Is the Association between Postpartum Depression and Early Maternal–Infant Relationships Contextually Determined by Avoidant Coping in the Mother?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Sample
2.2. Variables and Instruments
2.2.1. First Trimester of Pregnancy
2.2.2. Four Months after Childbirth
2.3. Procedure
2.4. Statistical Analysis
3. Results
3.1. Means, Standard Deviations, and Pearson Correlations between Study Variables
3.2. Moderation Analysis and Multivariate Linear Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Law, K.H.; Dimmock, J.; Guelfi, K.J.; Nguyen, T.; Gucciardi, D.; Jackson, B. Stress, Depressive Symptoms, and Maternal Self-Efficacy in First-Time Mothers: Modelling and Predicting Change across the First Six Months of Motherhood. Appl. Psychol. Health Well-Being 2019, 11, 126–147. [Google Scholar] [CrossRef] [Green Version]
- Hammer, P.; Hageman, I.; Garde, A.; Begtrup, L.; Flachs, E.; Hansen, J.; Hansen, Å.; Hougaard, K.; Kolstad, H.; Larsen, A.; et al. Night work and postpartum depression: A national register-based cohort study. Scand. J. Work. Environ. Health 2019, 45, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Dadi, A.F.; Miller, E.R.; Mwanri, L. Postnatal depression and its association with adverse infant health outcomes in low- and middle-income countries: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2020, 20, 416. [Google Scholar] [CrossRef] [PubMed]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.Y.; Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health 2019, 15, 1745506519844044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Śliwerski, A.; Kossakowska, K.; Jarecka, K.; Świtalska, J.; Bielawska-Batorowicz, E. The Effect of Maternal Depression on Infant Attachment: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 2675. [Google Scholar] [CrossRef] [Green Version]
- Turkcapar, A.F.; Kadıoğlu, N.; Aslan, E.; Tunc, S.; Zayıfoğlu, M.; Mollamahmutoğlu, L. Sociodemographic and clinical features of postpartum depression among Turkish women: A prospective study. BMC Pregnancy Childbirth 2015, 15, 108. [Google Scholar] [CrossRef] [Green Version]
- Spinelli, M.G. Postpartum Psychosis: Detection of Risk and Management. Am. J. Psychiatry 2009, 166, 405–408. [Google Scholar] [CrossRef]
- Guo, N.; Bindt, C.; Te Bonle, M.; Appiah-Poku, J.; Hinz, R.; Barthel, D.; Koffi, M.; Posdzich, S.; Deymann, S.; Barkmann, C.; et al. Association of Antepartum and Postpartum Depression in Ghanaian and Ivorian Women With Febrile Illness in Their Offspring: A Prospective Birth Cohort Study. Am. J. Epidemiol. 2013, 178, 1394–1402. [Google Scholar] [CrossRef] [Green Version]
- Cicchetti, D.; Rogosch, F.A.; Toth, S.L. Maternal depressive disorder and contextual risk: Contributions to the development of attachment insecurity and behavior problems in toddlerhood. Dev. Psychopathol. 1998, 10, 283–300. [Google Scholar] [CrossRef]
- Grace, S.L.; Evindar, A.; Stewart, D.E. The effect of postpartum depression on child cognitive development and behavior: A review and critical analysis of the literature. Arch. Womens Ment. Health 2003, 6, 263–274. [Google Scholar] [CrossRef]
- Kurstjens, S.; Wolke, D. Effects of Maternal Depression on Cognitive Development of Children Over the First 7 Years of Life. J. Child Psychol. Psychiatry 2001, 42, 623–636. [Google Scholar] [CrossRef]
- Anoop, S. Maternal depression and low maternal intelligence as risk factors for malnutrition in children: A community based case-control study from South India. Arch. Dis. Child. 2004, 89, 325–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahman, A.; Harrington, R.; Bunn, J. Can maternal depression increase infant risk of illness and growth impairment in developing countries? Child Care Health Dev. 2002, 28, 51–56. [Google Scholar] [CrossRef]
- World Health Organization. Maternal Mental Health and Child Health and Development in Low and Middle-Income Countries: Report of the Meeting, Geneva, Switzerland, 30 January–1 February 2008. Available online: https://apps.who.int/iris/handle/10665/43975 (accessed on 23 November 2020).
- Zhu, P.; Sun, M.-S.; Hao, J.-H.; Chen, Y.-J.; Jiang, X.-M.; Tao, R.-X.; Huang, K.; Tao, F.-B. Does prenatal maternal stress impair cognitive development and alter temperament characteristics in toddlers with healthy birth outcomes? Dev. Med. Child Neurol. 2014, 56, 283–289. [Google Scholar] [CrossRef] [Green Version]
- Conroy, S.; Pariante, C.M.; Marks, M.N.; Davies, H.A.; Farrelly, S.; Schacht, R.; Moran, P. Maternal Psychopathology and Infant Development at 18 Months: The Impact of Maternal Personality Disorder and Depression. J. Am. Acad. Child Adolesc. Psychiatry 2012, 51, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Giurgescu, C.; Zenk, S.N.; Templin, T.N.; Engeland, C.G.; Dancy, B.L.; Park, C.G.; Kavanaugh, K.; Dieber, W.; Misra, D.P. The Impact of Neighborhood Environment, Social Support, and Avoidance Coping on Depressive Symptoms of Pregnant African-American Women. Women’s Health Issues 2015, 25, 294–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984; ISBN 0-8261-4191-9. [Google Scholar]
- Folkman, S.; Moskowitz, J.T. Coping: Pitfalls and Promise. Annu. Rev. Psychol. 2004, 55, 745–774. [Google Scholar] [CrossRef]
- Kato, T. Frequently Used Coping Scales: A Meta-Analysis. Stress Health 2015, 31, 315–323. [Google Scholar] [CrossRef]
- Roth, S.; Cohen, L.J. Approach, avoidance, and coping with stress. Am. Psychol. 1986, 41, 813–819. [Google Scholar] [CrossRef]
- Carver, C.S.; Connor-Smith, J. Personality and Coping. Annu. Rev. Psychol. 2010, 61, 679–704. [Google Scholar] [CrossRef] [Green Version]
- Lazarus, R.S.; Folkman, S. Transactional theory and research on emotions and coping. Eur. J. Pers. 1987, 1, 141–169. [Google Scholar] [CrossRef]
- Arble, E.; Arnetz, B.B. A Model of First-responder Coping: An Approach/Avoidance Bifurcation. Stress Health 2017, 33, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Brooks, M.; Graham-Kevan, N.; Robinson, S.; Lowe, M. Supplemental Material for Trauma Characteristics and Posttraumatic Growth: The Mediating Role of Avoidance Coping, Intrusive Thoughts, and Social Support. Psychol. Trauma Theory Res. Pr. Policy 2019, 11, 232–238. [Google Scholar] [CrossRef] [Green Version]
- Bartone, P.T.; Homish, G.G. Influence of hardiness, avoidance coping, and combat exposure on depression in returning war veterans: A moderated-mediation study. J. Affect. Disord. 2020, 265, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Gauthier-Duchesne, A.; Hébert, M.; Daspe, M.-È. Culpabilité chez les enfants victimes d’agression sexuelle. Criminologie 2017, 50, 181–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aneja, J.; Chavan, B.S.; Huria, A.; Goel, P.; Kohli, N.; Chhabra, P. Perceived stress and its psychological correlates in pregnant women: An Indian study. Int. J. Cult. Ment. Health 2018, 11, 268–279. [Google Scholar] [CrossRef]
- Litz, B.T.; Orsillo, S.M.; Kaloupek, D.; Weathers, F. Emotional processing in posttraumatic stress disorder. J. Abnorm. Psychol. 2000, 109, 26–39. [Google Scholar] [CrossRef]
- Kashdan, T.B.; Breen, W.E.; Julian, T. Everyday strivings in war veterans with posttraumatic stress disorder: Suffering from a hyper-focus on avoidance and emotion regulation. Behav. Ther. 2010, 41, 350–363. [Google Scholar] [CrossRef] [Green Version]
- Barlow, D.H. Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. Am. Psychol. 2000, 55, 1247–1263. [Google Scholar] [CrossRef]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes, and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, E.; Sayal, K.; Townsend, E. Functional coping dynamics and experiential avoidance in a community sample with no self-injury vs. Non-suicidal self-injury only vs. those with both non-suicidal self-injury and suicidal behaviour. Int. J. Environ. Res. Public Health 2017, 14, 575. [Google Scholar] [CrossRef] [Green Version]
- Sandín, B.; Chorot, P. Cuestionario de afrontamiento del estrés (CAE): Desarrollo y validación preliminar. Rev. Psicopatol. Y Psicol. Clín. 2003, 8. [Google Scholar] [CrossRef]
- Quezada-Berumen, L.; Moral de la Rubia, J.; Ibarra-González, L.D.; González-Ramírez, M.T. Estudio de validación del Cuestionario de Afrontamiento del Estrés en personas trans de México. Rev. Psicopatol. Y Psicol. Clín. 2018, 23, 121. [Google Scholar] [CrossRef] [Green Version]
- Melendez, J.C.; Satorres, E.; Delhom, I. Personalidad y afrontamiento. ¿Qué rasgos predicen las estrategias adaptativas? Ann. Psicol. 2019, 36, 39–45. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Esteve, L.; Ascaso, C.; Ojuel, J.; Navarro, P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J. Affect. Disord. 2003, 75, 71–76. [Google Scholar] [CrossRef]
- Jairaj, C.; Fitzsimons, C.M.; McAuliffe, F.M.; O’Leary, N.; Joyce, N.; McCarthy, A.; Cassidy, E.; Donnelly, J.; Tully, E.; Imcha, M.; et al. A population survey of prevalence rates of antenatal depression in the Irish obstetric services using the Edinburgh Postnatal Depression Scale (EPDS). Arch. Womens Ment. Health 2019, 22, 349–355. [Google Scholar] [CrossRef]
- Loscalzo, Y.; Giannini, M.; Contena, B.; Gori, A.; Benvenuti, P. The Edinburgh Postnatal Depression Scale for Fathers: A contribution to the validation for an Italian sample. Gen. Hosp. Psychiatry 2015, 37, 251–256. [Google Scholar] [CrossRef]
- Wolke, D.; James-Roberts, I.S. Multi-Method Measurement of the Early Parent-Infant System with Easy and Difficult Newborns. Adv. Psychol. 1987, 46, 49–70. [Google Scholar]
- Meier, P.; Wolke, D.; Gutbrod, T.; Rust, L. The influence of infant irritability on maternal sensitivity in a sample of very premature infants. Infant Child Dev. 2003, 12, 159–166. [Google Scholar] [CrossRef]
- IBM Corp. IBM Corp IBM SPSS Statistics for Windows, Version 22.0; IBM Corp: Armonk, NY, USA, 2017. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis Second Edition A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017; ISBN 9781462534654. [Google Scholar]
- Lefkovics, E.; Rigó, J.; Kovács, I.; Talabér, J.; Szita, B.; Kecskeméti, A.; Szabó, L.; Somogyvári, Z.; Baji, I. Effect of maternal depression and anxiety on mother’s perception of child and the protective role of social support. J. Reprod. Infant Psychol. 2018, 36, 434–448. [Google Scholar] [CrossRef]
- Thomason, E.; Flynn, H.A.; Himle, J.A.; Volling, B.L. Are women’s parenting-specific beliefs associated with depressive symptoms in the perinatal period? Development of the rigidity of maternal beliefs scale. Depress. Anxiety 2015, 32, 141–148. [Google Scholar] [CrossRef] [Green Version]
- Kerstis, B.; Engström, G.; Edlund, B.; Aarts, C. Association between mothers’ and fathers’ depressive symptoms, sense of coherence and perception of their child’s temperament in early parenthood in Sweden. Scand. J. Public Health 2013, 41, 233–239. [Google Scholar] [CrossRef] [Green Version]
- Penengo, C.; Colli, C.; Garzitto, M.; Driul, L.; Cesco, M.; Balestrieri, M. Validation of the Italian version of the Revised Prenatal Coping Inventory (NuPCI) and its correlations with pregnancy-specific stress. BMC Pregnancy Childbirth 2020, 20, 466. [Google Scholar] [CrossRef]
- Catala, P.; Peñacoba, C.; Carmona, J.; Marin, D. Do maternal personality variables influence childbirth satisfaction? A longitudinal study in low-risk pregnancies. Women Health 2020, 60, 197–211. [Google Scholar] [CrossRef]
- Ozcan, H.; Ustundag, M.F.; Yilmaz, M.; Aydinoglu, U.; Ersoy, A.O.; Yapar Eyi, E.G. The Relationships between Prenatal Attachment, Basic Personality Traits, Styles of Coping with Stress, Depression, and Anxiety, and Marital Adjustment Among Women in the Third Trimester of Pregnancy. Eurasian J. Med. 2019, 51, 232–236. [Google Scholar] [CrossRef]
- Choi, K.W.; Sikkema, K.J.; Vythilingum, B.; Geerts, L.; Faure, S.C.; Watt, M.H.; Roos, A.; Stein, D.J. Maternal childhood trauma, postpartum depression, and infant outcomes: Avoidant affective processing as a potential mechanism. J. Affect. Disord. 2017, 211, 107–115. [Google Scholar] [CrossRef]
- Onat, G.; Karakoç, H. Three spirals: Breastfeeding problems, growth spurts, and postpartum depression. Perspect. Psychiatr. Care 2020. [Google Scholar] [CrossRef]
- Koutra, K.; Vassilaki, M.; Georgiou, V.; Koutis, A.; Bitsios, P.; Kogevinas, M.; Chatzi, L. Pregnancy, perinatal and postpartum complications as determinants of postpartum depression: The Rhea mother–child cohort in Crete, Greece. Epidemiol. Psychiatr. Sci. 2018, 27, 244–255. [Google Scholar] [CrossRef]
- Limas, E.A. Social Context of Breastfeeding: The Intersection between Attitudes and Postpartum Depression. Ph.D. Thesis, Indiana University, Bloomington, IN, USA, 2018. [Google Scholar]
- Bandura, A.; Pastorelli, C.; Barbaranelli, C.; Caprara, G.V. Self-efficacy pathways to childhood depression. J. Pers. Soc. Psychol. 1999, 76, 258–269. [Google Scholar] [CrossRef]
- Razurel, C.; Kaiser, B.; Antonietti, J.-P.; Epiney, M.; Sellenet, C. Relationship between perceived perinatal stress and depressive symptoms, anxiety, and parental self-efficacy in primiparous mothers and the role of social support. Women Health 2017, 57, 154–172. [Google Scholar] [CrossRef]
- Martini, J.; Petzoldt, J.; Einsle, F.; Beesdo-Baum, K.; Höfler, M.; Wittchen, H.-U. Risk factors and course patterns of anxiety and depressive disorders during pregnancy and after delivery: A prospective-longitudinal study. J. Affect. Disord. 2015, 175, 385–395. [Google Scholar] [CrossRef]
- Fathi, F.; Mohammad-Alizadeh-Charandabi, S.; Mirghafourvand, M. Maternal self-efficacy, postpartum depression, and their relationship with functional status in Iranian mothers. Women Health 2018, 58, 188–203. [Google Scholar] [CrossRef]
- Santos, H.P.; Kossakowski, J.J.; Schwartz, T.A.; Beeber, L.; Fried, E.I. Longitudinal network structure of depression symptoms and self-efficacy in low-income mothers. PLoS ONE 2018, 13, e0191675. [Google Scholar] [CrossRef] [Green Version]
- Bates, R.A.; Salsberry, P.J.; Justice, L.M.; Dynia, J.M.; Logan, J.A.R.; Gugiu, M.R.; Purtell, K.M. Relations of Maternal Depression and Parenting Self-Efficacy to the Self-Regulation of Infants in Low-Income Homes. J. Child Fam. Stud. 2020, 29, 2330–2341. [Google Scholar] [CrossRef]
- Lee, J.-S.; Koo, H.J. The relationship between adult attachment and depression in Korean mothers during the first 2years postpartum: A moderated mediation model of self-esteem and maternal efficacy. Pers. Individ. Dif. 2015, 79, 50–56. [Google Scholar] [CrossRef]
- Minamida, T.; Iseki, A.; Sakai, H.; Imura, M.; Okano, T.; Tanii, H. Do postpartum anxiety and breastfeeding self-efficacy and bonding at early postpartum predict postpartum depression and the breastfeeding method? Infant Ment. Health J. 2020, 41, 662–676. [Google Scholar] [CrossRef]
- Koury, A.J.; Dynia, J.; Dore, R.; Logan, J.A.R.; Purtell, K.M.; Joy, E.; Salsberry, P. Food Insecurity and Depression among Economically Disadvantaged Mothers: Does Maternal Efficacy Matter? Appl. Psychol. Health Well-Being 2020, 12, 432–448. [Google Scholar] [CrossRef]
- Haskell, A.M.; Britton, P.C.; Servatius, R.J. Toward an assessment of escape/avoidance coping in depression. Behav. Brain Res. 2020, 381, 112363. [Google Scholar] [CrossRef]
- Siepsiak, M.; Sobczak, A.M.; Bohaterewicz, B.; Cichocki, Ł.; Dragan, W.Ł. Prevalence of Misophonia and Correlates of Its Symptoms among Inpatients with Depression. Int. J. Environ. Res. Public Health 2020, 17, 5464. [Google Scholar] [CrossRef]
- Belanger, R.L. Risk and Resilience for Postpartum Depression in Mothers of Infants Who Required Neonatal-Intensive-Care-Unit Hospitalization. Ph.D. Thesis, University of Maryland, College Park, MD, USA, 2018. [Google Scholar]
- Lasheras, G.; Farré-Sender, B.; Porta, R.; Mestre-Bach, G. Risk factors for postpartum depression in mothers of newborns admitted to neonatal intensive care unit. J. Reprod. Infant Psychol. 2020, 1–15. [Google Scholar] [CrossRef]
- Gómez Penedo, J.M.; Coyne, A.E.; Constantino, M.J.; Krieger, T.; Hayes, A.M. Theory-specific patient change processes and mechanisms in different cognitive therapies for depression. J. Consult. Clin. Psychol. 2020, 88, 774–785. [Google Scholar] [CrossRef] [PubMed]
- Chou, W.-P.; Yen, C.-F.; Liu, T.-L. Predicting Effects of Psychological Inflexibility/Experiential Avoidance and Stress Coping Strategies for Internet Addiction, Significant Depression, and Suicidality in College Students: A Prospective Study. Int. J. Environ. Res. Public Health 2018, 15, 788. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Variable | Cronbach alpha | Mean (SD) | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.Avoidance | 0.72 | 9.15 (3.71) | 0.09 | 0.06 | 0.13 | −0.04 | −0.16 | 0.13 | 0.30 ** | 0.08 | −0.23 * |
| 2. PPD | 0.88 | 6.08 (4.86) | −0.13 | 0.22 * | −0.10 | −0.25 ** | 0.30 ** | 0.51 ** | 0.30 ** | −0.43 ** | |
| 3. Alert-Interest | 0.69 | 32.18 (4.64) | 0.09 | 0.08 | 0.06 | 0.02 | −0.12 | −0.03 | 0.12 | ||
| 4. Unstable-Irregular | 0.78 | 27.84 (11.92) | −0.74 ** | -0.13 | 0.69 ** | 0.55 ** | 0.09 | −0.46 ** | |||
| 5. Easy Temperament | 0.80 | 14.85 (2.97) | 0.07 | −0.52 ** | −0.39 ** | −0.02 | 0.48 ** | ||||
| 6. ADL | 0.79 | 16.01 (4.63) | −0.05 | −0.27 ** | 0.08 | 0.40 ** | |||||
| 7. IDL | 0.80 | 7.02 (5.38) | 0.46 ** | 0.29 ** | −0.37 ** | ||||||
| 8. LCC | 0.78 | 14.73 (9.66) | 0.25 ** | −0.67 ** | |||||||
| 9. LCL | 0.68 | 7.43 (6.22) | −0.21 * | ||||||||
| 10.GLS | 0.81 | 15.03 (3.05) |
| Variable | R2 | F | p | Beta | t | p | 95% CI |
|---|---|---|---|---|---|---|---|
| DV = A | 0.08 | 2.29 | 0.083 | ||||
| PPD | −0.17 | −1.80 | 0.074 | −0.36, 0.02 | |||
| Avoidance | 0.26 | 1.80 | 0.063 | −0.01, 0.511 | |||
| Interaction | −0.01 | −0.40 | 0.689 | −0.07, 0.05 | |||
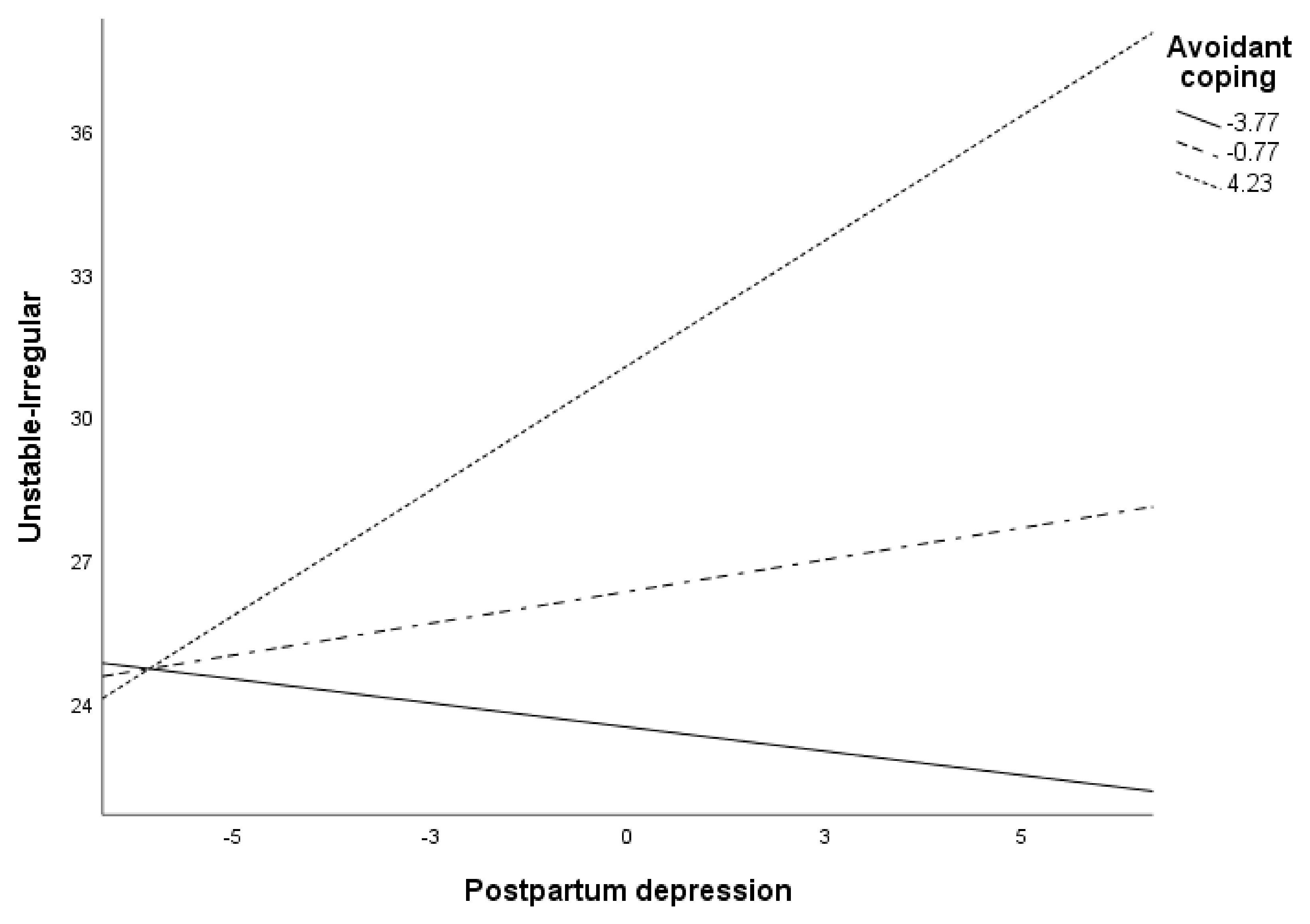
| DV = UI | 0.15 | 4.84 | 0.003 | ||||
| PPD | 0.39 | 1.73 | 0.086 | −0.06, 0.83 | |||
| Avoidance | 0.95 | 3.03 | 0.003 | 0.33, 1.56 | |||
| Interaction | 0.16 | 2.19 | 0.031 | 0.01, 0.30 | |||
| DV = ET | 0.14 | 3.72 | 0.015 | ||||
| PPD | −0.06 | −0.92 | 0.358 | −0.18, 0.07 | |||
| Avoidance | −0.11 | −1.31 | 0.191 | −0.28, 0.06 | |||
| Interaction | −0.06 | −3.10 | 0.002 | −0.09, −0.02 | |||
| DV = ADL | 0.10 | 3.17 | 0.028 | ||||
| PPD | −0.19 | −2.04 | 0.044 | −0.37, −0.01 | |||
| Avoidance | −0.18 | −1.40 | 0.164 | −0.44, 0.08 | |||
| Interaction | 0.04 | 1.23 | 0.221 | −0.02, 0.09 | |||
| DV = IDL | 0.16 | 5.14 | 0.002 | ||||
| PPD | 0.32 | 2.91 | 0.004 | 0.10, 0.54 | |||
| Avoidance | 0.31 | 2.06 | 0.041 | 0.01, 0.60 | |||
| Interaction | 0.07 | 1.90 | 0.060 | −0.01, 0.14 | |||
| DV = LCL | 0.08 | 2.40 | 0.073 | ||||
| PPD | 0.39 | 2.66 | 0.009 | 0.10, 0.67 | |||
| Avoidance | −0.06 | −0.31 | 0.760 | −0.46, 0.33 | |||
| Interaction | −0.01 | .20 | 0.845 | −0.11, 0.09 | |||
| DV = LCC | 0.40 | 18.71 | <0.001 | ||||
| PPD | 1.01 | 6.48 | <0.001 | 0.71, 1.32 | |||
| Avoidance | 0.81 | 3.66 | <0.001 | 0.37, 1.24 | |||
| Interaction | 0.11 | 2.25 | 0.027 | 0.01, 0.21 | |||
| DV = GLS | 0.28 | 8.67 | <0.001 | ||||
| PPD | −0.26 | −4.74 | <0.001 | −0.37, −0.15 | |||
| Avoidance | −0.08 | −0.93 | 0.355 | −0.24, 0.09 | |||
| Interaction | −0.05 | −2.73 | 0.007 | −0.09, −0.01 |
| Variable | Avoidance | Beta (PPD) | t | p | 95% CI |
|---|---|---|---|---|---|
| UI | |||||
| −3.77 | −0.20 | −0.63 | 0.528 | −0.83, 0.43 | |
| −0.77 | 0.27 | 1.21 | 0.229 | −0.17, 0.70 | |
| 4.22 | 1.05 | 2.59 | 0.011 | 0.24, 1.85 | |
| ET | |||||
| −3.77 | 0.16 | 1.86 | 0.067 | −0.01, 0.33 | |
| −0.77 | −0.01 | −0.23 | 0.819 | −0.14, 0.11 | |
| 4.22 | −0.30 | −2.75 | 0.007 | −0.52, −0.08 | |
| LCC | |||||
| −3.77 | 0.59 | 2.64 | 0.009 | 0.15, 1.03 | |
| −0.77 | 0.93 | 6.00 | <0.001 | 0.62, 1.23 | |
| 4.22 | 1.49 | 5.25 | <0.001 | 0.93, 2.05 | |
| GLS | |||||
| −3.71 | −0.08 | −0.96 | 0.338 | −0.23, 0.08 | |
| −0.71 | −0.23 | −4.18 | <0.001 | −0.33, 0.12 | |
| 3.28 | −0.43 | −4.76 | <0.001 | −0.61, −0.25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peñacoba Puente, C.; Suso-Ribera, C.; Blanco Rico, S.; Marín, D.; San Román Montero, J.; Catalá, P. Is the Association between Postpartum Depression and Early Maternal–Infant Relationships Contextually Determined by Avoidant Coping in the Mother? Int. J. Environ. Res. Public Health 2021, 18, 562. https://doi.org/10.3390/ijerph18020562
Peñacoba Puente C, Suso-Ribera C, Blanco Rico S, Marín D, San Román Montero J, Catalá P. Is the Association between Postpartum Depression and Early Maternal–Infant Relationships Contextually Determined by Avoidant Coping in the Mother? International Journal of Environmental Research and Public Health. 2021; 18(2):562. https://doi.org/10.3390/ijerph18020562
Chicago/Turabian StylePeñacoba Puente, Cecilia, Carlos Suso-Ribera, Sheila Blanco Rico, Dolores Marín, Jesús San Román Montero, and Patricia Catalá. 2021. "Is the Association between Postpartum Depression and Early Maternal–Infant Relationships Contextually Determined by Avoidant Coping in the Mother?" International Journal of Environmental Research and Public Health 18, no. 2: 562. https://doi.org/10.3390/ijerph18020562
APA StylePeñacoba Puente, C., Suso-Ribera, C., Blanco Rico, S., Marín, D., San Román Montero, J., & Catalá, P. (2021). Is the Association between Postpartum Depression and Early Maternal–Infant Relationships Contextually Determined by Avoidant Coping in the Mother? International Journal of Environmental Research and Public Health, 18(2), 562. https://doi.org/10.3390/ijerph18020562






