Regional Prevalence of Dyslipidemia, Healthcare Utilization, and Cardiovascular Disease Risk in South Korean: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Database and Data Collection
2.2. Variables
2.3. Ethical Consideration
2.4. Patient and Public Involvement
2.5. Statistical Analysis
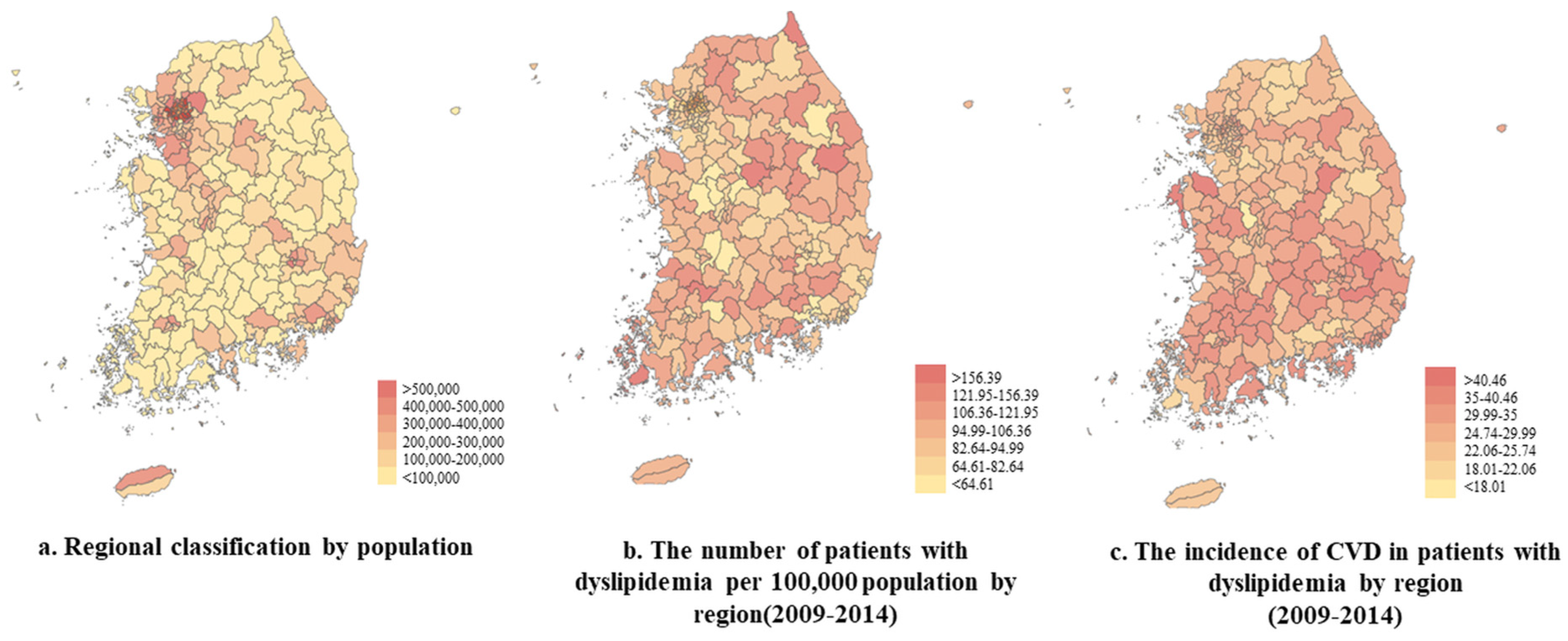
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Roth, G.A.; Naghavi, M.; Parmar, P.; Krishnamurthi, R.; Chugh, S.; Mensah, G.A.; Norrving, B.; Shiue, I.; Ng, M.; et al. Global burden of stroke and risk factors in 188 Ctries, during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016, 15, 913–924. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.; Sui, X.; Church, T.S.; Lavie, C.J.; Jackson, A.S.; Blair, S.N. Changes in fitness and fatness on the development of cardiovascular disease risk factors: Hypertension, metabolic syndrome, and hypercholesterolemia. J. Am. Coll. Cardiol. 2012, 59, 665–672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Purnell, T.S.; Calhoun, E.A.; Golden, S.H.; Halladay, J.R.; Krok-Schoen, J.L.; Appelhans, B.M.; Cooper, L.A. Achieving Health Equity: Closing the Gaps in Health Care Disparities, Interventions, and Research. Health Aff. 2016, 35, 1410–1415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graham, G. Disparities in cardiovascular disease risk in the United States. Curr. Cardiol. Rev. 2015, 11, 238–245. [Google Scholar] [CrossRef] [Green Version]
- Valderrama, A.L.; Gillespie, C.; Mercado, C. Racial/Ethnic disparities in the awareness, treatment, and control of hypertension—United States, 2003–2010. MMWR. Morb. Mortal. Wkly. Rep. 2013, 62, 351. [Google Scholar]
- Matthews, K.A.; Croft, J.B.; Liu, Y.; Lu, H.; Kanny, D.; Wheaton, A.G.; Cunningham, T.J.; Khan, L.K.; Caraballo, R.S.; Holt, J.B.; et al. Health-related behaviors by urban-rural county classification—United States, 2013. Mmwr Surveill. Summ. 2017, 66, 1. [Google Scholar] [CrossRef]
- Hutchinson, R.N.; Shin, S. Systematic review of health disparities for cardiovascular diseases and associated factors among American Indian and Alaska Native populations. PLoS ONE 2014, 9, e80973. [Google Scholar] [CrossRef]
- Caldwell, J.T.; Ford, C.L.; Wallace, S.P.; Wang, M.C.; Takahashi, L.M. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. Am. J. Public Health 2016, 106, 1463–1469. [Google Scholar] [CrossRef]
- Singh, G.K.; Siahpush, M. Widening rural–urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. J. Urban Health 2014, 91, 272–292. [Google Scholar] [CrossRef]
- Bove, A.A.; Santamore, W.P.; Homko, C.; Kashem, A.; Cross, R.; McConnell, T.R.; Shirk, G.; Menapace, F. Reducing cardiovascular disease risk in medically underserved urban and rural communities. Am. Heart J. 2011, 161, 351–359. [Google Scholar] [CrossRef]
- Boo, S.; Yoon, Y.J.; Oh, H. Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database: A cross-sectional analysis. Medicine 2018, 97, e13713. [Google Scholar] [CrossRef] [PubMed]
- Rhee, E.-J.; Kim, H.C.; Kim, J.H.; Lee, E.Y.; Kang, J.H.; Kim, E.M.; Song, Y.; Lim, J.H.; Kim, H.J.; Choi, S.; et al. 2018 Guidelines for the Management of Dyslipidemia in Korea. J. Lipid Atheroscler. 2019, 8, 78–131. [Google Scholar] [CrossRef] [PubMed]
- Supiyev, A.; Nurgozhin, T.; Zhumadilov, Z.; Peasey, A.; Hubacek, J.A.; Bobak, M. Prevalence, awareness, treatment and control of dyslipidemia in older persons in urban and rural population in the Astana region, Kazakhstan. BMC Public Health 2017, 17, 651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Opoku, S.; Gan, Y.; Fu, W.; Chen, D.; Addo-Yobo, E.; Trofimovitch, D.; Yue, W.; Yan, F.; Wang, Z.; Lu, Z. Prevalence and risk factors for dyslipidemia among adults in rural and urban China: Findings from the China National Stroke Screening and prevention project (CNSSPP). BMC Public Health 2019, 19, 1500. [Google Scholar] [CrossRef]
- Gökler, M.E.; Buğrııl, N.; Metintaş, S.; Kalyoncu, C. Adolescent obesity and associated cardiovascular risk factors of rural and urban life (Eskisehir, Turkey). Cent. Eur. J. Public Health 2015, 23, 20–25. [Google Scholar] [CrossRef] [Green Version]
- Otsubo, T.; Goto, E.; Morishima, T.; Ikai, H.; Yokota, C.; Minematsu, K.; Imanaka, Y. Regional variations in in-hospital mortality, care processes, and spending in acute ischemic stroke patients in Japan. J. Stroke Cerebrovasc. Dis. 2015, 24, 239–251. [Google Scholar] [CrossRef]
- Seabury, S.; Bognar, K.; Xu, Y.; Huber, C.; Commerford, S.R.; Tayama, D. Regional disparities in the quality of stroke care. Am. J. Emerg. Med. 2017, 35, 1234–1239. [Google Scholar] [CrossRef] [Green Version]
- Jang, S.; Lee, J. Prevalence and management of dyslipidemia, hypertension, diabetes among adults in Gangwon-do, Korea: The 2013–2014 KNHSP. J. Korea Acad. Ind. Coop. Soc. 2017, 18, 625–636. [Google Scholar]
- Lee, J.; Lee, J.S.; Park, S.-H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service–National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2017, 46, e15. [Google Scholar] [CrossRef]
- Kim, H.-J.; Ruger, J.P. Socioeconomic disparities in behavioral risk factors and health outcomes by gender in the Republic of Korea. BMC Public Health 2010, 10, 195. [Google Scholar] [CrossRef] [Green Version]
- Park, E. A comparison of community health status by region and an investigation of related factors using community health indicators. J. Korean Acad. Community Health Nurs. 2012, 23, 31–39. [Google Scholar] [CrossRef] [Green Version]
- Vinueza, R.; Boissonnet, C.P.; Acevedo, M.; Uriza, F.; Benitez, F.J.; Silva, H.; Schargrodsky, H.; Champagne, B.; Wilson, E. Dyslipidemia in seven Latin American cities: CARMELA study. Prev. Med. 2010, 50, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.C. Epidemiology of dyslipidemia in Korea. J. Korean Med. Assoc. 2016, 59, 352–357. [Google Scholar] [CrossRef] [Green Version]
- Zhao, W.-H.; Zhang, J.; Zhai, Y.; You, Y.; Man, Q.-Q.; Wang, C.-R.; Li, H.; Li, Y.; Yang, X.-G. Blood lipid profile and prevalence of dyslipidemia in Chinese adults. Biomed. Environ. Sci. BES 2007, 20, 329–335. [Google Scholar] [PubMed]
- Graves, B.A. Integrative Literature Review: A Review of Literature Related to Geographical Information Systems, Healthcare Access, and Health Outcomes. Perspect. Health Inf. Manag. 2008, 5, 5. [Google Scholar]
- Crosby, R.A.; Wendel, M.L.; Vanderpool, R.C.; Casey, B.R. Rural Populations and Health: Determinants, Disparities, and Solutions; John Wiley & Sons: San Francisco, CA, USA, 2012. [Google Scholar]

| Variables | CVD | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Yes | No | Total | |||||
| Region | |||||||
| <100,000 population | 1635 | (28.8) | 4039 | (71.2) | 5674 | (10.8) | <0.0001 |
| 100,000–200,000 | 1674 | (24.8) | 5085 | (75.2) | 6759 | (12.9) | |
| 200,000–300,000 | 3042 | (23.1) | 10,120 | (76.9) | 13,162 | (25.1) | |
| 300,000–400,000 | 2517 | (23.1) | 8405 | (77.0) | 10,922 | (20.9) | |
| 400,000–500,000 | 2095 | (22.2) | 7357 | (77.8) | 9452 | (18.1) | |
| >500,000 | 1480 | (23.1) | 4928 | (76.9) | 6408 | (12.2) | |
| Diabetes | |||||||
| Yes | 3832 | (30.9) | 8556 | (69.1) | 12,388 | (23.7) | <0.0001 |
| No | 8611 | (21.5) | 31,378 | (78.5) | 39,989 | (76.4) | |
| Prescribed Medication | |||||||
| Yes | 1955 | (17.4) | 9257 | (82.6) | 11,212 | (21.4) | <0.0001 |
| No | 10,488 | (25.5) | 30,677 | (74.5) | 41,165 | (78.6) | |
| Risk score | |||||||
| 0 | 4363 | (16.6) | 21,955 | (83.4) | 26,318 | (50.3) | <0.0001 |
| 1 | 5374 | (27.9) | 13,884 | (72.1) | 19,258 | (36.8) | |
| 2 | 2370 | (38.4) | 3805 | (61.6) | 6175 | (11.8) | |
| ≥3 | 336 | (53.7) | 290 | (46.3) | 626 | (1.2) | |
| CCI | 2.29 | ±2.55 | 1.73 | ±2.11 | 1.86 | ±2.23 | <0.0001 |
| BMI | 24.83 | ±3.23 | 24.07 | ±3.13 | 24.25 | ±3.17 | <0.0001 |
| Healthcare utilization(per year) | |||||||
| Costs (Unit: KRW) | 83,887 | ±133,275 | 64,262 | ±153,921 | 68,924 | ±149,507 | <0.0001 |
| outpatient visiting | 4.18 | ± 3.08 | 2.93 | ± 2.58 | 3.22 | ± 2.76 | <0.0001 |
| Sex | |||||||
| Male | 5813 | (24.1) | 18,308 | (75.9) | 24,121 | (46.1) | 0.0906 |
| Female | 6630 | (23.5) | 21,626 | (76.5) | 28,256 | (54.0) | |
| Age | |||||||
| 20–34 | 265 | (7.7) | 3184 | (92.3) | 3449 | (6.6) | <.0001 |
| 35–49 | 2795 | (16.7) | 13,984 | (83.3) | 16,779 | (32.0) | |
| 50–64 | 6492 | (26.0) | 18,502 | (74.0) | 24,994 | (47.7) | |
| ≥65 | 2891 | (40.4) | 4264 | (59.6) | 7155 | (13.7) | |
| Income | |||||||
| Low | 2999 | (24.2) | 9379 | (75.8) | 12,378 | (23.6) | 0.1396 |
| Low-moderate | 2989 | (23.3) | 9865 | (76.8) | 12,854 | (24.5) | |
| Moderate-high | 2754 | (23.4) | 9042 | (76.7) | 11,796 | (22.5) | |
| High | 3701 | (24.1) | 11,648 | (75.9) | 15,349 | (29.3) | |
| Insurance | |||||||
| Medicaid | 325 | (28.7) | 806 | (71.3) | 1131 | (2.2) | <0.0001 |
| Self-Employed | 4173 | (25.2) | 12,375 | (74.8) | 16,548 | (31.6) | |
| Employees | 7945 | (22.9) | 26,753 | (77.1) | 34,698 | (66.3) | |
| Year of diagnosis | |||||||
| 2009 | 2146 | (33.8) | 4208 | (66.2) | 6354 | (12.1) | <0.0001 |
| 2010 | 3866 | (34.1) | 7487 | (66.0) | 11,353 | (21.7) | |
| 2011 | 2348 | (25.7) | 6798 | (74.3) | 9146 | (17.5) | |
| 2012 | 1747 | (20.2) | 6898 | (79.8) | 8645 | (16.5) | |
| 2013 | 1313 | (16.0) | 6919 | (84.1) | 8232 | (15.7) | |
| 2014 | 1023 | (11.8) | 7624 | (88.2) | 8647 | (16.5) | |
| Total | 12,443 | (23.8) | 39,934 | (76.2) | 52,377 | (100.0) | |
| Variables | CVD | Types of CVD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ischemic Heart Disease | Cerebrovascular Disease | Hypertension | ||||||||||
| OR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |||||
| Region | ||||||||||||
| <100,000 population | 1.147 | 1.051 | 1.252 | 1.137 | 1.146 | 1.561 | 1.181 | 1.008 | 1.384 | 1.056 | 0.973 | 1.146 |
| 100,000–200,000 | 1.055 | 0.969 | 1.149 | 1.169 | 1.000 | 1.366 | 1.105 | 0.941 | 1.297 | 0.995 | 0.918 | 1.079 |
| 200,000–300,000 | 1.041 | 0.966 | 1.122 | 1.263 | 1.100 | 1.450 | 1.172 | 1.018 | 1.350 | 0.976 | 0.909 | 1.049 |
| 300,000–400,000 | 1.016 | 0.940 | 1.098 | 1.105 | 0.956 | 1.276 | 1.008 | 0.868 | 1.171 | 0.998 | 0.927 | 1.074 |
| 400,000–500,000 | 0.970 | 0.895 | 1.051 | 1.111 | 0.958 | 1.289 | 1.048 | 0.900 | 1.221 | 0.930 | 0.862 | 1.005 |
| >500,000 | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - |
| Diabetes | ||||||||||||
| Yes | 1.070 | 1.017 | 1.125 | 1.008 | 0.924 | 1.010 | 1.063 | 0.972 | 1.163 | 1.058 | 1.009 | 1.109 |
| No | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - |
| Prescribed Medication | ||||||||||||
| Yes | 0.730 | 0.689 | 0.774 | 0.712 | 0.637 | 0.796 | 0.774 | 0.692 | 0.867 | 0.732 | 0.691 | 0.776 |
| No | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - |
| Risk score | ||||||||||||
| 0 | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - |
| 1 | 1.460 | 1.387 | 1.536 | 1.336 | 1.219 | 1.465 | 1.205 | 1.095 | 1.326 | 1.440 | 1.368 | 1.516 |
| 2 | 2.035 | 1.898 | 2.182 | 1.553 | 1.377 | 1.751 | 1.348 | 1.190 | 1.528 | 2.003 | 1.878 | 2.137 |
| ≥3 | 3.591 | 3.010 | 4.283 | 2.022 | 1.545 | 2.648 | 1.808 | 1.385 | 2.362 | 3.129 | 2.745 | 3.567 |
| CCI | 1.066 | 1.055 | 1.077 | 1.094 | 1.076 | 1.112 | 1.126 | 1.108 | 1.145 | 1.034 | 1.024 | 1.044 |
| BMI | 1.082 | 1.074 | 1.089 | 1.032 | 1.019 | 1.045 | 1.007 | 0.993 | 1.021 | 1.086 | 1.079 | 1.093 |
| Sex | ||||||||||||
| Male | 1.025 | 0.978 | 1.075 | 1.254 | 1.155 | 1.361 | 1.099 | 1.009 | 1.196 | 0.987 | 0.944 | 1.033 |
| Female | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - |
| Age | ||||||||||||
| 20–34 | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - |
| 35–49 | 2.285 | 1.997 | 2.613 | 2.941 | 2.106 | 4.106 | 3.348 | 2.132 | 5.259 | 2.044 | 1.782 | 2.345 |
| 50–64 | 3.623 | 3.169 | 4.143 | 5.151 | 3.700 | 7.172 | 7.756 | 4.964 | 12.117 | 2.821 | 2.460 | 3.234 |
| ≥65 | 6.195 | 5.364 | 7.155 | 7.028 | 4.989 | 9.899 | 15.884 | 10.094 | 24.994 | 4.326 | 3.744 | 4.999 |
| Income | ||||||||||||
| Low | 1.082 | 1.017 | 1.150 | 0.918 | 0.824 | 1.022 | 0.891 | 0.795 | 0.998 | 1.195 | 1.127 | 1.267 |
| Low-moderate | 1.085 | 1.023 | 1.151 | 0.930 | 0.839 | 1.031 | 0.962 | 0.863 | 1.071 | 1.166 | 1.102 | 1.234 |
| Moderate-high | 1.037 | 0.976 | 1.102 | 0.919 | 0.829 | 1.020 | 0.931 | 0.835 | 1.038 | 1.082 | 1.021 | 1.147 |
| High | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - |
| Insurance | ||||||||||||
| Medicaid | 1.212 | 1.047 | 1.403 | 1.229 | 0.959 | 1.575 | 1.733 | 1.375 | 2.186 | 1.041 | 0.908 | 1.192 |
| Self-Employed | 1.044 | 0.997 | 1.094 | 1.054 | 0.972 | 1.143 | 1.035 | 0.951 | 1.127 | 1.055 | 1.010 | 1.102 |
| Employees | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - |
| Year of diagnosis | ||||||||||||
| 2009 | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - | 1.000 | - | - |
| 2010 | 0.829 | 0.770 | 0.892 | 0.803 | 0.708 | 0.910 | 0.779 | 0.680 | 0.892 | 1.036 | 0.967 | 1.109 |
| 2011 | 0.600 | 0.555 | 0.648 | 0.721 | 0.629 | 0.825 | 0.704 | 0.608 | 0.816 | 0.956 | 0.887 | 1.029 |
| 2012 | 0.437 | 0.403 | 0.474 | 0.587 | 0.505 | 0.682 | 0.632 | 0.540 | 0.741 | 0.868 | 0.801 | 0.941 |
| 2013 | 0.327 | 0.300 | 0.357 | 0.580 | 0.493 | 0.683 | 0.691 | 0.583 | 0.819 | 0.835 | 0.765 | 0.911 |
| 2014 | 0.218 | 0.199 | 0.239 | 0.544 | 0.457 | 0.649 | 0.555 | 0.458 | 0.673 | 0.870 | 0.792 | 0.956 |
| Variables | Healthcare Expenditure | Outpatient Visiting | ||||
|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | |||
| Region | ||||||
| <100,000 population | 1.072 | 1.017 | 1.130 | 1.080 | 1.050 | 1.111 |
| 100,000–200,000 | 1.048 | 0.971 | 1.131 | 1.039 | 1.012 | 1.067 |
| 200,000–300,000 | 1.041 | 0.994 | 1.090 | 1.024 | 1.001 | 1.047 |
| 300,000–400,000 | 1.050 | 0.989 | 1.115 | 1.026 | 1.002 | 1.050 |
| 400,000–500,000 | 1.019 | 0.974 | 1.066 | 1.030 | 1.005 | 1.055 |
| >500,000 | 1.000 | - | - | 1.000 | - | - |
| Diabetes before dyslipidemia | ||||||
| Yes | 1.461 | 1.409 | 1.515 | 1.620 | 1.595 | 1.646 |
| No | 1.000 | - | - | 1.000 | - | - |
| Prescribed Medication | ||||||
| Yes | 0.702 | 0.680 | 0.725 | 1.018 | 1.002 | 1.035 |
| No | 1.000 | - | - | 1.000 | - | - |
| Risk score for CVD | ||||||
| 0 | 1.000 | - | - | 1.000 | - | - |
| 1 | 1.028 | 0.980 | 1.078 | 1.043 | 1.026 | 1.059 |
| 2 | 0.982 | 0.940 | 1.025 | 1.064 | 1.039 | 1.089 |
| ≥3 | 1.030 | 0.943 | 1.124 | 1.101 | 1.038 | 1.168 |
| CCI | 1.064 | 1.055 | 1.073 | 1.033 | 1.029 | 1.036 |
| BMI | 1.009 | 1.000 | 1.017 | 1.013 | 1.011 | 1.015 |
| Sex | ||||||
| Male | 0.912 | 0.880 | 0.945 | 0.887 | 0.874 | 0.901 |
| Female | 1.000 | - | - | 1.000 | - | - |
| Age | ||||||
| 20–34 | 1.000 | - | - | 1.000 | - | - |
| 35–49 | 1.071 | 0.945 | 1.215 | 1.340 | 1.300 | 1.382 |
| 50–64 | 1.119 | 0.988 | 1.267 | 1.549 | 1.502 | 1.598 |
| ≥65 | 1.145 | 0.997 | 1.314 | 1.648 | 1.589 | 1.710 |
| Income | ||||||
| Low | 0.988 | 0.930 | 1.049 | 1.047 | 1.027 | 1.067 |
| Low-moderate | 0.975 | 0.935 | 1.017 | 1.038 | 1.018 | 1.057 |
| Moderate-high | 1.018 | 0.966 | 1.072 | 1.036 | 1.017 | 1.055 |
| High | 1.000 | - | - | 1.000 | - | - |
| Insurance | ||||||
| Medicaid | 1.395 | 1.265 | 1.539 | 1.244 | 1.178 | 1.313 |
| Self-Employed | 1.023 | 0.977 | 1.072 | 1.013 | 0.998 | 1.028 |
| Employees | 1.000 | - | - | 1.000 | - | - |
| Year of diagnosis | ||||||
| 2009 | 1.000 | - | - | 1.000 | - | - |
| 2010 | 1.259 | 1.164 | 1.361 | 1.065 | 1.039 | 1.092 |
| 2011 | 1.112 | 1.046 | 1.183 | 0.983 | 0.958 | 1.009 |
| 2012 | 0.996 | 0.933 | 1.063 | 0.959 | 0.934 | 0.985 |
| 2013 | 0.983 | 0.914 | 1.057 | 0.927 | 0.903 | 0.953 |
| 2014 | 0.971 | 0.911 | 1.034 | 0.929 | 0.904 | 0.955 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, K.-T.; Kim, S. Regional Prevalence of Dyslipidemia, Healthcare Utilization, and Cardiovascular Disease Risk in South Korean: A Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 538. https://doi.org/10.3390/ijerph18020538
Han K-T, Kim S. Regional Prevalence of Dyslipidemia, Healthcare Utilization, and Cardiovascular Disease Risk in South Korean: A Retrospective Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(2):538. https://doi.org/10.3390/ijerph18020538
Chicago/Turabian StyleHan, Kyu-Tae, and SeungJu Kim. 2021. "Regional Prevalence of Dyslipidemia, Healthcare Utilization, and Cardiovascular Disease Risk in South Korean: A Retrospective Cohort Study" International Journal of Environmental Research and Public Health 18, no. 2: 538. https://doi.org/10.3390/ijerph18020538





