Mass Gathering Medicine in Soccer Leagues: A Review and Creation of the SALEM Tool
Abstract
:1. Introduction
2. Healthcare Risks of Football MG Events
3. Influential Factors of the Healthcare System’s Response
4. MG in Football and History of Disasters
5. Impact of the COVID-19 Pandemic on Football
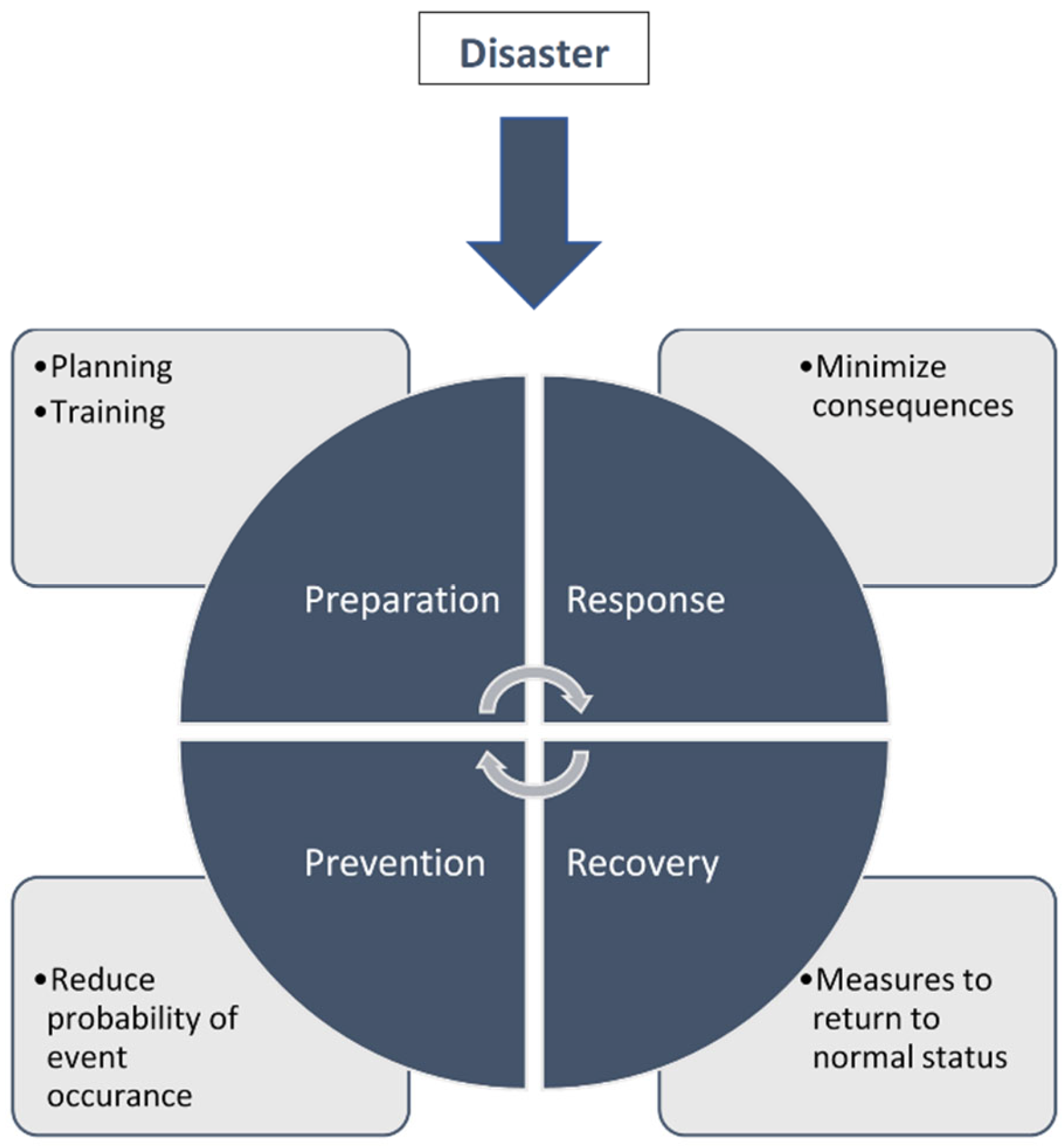
6. Preparation and Planning for Football MG Events
7. SALEM Tool: A Mass Gatherings Risk Assessment Framework
8. Key Insights and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- WHO. Public Health for Mass Gatherings: Key Considerations. World Health Organisation. Available online: https://apps.who.int/iris/bitstream/handle/10665/162109/WHO_HSE_GCR_2015.5_eng.pdf;jsessionid=20CDEF66BA427C7DB54004047BD811E4?sequence=1 (accessed on 21 June 2021).
- Aitsi-Selmi, A.; Murray, V.; Heymann, D.; McCloskey, B.; Azhar, E.I.; Petersen, E.; Zumla, A.; Dar, O. Reducing risks to health and wellbeing at mass gatherings: The role of the sendai framework for disaster risk reduction. Int. J. Infect. Dis. 2016, 47, 101–104. [Google Scholar] [CrossRef] [Green Version]
- McCloskey, B.; Endericks, T.; Catchpole, M.; Zambon, M.; McLauchlin, J.; Shetty, N.; Manuel, R.; Turbitt, D.; Smith, G.; Crook, P.; et al. London 2012 Olympic and Paralympic Games: Public health surveillance and epidemiology. Lancet 2014, 383, 2083–2089. [Google Scholar] [CrossRef]
- Memish, Z.A.; Zumla, A.; Alhakeem, R.F.; Assiri, A.; Turkestani, A.; Al Harby, K.D.; Alyemni, M.; Dhafar, K.; Gautret, P.; Barbeschi, M.; et al. Hajj: Infectious disease surveillance and control. Lancet 2014, 383, 2073–2082. [Google Scholar] [CrossRef]
- Smallwood, C.A.H.; Arbuthnott, K.G.; Banczak-Mysiak, B.; Borodina, M.; Coutinho, A.P.; Payne-Hallström, L.; Lipska, E.; Lyashko, V.; Miklasz, M.; Miskiewicz, P.; et al. Euro 2012 European football championship finals: Planning for a health legacy. Lancet 2014, 383, 2090–2097. [Google Scholar] [CrossRef]
- Abubakar, I.; Gautret, P.; Brunette, G.W.; Blumberg, L.; Johnson, D.; Poumerol, G.; Memish, Z.A.; Barbeschi, M.; Khan, A.S. Global perspectives for prevention of infectious diseases associated with mass gatherings. Lancet. Infect. Dis. 2012, 12, 66–74. [Google Scholar] [CrossRef]
- Schwartz, B.; Nafziger, S.; Milsten, A.; Luk, J.; Yancey, A. Mass gathering medical care: Resource document for the national association of EMS physicians position statement. Prehosp. Emerg. Care 2015, 19, 559–568. [Google Scholar]
- Tavan, A.; Tafti, A.D.; Nekoie-Moghadam, M.; Ehrampoush, M.; Vafaei Nasab, M.R.; Tavangar, H.; Fallahzadeh, H. Risks threatening the health of people participating in mass gatherings: A systematic review. J. Educ. Health Promot. 2019, 8, 209. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.S. Olympic medicine. N. Engl. J. Med. 2012, 367, 289–292. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, Q.A.; Memish, Z.A. From the “Madding Crowd” to mass gatherings-religion, sport, culture and public health. Travel Med. Infect. Dis. 2019, 28, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Boston Athletic Association. Boston Marathon History: Boston Marathon Facts. 2014. Available online: http://216.235.243.43/races/boston-marathon/boston-marathon-history/boston-marathon-facts.aspx (accessed on 21 June 2021).
- FIFA. FIFA Survey: Approximately 250 Million Footballers Worldwide; FIFA: Zürich, Switzerland, 2013. [Google Scholar]
- Hines, K. Mass gathering medicine. Trauma 2000, 2, 143–151. [Google Scholar]
- AlNsour, M.; Fleischauer, A. Public health considerations for mass gatherings in the Middle East and North Africa (MENA) region. East. Mediterr. Health J. 2013, 19 (Suppl. S2), S42–S47. [Google Scholar] [CrossRef]
- Cariappa, M.P.; Singh, B.P.; Mahen, A.; Bansal, A.S. Kumbh Mela 2013: Healthcare for the millions. Med. J. Armed Forces India 2015, 71, 278–281. [Google Scholar] [CrossRef] [Green Version]
- Blumberg, L.; Regmi, J.; Endricks, T.; McCloskey, B.; Petersen, E.; Zumla, A.; Barbeschi, M. Hosting of mass gathering sporting events during the 2013–2016 Ebola virus outbreak in West Africa: Experience from three African countries. Int. J. Infect. Dis. 2016, 47, 38–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sokhna, C.; Mboup, B.M.; Sow, P.G.; Camara, G.; Dieng, M.; Sylla, M.; Gueye, L.; Sow, D.; Diallo, A.; Parola, P.; et al. Communicable and non-communicable disease risks at the Grand Magal of Touba: The largest mass gathering in Senegal. Travel Med. Infect. Dis. 2017, 19, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Ishola, D.A.; Phin, N. Could influenza transmission be reduced by restricting mass gatherings? Towards an evidence-based policy framework. J. Epidemiol. Glob. Health 2011, 1, 33–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Communicable Disease Alert and Response for Mass Gatherings; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Yezli, S.; Assiri, A.; Nabulsi, H.; Awam, A.; Blumberg, L.; Endericks, T.; Stergachis, A.; Reicher, S.; McCloskey, B.; Petersen, E.; et al. From mass gatherings medicine to mass gatherings health: Conclusions from the 3rd International Conference on mass gatherings medicine, Riyadh, Kingdom of Saudi Arabia. Int. J. Infect. Dis. 2018, 66, 128–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Odone, A.; Delmonte, D.; Scognamiglio, T.; Signorelli, C. COVID-19 deaths in Lombardy, Italy: Data in context. Lancet Public Health 2020, 5, e310. [Google Scholar] [CrossRef]
- Signorelli, C.; Scognamiglio, T.; Odone, A. COVID-19 in Italy: Impact of containment measures and prevalence estimates of infection in the general population. Acta Biomed. 2020, 91, 175–179. [Google Scholar] [CrossRef]
- Signorelli, C.; Odone, A.; Riccò, M.; Bellini, L.; Croci, R.; Oradini-Alacreu, A.; Fiacchini, D.; Burioni, R. Major sports events and the transmission of sars-cov-2: Analysis of seven case-studies in europe. Acta Biomed. 2020, 91, 242–244. [Google Scholar] [CrossRef]
- Bieler, D. ‘A Biological Bomb’: Champions League Match in Italy Linked to Epicentre of Coronavirus Outbreak. The Independent. 2020. Available online: https://www.independent.co.uk/news/world/coronavirus-italy-champions-league-atlanta-valencia-milan-bergamo-a9426616.html (accessed on 28 June 2021).
- Soomaroo, L.; Murray, V. Disasters at mass gatherings: Lessons from history. PLoS Curr. 2012, 4, RRN1301. [Google Scholar] [CrossRef]
- Salamati, P.; Rahimi-Movaghar, V. Hajj stampede in Mina, 2015: Need for intervention. Arch. Trauma Res. 2016, 5, e36308. [Google Scholar] [CrossRef]
- Shujaa, A.; Alhamid, S. Health response to Hajj mass gathering from emergency perspective, narrative review. Turk. J. Emerg. Med. 2015, 15, 172–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alhadhira, A.; Molloy, M.S.; Casasola, M.; Sarin, R.R.; Massey, M.; Voskanyan, A.; Ciottone, G.R. Use of dimensional analysis in the X-, Y-, and Z-Axis to predict occurrence of injury in human stampede. Disaster Med. Public Health Prep. 2019, 14, 248–255. [Google Scholar] [CrossRef]
- Ranse, J.; Zeitz, K. Chain of survival at mass gatherings: A case series of resuscitation events. Prehosp. Disaster Med. 2010, 25, 457–463. [Google Scholar] [CrossRef]
- Turris, S.A.; Lund, A.; Hutton, A.; Bowles, R.; Ellerson, E.; Steenkamp, M.; Ranse, J.; Arbon, P. Mass-gathering health research foundational theory: Part 2—Event modeling for mass gatherings. Prehosp. Disaster Med. 2014, 29, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Health conditions for travellers to Saudi Arabia for the pilgrimage to Mecca (Hajj). Relev. Epidemiol. Hebd. 2013, 88, 343–347.
- Hutton, A.; Zeitz, K.; Brown, S.; Arbon, P. Assessing the psychosocial elements of crowds at mass gatherings. Prehosp. Disaster Med. 2011, 26, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, N.; Reicher, S. The psychology of health and well-being in mass gatherings: A review and a research agenda. J. Epidemiol. Glob. Health 2016, 6, 49–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hutton, A.; Ranse, J.; Gray, K.L.; Turris, S.; Lund, A.; Munn, M.B. Psychosocial influences on patient presentations: Considerations for research and evaluation at mass-gathering events. Prehosp. Disaster Med. 2020, 35, 197–205. [Google Scholar] [CrossRef]
- Bennett, S.A. Demonisation as explanation? A systems theory-informed analysis of the origins of, and reaction to the 1946 Burnden Park and 1989 Hillsborough football stadium disasters. Int. J. Disaster Risk Reduct. 2017, 21, 405–418. [Google Scholar] [CrossRef]
- Helbing, D.; Farkas, I.J.; Vicsek, T. 11. Crowd disasters and simulation of panic situations. In The Science of Disasters; Springer: Berlin/Heidelberg, Germany, 2002; Volume 2, p. 331. [Google Scholar]
- Akin, Y. 6 Not just a game: The Kayseri vs. Sivas football disaster. Soccer Soc. 2004, 5, 219–232. [Google Scholar] [CrossRef]
- Darby, P.; Johnes, M.; Mellor, G. Football disasters: A conceptual frame. Soccer Soc. 2004, 5, 125–133. [Google Scholar] [CrossRef]
- Walker, G. 3 ‘The ibrox stadium disaster of 1971’. Soccer Soc. 2004, 5, 169–182. [Google Scholar] [CrossRef]
- Darby, P. 8 A context of vulnerability: The zambian air disaster, 1993. Soccer Soc. 2004, 5, 248–264. [Google Scholar] [CrossRef]
- Molloy, M.S. Management of mass gatherings. In Koenig and Schultz’s Disaster Medicine: Comprehensive Principles and Practices; Schultz, C.H., Koenig, K.L., Eds.; Cambridge University Press: Cambridge, UK, 2016; pp. 265–293. ISBN 9781107040755. [Google Scholar]
- Zeller, M. Sport and Society in the Soviet Union: The Politics of Football after Stalin; Bloomsbury Publishing: New York, NY, USA, 2018. [Google Scholar]
- Broeze, C.L.; Falder, S.; Rea, S.; Wood, F. Burn disasters—An audit of the literature. Prehosp. Disaster Med. 2010, 25, 555–579. [Google Scholar] [CrossRef] [PubMed]
- Logan, C.; Gosseye, J. Architecture and the Spectre of the Crowd. Archit. Theory Rev. 2019, 23, 171–177. [Google Scholar] [CrossRef] [Green Version]
- Elshawarby, M.K. Football Stadiums’ Disasters, University of Peloponnese. 2015. Available online: https://amitos.library.uop.gr/xmlui/bitstream/handle/123456789/4803/Mohamed%20Shawarby%20Thesis%20-%20Final%20Version%2026-4-2016.pdf?sequence=1l (accessed on 28 June 2021).
- Kerr, G.W. Emergency medical planning at soccer matches. Int. Sport Med. J. 2003, 4, 1–5. [Google Scholar]
- Alegi, P. 7 ‘Like cows driven to a dip’: The 2001 ellis park stadium disaster in South Africa. Soccer Soc. 2004, 5, 233–247. [Google Scholar] [CrossRef]
- Pollard, R.; Gómez, M.A. Home advantage in football in South-West Europe: Long-term trends, regional variation, and team differences. Eur. J. Sport Sci. 2009, 9, 341–352. [Google Scholar] [CrossRef]
- Madzimbamuto, F.D. A hospital response to a soccer stadium stampede in Zimbabwe. Emerg. Med. J. 2003, 20, 556–559. [Google Scholar] [CrossRef] [Green Version]
- Künzler, D. Ivory coast BT. In The Palgrave International Handbook of Football and Politics; De Waele, J.-M., Gibril, S., Gloriozova, E., Spaaij, R., Eds.; Springer International Publishing: Cham, Germany, 2018; pp. 385–402. ISBN 978-3-319-78777-0. [Google Scholar]
- Hughson, J.; Moore, K.; Spaaij, R.; Maguire, J. (Eds.) Football hooliganism. In Routledge Handbook of Football Studies; Taylor & Francis: Oxfordshire, UK, 2016; pp. 364–374. [Google Scholar]
- Abaza, M. Violence, dramaturgical repertoires and neoliberal imaginaries in Cairo. Theory Cult. Soc. 2016, 33, 111–135. [Google Scholar] [CrossRef]
- Bledsoe, B.; Songer, P.; Buchanan, K.; Westin, J.; Hodnick, R.; Gorosh, L. Burning man 2011: Mass gathering medical care in an austere environment. Prehosp. Emerg. Care 2012, 16, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.-H.; Liu, F.; Liu, Y.-M.; Jiang, X.-R.; Zhao, Z.-X. Emergency preparedness for mass gatherings: Lessons of “12.31” stampede in Shanghai Bund. Chin. J. Traumatol. 2017, 20, 240–242. [Google Scholar] [CrossRef] [PubMed]
- Polkinghorne, B.G.; Massey, P.D.; Durrheim, D.N.; Byrnes, T.; MacIntyre, C.R. Prevention and surveillance of public health risks during extended mass gatherings in rural areas: The experience of the tamworth country music festival, Australia. Public Health 2013, 127, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Thackway, S.; Churches, T.; Fizzell, J.; Muscatello, D.; Armstrong, P. Should cities hosting mass gatherings invest in public health surveillance and planning? Reflections from a decade of mass gatherings in Sydney, Australia. BMC Public Health 2009, 9, 324. [Google Scholar] [CrossRef] [Green Version]
- WHO. General Information on Risk Communication; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Flynn, B.W.; Philbin, J.P. Risk and crisis communications. In Integrating Emergency Management and Disaster Behavioral Health: One Picture through Two Lenses; Butterworth-Heinemann: Oxford, UK, 2017; ISBN 9780128036396. [Google Scholar]
- Abrams, E.M.; Greenhawt, M. Risk communication during COVID-19. J. Allergy Clin. Immunol. Pract. 2020, 8, 1791–1794. [Google Scholar] [CrossRef]
- Ranse, J.; Hutton, A.; Keene, T.; Lenson, S.; Luther, M.; Bost, N.; Johnston, A.N.B.; Crilly, J.; Cannon, M.; Jones, N.; et al. Health service impact from mass gatherings: A systematic literature review. Prehosp. Disaster Med. 2017, 32, 71–77. [Google Scholar] [CrossRef]
- Steffen, R.; Bouchama, A.; Johansson, A.; Dvorak, J.; Isla, N.; Smallwood, C.; Memish, Z.A. Non-communicable health risks during mass gatherings. Lancet Infect. Dis. 2012, 12, 142–149. [Google Scholar] [CrossRef]
- Smith, W.P.; Wessels, V.; Naicker, D.; Leuenberger, E.; Fuhri, P.; Wallis, L.A. Development of a mass-gathering medical resource matrix for a developing world scenario. Prehosp. Disaster Med. 2010, 25, 547–552. [Google Scholar] [CrossRef]
- Ranse, J.; Hutton, A.; Turris, S.A.; Lund, A. Enhancing the minimum data set for mass-gathering research and evaluation: An integrative literature review. Prehosp. Disaster Med. 2014, 29, 280–289. [Google Scholar] [CrossRef]
- Elliott, D.; Smith, D. Football stadia disasters in the United Kingdom: Learning from tragedy? Ind. Environ. Cris. Q. 1993, 7, 205–229. [Google Scholar] [CrossRef]
- Popplewell, O. The Papers of the Popplewell Inquiry into Crowd Safety at Sports Grounds. University of Bradford Special Collections. 1985. Available online: https://www.bradford.ac.uk/library/special-collections/collections/papers-of-the-popplewell-inquiry/l (accessed on 28 June 2021).
- Rt Hon Lord Justice Taylor. Final Report into the Hillsborough Stadium Disaster. 1989. Available online: https://www.jesip.org.uk/uploads/media/incident_reports_and_inquiries/Hillsborough%20Stadium%20Disaster%20final%20report.pdf (accessed on 28 June 2021).
- Impact of the COVID-19 Pandemic on Association Football [Internet]. 2020. Available online: https://en.wikipedia.org/wiki/Impact_of_the_COVID-19_pandemic_on_association_football (accessed on 22 July 2020).
- ESPN. Coronavirus: Player at Italian Third Tier is First European Footballer Diagnosed; ESPN: Bristol, CT, USA, 2020. [Google Scholar]
- Corsini, A.; Bisciotti, G.N.; Eirale, C.; Volpi, P. Football cannot restart soon during the COVID-19 emergency! A critical perspective from the Italian experience and a call for action. Br. J. Sports Med. 2020, 54, 1186–1187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beijing Halts Sports Events after New Covid Cases. 2020. Available online: https://www.sportbusiness.com/news/beijing-halts-sports-events-after-new-covid-cases/ (accessed on 22 July 2020).
- Amid COVID-19 outbreak, J. League Postpones All Matches until March 15. Available online: https://www.japantimes.co.jp/sports/2020/02/25/soccer/j-league/jleague-cancels-levain-cup-coronavirus/ (accessed on 22 July 2020).
- Wuhan Coronavirus: Lunar New Year Cup Cancelled by Government Just Hours after HKFA Promotes The Event. Available online: https://www.scmp.com/sport/hong-kong/article/3047415/wuhan-virus-lunar-new-year-cup-go-ahead-hong-kong-despite (accessed on 22 July 2020).
- OFFICIAL: CAF Postpone Interclubs Competitions Semi-Finals. Available online: https://www.kingfut.com/2020/09/10/caf-interclubs-competitions-postponed/ (accessed on 22 July 2020).
- Coronavirus: Saudi Football League Looking at August 20 Return Date. Available online: https://english.alarabiya.net/coronavirus/2020/05/13/Coronavirus-Saudi-football-league-looking-at-August-20-return-date (accessed on 22 July 2020).
- Arabian Business. Almost 100 Saudi Football Players, Staff Test Positive for Covid-19; Arabian Business: Dubai, United Arab Emirates, 2020. [Google Scholar]
- WHO. Guidance on Mass Gatherings & Sports Events; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- WHO. Considerations for Sports Federations/Sports Event Organizers When Planning Mass Gatherings in the Context of COVID-19; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Saudi Center for Disease Prevention and Control Sports Exercise Protocols. 2020. Available online: https://covid19.cdc.gov.sa/professionals-health-workers/preventive-protocols-from-29-10-1441/sports-exercise-protocols-en/ (accessed on 28 June 2021).
- The Official Saudi Press Agency. Prince Mohammed bin Salman Cup’s Professional League to Resume, with Precautionary Measures; The Official Saudi Press Agency: Riyadh, Saudi Arabia, 2020. [Google Scholar]
- Al Hilal-Update on AFC Champions League. AFC Champions League. 2020. Available online: https://www.the-afc.com/competitions/afc-champions-league/latest/news/latest-update-on-afc-champions-league-west-x5334 (accessed on 28 June 2021).
- Kramer, E.; Dvořák, J. Football Emergency Medicine Manual, 2nd ed.; FIFA: Zürich, Switzerland, 2015. [Google Scholar]
- Alaska, Y.A.; Aldawas, A.D.; Aljerian, N.A.; Memish, Z.A.; Suner, S. The impact of crowd control measures on the occurrence of stampedes during Mass Gatherings: The Hajj experience. Travel Med. Infect. Dis. 2017, 15, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Johansson, A.; Batty, M.; Hayashi, K.; Al Bar, O.; Marcozzi, D.; Memish, Z.A. Crowd and environmental management during mass gatherings. Lancet Infect. Dis. 2012, 12, 150–156. [Google Scholar] [CrossRef] [Green Version]
- Sharma, U.; Desikachari, B.; Sarma, S. Content validity of the newly developed risk assessment tool for religious mass gathering events in an Indian setting (mass gathering risk assessment tool-MGRAT). J. Fam. Med. Prim. Care 2019, 8, 2207. [Google Scholar] [CrossRef]
- Gallego, V.; Berberian, G.; Lloveras, S.; Verbanaz, S.; Chaves, T.S.S.; Orduna, T.; Rodriguez-Morales, A.J. The 2014 FIFA World Cup: Communicable disease risks and advice for visitors to Brazil—A review from the Latin American society for travel medicine (SLAMVI). Travel Med. Infect. Dis. 2014, 12, 208–218. [Google Scholar] [CrossRef]
- Khorram-Manesh, A. Facilitating multiagency collaboration before mass gatherings—The development of MAGRAT (mass gathering risk assessment tool). Biomed. J. Sci. Tech. Res. 2020, 24, 18607–18616. [Google Scholar] [CrossRef] [Green Version]
- Sharma, U.; Desikachari, B.R.; Sarma, S. Protocol for development of a risk assessment tool for planning and management of religious mass-gathering events of India—A health system-strengthening initiative. Pilot Feasibility Stud. 2019, 5, 1–9. [Google Scholar] [CrossRef]
- WHO. WHO Mass Gathering COVID-19 Risk Assessment Tool—Generic Events. Available online: https://www.who.int/publications/i/item/10665-333185 (accessed on 12 September 2021).
- COVID-19 Mass Gathering Event Risk Assessment Tool | East Cambridgeshire District Council. Available online: https://www.eastcambs.gov.uk/community/covid-19-mass-gathering-event-risk-assessment-tool (accessed on 12 September 2021).
- McCloskey, B.; Zumla, A.; Lim, P.L.; Endericks, T.; Arbon, P.; Cicero, A.; Borodina, M. A risk-based approach is best for decision making on holding mass gathering events. Lancet 2020, 395, 1256–1257. [Google Scholar] [CrossRef]
- Khan, A.; Yezli, S.; Ciottone, G.; Borodina, M.; Ranse, J.; Gautret, P.; Turris, S.; Lund, A.; Memish, Z.A.; Sharma, A.; et al. Recommendations from the 4th international conference on mass gatherings medicine, Saudi Arabia. East. Mediterr. Health J. 2020, 26, 503–505. [Google Scholar] [CrossRef] [Green Version]
- Bieh, K.L.; Khan, A.; El-Ganainy, A.; Alotaibi, B.; Ghallab, S.; Abdulmalek, N.; Mukhtar, N.; Jokhdar, H. Guidance for health risk assessment at recurrent mass gatherings: The Jeddah tool framework. Prehosp. Disaster Med. 2021, 36, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Saudi Arabia. COVID-19 Health Risk Assessment (HRA) Related to Infection Transmission in Events and Gatherings—Salem Tool (V 1.0); Ministry of Health Saudi Arabia: Riyadh, Saudi Arabia, 2020.
- Khan, A.; Lezor Bieh, K.; El-Ganainy, A.; Ghallab, S.; Assiri, A.; Jokhdar, H.; Lezor, K.; Manager, B. Estimating the COVID-19 risk during the Hajj pilgrimage. J. Travel Med. 2020, taaa157. [Google Scholar] [CrossRef] [PubMed]
- Yezli, S.; Khan, A.A. The Jeddah tool. A health risk assessment framework for mass gatherings. Saudi Med. J. 2020, 41, 121–122. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Hajj and Umrah. Hajj 1441H is Decided to Take Place This Year with Limited Number of Pilgrims from All Nationalities Residing in Saudi Arabia. Available online: https://www.spa.gov.sa/viewfullstory.php?lang=en&newsid=2100951 (accessed on 18 September 2021).
- Jokhdar, H.; Khan, A.; Asiri, S.; Motair, W.; Assiri, A.; Alabdulaali, M. COVID-19 mitigation plans during Hajj 2020: A success story of zero cases. Health Secur. 2020, 19, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Memish, Z.A.; Stephens, G.M.; Steffen, R.; Ahmed, Q.A. Emergence of medicine for mass gatherings: Lessons from the Hajj. Lancet Infect. Dis. 2012, 12, 56–65. [Google Scholar] [CrossRef]
| Location and Stadium | Football Event | Incident | Casualties | Date |
|---|---|---|---|---|
| Bolton, England Burnden Park Stadium [35] | English Football Association Challenge Cup match | A wall collapsed in the stadium before the match crushing fans and sparking a stampede | 33 deaths 400 injured | March 1946 |
| Santiago, Chile Estadio Nacional de Chile [36] | The finals match of the South American soccer tournament | Human crush between fans entering the stadium | 6 deaths Unknown injuries | March 1955 |
| Lima, Peru The National Stadium [36] | Olympic qualifying match | Human crush and asphyxiation between fans due to overcrowded exiting after police fired tear gas | 318 deaths 500 injured | May 1964 * |
| Kayseri, Turkey Kayseri Atatürk Stadium [37] | Turkish league match | Human crush sparked by stone-throwing and weapon clashes between fans of the two teams | 40 deaths 600 injured | September 1967 |
| Buenos Aires, Argentina [38] | First-division league match | Asphyxiation and Human crush against closed Stadium exit between fans unaware of the closed passage | 74 deaths 150 injured | June 1968 |
| Glasgow, UK Ibrox Stadium [39] | Football match | Human crush between fans entering and exiting the stadium | 66 deaths 140 injured | January 1971 |
| Salvador, Brazil Estádio Fonte Nova [36] | Football match | Human crush sparked by a fight between fans | 4 deaths 1500 injured | March 1971 |
| Cairo, Egypt Zamalek stadium [40] | Friendly football match | Human crush due to overcrowding during the influx of fans | 49 deaths 50 injured | February 1974 |
| Yaounde, Cameroon [40] | World Cup qualifying match | Mass fight among fans of two teams | 2 deaths Unknown injuries | October 1976 |
| Port-au-Prince, Haiti [41] | World Cup qualifying match | Human crush and gunshots sparked by panic after firecracker | 6 deaths | December 1976 |
| Piraeus, Greece Karaiskakis Stadium [36] | Derby football match | Human crush among fans exiting stadium through the partially closed exit | 21 deaths 55 injured | February 1981 |
| Moscow, Soviet Union Central Lenin Stadium [42] | European Cup match | Human crush and asphyxiation between exiting and returning fans | 66 deaths 61 injured | October 1982 |
| Bradford, UK Valley Parade stadium [43] | English league football match | Fire in the Valley Parade stadium | 56 deaths 240 injured | May 1985 |
| Brussels, Belgium Heysel Stadium [44] | European Champions Cup Final match | Human crush among Italian fans escaping English fans against a collapsing wall | 39 deaths 600 injured | May 1985 |
| Tripoli, Libya Tripoli International Stadium [45] | Football match | Human crush sparked by knife-wielding fan and triggering the collapse of a part of the stadium | 20 deaths Unknown injuries | March 1987 |
| Kathmandu, Nepal Dasarath Rangasala Stadium [46] | International football match | Human crush against closed stadium exit sparked by a hailstorm | 93 deaths 100 injured | March 1988 |
| Sheffield, UK Hillsborough Stadium [35] | The FA Cup semi-final match | Human crush due to overcrowding during the influx of fans | 96 deaths 766 injured | April 1989 |
| Orkney, South Africa Oppenheimer Stadium [47] | A friendly association football match | Human crush among fans escaping from fan brawls | 43 deaths 100 injured | January 1991 |
| Bastia, the French island of Corsica Stade Armand Cesari [48] | French Cup semi-final match | Stadium terrace collapse underneath fans before the match | 17 deaths 1900 injured | May 1992 |
| Lusaka, Zambia Independence Stadium [45] | World Cup qualifying game. | Human crush during overcrowded fan exit celebrating victory | 15 deaths 52 injured | June 1996 |
| Guatemala City, Guatemala Estadio Doroteo Guamuch Flores [45] | World Cup qualifying match | Human crush due to overcrowding during the influx of fans | 83 deaths 140 injured | October 1996 |
| Harare, Zimbabwe National Sports Stadium [49] | World Cup qualifying match | Human crush during overcrowded fan exit after police fired tear gas | 13 deaths Unknown injuries | July 2000 |
| Salvador, Brazil Estádio Fonte Nova [45] | Local derby match | Upper terrace collapse | 7 deaths 10 injuries | 2007 |
| Johannesburg, South Africa Ellis Park Stadium [47] | South African league match | Human crush due to overcrowding during the influx of fans | 43 deaths Unknown injuries | April 2001 |
| Abidjan, Ivory Coast Stade Félix Houphouët-Boigny [50] | World Cup qualification match | Human crush due to overcrowding of fans before the match after police fired tear gas | 20 deaths 135 injuries | March 2009 |
| Port Said, Egypt Port Said Stadium [51] | Egyptian Premier League football match | Human crush among fans exiting the stadium | 74 deaths Unknown injuries | February 2012 |
| Kinshasa, Congo Tata Raphaël Stadium [45] | Congo league match | Human crush among fans sparked by police firing tear gas | 15 deaths 24 injuries | May 2014 |
| Cairo, Egypt Air Defense Stadium [52] | Egyptian Premier League football match | Human crush due to overcrowding during the influx of fans sparked by police firing tear gas | 28 deaths Unknown injuries | February 2015 |
| 1 | The category of the event (music festivals, exhibitions, or sports competitions, etc.) |
| 2 | The expected number of attendees |
| 3 | The criteria of attendees (families, sports club fans, community support groups, international stars, or VIP) |
| 4 | The nature of attendees’ movements (static audience, young children who need constant monitoring, people with motor disabilities, people who require personal assistance) |
| 5 | The age group of attendees |
| 6 | The site of the event (open area, specific walled area, inside a building, spacious or narrow area) |
| 7 | Available health resources (district hospitals, public hospitals, small hospitals, mobile clinic) |
| 8 | The distance to the nearest public or reference hospital |
| 9 | Time for the nearest general or reference hospital |
| 10 | Duration of the event per day |
| 11 | The number of days for the event |
| 12 | Possibility of drugs misuse |
| 13 | The time of the event |
| 14 | The expected temperature at the venue of the event |
| 15 | Types of activities in the event (high-risk activities, high competition among participants (ex: wrestling), the interaction between the attendees (for example the final matches), presence of cars or vehicles, including offers or race, presence of fireworks, presence of firearms or flames) |
| 16 | Accidents that occurred in previous activities or the same place or expected accidents |
| 17 | Food catering services (applying and controlling the specified standards for food catering services, municipality approval is obtained, and valid food catering services are provided) |
| Low-risk events | Events categorized as low severity recommend risk communication (at the population level), improved monitoring and surveillance, and medical care for the event |
| Medium-risk events | Medium severity events recommend risk communication (dedicated to the event), active surveillance, medical care for the event, and protective measures for the event (personal protective equipment, handwashing) |
| High-risk events | High-risk events recommend reducing the number of guests/visitors, adjustment of the crowd flow and seating arrangements, and reducing communication between participants, regulators, and service providers |
| Severe-risk events | Events with severe risk recommend restructuring the event, changing or moving the event site, postponing or rescheduling the event, or canceling the event |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, A.A.; Sabbagh, A.Y.; Ranse, J.; Molloy, M.S.; Ciottone, G.R. Mass Gathering Medicine in Soccer Leagues: A Review and Creation of the SALEM Tool. Int. J. Environ. Res. Public Health 2021, 18, 9973. https://doi.org/10.3390/ijerph18199973
Khan AA, Sabbagh AY, Ranse J, Molloy MS, Ciottone GR. Mass Gathering Medicine in Soccer Leagues: A Review and Creation of the SALEM Tool. International Journal of Environmental Research and Public Health. 2021; 18(19):9973. https://doi.org/10.3390/ijerph18199973
Chicago/Turabian StyleKhan, Anas A., Abdulrahman Y. Sabbagh, Jamie Ranse, Michael S. Molloy, and Gregory R. Ciottone. 2021. "Mass Gathering Medicine in Soccer Leagues: A Review and Creation of the SALEM Tool" International Journal of Environmental Research and Public Health 18, no. 19: 9973. https://doi.org/10.3390/ijerph18199973
APA StyleKhan, A. A., Sabbagh, A. Y., Ranse, J., Molloy, M. S., & Ciottone, G. R. (2021). Mass Gathering Medicine in Soccer Leagues: A Review and Creation of the SALEM Tool. International Journal of Environmental Research and Public Health, 18(19), 9973. https://doi.org/10.3390/ijerph18199973






