef]
- Brugger, H.; Durrer, B.; Elsensohn, F.; Paal, P.; Strapazzon, G.; Winterberger, E.; Zafren, K.; Boyd, J. Resuscitation of avalanche victims: Evi-dence-based guidelines of the international commission for mountain emergency medicine (ICAR MEDCOM): Intended for physi-cians and other advanced life support personnel. Resuscitation 2013, 84, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D. 10 years of avalanche rescues in the United States, 2003/04 to 2012/13. Avalanche Rev. 2015, 33, 22–24. [Google Scholar]
- Schweizer, J.; Lütschg, M. Characteristics of human-triggered avalanches. Cold Reg. Sci. Technol. 2001, 33, 147–162. [Google Scholar] [CrossRef]
- Rainer, B.; Frimmel, C.; Sumann, G.; Brugger, H.; Kinzl, J.F.; Lederer, W. Correlation between avalanche emergencies and avalanche danger forecast in the alpine region of Tyrol. Eur. J. Emerg. Med. 2008, 15, 43–47. [Google Scholar] [CrossRef]
- Strapazzon, G.; Schweizer, J.; Chiambretti, I.; Brodmann Maeder, M.; Brugger, H.; Zafren, K. Effects of Climate Change on Ava-lanche Accidents and Survival. Front Physiol. 2021, 12, 639433. [Google Scholar] [CrossRef]
- Strapazzon, G.; Paal, P.; Schweizer, J.; Falk, M.; Reuter, B.; Schenk, K.; Gatterer, H.; Grasegger, K.; Cappello, T.D.; Malacrida, S.; et al. Effects of snow properties on humans breathing into an artificial air pocket–An experimental field study. Sci. Rep. 2017, 7, 17675. [Google Scholar] [CrossRef] [PubMed]
- Brugger, H.; Durrer, B.; Adler-Kastner, L.; Falk, M.; Tschirky, F. Field management of avalanche victims. Resuscitation 2001, 51, 7–15. [Google Scholar] [CrossRef]
- Haegeli, P.; Falk, M.; Brugger, H.; Etter, H.-J.; Boyd, J. Comparison of avalanche survival patterns in Canada and Switzerland. Can. Med. Assoc. J. 2011, 183, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Van Tilburg, C.; Grissom, C.K.; Zafren, K.; McIntosh, S.; Radwin, M.I.; Paal, P.; Haegeli, P.; Smith, W.W.R.; Wheeler, A.R.; Weber, D.; et al. Wilderness Medical Society Practice Guidelines for Prevention and Management of Avalanche and Nonavalanche Snow Burial Accidents. Wilderness Environ. Med. 2017, 28, 23–42. [Google Scholar] [CrossRef]
- Falk, M.; Brugger, H.; Adler-Kastner, L. Avalanche survival chances. Nature 1994, 368, 21. [Google Scholar] [CrossRef]
- Procter, E.; Strapazzon, G.; Cappello, T.D.; Zweifel, B.; Würtele, A.; Renner, A.; Falk, M.; Brugger, H. Burial duration, depth and air pocket explain avalanche survival patterns in Austria and Switzerland. Resuscitation 2016, 105, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Strapazzon, G.; Brugger, H.; Paal, P.; Brown, D. Reconsidering the air pocket around mouth and nose as a positive outcome predictor in completely buried avalanche victims. Resuscitation 2020, 152, 208–209. [Google Scholar] [CrossRef]
- Strapazzon, G.; Putzer, G.; Cappello, T.D.; Falla, M.; Braun, P.; Falk, M.; Glodny, B.; Pinggera, D.; Helbok, R.; Brugger, H. Effects of hypothermia, hypoxia, and hypercapnia on brain oxygenation and hemodynamic parameters during simulated avalanche burial: A porcine study. J. Appl. Physiol. 2021, 130, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Brugger, H.; Etter, H.J.; Boyd, J.; Falk, M. Causes of death from avalanche. Wilderness Environ. Med. 2009, 20, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Paal, P.; Strapazzon, G.; Braun, P.; Ellmauer, P.P.; Schroeder, D.C.; Sumann, G.; Werner, A.; Wenzel, V.; Falk, M.; Brugger, H. Factors affecting survival from avalanche burial—A randomised prospective porcine pilot study. Resuscitation 2013, 84, 239–243. [Google Scholar] [CrossRef]
- Brugger, H.; Sumann, G.; Meister, R.; Adler-Kastner, L.; Mair, P.; Gunga, H.C.; Schobersberger, W.; Falk, M. Hypoxia and hypercapnia during respiration into an artificial air pocket in snow: Implications for avalanche survival. Resuscitation 2003, 58, 81–88. [Google Scholar] [CrossRef]
- Strapazzon, G.; Gatterer, H.; Falla, M.; Cappello, T.D.; Malacrida, S.; Turner, R.; Schenk, K.; Paal, P.; Falk, M.; Schweizer, J.; et al. Hypoxia and hypercapnia effects on cerebral oxygen saturation in avalanche burial: A pilot human experimental study. Resuscitation 2020, 158, 175–182. [Google Scholar] [CrossRef]
- Boyd, J.; Brugger, H.; Shuster, M. Prognostic factors in avalanche resuscitation: A systematic review. Resuscitation 2010, 81, 645–652. [Google Scholar] [CrossRef]
- Lott, C.; Truhlář, A.; Alfonzo, A.; Barelli, A.; González-Salvado, V.; Hinkelbein, J.; Nolan, J.P.; Paal, P.; Perkins, G.D.; Thies, K.-C.; et al. European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances. Resuscitation 2021, 161, 152–219. [Google Scholar] [CrossRef]
- Eidenbenz, D.; Techel, F.; Kottmann, A.; Rousson, V.; Carron, P.-N.; Albrecht, R.; Pasquier, M. Survival probability in avalanche victims with long burial (≥60 min): A retrospective study. Resuscitation 2021. [Google Scholar] [CrossRef] [PubMed]
- Paal, P.; Gordon, L.; Strapazzon, G.; Brodmann Maeder, M.; Putzer, G.; Walpoth, B.; Wanscher, M.; Brown, D.; Holzer, M.; Broessner, G.; et al. Accidental hypothermia-an update: The content of this review is endorsed by the International Commission for Mountain Emergency Medicine (ICAR MEDCOM). Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 111. [Google Scholar] [CrossRef] [PubMed]
- Locher, T.; Walpoth, B.H. Differential diagnosis of circulatory failure in hypothermic avalanche victims: Retrospective analysis of 32 avalanche accidents. Praxis 1996, 85, 1275–1282. [Google Scholar]
- Oberhammer, R.; Beikircher, W.; Hörmann, C.; Lorenz, I.; Pycha, R.; Adler-Kastner, L.; Brugger, H. Full recovery of an avalanche victim with profound hypothermia and prolonged cardiac arrest treated by extracorporeal re-warming. Resuscitation 2008, 76, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Mittermair, C.; Foidl, E.; Wallner, B.; Brugger, H.; Paal, P. Extreme Cooling Rates in Avalanche Victims: Case Report and Narrative Review. High Alt. Med. Biol. 2021, 22, 235–240. [Google Scholar] [CrossRef]
- Hohlrieder, M.; Brugger, H.; Schubert, H.M.; Pavlic, M.; Ellerton, J.; Mair, P. Pattern And Severity of Injury in Avalanche Victims. High Alt. Med. Biol. 2007, 8, 56–61. [Google Scholar] [CrossRef]
- Brugger, H.; Durrer, B.; Adler-Kastner, L. On-site triage of avalanche victims with asystole by the emergency doctor. Resuscitation 1996, 31, 11–16. [Google Scholar] [CrossRef]
- Brugger, H.; Durrer, B. On-Site Treatment of Avalanche Victims ICAR-MEDCOM-Recommendation. High Alt. Med. Biol. 2002, 3, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Soar, J.; Perkins, G.; Abbas, G.; Alfonzo, A.; Barelli, A.; Bierens, J.J.; Brugger, H.; Deakin, C.D.; Dunning, J.; Georgiou, M.; et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation 2010, 81, 1400–1433. [Google Scholar] [CrossRef] [PubMed]
- Vanden Hoek, T.L.; Morrison, L.J.; Shuster, M.; Donnino, M.; Sinz, E.; Lavonas, E.J.; Jeejeebhoy, F.M.; Gabrielli, A. Part 12: Cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010, 122, S829–S861. [Google Scholar] [CrossRef] [PubMed]
- Soar, J.; Bossaert, L.L.; Monsieurs, K.; Nikolaou, N.I.; Truhlář, A.; Zideman, D.A.; Maconochie, I.K.; Nolan, J.P.; Greif, R.; Perkins, G.D.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation 2015, 95, 1–80. [Google Scholar] [CrossRef]
- Mair, P.; Frimmel, C.; Vergeiner, G.; Hohlrieder, M.; Moroder, L.; Hoesl, P.; Voelckel, W. Emergency medical helicopter operations for ava-lanche accidents. Resuscitation 2013, 84, 492–495. [Google Scholar] [CrossRef]
- Wallner, B.; Moroder, L.; Brandt, A.; Mair, P.; Erhart, S.; Bachler, M.; Putzer, G.; Turner, R.; Strapazzon, G.; Falk, M.; et al. Extrication Times During Avalanche Companion Rescue: A Randomized Single-Blinded Manikin Study. High Alt. Med. Biol. 2019, 20, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Grasegger, K.; Strapazzon, G.; Procter, E.; Brugger, H.; Soteras, I. Avalanche Survival After Rescue With the RECCO Rescue System: A Case Report. Wilderness Environ. Med. 2016, 27, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Strapazzon, G.; Beikircher, W.; Procter, E.; Brugger, H. Msc Electrical Heart Activity Recorded During Prolonged Avalanche Burial. Circulation 2012, 125, 646–647. [Google Scholar] [CrossRef] [PubMed]
- Strapazzon, G.; Procter, E.; Paal, P.; Brugger, H. Pre-hospital core temperature measurement in accidental and therapeutic hy-pothermia. High Alt. Med. Biol. 2014, 15, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Pasquier, M.; Paal, P.; Kosinski, S.; Brown, D.; Podsiadlo, P.; DaRocha, T. Esophageal Temperature Measurement. N. Engl. J. Med. 2020, 383, e93. [Google Scholar] [CrossRef] [PubMed]
- Strapazzon, G.; Procter, E.; Putzer, G.; Avancini, G.; Cappello, T.D.; Überbacher, N.; Hofer, G.; Rainer, B.; Rammlmair, G.; Brugger, H. Influence of low ambient temperature on epitympanic temperature measurement: A prospective randomized clinical study. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 90. [Google Scholar] [CrossRef]
- Spahn, D.R.; Bouillon, B.; Cerny, V.; Duranteau, J.; Filipescu, D.; Hunt, B.J.; Komadina, R.; Maegele, M.; Nardi, G.; Riddez, L.; et al. The European guideline on management of major bleeding and coagulopathy following trauma: Fifth edition. Crit. Care 2019, 23, 98. [Google Scholar] [CrossRef]
- Sumann, G.; Moens, D.; Brink, B.; Brodmann Maeder, M.; Greene, M.; Jacob, M.; Koirala, P.; Zafren, K.; Ayala, M.; Musi, M.; et al. Multiple trauma management in mountain environments—A scoping review: Evidence based guidelines of the International Commission for Mountain Emergency Medicine (ICAR MedCom). Intended for physicians and other advanced life support personnel. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 1–22. [Google Scholar] [CrossRef]
- Papenhausen, M.; Burke, L.; Antony, A.; Phillips, J. Severe hypothermia with cardiac arrest: Complete neurologic recovery in a 4-year-old child. J. Pediatr. Surg. 2001, 36, 1590–1592. [Google Scholar] [CrossRef] [PubMed]
- Osborne, L.; El-Din, A.S.K.; Smith, J.E. Survival after prolonged cardiac arrest and accidental hypothermia. BMJ 1984, 289, 881–882. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gillen, J.P.; Vogel, M.F.; Holterman, R.K.; Skiendzielewski, J.J. Ventricular fibrillation during orotracheal intubation of hypothermic dogs. Ann. Emerg. Med. 1986, 15, 412–416. [Google Scholar] [CrossRef]
- Danzl, D.F.; Pozos, R.S.; Auerbach, P.S.; Glazer, S.; Goetz, W.; Johnson, E.; Jui, J.; Lilja, P.; Marx, J.A.; Miller, J.; et al. Multicenter hypothermia survey. Ann. Emerg. Med. 1987, 16, 1042–1055. [Google Scholar] [CrossRef]
- Soar, J.; Böttiger, B.W.; Carli, P.; Couper, K.; Deakin, C.D.; Djärv, T.; Lott, C.; Olasveengen, T.; Paal, P.; Pellis, T.; et al. European Resuscitation Council Guidelines 2021: Adult advanced life support. Resuscitation 2021, 161, 115–151. [Google Scholar] [CrossRef]
- Gruber, E.; Oberhammer, R.; Balkenhol, K.; Strapazzon, G.; Procter, E.; Brugger, H.; Falk, M.; Paal, P. Basic life support trained nurses ventilate more efficiently with laryngeal mask supreme than with facemask or laryngeal tube suction-disposable--a prospective, randomized clinical trial. Resuscitation 2014, 85, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Musi, M.E.; Sheets, A.; Zafren, K.; Brugger, H.; Paal, P.; Hölzl, N.; Pasquier, M. Clinical staging of accidental hypothermia: The Revised Swiss System: Recommendation of the International Commission for Mountain Emergency Medicine (ICAR MedCom). Resuscitation 2021, 162, 182–187. [Google Scholar] [CrossRef]
- Thomassen, Ø.; Færevik, H.; Østerås, Ø.; Sunde, G.; Zakariassen, E.; Sandsund, M.; Heltne, J.; Brattebø, G. Comparison of three different prehospital wrapping methods for preventing hypothermia—A crossover study in humans. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19, 41. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.J.; Brugger, H.; Boyd, J.; Paal, P. Accidental hypothermia. N. Engl. J. Med. 2012, 367, 1930–1938. [Google Scholar] [CrossRef] [PubMed]
- Mair, P.; Brugger, H.; Mair, B.; Moroder, L.; Ruttmann, E. Is extracorporeal rewarming indicated in avalanche victims with un-witnessed hypothermic cardiorespiratory arrest? High Alt. Med. Biol. 2014, 15, 500–503. [Google Scholar] [CrossRef] [PubMed]
- Rauch, S.; Strapazzon, G.; Brodmann, M.; Fop, E.; Masoner, C.; Rauch, L.; Forti, A.; Pietsch, U.; Mair, P.; Brugger, H. Implementation of a mechanical CPR device in a physician staffed HEMS-A prospective observational study. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 36. [Google Scholar] [CrossRef]
- Holmberg, M.J.; Issa, M.S.; Moskowitz, A.; Morley, P.; Welsford, M.; Neumar, R.W.; Paiva, E.F.; Coker, A.; Hansen, C.K.; Andersen, L.W.; et al. Vasopressors during adult cardiac arrest: A systematic review and meta-analysis. Resuscitation 2019, 139, 106–121. [Google Scholar] [CrossRef]
- Finn, J.; Jacobs, I.; Williams, T.A.; Gates, S.; Perkins, G.D. Adrenaline and vasopressin for cardiac arrest. Cochrane Database Syst. Rev. 2019, 2019, CD003179. [Google Scholar] [CrossRef]
- Corssen, G.; Allarde, R.; Brosch, F.; Arbenz, G. Ketamine as the Sole Anesthetic in Open-Heart Surgery. Anesth. Analg. 1970, 49, 1025–1031. [Google Scholar] [CrossRef]
- Lundgren, P.; Henriksson, O.; Naredi, P.; Björnstig, U. The effect of active warming in prehospital trauma care during road and air ambulance transportation-A clinical randomized trial. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19, 59. [Google Scholar] [CrossRef]
- Buzello, W.; Pollmaecher, T.; Schluermann, D.; Urbanyi, B. The influence of hypothermic cardiopulmonary bypass on neuro-muscular transmission in the absence of muscle relaxants. Anesthesiology 1986, 64, 279–281. [Google Scholar] [CrossRef]
- Withington, D.; Ménard, G.; Harris, J.; Kulkarni, P.; Donati, F.; Varin, F. Vecuronium pharmacokinetics and pharmacodynamics during hypothermic cardiopulmonary bypass in infants and children. Can. J. Anesth. 2000, 47, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Laycock, J.R.; Loughman, E. Suxamethonium-induced hyperkalaemia following cold injury. Anaesthesia 1986, 41, 739–741. [Google Scholar] [CrossRef] [PubMed]
- Pasquier, M.; Hugli, O.; Paal, P.; Darocha, T.; Blancher, M.; Husby, P.; Silfvast, T.; Carron, P.-N.; Rousson, V. Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: The HOPE score. Resuscitation 2018, 126, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Pasquier, M.; Rousson, V.; Darocha, T.; Bouzat, P.; Kosiński, S.; Sawamoto, K.; Champigneulle, B.; Wiberg, S.; Wanscher, M.C.J.; Maeder, M.B.; et al. Hypothermia outcome prediction after extra-corporeal life support for hypothermic cardiac arrest patients: An external validation of the HOPE score. Resuscitation 2019, 139, 321–328. [Google Scholar] [CrossRef]
- Brugger, H.; Bouzat, P.; Pasquier, M.; Mair, P.; Fieler, J.; Darocha, T.; Blancher, M.; de Riedmatten, M.; Falk, M.; Paal, P.; et al. Cut-off values of serum potassium and core temperature at hospital admission for extracorporeal rewarming of avalanche victims in cardiac arrest: A retrospective multi-centre study. Resuscitation 2019, 139, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Strapazzon, G.; Plankensteiner, J.; Mair, P.; Ruttmann, E.; Brugger, H. Triage and survival of avalanche victims with out-of-hospital cardiac arrest in Austria between 1987 and 2009. Resuscitation 2012, 83, e81. [Google Scholar] [CrossRef]
- Strapazzon, G.; Migliaccio, D.; Fontana, D.; Stawinoga, A.E.; Milani, M.; Brugger, H. Knowledge of the Avalanche Victim Resusci-tation Checklist and Utility of a Standardized Lecture in Italy. Wilderness Environ. Med. 2018, 29, 56–60. [Google Scholar] [CrossRef]
- Kottmann, A.; Blancher, M.; Spichiger, T.; Elsensohn, F.; Létang, D.; Boyd, J.; Strapazzon, G.; Ellerton, J.; Brugger, H. The Avalanche Victim Resuscitation Checklist, a new concept for the management of avalanche victims. Resuscitation 2015, 91, e7–e8. [Google Scholar] [CrossRef] [PubMed]
- DaRocha, T.; Kosinski, S.; Moskwa, M.; Jarosz, A.; Sobczyk, R.; Galazkowski, R.; Slowik, M.; Drwila, R. The Role of Hypothermia Coordinator: A Case of Hypothermic Cardiac Arrest Treated with ECMO. High Alt. Med. Biol. 2015, 16, 352–355. [Google Scholar] [CrossRef]
- Paal, P.; Milani, M.; Brown, D.; Boyd, J.; Ellerton, J. Termination of Cardiopulmonary Resuscitation in Mountain Rescue. High Alt. Med. Biol. 2012, 13, 200–208. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rauch, S.; Strapazzon, G.; Brugger, H. On-Site Medical Management of Avalanche Victims—A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 10234. https://doi.org/10.3390/ijerph181910234
Rauch S, Strapazzon G, Brugger H. On-Site Medical Management of Avalanche Victims—A Narrative Review. International Journal of Environmental Research and Public Health. 2021; 18(19):10234. https://doi.org/10.3390/ijerph181910234
Chicago/Turabian StyleRauch, Simon, Giacomo Strapazzon, and Hermann Brugger. 2021. "On-Site Medical Management of Avalanche Victims—A Narrative Review" International Journal of Environmental Research and Public Health 18, no. 19: 10234. https://doi.org/10.3390/ijerph181910234
APA StyleRauch, S., Strapazzon, G., & Brugger, H. (2021). On-Site Medical Management of Avalanche Victims—A Narrative Review. International Journal of Environmental Research and Public Health, 18(19), 10234. https://doi.org/10.3390/ijerph181910234







