Prediction of Cardiorespiratory Fitness in Czech Adults: Normative Values and Association with Cardiometabolic Health
Abstract
:1. Introduction
2. Materials and Methods
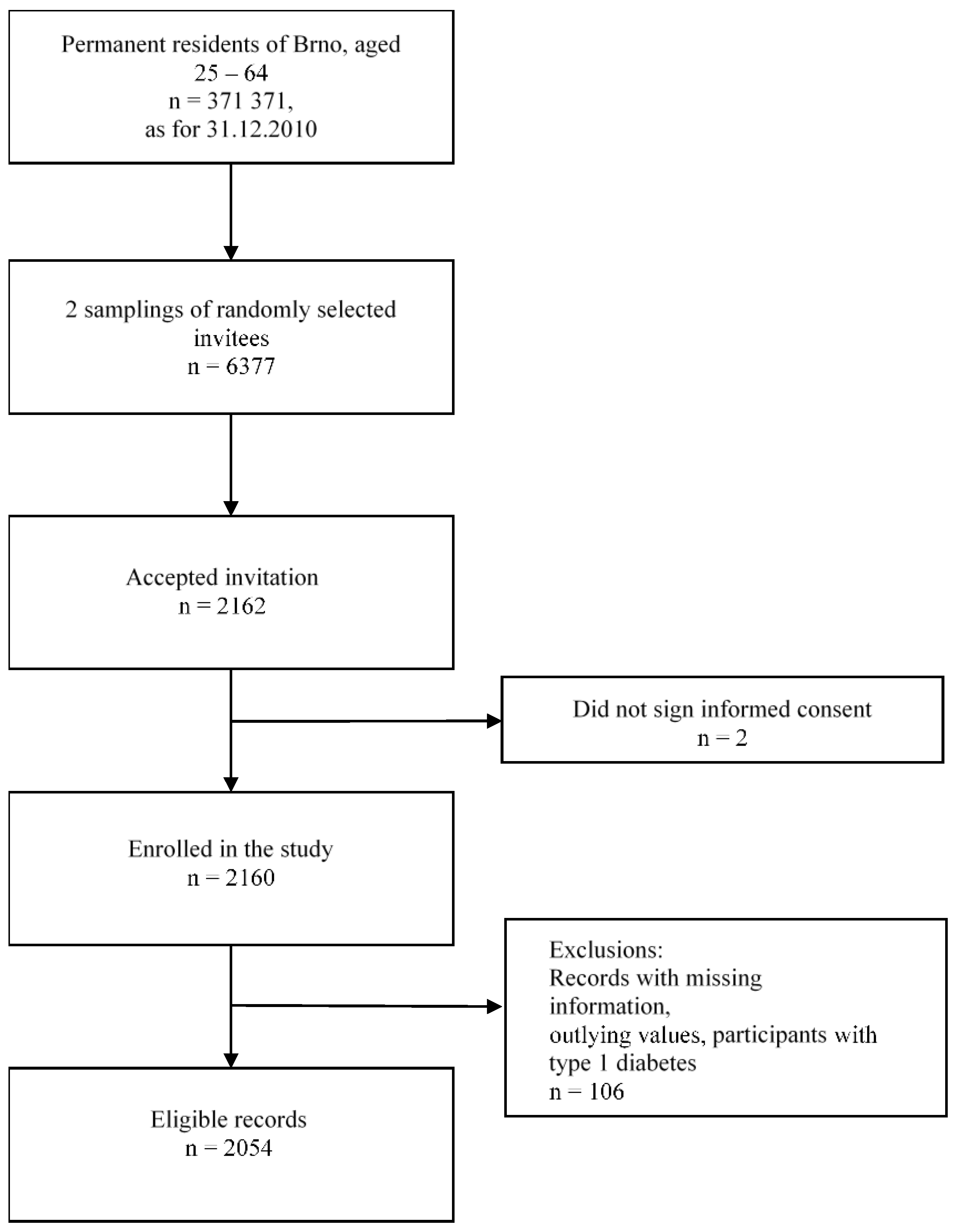
2.1. Study Design and Population
2.2. Sampling
2.3. Data Collection
2.4. Variables Definition
2.5. Cardiometabolic Outcomes
2.6. Cardiorespiratory Fitness Estimation
2.7. Data Analysis
3. Results
3.1. Subjects’ Characteristics
3.2. Association of Cardiorespiratory Fitness and Cardiometabolic Risk Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statements
Acknowledgments
Conflicts of Interest
References
- Movsisyan, N.K.; Vinciguerra, M.; Medina-Inojosa, J.R.; Lopez-Jimenez, F. Cardiovascular Diseases in Central and Eastern Europe: A Call for More Surveillance and Evidence-Based Health Promotion. Ann. Glob. Health 2020, 86, 21. [Google Scholar] [CrossRef] [PubMed]
- Cobb, F.R.; Kraus, W.E.; Root, M.; Allen, J.D. Assessing risk for coronary heart disease: Beyond Framingham. Am. Heart J. 2003, 146, 572–580. [Google Scholar] [CrossRef]
- Kokkinos, P.; Myers, J. Physical Activity, Cardiorespiratory Fitness, and Health: A Historical Perspective. In Cardiorespiratory Fitness in Cardiometabolic Diseases; Kokkinos, P., Narayan, P., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 1–9. [Google Scholar]
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Despres, J.P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e653–e699. [Google Scholar] [CrossRef] [PubMed]
- Lamoureux, N.R.; Fitzgerald, J.S.; Norton, K.I.; Sabato, T.; Tremblay, M.S.; Tomkinson, G.R. Temporal Trends in the Cardiorespiratory Fitness of 2,525,827 Adults Between 1967 and 2016: A Systematic Review. Sports Med. 2019, 49, 41–55. [Google Scholar] [CrossRef] [PubMed]
- Blair, S.N.; Kohl, H.W.; Paffenbarger, R.S.; Clark, D.G.; Cooper, K.H.; Gibbons, L.W. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA 1995, 273, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Farrell, S.W.; DeFina, L.F.; Radford, N.B.; Leonard, D.; Barlow, C.E.; Pavlovic, A.; Willis, B.L.; Haskell, W.L.; Lee, I.M. Relevance of Fitness to Mortality Risk in Men Receiving Contemporary Medical Care. J. Am. Coll. Cardiol. 2020, 75, 1538–1547. [Google Scholar] [CrossRef] [PubMed]
- Pavlovska, I.; Polcrova, A.; Mechanick, J.I.; Brož, J.; Infante-Garcia, M.M.; Nieto-Martínez, R.; Maranhao Neto, G.A.; Kunzova, S.; Skladana, M.; Novotny, J.S.; et al. Dysglycemia and Abnormal Adiposity Drivers of Cardiometabolic-Based Chronic Disease in the Czech Population: Biological, Behavioral, and Cultural/Social Determinants of Health. Nutrients 2021, 13, 2338. [Google Scholar] [CrossRef] [PubMed]
- LaMonte, M.J. Physical Activity, Fitness, and Coronary Heart Disease. In Cardiorespiratory Fitness in Cardiometabolic Diseases; Kokkinos, P., Narayan, P., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 295–318. [Google Scholar]
- Balady, G.J.; Arena, R.; Sietsema, K.; Myers, J.; Coke, L.; Fletcher, G.F.; Forman, D.; Franklin, B.; Guazzi, M.; Gulati, M.; et al. Clinician’s Guide to cardiopulmonary exercise testing in adults: A scientific statement from the American Heart Association. Circulation 2010, 122, 191–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seliger, V.; Máček, M.; Horák, J.; Pirič, J.; Handzo, P.; Rouš, J.; Jirka, Z. Work capacity of the Czechoslovakian population. Eur. J. Appl. Physiol. Occup. Physiol. 1978, 39, 155–164. [Google Scholar] [CrossRef]
- Grigaliūnienė, A.; Ramonas, A.; Čelutkienė, J.; Šileikienė, V.; Rudys, A.; Juocevičiu, A.; Laucevičiu, A. Cardiorespiratory parameters of exercise capacity in a healthy Lithuanian population: The pilot study. Hell. J. Cardiol. 2013, 54, 107–118. [Google Scholar]
- Tammelin, T.; Nayha, S.; Rintamaki, H. Cardiorespiratory fitness of males and females of northern Finland birth cohort of 1966 at age 31. Int. J. Sports Med. 2004, 25, 547–552. [Google Scholar] [CrossRef]
- Koch, B.; Schäper, C.; Ittermann, T.; Spielhagen, T.; Dörr, M.; Völzke, H.; Opitz, C.F.; Ewert, R.; Gläser, S. Reference values for cardiopulmonary exercise testing in healthy volunteers: The SHIP study. Eur. Respir. J. 2009, 33, 389–397. [Google Scholar] [CrossRef] [Green Version]
- Edvardsen, E.; Hansen, B.H.; Holme, I.M.; Dyrstad, S.M.; Anderssen, S.A. Reference values for cardiorespiratory response and fitness on the treadmill in a 20- to 85-year-old population. Chest 2013, 144, 241–248. [Google Scholar] [CrossRef]
- Ekblom-Bak, E.; Ekblom, O.; Andersson, G.; Wallin, P.; Soderling, J.; Hemmingsson, E.; Ekblom, B. Decline in cardiorespiratory fitness in the Swedish working force between 1995 and 2017. Scand. J. Med. Sci. Sports 2019, 29, 232–239. [Google Scholar] [CrossRef]
- Ingle, L.; Rigby, A.; Brodie, D.; Sandercock, G. Normative reference values for estimated cardiorespiratory fitness in apparently healthy British men and women. PLoS ONE 2020, 15, e0240099. [Google Scholar] [CrossRef]
- Khan, H.; Jaffar, N.; Rauramaa, R.; Kurl, S.; Savonen, K.; Laukkanen, J.A. Cardiorespiratory fitness and nonfatalcardiovascular events: A population-based follow-up study. Am. Heart J. 2017, 184, 55–61. [Google Scholar] [CrossRef]
- Appelqvist-Schmidlechner, K.; Vaara, J.P.; Vasankari, T.; Hakkinen, A.; Mantysaari, M.; Kyrolainen, H. Muscular and cardiorespiratory fitness are associated with health-related quality of life among young adult men. BMC Public Health 2020, 20, 842. [Google Scholar] [CrossRef]
- Shigdel, R.; Dalen, H.; Sui, X.; Lavie, C.J.; Wisloff, U.; Ernstsen, L. Cardiorespiratory Fitness and the Risk of First Acute Myocardial Infarction: The HUNT Study. J. Am. Heart Assoc. 2019, 8, e010293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garnvik, L.E.; Malmo, V.; Janszky, I.; Ellekjaer, H.; Wisloff, U.; Loennechen, J.P.; Nes, B.M. Physical activity, cardiorespiratory fitness, and cardiovascular outcomes in individuals with atrial fibrillation: The HUNT study. Eur Heart J. 2020, 41, 1467–1475. [Google Scholar] [CrossRef] [PubMed]
- Clausen, J.S.R.; Marott, J.L.; Holtermann, A.; Gyntelberg, F.; Jensen, M.T. Midlife Cardiorespiratory Fitness and the Long-Term Risk of Mortality: 46 Years of Follow-Up. J. Am. Coll. Cardiol. 2018, 72, 987–995. [Google Scholar] [CrossRef] [PubMed]
- Aberg, N.D.; Adiels, M.; Lindgren, M.; Nyberg, J.; Georg Kuhn, H.; Robertson, J.; Schaufelberger, M.; Sattar, N.; Aberg, M.; Rosengren, A. Diverging trends for onset of acute myocardial infarction, heart failure, stroke and mortality in young males: Role of changes in obesity and fitness. J. Intern. Med. 2021. [Google Scholar] [CrossRef]
- Eriksson, J.S.; Ekblom, B.; Andersson, G.; Wallin, P.; Ekblom-Bak, E. Scaling VO2max to body size differences to evaluate associations to CVD incidence and all-cause mortality risk. BMJ Open Sport Exerc. Med. 2021, 7, e000854. [Google Scholar] [CrossRef]
- Holmlund, T.; Ekblom, B.; Borjesson, M.; Andersson, G.; Wallin, P.; Ekblom-Bak, E. Association between change in cardiorespiratory fitness and incident hypertension in Swedish adults. Eur. J. Prev. Cardiol. 2020, 2047487320942997. [Google Scholar] [CrossRef]
- Laukkanen, J.A.; Kunutsor, S.K.; Yates, T.; Willeit, P.; Kujala, U.M.; Khan, H.; Zaccardi, F. Prognostic Relevance of Cardiorespiratory Fitness as Assessed by Submaximal Exercise Testing for All-Cause Mortality: A UK Biobank Prospective Study. Mayo Clin. Proc. 2020, 95, 867–878. [Google Scholar] [CrossRef] [PubMed]
- Tarp, J.; Grontved, A.; Sanchez-Lastra, M.A.; Dalene, K.E.; Ding, D.; Ekelund, U. Fitness, Fatness, and Mortality in Men and Women From the UK Biobank: Prospective Cohort Study. J. Am. Heart Assoc. 2021, 10, e019605. [Google Scholar] [CrossRef] [PubMed]
- Maranhao Neto, G.; Pedreiro, R.; Oliveira, A.; Machado, S.; Vieira, L.; Marques Neto, S.; Leon, A.P. Prediction of cardiorespiratory fitness in the brazilian population aged 20 to 59 years: A non-exercise model approach with self-reported variables. Rev. Da Educ. Física/Uem 2019, 30, e3068. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, S.; Lavie, C.J.; Zhang, J.; Sui, X. An Overview of Non-exercise Estimated Cardiorespiratory Fitness: Estimation Equations, Cross-Validation and Application. J. Sci. Sport Exerc. 2019, 1, 38–53. [Google Scholar] [CrossRef] [Green Version]
- Maranhao Neto, G.A.; Alves, I.; Lattari, E.; Oliveira, A.J.; Machado, S.; Neto, S.M.; Sui, X. Association between type 2 diabetes and non-exercise estimated cardiorespiratory fitness among adults: Evidences from a middle-income country. Public Health 2020, 189, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Movsisyan, N.K.; Vinciguerra, M.; Lopez-Jimenez, F.; Kunzova, S.; Homolka, M.; Jaresova, J.; Cifkova, R.; Sochor, O. Kardiovize Brno 2030, a prospective cardiovascular health study in Central Europe: Methods, baseline findings and future directions. Eur. J. Prev. Cardiol. 2018, 25, 54–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. The Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Back, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Jackson, A.S.; Sui, X.; O’Connor, D.P.; Church, T.S.; Lee, D.C.; Artero, E.G.; Blair, S.N. Longitudinal cardiorespiratory fitness algorithms for clinical settings. Am. J. Prev. Med. 2012, 43, 512–519. [Google Scholar] [CrossRef] [Green Version]
- Bakker, E.A.; Sui, X.; Brellenthin, A.G.; Lee, D.C. Physical activity and fitness for the prevention of hypertension. Curr. Opin. Cardiol. 2018, 33, 394–401. [Google Scholar] [CrossRef]
- Phillips, S.A.; Das, E.; Wang, J.; Pritchard, K.; Gutterman, D.D. Resistance and aerobic exercise protects against acute endothelial impairment induced by a single exposure to hypertension during exertion. J. Appl. Physiol. (1985) 2011, 110, 1013–1020. [Google Scholar] [CrossRef] [Green Version]
- Carbone, S.; Del Buono, M.G.; Ozemek, C.; Lavie, C.J. Obesity, risk of diabetes and role of physical activity, exercise training and cardiorespiratory fitness. Prog. Cardiovasc. Dis. 2019, 62, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Nojima, H.; Yoneda, M.; Watanabe, H.; Yamane, K.; Kitahara, Y.; Sekikawa, K.; Yamamoto, H.; Yokoyama, A.; Hattori, N.; Kohno, N. Association between aerobic capacity and the improvement in glycemic control after the exercise training in type 2 diabetes. Diabetol. Metab. Syndr. 2017, 9, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soran, H.; Schofield, J.D.; Durrington, P.N. Antioxidant properties of HDL. Front. Pharm. 2015, 6, 222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruiz-Ramie, J.J.; Barber, J.L.; Sarzynski, M.A. Effects of exercise on HDL functionality. Curr. Opin. Lipidol. 2019, 30, 16–23. [Google Scholar] [CrossRef]
- Khan, A.A.; Mundra, P.A.; Straznicky, N.E.; Nestel, P.J.; Wong, G.; Tan, R.; Huynh, K.; Ng, T.W.; Mellett, N.A.; Weir, J.M.; et al. Weight Loss and Exercise Alter the High-Density Lipoprotein Lipidome and Improve High-Density Lipoprotein Functionality in Metabolic Syndrome. Arter. Thromb. Vasc. Biol. 2018, 38, 438–447. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Zhang, J.; Zhou, J.; Ernstsen, L.; Lavie, C.J.; Hooker, S.P.; Sui, X. Nonexercise Estimated Cardiorespiratory Fitness and Mortality Due to All Causes and Cardiovascular Disease: The NHANES III Study. Mayo Clin. Proc. Innov. Qual Outcomes 2017, 1, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Hamer, M.; O’Donovan, G.; Batty, G.D.; Kivimaki, M. A non-exercise testing method for estimating cardiorespiratory fitness: Associations with all-cause and cardiovascular mortality in a pooled analysis of eight population-based cohorts. Eur. Heart J. 2013, 34, 750–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohta, T.; Nagashima, J.; Sasai, H.; Ishii, N. Relationship of Cardiorespiratory Fitness and Body Mass Index with the Incidence of Dyslipidemia among Japanese Women: A Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 4647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, C.S.; Chang, S.T.; Nfor, O.N.; Lee, K.J.; Lee, S.S.; Liaw, Y.P. Effects of Regular Aerobic Exercise and Resistance Training on High-Density Lipoprotein Cholesterol Levels in Taiwanese Adults. Int. J. Environ. Res. Public Health 2019, 16, 2003. [Google Scholar] [CrossRef] [Green Version]
- Mann, S.; Beedie, C.; Jimenez, A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: Review, synthesis and recommendations. Sports Med. 2014, 44, 211–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cáceres, J.M.; Ulbrich, A.Z.; Panigas, T.F.; Benetti, M. Equações de predição da aptidão cardiorrespiratória de adultos sem teste de exercícios físicos. Rev. Bras. Cineantropometria E Desempenho Hum. 2012, 14, 287–295. [Google Scholar] [CrossRef] [Green Version]
- Brawner, C.A.; Ehrman, J.K.; Bole, S.; Kerrigan, D.J.; Parikh, S.S.; Lewis, B.K.; Gindi, R.M.; Keteyian, C.; Abdul-Nour, K.; Keteyian, S.J. Inverse Relationship of Maximal Exercise Capacity to Hospitalization Secondary to Coronavirus Disease 2019. Mayo Clin. Proc. 2021, 96, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Christensen, R.A.G.; Arneja, J.; St Cyr, K.; Sturrock, S.L.; Brooks, J.D. The association of estimated cardiorespiratory fitness with COVID-19 incidence and mortality: A cohort study. PLoS ONE 2021, 16, e0250508. [Google Scholar] [CrossRef] [PubMed]
- Zbinden-Foncea, H.; Francaux, M.; Deldicque, L.; Hawley, J.A. Does High Cardiorespiratory Fitness Confer Some Protection Against Proinflammatory Responses After Infection by SARS-CoV-2? Obes. (Silver Spring) 2020, 28, 1378–1381. [Google Scholar] [CrossRef] [PubMed]
- Mayo, X.; Liguori, G.; Iglesias-Soler, E.; Copeland, R.J.; Clavel San Emeterio, I.; Lowe, A.; Del Villar, F.; Jimenez, A. The active living gender’s gap challenge: 2013–2017 Eurobarometers physical inactivity data show constant higher prevalence in women with no progress towards global reduction goals. BMC Public Health 2019, 19, 1677. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mechanick, J.I.; Farkouh, M.E.; Newman, J.D.; Garvey, W.T. Cardiometabolic-Based Chronic Disease, Adiposity and Dysglycemia Drivers: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 525–538. [Google Scholar] [CrossRef]
- Pavlovska, I.; Mechanick, J.I.; Maranhao Neto, G.A.; Infante-Garcia, M.M.; Nieto-Martinez, R.; Kunzova, S.; Polcrova, A.; Vysoky, R.; Medina-Inojosa, J.R.; Lopez-Jimenez, F.; et al. Arterial Stiffness and Cardiometabolic-Based Chronic Disease: The Kardiovize Study. Endocr Pr. 2021, 27, 571–578. [Google Scholar] [CrossRef]
- Gonzalez-Rivas, J.P.; Mechanick, J.I.; Hernandez, J.P.; Infante-Garcia, M.M.; Pavlovska, I.; Medina-Inojosa, J.R.; Kunzova, S.; Nieto-Martinez, R.; Brož, J.; Busetto, L.; et al. Prevalence of adiposity-based chronic disease in middle-aged adults from Czech Republic: The Kardiovize study. Obes. Sci. Pract. 2021. [Google Scholar] [CrossRef]
- Peterman, J.E.; Harber, M.P.; Imboden, M.T.; Whaley, M.H.; Fleenor, B.S.; Myers, J.; Arena, R.; Finch, W.H.; Kaminsky, L.A. Accuracy of Nonexercise Prediction Equations for Assessing Longitudinal Changes to Cardiorespiratory Fitness in Apparently Healthy Adults: BALL ST Cohort. J. Am. Heart Assoc. 2020, 9, e015117. [Google Scholar] [CrossRef] [PubMed]
- Maranhão Neto, G.A.; de Leon, A.P.; Lira, V.A.; Farinatti, P.T. Assessment of Cardiorespiratory Fitness without Exercise in Elderly Men with Chronic Cardiovascular and Metabolic Diseases. J. Aging Res. 2012, 2012, 518045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Movsisyan, N.K.; Sochor, O.; Kralikova, E.; Cifkova, R.; Ross, H.; Lopez-Jimenez, F. Current and past smoking patterns in a Central European urban population: A cross-sectional study in a high-burden country. BMC Public Health 2016, 16, 571. [Google Scholar] [CrossRef] [Green Version]
| Variables | Men | Women | p |
|---|---|---|---|
| (n = 932) | (n = 1122) | ||
| Age categories (%) | |||
| 25–34 | 17.6 | 15.2 | |
| 35–44 | 26 | 24.2 | |
| 45–54 | 26.5 | 26.6 | |
| 55–64 | 29.9 | 36 | 0.179 |
| BMI (kg/m2) | 26.0 (5.0) | 24.0 (6.0) | <0.001 |
| Waist Circumference (cm) | 95.0 (16.0) | 82.0 (18.0) | <0.001 |
| Resting Heart Rate (bpm) | 68.6 (14.0) | 71.4 (12.2) | <0.001 |
| Hypertension (%) | 43.7 | 33.4 | <0.001 |
| Type 2 Diabetes (%) | 6.1 | 3.1 | <0.001 |
| Low HDL-c (%) | 12.5 | 14.7 | 0.158 |
| High LDL-c (%) | 69.4 | 57.1 | <0.001 |
| Hypertriglyceridemia (%) | 29.5 | 13.5 | <0.001 |
| Hypercholesterolemia (%) | 52.2 | 57.3 | 0.022 |
| Physically Active (%) | 87.7 | 88.8 | 0.279 |
| Current Smokers (%) | 25.2 | 22 | 0.231 |
| Alcohol Users (%) | 90 | 78.8 | <0.001 |
| Educational Level (%) | |||
| Low | 20.5 | 18.6 | |
| Middle | 33.3 | 42.6 | |
| High | 46.1 | 38.7 | <0.001 |
| Household income (Euro) (%) | |||
| Low (<1200) | 33.5 | 50 | |
| Middle (1200–1800) | 34 | 30.4 | |
| High (>1800) | 32.5 | 19.6 | <0.001 |
| Living in Couple (%) | 66.4 | 58.9 | <0.001 |
| Medications (%) | |||
| Diuretic | 7.6 | 6.1 | 0.21 |
| Vasodilator | 24.4 | 19.7 | 0.011 |
| Hypoglycemic agents | 3.5 | 4.5 | 0.294 |
| Hypolipidemic agents | 11.8 | 9 | 0.056 |
| Age Categories | Q1 (Lowest) | Q2 | Q3 | Q4 (Highest) |
|---|---|---|---|---|
| Men (n = 932) | ||||
| 25–34 | ≤12.0 | >12.0–13.3 | >13.3–14.0 | >14.0 |
| 35–44 | ≤11.9 | >11.9–13.0 | >13.0–13.9 | >13.9 |
| 45–54 | ≤11.0 | >11.0–12.3 | >12.3–13.0 | >13.0 |
| 55–64 | ≤9.9 | >9.9–10.9 | >10.9–11.9 | >11.9 |
| Women (n = 1122) | ||||
| 25–34 | ≤10.2 | >10.2–10.6 | >10.6–11.0 | >11.0 |
| 35–44 | ≤9.6 | >9.6–10.3 | >10.3–10.8 | >10.8 |
| 45–54 | ≤8.8 | >8.8–9.6 | >9.6–10.2 | >10.2 |
| 55–64 | ≤7.9 | >7.9–8.6 | >8.6–9.2 | >9.2 |
| CRF and Hypertension | |||||
|---|---|---|---|---|---|
| Quartiles of Fitness | Hypertension | Model 1 a | 95% CI | Model 2 b | 95% CI |
| (%) ** | OR | OR | |||
| Q1—lowest | 58.2 | 1 | 1 | ||
| Q2 | 40.2 | 0.48 ** | 0.38–0.61 | 0.69 * | 0.49–0.96 |
| Q3 | 28.7 | 0.29 ** | 0.22–0.37 | 0.48 ** | 0.32–0.72 |
| Q4—highest | 21.1 | 0.19 ** | 0.14–0.25 | 0.36 ** | 0.22–0.60 |
| METs per Unit | 0.73 ** | 0.69–0.77 | 0.59 ** | 0.50–0.70 | |
| CRF and Type 2 Diabetes | |||||
| Quartiles of Fitness | Type 2 Diabetes | Model 1 a | 95% CI | Model 2 c | 95% CI |
| (%) ** | OR | OR | |||
| Q1—lowest | 10.3 | 1 | 1 | ||
| Q2 | 4 | 0.36 ** | 0.22–0.60 | 0.48 * | 0.26–0.88 |
| Q3 | 1.6 | 0.15 ** | 0.07–0.31 | 0.22 ** | 0.09–0.54 |
| Q4—highest | 1.1 | 0.10 ** | 0.04–0.24 | 0.16 ** | 0.05–0.47 |
| METs per Unit | 0.79 ** | 0.71–0.88 | 0.50 ** | 0.36–0.70 | |
| CRF and Low HDL-c | |||||
| Quartiles of Fitness | Low HDL-c (%) ** | Model 1 a | 95% CI | Model 2 d | 95% CI |
| OR | OR | ||||
| Q1—lowest | 26.1 | 1 | 1 | ||
| Q2 | 14.9 | 0.49 ** | 0.36–0.67 | 0.86 | 0.59–1.24 |
| Q3 | 7.4 | 0.23 ** | 0.15–0.33 | 0.47 ** | 0.29–0.77 |
| Q4—highest | 4.1 | 0.12 ** | 0.07–0.20 | 0.32 ** | 0.17–0.60 |
| METs per Unit | 0.71 ** | 0.66–0.76 | 0.82 | 0.67–1.00 | |
| CRF and High LDL-c | |||||
| Quartiles of Fitness | High LDL-c (%) ** | Model 1 a | 95% CI | Model 2 d | 95% CI |
| OR | OR | ||||
| Q1—lowest | 66.8 | 1 | 1 | ||
| Q2 | 65.4 | 0.94 | 0.73–1.20 | 0.78 | 0.55–1.10 |
| Q3 | 61.2 | 0.78 | 0.61–1.00 | 0.53 ** | 0.36–0.79 |
| Q4—highest | 56.1 | 0.63 ** | 0.49–0.82 | 0.33 ** | 0.21–0.53 |
| METs per Unit | 0.90 ** | 0.86–0.94 | 0.82 * | 0.69–0.97 | |
| CRF and Hypertriglyceridemia | |||||
| Quartiles of Fitness | Hypertriglyceridemia (%) ** | Model 1 a | 95% CI | Model 2 d | 95% CI |
| OR | OR | ||||
| Q1—lowest | 35.7 | 1 | 1 | ||
| Q2 | 23.9 | 0.57 ** | 0.44–0.74 | 0.62 ** | 0.45–0.86 |
| Q3 | 14.2 | 0.30 ** | 0.22–0.40 | 0.33 ** | 0.22–0.50 |
| Q4—highest | 5.9 | 0.11 ** | 0.07–0.17 | 0.13 ** | 0.07–0.23 |
| METs per Unit | 0.91 ** | 0.87–0.96 | 0.68 ** | 0.57–0.81 | |
| CRF and Hypercholesterolemia | |||||
| Quartiles of Fitness | Hypercholesterolemia (%) * | Model 1 a | 95% CI | Model 2 d | 95% CI |
| OR | OR | ||||
| Q1—lowest | 56.8 | 1 | 1 | ||
| Q2 | 58.5 | 1.07 | 0.85–1.36 | 0.89 | 0.65–1.21 |
| Q3 | 54.2 | 0.9 | 0.71–1.15 | 0.65 * | 0.45–0.62 |
| Q4—highest | 49.6 | 0.75 * | 0.58–0.96 | 0.44 ** | 0.29–0.69 |
| METs per Unit | 0.89 ** | 0.85–0.93 | 0.92 | 0.79–1.06 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maranhao Neto, G.A.; Pavlovska, I.; Polcrova, A.; Mechanick, J.I.; Infante-Garcia, M.M.; Hernandez, J.P.; Araujo, M.A.; Nieto-Martinez, R.; Gonzalez-Rivas, J.P. Prediction of Cardiorespiratory Fitness in Czech Adults: Normative Values and Association with Cardiometabolic Health. Int. J. Environ. Res. Public Health 2021, 18, 10251. https://doi.org/10.3390/ijerph181910251
Maranhao Neto GA, Pavlovska I, Polcrova A, Mechanick JI, Infante-Garcia MM, Hernandez JP, Araujo MA, Nieto-Martinez R, Gonzalez-Rivas JP. Prediction of Cardiorespiratory Fitness in Czech Adults: Normative Values and Association with Cardiometabolic Health. International Journal of Environmental Research and Public Health. 2021; 18(19):10251. https://doi.org/10.3390/ijerph181910251
Chicago/Turabian StyleMaranhao Neto, Geraldo A., Iuliia Pavlovska, Anna Polcrova, Jeffrey I. Mechanick, Maria M. Infante-Garcia, Jose Pantaleón Hernandez, Miguel A. Araujo, Ramfis Nieto-Martinez, and Juan P. Gonzalez-Rivas. 2021. "Prediction of Cardiorespiratory Fitness in Czech Adults: Normative Values and Association with Cardiometabolic Health" International Journal of Environmental Research and Public Health 18, no. 19: 10251. https://doi.org/10.3390/ijerph181910251
APA StyleMaranhao Neto, G. A., Pavlovska, I., Polcrova, A., Mechanick, J. I., Infante-Garcia, M. M., Hernandez, J. P., Araujo, M. A., Nieto-Martinez, R., & Gonzalez-Rivas, J. P. (2021). Prediction of Cardiorespiratory Fitness in Czech Adults: Normative Values and Association with Cardiometabolic Health. International Journal of Environmental Research and Public Health, 18(19), 10251. https://doi.org/10.3390/ijerph181910251






