Implementing Food Environment Policies at Scale: What Helps? What Hinders? A Systematic Review of Barriers and Enablers
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Study Selection
2.3. Quality Appraisal, Data Extraction and Synthesis
3. Results
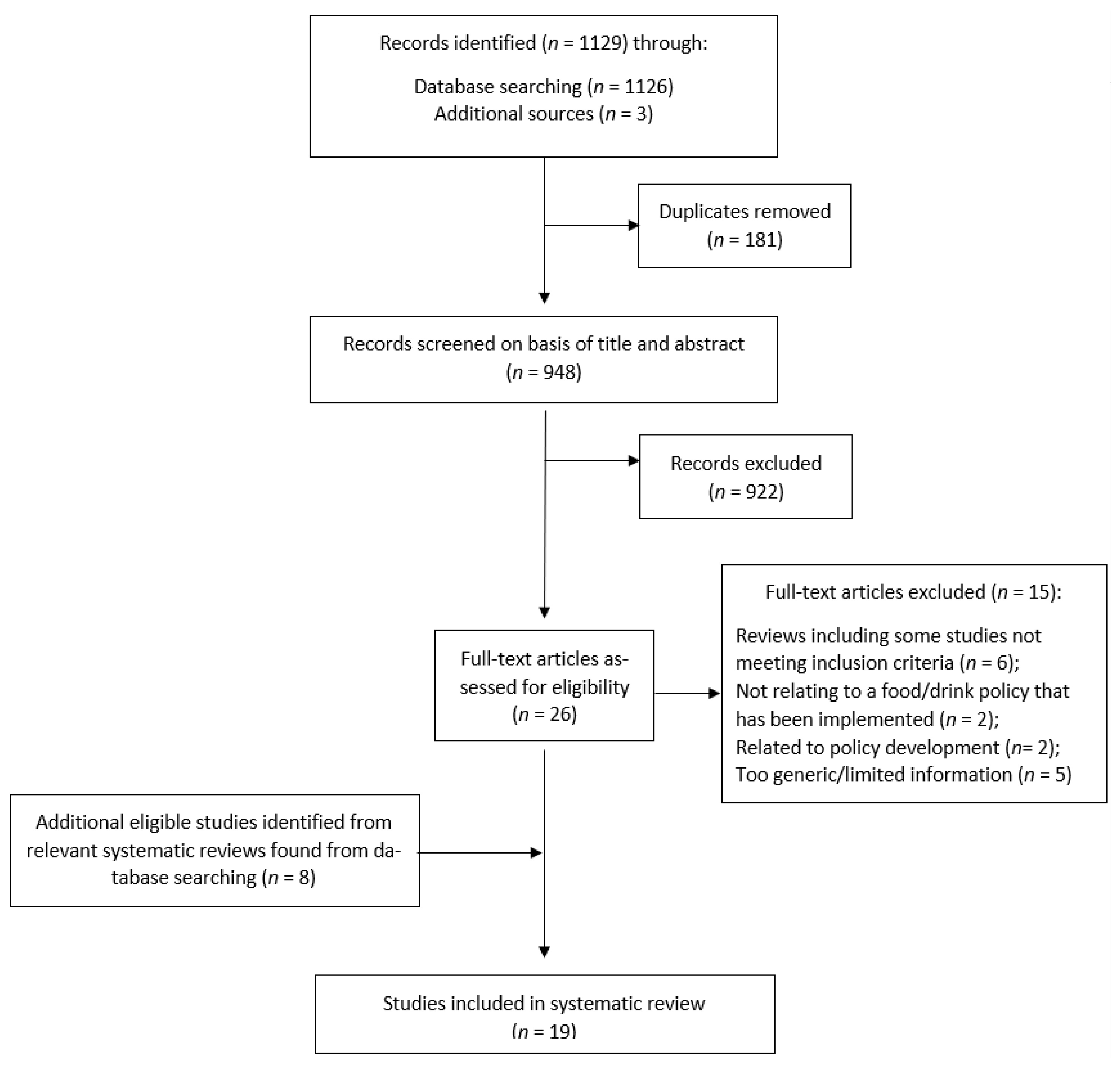
3.1. Study Selection
3.2. Study Characteristics
3.3. Policy Implementation Settings
3.4. Measures Used to Determine Policy Implementation Success
3.5. Barriers to Policy Implementation
| Overarching Themes and Sub-Themes for Identified Barriers | Number of Studies | References |
|---|---|---|
| Negative perceptions of the policy a | 10 | [24,28,35,43,44,47,48,50,51,52] |
| • Misinterpretation/difficulty in understanding policy content/lack of clarity | 3 | [24,43,44] |
| • Incompatible/inconsistent with stakeholders’ views on food offerings and consumer demands | 3 | [28,35,48] |
| • Nanny state/top-down approach | 2 | [24,50] |
| • Reduced parental autonomy | 2 | [47,51] |
| • Too restrictive | 1 | [52] |
| Implementation factors | 15 | [22,24,25,30,35,36,42,43,45,46,48,49,50,51,52] |
| Organisational | 12 | [22,30,35,36,42,43,45,46,48,49,50,51] |
| • Lack of stakeholder engagement, prioritisation of the policy | 11 | [22,35,36,42,43,45,46,48,49,50,51] |
| • Lack of time, money, staff, resources | 6 | [30,35,43,46,49,51] |
| • Lack of leadership, management commitment | 2 | [35,45] |
| • Ineffective implementation processes adopted | 1 | [43] |
| Contextual | 15 | [22,24,25,30,35,36,42,43,45,46,48,49,50,51,52] |
| • Lack of supply of policy-compliant/healthy products | 5 | [24,30,35,42,45] |
| • Rural facility location (vs. urban), school type (e.g., primary vs. secondary, public vs. private), non-supportive management structures, external management of food supply | 5 | [24,25,30,36,43] |
| • Lack of information, guidance and/or training support from the policy level | 5 | [35,36,43,49,52] |
| • Lack of enforcement | 3 | [35,43,49] |
| • Difficulty forming partnerships/conflicts of interest | 2 | [46,49] |
| • Marketing and promotion of EDNP foods within facility | 1 | [43] |
| Stakeholder responses b | 10 | [22,24,26,28,36,43,44,45,50,51] |
| • Consumer resistance (e.g., personal preferences, family habits) | 8 | [22,24,26,36,43,45,50,51] |
| • Complaints (e.g., educators overstepping boundaries/undermining parental authority, less convenient) | 5 | [26,28,44,45,51] |
| • Food/drink purchase displacement externally | 2 | [24,28] |
| Perceived policy impacts | 11 | [22,24,26,28,36,42,43,44,45,50,52] |
| • Loss of profits/revenue, commercial viability | 8 | [24,28,36,42,43,44,45,50] |
| • Higher food cost/food insecurity | 5 | [22,26,36,44,52] |
| • Food/drink external displacement due to access to external food outlets c | 2 | [43,52] |
| • Increased labour cost | 1 | [22] |
| • Difficulty finding fundraising alternatives | 1 | [44] |
3.5.1. Perceptions of the Implemented Policy
3.5.2. Organisational and Contextual Factors Influencing Policy Implementation
- Twelve studies (10 in school settings, two in hospital/health facility settings) mentioned organisational barriers to policy implementation [22,30,35,36,42,43,46,48,49,50,51], most frequently lack of engagement and/or prioritisation of the policy by stakeholders (e.g., school principals and staff, parents) [22,35,36,42,43,45,46,48,49,50,51], and lack of time, money, staff and/or resources [30,35,43,46,49,51].
- Fifteen studies (13 in school settings, two in hospital/health facility settings) reported contextual factors as barriers to policy implementation [22,24,25,30,35,36,42,43,45,46,48,49,50,51,52]. Commonly cited barriers were lack of supply of policy-compliant or healthy products [24,30,35,42,45], school location, type, and/or management structures [24,25,30,36,43], and lack of information, guidance and/or training support from the policy level [35,36,43,49,52].
3.5.3. Stakeholder Responses to the Implemented Policy
3.5.4. Perceived Policy Impacts
3.5.5. Barriers Reported in Studies Reporting Successful versus Unsuccessful Implementation
3.5.6. Barriers Reported in Studies Relating to a Mandatory versus Voluntary Policy Implementation
3.6. Mitigation of Barriers
- Increasing stakeholder engagement by involving community members in discussions and supporting existing partnerships with external organisations, for example schools working with local health organisations to host health-promoting activities as part of a “wellness week” (school setting) [46];
- Taking a long-term approach to help students and vending machine suppliers to adapt to changes with time (school setting) [42];
- Non-negotiable and permanent nature of a school policy helping to settle complaints from parents and children (school setting) [26]; and
- Training of school canteen staff to develop canteen menus that comply with the policy and that consider infrastructure and staffing constraints (school setting) [26].
3.7. Enabling Factors
| Overarching Themes and Sub-Themes for Identified Enablers | Number of Studies | References |
|---|---|---|
| Positive perceptions of the policy | 4 | [25,44,47,48] |
| • Easy to understand | 4 | [25,44,47,48] |
| • In line with stakeholders’ views/demands | 2 | [47,48] |
| • Nanny state/top-down approach | 1 | [44] |
| • In line with parental rights | 1 | [47] |
| Implementation factors | 13 | [24,25,26,28,30,42,43,44,45,46,47,51,52] |
| Organisational | 11 | [24,25,26,28,35,42,43,46,47,51,52] |
| • Stakeholder engagement, whole-school approach, prioritisation | 9 | [24,25,26,35,42,43,47,51,52] |
| • Leadership, school/policy champion, management commitment, organisational capacity | 5 | [28,35,42,46,52] |
| • Effective implementation processes adopted | 1 | [42] |
| Contextual | 9 | [24,26,30,42,43,44,45,46,47] |
| • Information, guidance and/or training support from the policy level/higher-level support | 6 | [26,30,44,45,46,47] |
| • Supply of policy-compliant/healthy products | 2 | [24,44] |
| • Healthy eating marketing | 1 | [42] |
| • Previous involvement with a voluntary food categorisation system | 1 | [47] |
| • Monitoring/enforcement of policy compliance | 1 | [43] |
| • External partnerships with the community (e.g., local farms, community centres) | 1 | [42] |
| • Part of a multisector effort | 1 | [30] |
| Stakeholder responses | 6 | [26,30,44,47,48,50] |
| • Acceptance of policy/change, positive attitude | 4 | [26,44,47,50] |
| • Ease of implementation, policy providing legitimacy to make changes | 2 | [26,48] |
| • Public recognition of accomplishments | 1 | [30] |
| Perceived impacts | 2 | [25,48] |
| • Belief in profits/revenue, commercial viability | 1 | [25] |
| • Increased availability of healthy foods | 1 | [48] |
3.7.1. Perceptions of the Implemented Policy
3.7.2. Organisational and Contextual Factors Enabling Policy Implementation
- Enabling contextual factors were also reported by nine studies (seven in school settings, two in hospital/health facility settings) [24,26,30,42,43,44,45,46,47]. The most frequently cited factors were access to information, guidance and/or training support such as implementation guides, support materials, technical assistance, or training of canteen managers, from the policy level or higher-level support [26,30,44,45,46,47], and availability of policy-compliant or healthy products from suppliers [24,44].
3.7.3. Stakeholder Responses to the Implemented Policy
3.7.4. Perceived Policy Impacts
3.7.5. Enablers Reported in Studies Reporting Successful versus Unsuccessful Implementation
3.7.6. Enablers Reported in Studies Relating to Mandatory versus Voluntary Implementation
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fact Sheet: Obesity and Overweight [Internet]. Geneva: World Health Organization; 1 April 2020. Available online: http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 29 August 2021).
- Di Cesare, M.; Sorić, M.; Bovet, P.; Jaime Miranda, J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organisation. Report of the Commission on Ending Childhood Obesity. In Implementation Plan: Executive Summary; Report No.: WHO/NMH/PND/ECHO/17.1; World Health Organisation: Geneva, Switzerland, 2017. [Google Scholar]
- Organisation for Economic Co-Operation and Development. The Heavy Burden of Obesity: The Economics of Prevention; [Internet]; OECD Health Policy Studies, OECD Publishing: Paris, France, 2019. [Google Scholar] [CrossRef]
- Gortmaker, S.L.; Swinburn, B.A.; Levy, D.; Carter, R.; Mabry, P.; Finegood, D.T.; Huang, T.; Marsh, T.; Moodie, M. Changing the future of obesity: Science, policy, and action. Lancet 2011, 378, 838–847. [Google Scholar] [CrossRef] [Green Version]
- Vandevijvere, S.; Dominick, C.; Devi, A.; Swinburn, B. The healthy food environment policy index: Findings of an expert panel in New Zealand. Bull. World Health Organ. 2015, 93, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Butland, B.; Jebb, S.; Kopelman, P.; McPherson, K.; Thomas, S.; Mardell, J.; Parry, V. Foresight, Tackling Obesities: Future Choices–Project Report, 2nd ed.; Government Office for Science: London, UK, 2007. [Google Scholar]
- Hawkes, C.; Jewell, J.; Allen, K. A food policy package for healthy diets and the prevention of obesity and diet-related non-communicable diseases: The NOURISHING framework. Obes. Rev. 2013, 14 (Suppl. 2), 159–168. [Google Scholar] [CrossRef]
- Swinburn, B.; Sacks, G.; Vandevijvere, S.; Kumanyika, S.; Lobstein, T.; Neal, B.; Barquera, S.; Friel, S.; Hawkes, C.; Kelly, B.; et al. INFORMAS (International Network for Food and Obesity/non-communicable diseases Research, Monitoring and Action Support): Overview and key principles. Obes. Rev. 2013, 14 (Suppl. 1), 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bos, C.; Lans, I.; Van Rijnsoever, F.; Van Trijp, H. Consumer Acceptance of Population-Level Intervention Strategies for Healthy Food Choices: The Role of Perceived Effectiveness and Perceived Fairness. Nutrients 2015, 7, 5370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellew, W.; Bauman, A.; Kite, J.; Foley, B.; Reece, L.; Thomas, M.; Mihrshahi, S.; King, L. Obesity prevention in children and young people: What policy actions are needed? Public Health Res. Pract. 2019, 29, e2911902. [Google Scholar] [CrossRef] [Green Version]
- Bleich, S.N.; Vercammen, K.A.; Zata, L.Y.; Frelier, J.M.; Ebbeling, C.B.; Peeters, A. Interventions to prevent global childhood overweight and obesity: A systematic review. Lancet Diabetes Endocrinol. 2018, 6, 332–346. [Google Scholar] [CrossRef]
- Story, M.; Kaphingst, K.M.; Robinson-O’Brien, R.; Glanz, K. Creating healthy food and eating environments: Policy and environmental approaches. Annu. Rev. Public Health 2008, 29, 253–272. [Google Scholar] [CrossRef] [Green Version]
- World Cancer Research Fund International. NOURISHING and MOVING Policy Databases [Web Portal]; World Cancer Research Fund International: London, UK, [Date Unknown]; Available online: http://policydatabase.wcrf.org/ (accessed on 29 August 2021).
- Physical Activity Nutrition Obesity Research Group. Validity Testing of Food and Drink Benchmark as a Standard for a Retail Food Environment; Prepared for the NSW Ministry of Health, Sydney; Physical Activity Nutrition Obesity Research Group, Prevention Research Collaboration, Sydney School of Public Health, The University of Sydney: Sydney, Australia, 2020. [Google Scholar]
- Rice, L.; Benson, C.; Podrabsky, M.; Otten, J.J. The development and adoption of the first statewide comprehensive policy on food service guidelines (Washington State Executive Order 13-06) for improving the health and productivity of state employees and institutionalized populations. Transl. Behav. Med. 2019, 9, 48–57. [Google Scholar] [CrossRef] [Green Version]
- Kumanyika, S.K.; Obarzanek, E.; Stettler, N.; Bell, R.; Field, A.E.; Fortmann, S.P.; Franklin, B.A.; Gillman, M.W.; Lewis, C.E.; Poston, W.C.; et al. Population-based prevention of obesity. The need for comprehensive promotion of healthful eating, physical activity, and energy balance. A scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (Formerly the Expert Panel on Population and Prevention Science). Circulation 2008, 118, 428–464. [Google Scholar]
- Vanderlee, L.; Goorang, S.; Karbasy, K.; Vandevijvere, S.; L’Abbé, M.R. Policies to create healthier food environments in Canada: Experts’ evaluation and prioritized actions using the Healthy Food Environment Policy Index (Food-EPI). Int. J. Environ. Res. Public Health 2019, 16, 4473. [Google Scholar] [CrossRef] [Green Version]
- McIsaac, J.D.; Spencer, R.; Chiasson, K.; Kontak, J.; Kirk, S.F.L. Factors influencing the implementation of nutrition policies in schools: A scoping review. Health Educ. Behav. 2019, 46, 224–250. [Google Scholar] [CrossRef]
- World Health Organization. Taking Action on Childhood Obesity; Report No.: WHO/NMH/PND/ECHO/18.1; World Health Organisation: Geneva, Switzerland, 2018. [Google Scholar]
- Jensen, C.D.; Sato, A.F.; McMurtry, C.; Hart, C.N.; Jelalian, E. School nutrition policy: An evaluation of the Rhode Island healthier beverages policy in schools. Infant. Child Adolesc. Nutr. 2012, 4, 276–282. [Google Scholar] [CrossRef]
- Woodward-Lopez, G.; Gosliner, W.; Samuels, S.E.; Craypo, L.; Kao, J.; Crawford, P.B. Lessons learned from evaluations of California’s statewide school nutrition standards. Am. J. Public Health 2010, 100, 2137–2145. [Google Scholar] [CrossRef] [PubMed]
- Vine, M.M.; Harrington, D.W.; Butler, A.; Patte, K.; Godin, K.; Leatherdale, S.T. Compliance with school nutrition policies in Ontario and Alberta: An assessment of secondary school vending machine data from the COMPASS study. Can. J. Public Health 2017, 108, e43–e48. [Google Scholar] [CrossRef] [PubMed]
- Matthews, A.; Nelson, M.; Kaur, A.; Rayner, M.; Kelly, P.; Cowburn, G. Where has all the chocolate gone? A national survey assesses the effects of recent legislation to improve the nutritional quality of English secondary-school vending. Public Health Nutr. 2011, 14, 1394–1402. [Google Scholar] [CrossRef] [Green Version]
- Dick, M.; Lee, A.; Bright, M.; Turner, K.; Edwards, R.; Dawson, J.; Miller, J. Evaluation of implementation of a healthy food and drink supply strategy throughout the whole school environment in Queensland state schools, Australia. Eur. J. Clin. Nutr. 2012, 66, 1124–1129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pettigrew, S.; Pescud, M.; Donovan, R.J. Stakeholder perceptions of a comprehensive school food policy in Western Australia. Health Policy 2012, 108, 100–104. [Google Scholar] [CrossRef]
- Boelsen-Robinson, T.; Blake, M.R.; Backholer, K.; Hettiarachchi, J.; Palermo, C.; Peeters, A. Implementing healthy food policies in health services: A qualitative study. Nutr. Diet. 2018, 30, 30. [Google Scholar] [CrossRef]
- Olstad, D.L.; Lieffers, J.R.; Raine, K.D.; McCargar, L.J. Implementing the Alberta nutrition guidelines for children and youth in a recreational facility. Can. J. Diet. Pract. Res. 2011, 72, 177. [Google Scholar] [CrossRef] [PubMed]
- Huse, O.; Blake, M.R.; Brooks, R.; Corben, K.; Peeters, A. The effect on drink sales of removal of unhealthy drinks from display in a self-service café. Public Health Nutr. 2016, 19, 3142–3145. [Google Scholar] [CrossRef] [Green Version]
- Moran, A.; Krepp, E.M.; Johnson Curtis, C.; Lederer, A. An intervention to increase availability of healthy foods and beverages in New York city hospitals: The Healthy Hospital Food Initiative, 2010–2014. Prev. Chronic Dis. 2016, 13, E77. [Google Scholar] [CrossRef]
- Cradock, A.L.; Kenney, E.L.; McHugh, A.; Conley, L.; Mozaffarian, R.S.; Reiner, J.F.; Gortmaker, S.L. Evaluating the impact of the healthy beverage executive order for city agencies in Boston, Massachussetts, 2011–2013. Prev. Chronic Dis. 2015, 10, E147. [Google Scholar]
- French, S.A.; Harnack, L.J.; Hannan, P.J.; Mitchell, N.R.; Gerlach, A.; Toomey, T.L. Worskite environment intervention to prevent obesity among metropolitan transit workers. Prev. Med. 2010, 50, 180–185. [Google Scholar] [CrossRef] [Green Version]
- Gardner, C.D.; Whitsel, L.P.; Thordike, A.N.; Marrow, M.W.; Otten, J.J.; Foster, G.D.; Carson, J.A.S.; Johnson, R.K. Food-and-beverage environment and procurement policies for healthier work environments. Nutr. Rev. 2014, 72, 390–410. [Google Scholar] [CrossRef]
- Ni Mhurchu, C. Effects of Healthier Food Choices in the School Setting on Children’s Health, Education and Nutrition. A Summary of Evidence; Prepared for the Heart Foundation of New Zealand; Clinical Trials Research Unit, School of Population Health, University of Auckland: Auckland, New Zealand, 2011. [Google Scholar]
- Budd, E.L.; Schwarz, C.; Yount, B.W.; Haire-Joshu, D. Factors influencing the implementation of school wellness policies in the United States, 2009. Prev. Chronic Dis. 2012, 9, 110296. [Google Scholar] [CrossRef] [Green Version]
- Downs, S.M.; Farmer, A.; Quintanilha, M.; Berry, T.R.; Mager, D.R.; Willows, N.D.; McCargar, L.J. From paper to practice: Barriers to adopting nutrition guidelines in schools. J. Nutr. Educ. Behav. 2012, 44, 114–122. [Google Scholar] [CrossRef]
- Lawlis, T.; Knox, M.; Jamieson, M. School canteens: A systematic review of the policy, perceptions and use from an Australian perspective. Nutr. Diet. 2016, 73, 389–398. [Google Scholar] [CrossRef]
- Welker, E.; Lott, M.; Story, M. The school food environment and obesity prevention: Progress over the last decade. Curr. Obes. Rep. 2016, 5, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, B.; Thomas, M. Implementing Policies to Increase the Availability and Promotion of Healthy Food and Drinks, Delivered at Scale: Barriers and Enablers. A Rapid Evidence Review; Prepared for the NSW Ministry of Health, Sydney; Physical Activity Nutrition Obesity Research Group, Prevention Research Collaboration, Sydney School of Public Health, The University of Sydney: Sydney, Australia, 2019. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [Green Version]
- Critical Appraisal Skills Programme. CASP (Qualitative) Checklist. 2018. Available online: http://casp-uk.net/casp-tools-checklists/ (accessed on 29 August 2021).
- Bassler, E.J.; Chriqui, J.F.; Stagg, F.; Schneider, L.M.; Infusino, K.; Akada, Y. Controlling Junk Food and the Bottom Line: Case Studies of Schools Successfully Implementing Strong Nutrition Standards for Competitive Foods and Beverages; Illinois Public Health Institute: Chicago, IL, USA, 2013. [Google Scholar]
- Girona, A.; Iragola, V.; Alcaire, F.; Curutchet, M.R.; Pereira, P.; Magnani, D.; Barreto, P.; Petingi, S.; Allegue, G.; Conzalo, G.; et al. Factors underlying compliance with a healthy snacking initiative in the school environment: Accounts of school principals in Montevideo (Uruguay). Public Health Nutr. 2018, 22, 726–737. [Google Scholar] [CrossRef]
- Masse, L.C.; Naiman, D.; Naylor, P.J. From policy to practice: Implementation of physical activity and food policies in schools. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 71. [Google Scholar] [CrossRef] [Green Version]
- Miller, J.; Lee, A.; Obersky, N.; Edwards, R. Implementation of A Better Choice Healthy Food and Drink Supply Strategy for staff and visitors in government-owned health facilities in Queensland, Australia. Public Health Nutr. 2015, 18, 1602–1609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orava, T.; Manske, S.; Hanning, R. Support for healthy eating at schools according to the comprehensive school health framework: Evaluation during the early years of the Ontario School Food and Beverage Policy implementation. Health Promot. Chronic Dis. Prev. Can. 2017, 37, 303–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pettigrew, S.; Donova, R.J.; Jalleh, G.; Pescud, M. Predictors of positive outcomes of a school food provision policy in Australia. Health Promot. Int. 2013, 29, 317–327. [Google Scholar] [CrossRef] [Green Version]
- Pettigrew, S.; Talati, Z.; Sauzier, M.; Ferguson, A. Stakeholder perceptions of a school food policy ten years on. Public Health Nutr. 2018, 21, 1370–1374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reeve, E.; Thow, A.M.; Bell, C.; Engelhardt, K.; Gamolo-Naliponguit, E.C.; Go, J.J.; Sacks, G. Implementation lessons for school food policies and marketing restrictions in the Philippines: A qualitative policy analysis. Global Health 2018, 14, 8. [Google Scholar] [CrossRef]
- Roberts, S.M.; Pobocik, R.S.; Deek, R.; Besgrove, A.; Prostine, B.A. A qualitative study of junior high school principals’ and school food service directors’ experiences with the Texas school nutrition policy. J. Nutr. Educ. Behav. 2009, 41, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Schuler, B.R.; Saksvig, B.I.; Nduka, J.; Beckerman, S.; Jaspers, L.; Black, M.M.; Hager, E.R. Barriers and enablers to the implementation of school wellness policies: An economic perspective. Health Promot. Pract. 2018, 19, 873–883. [Google Scholar] [CrossRef]
- Vine, M.M.; Elliott, S.J. Examining local-level factors shaping school nutrition policy implementation in Ontario, Canada. Public Health Nutr. 2014, 17, 1290–1298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raine, K.D.; Atkey, K.; Olstad, D.L.; Ferdinands, A.R.; Beaulieu, D.; Buhler, S.; Norm, C.; Brian, C.; Mary, L.; Ashley, L.; et al. Healthy food procurement and nutrition standards in public facilities: Evidence synthesis and consensus policy recommendations. Health Promot. Chronic Dis. Prev. Can. 2018, 38, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Blake, M.R.; Backholer, K.; Lancsar, E.; Boelsen-Robinson, T.; Mah, C.; Brimblecombe, J.; Zorbas, C.; Billich, N.; Peeters, A. Investigating business outcomes of healthy food retail strategies: A systematic scoping review. Obes. Rev. 2019, 20, 1384–1399. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Williams, F.; Masters, R.; Hyseni, L.; St Denny, E.; O’Flaherty, M.; Capewell, S. The QUEST for effective and equitable policies to prevent non-communicable diseases: Co-production lessons from stakeholder workshops. Int. J. Health Policy Manag. 2020. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, J.; Madden, K.; Fletcher, A.; Midgley, L.; Grant, A.; Cox, G.; Moore, L.; Campbell, R.; Murphy, S.; Bonell, C.; et al. Development of a framework for the co-production and prototyping of public health interventions. BMC Public Health 2017, 17, 689. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, M.; Sicilia, M.; Howlett, M. Understanding co-production as a new public governance tool. Policy Soc. 2018, 37, 277–293. [Google Scholar] [CrossRef] [Green Version]
- Middel, C.N.H.; Schuitmaker-Warnaar, T.J.; Mackenbach, J.D.; Broerse, J.E.W. Systematic review: A systems innovation perspective on barriers and facilitators for the implementation of healthy food-store interventions. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 108. [Google Scholar] [CrossRef] [Green Version]
| Items | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Study type | Studies of any design | None |
| Policy description | All types of healthy food and/or drink policies * implemented on a scale that can have an impact at a broad community level Include federal, state/regional policies | Not related to implementation of a healthy food and/or drink policy Unlikely to have a broad community level impact |
| Scale | At scale (≥10 sites **) | Scale too small (<10 sites) |
| Settings | Non-commercial *** food retail settings (government or non-government) Hospitals/Health services Schools Sport and recreation Workplaces Museums Zoos Stadia | Commercial food retail settings Food service (e.g., in-patient hospital food, government-subsidised school meals) Childcare settings |
| Type of food retail provision | Vending machines Workplace cafeterias Cafes Kiosks School canteens Fundraising outlets | Shopping centres Supermarkets Convenience stores Catering services One-off fundraising outlets (e.g., school bake sales) |
| Promotional activities | Pricing Placement of food/drinks Retail point of sale advertisements | Kilojoule labelling |
| Implementation barriers/enablers | Reports on barriers and/or enablers of policy implementation | Does not report on or provides extremely limited information on barriers and/or enablers of policy implementation |
| Population of interest | All | None |
| Language of publication | English | Not in English |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, B.; Cranney, L.; Bellew, B.; Thomas, M. Implementing Food Environment Policies at Scale: What Helps? What Hinders? A Systematic Review of Barriers and Enablers. Int. J. Environ. Res. Public Health 2021, 18, 10346. https://doi.org/10.3390/ijerph181910346
Nguyen B, Cranney L, Bellew B, Thomas M. Implementing Food Environment Policies at Scale: What Helps? What Hinders? A Systematic Review of Barriers and Enablers. International Journal of Environmental Research and Public Health. 2021; 18(19):10346. https://doi.org/10.3390/ijerph181910346
Chicago/Turabian StyleNguyen, Binh, Leonie Cranney, Bill Bellew, and Margaret Thomas. 2021. "Implementing Food Environment Policies at Scale: What Helps? What Hinders? A Systematic Review of Barriers and Enablers" International Journal of Environmental Research and Public Health 18, no. 19: 10346. https://doi.org/10.3390/ijerph181910346
APA StyleNguyen, B., Cranney, L., Bellew, B., & Thomas, M. (2021). Implementing Food Environment Policies at Scale: What Helps? What Hinders? A Systematic Review of Barriers and Enablers. International Journal of Environmental Research and Public Health, 18(19), 10346. https://doi.org/10.3390/ijerph181910346






