Association of Greenness with Blood Pressure among Individuals with Type 2 Diabetes across Rural to Urban Community Types in Pennsylvania, USA
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Electronic Health Record Measures
2.2.1. Blood Pressure
2.2.2. Individual Covariates
2.3. Environmental Measures
2.3.1. Proximate Greenness
2.3.2. Percent Forest
2.3.3. Community Socioeconomic Deprivation
2.4. Statistical Analyses
3. Results
3.1. Characteristics of Study Individuals and Communities
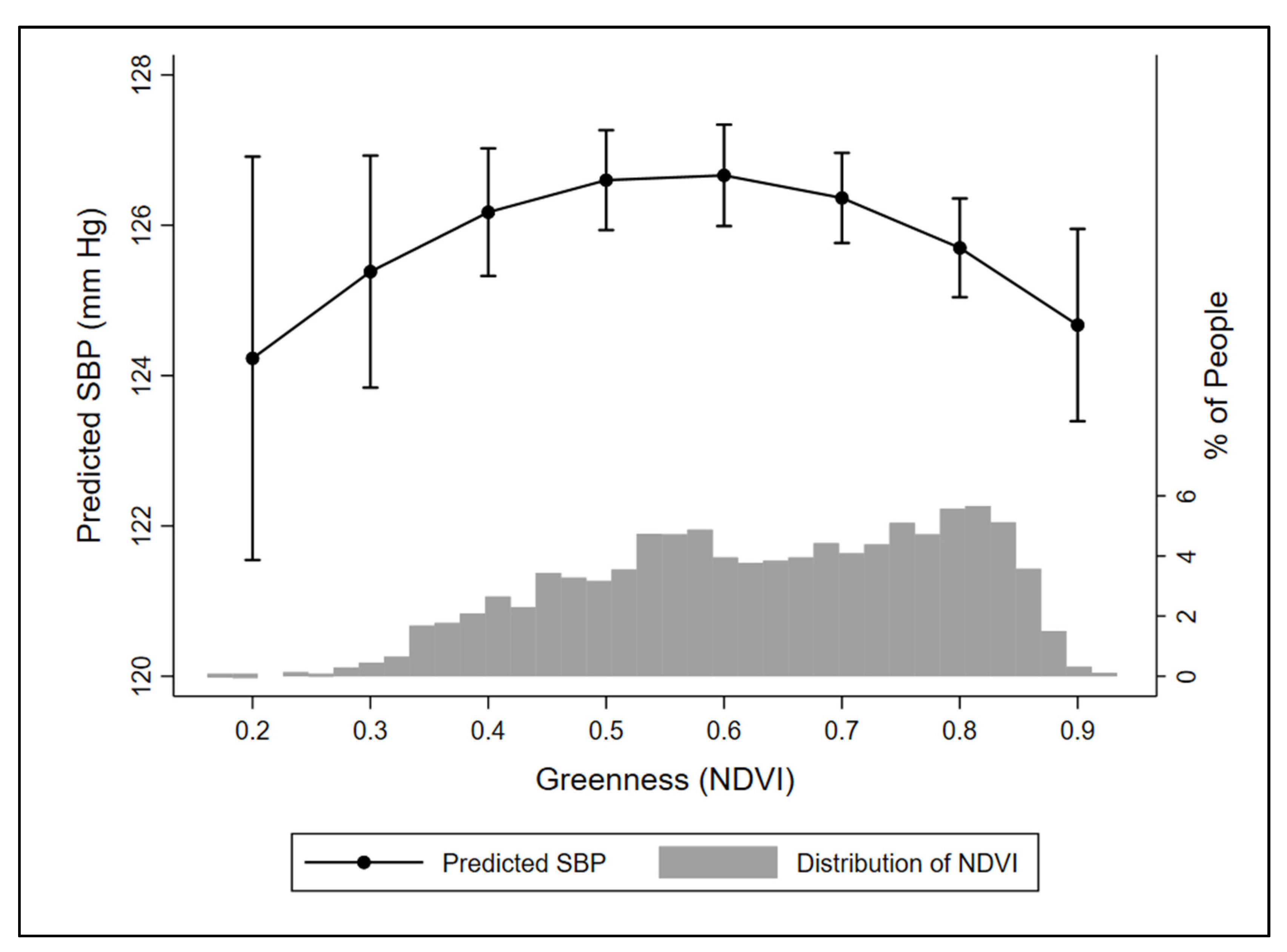
3.2. Associations of Greenness and Blood Pressure
3.3. Effect Modification by Percent Forest on Associations of Greenness with Blood Pressure
3.4. Disentangling Potential Confounding of Greenness and Blood Pressure Associations by Season
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hartig, T.; Mitchell, R.; de Vries, S.; Frumkin, H. Nature and health. Annu. Rev. Public Health 2014, 35, 207–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Markevych, I.; Schoierer, J.; Hartig, T.; Chudnovsky, A.; Hystad, P.; Dzhambov, A.M.; de Vries, S.; Triguero-Mas, M.; Brauer, M.; Nieuwenhuijsen, M.J.; et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ. Res. 2017, 158, 301–317. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S. Aesthetic and Affective Response to Natural Environment. In Behavior and the Natural Environment; Altman, I., Wohlwill, J.F., Eds.; Springer: Boston, MA, USA, 1983; pp. 85–125. [Google Scholar] [CrossRef]
- Fong, K.C.; Hart, J.E.; James, P. A Review of Epidemiologic Studies on Greenness and Health: Updated Literature through 2017. Curr. Environ. Health Rep. 2018, 5, 77–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le-Scherban, F.; Ballester, L.; Castro, J.C.; Cohen, S.; Melly, S.; Moore, K.; Buehler, J.W. Identifying neighborhood characteristics associated with diabetes and hypertension control in an urban African-American population using geo-linked electronic health records. Prev. Med. Rep. 2019, 15, 100953. [Google Scholar] [CrossRef] [PubMed]
- Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. 2018, 166, 628–637. [Google Scholar] [CrossRef]
- Wen, Y.; Yan, Q.; Pan, Y.; Gu, X.; Liu, Y. Medical empirical research on forest bathing (Shinrin-yoku): A systematic review. Environ. Health Prev. Med. 2019, 24, 70. [Google Scholar] [CrossRef] [Green Version]
- Lastra, G.; Syed, S.; Kurukulasuriya, L.R.; Manrique, C.; Sowers, J.R. Type 2 Diabetes Mellitus and Hypertension: An Update. Endocrinol. Metab. Clin. 2014, 43, 103–122. [Google Scholar] [CrossRef] [Green Version]
- De Boer, I.H.; Bangalore, S.; Benetos, A.; Davis, A.M.; Michos, E.D.; Muntner, P.; Rossing, P.; Zoungas, S.; Bakris, G. Diabetes and Hypertension: A Position Statement by the American Diabetes Association. Diabetes Care 2017, 40, 1273–1284. [Google Scholar] [CrossRef] [Green Version]
- Hu, G.; Jousilahti, P.; Tuomilehto, J. Joint effects of history of hypertension at baseline and type 2 diabetes at baseline and during follow-up on the risk of coronary heart disease. Eur. Heart J. 2007, 28, 3059–3066. [Google Scholar] [CrossRef] [Green Version]
- Shay, C.M.; Gooding, H.S.; Murillo, R.; Foraker, R. Understanding and Improving Cardiovascular Health: An Update on the American Heart Association’s Concept of Cardiovascular Health. Prog. Cardiovasc. Dis. 2015, 58, 41–49. [Google Scholar] [CrossRef]
- Wheeler, B.W.; Lovell, R.; Higgins, S.L.; White, M.P.; Alcock, I.; Osborne, N.J.; Husk, K.; Sabel, C.E.; Depledge, M.H. Beyond greenspace: An ecological study of population general health and indicators of natural environment type and quality. Int. J. Health Geogr. 2015, 14, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, L.; Hochuli, D.F. Defining greenspace: Multiple uses across multiple disciplines. Landsc. Urban Plan. 2017, 158, 25–38. [Google Scholar] [CrossRef] [Green Version]
- White, M.P.; Pahl, S.; Ashbullby, K.; Herbert, S.; Depledge, M.H. Feelings of restoration from recent nature visits. J. Environ. Psychol. 2013, 35, 40–51. [Google Scholar] [CrossRef]
- Bach Pagès, A.; Peñuelas, J.; Clarà, J.; Llusià, J.; Campillo i López, F.; Maneja, R. How Should Forests Be Characterized in Regard to Human Health? Evidence from Existing Literature. Int. J. Environ. Res. Public Health 2020, 17, 1027. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ideno, Y.; Hayashi, K.; Abe, Y.; Ueda, K.; Iso, H.; Noda, M.; Lee, J.S.; Suzuki, S. Blood pressure-lowering effect of Shinrin-yoku (Forest bathing): A systematic review and meta-analysis. BMC Complement. Altern. Med. 2017, 17, 409. [Google Scholar] [CrossRef] [PubMed]
- Akpinar, A.; Barbosa-Leiker, C.; Brooks, K.R. Does green space matter? Exploring relationships between green space type and health indicators. Urban For. Urban Green. 2016, 20, 407–418. [Google Scholar] [CrossRef]
- Hirsch, A.G.; Carson, A.P.; Lee, N.L.; McAlexander, T.; Mercado, C.; Siegel, K.; Black, N.C.; Elbel, B.; Long, D.L.; Lopez, P.; et al. The Diabetes Location, Environmental Attributes, and Disparities Network: Protocol for Nested Case Control and Cohort Studies, Rationale, and Baseline Characteristics. JMIR Res. Protoc. 2020, 9, e21377. [Google Scholar] [CrossRef]
- Casey, J.A.; Savitz, D.A.; Rasmussen, S.G.; Ogburn, E.L.; Pollak, J.; Mercer, D.G.; Schwartz, B.S. Unconventional Natural Gas Development and Birth Outcomes in Pennsylvania, USA. Epidemiology 2016, 27, 163–172. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, B.S.; Pollak, J.S.; Poulsen, M.N.; Bandeen-Roche, K.; Moon, K.A.; DeWalle, J.; Siegel, K.R.; Mercado, C.I.; Imperatore, G.; Hirsch, A.G. Association of community types and features in a case-control analysis of new onset type 2 diabetes across a diverse geography in Pennsylvania. BMJ Open 2021, in press. [Google Scholar]
- Casey, J.A.; Pollak, J.; Glymour, M.M.; Mayeda, E.R.; Hirsch, A.G.; Schwartz, B.S. Measures of SES for Electronic Health Record-based Research. Am. J. Prev. Med. 2017. [Google Scholar] [CrossRef]
- Schwartz, B.S.; Stewart, W.F.; Godby, S.; Pollak, J.; Dewalle, J.; Larson, S.; Mercer, D.G.; Glass, T.A. Body mass index and the built and social environments in children and adolescents using electronic health records. Am. J. Prev. Med. 2011, 41, e17–e28. [Google Scholar] [CrossRef]
- Poulsen, M.N.; Glass, T.A.; Pollak, J.; Bandeen-Roche, K.; Hirsch, A.G.; Bailey-Davis, L.; Schwartz, B.S. Associations of multidimensional socioeconomic and built environment factors with body mass index trajectories among youth in geographically heterogeneous communities. Prev. Med. Rep. 2019, 15, 100939. [Google Scholar] [CrossRef] [PubMed]
- Yeager, R.; Riggs, D.W.; DeJarnett, N.; Tollerud, D.J.; Wilson, J.; Conklin, D.J.; O’Toole, T.E.; McCracken, J.; Lorkiewicz, P.; Xie, Z.; et al. Association Between Residential Greenness and Cardiovascular Disease Risk. J. Am. Heart Assoc. 2018, 7, e009117. [Google Scholar] [CrossRef] [PubMed]
- Didan, K. MYD13Q1 MODIS/Aqua Vegetation Indices 16-Day L3 Global 250m SIN Grid V006 [Data set]. NASA EOSDIS Land Processes DAAC. 2015. Available online: https://doi.org/10.5067/MODIS/MYD13Q1.006 (accessed on 11 January 2021).
- Manson, S.; Schroeder, J.; Van Riper, D.; Ruggles, S. IPUMS National Historical Geographic Information System, 14th ed.; IPUMS: Minneapolis, MN, USA, 2019. [Google Scholar] [CrossRef]
- Nau, C.; Schwartz, B.S.; Bandeen-Roche, K.; Liu, A.; Pollak, J.; Hirsch, A.; Bailey-Davis, L.; Glass, T.A. Community socioeconomic deprivation and obesity trajectories in children using electronic health records. Obesity 2015, 23, 207–212. [Google Scholar] [CrossRef] [Green Version]
- Yang, B.Y.; Markevych, I.; Bloom, M.S.; Heinrich, J.; Guo, Y.; Morawska, L.; Dharmage, S.C.; Knibbs, L.D.; Jalaludin, B.; Jalava, P.; et al. Community greenness, blood pressure, and hypertension in urban dwellers: The 33 Communities Chinese Health Study. Environ. Int. 2019, 126, 727–734. [Google Scholar] [CrossRef]
- Westreich, D.; Cole, S.R. Invited commentary: Positivity in practice. Am. J. Epidemiol. 2010, 171, 674–677; discussion 678–681. [Google Scholar] [CrossRef] [Green Version]
- Modesti, P.A.; Morabito, M.; Massetti, L.; Rapi, S.; Orlandini, S.; Mancia, G.; Gensini, G.F.; Parati, G. Seasonal blood pressure changes: An independent relationship with temperature and daylight hours. Hypertension 2013, 61, 908–914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, M. Trends in Diabetes Management Among US Adults: 1999–2016. J. Gen. Intern. Med. 2020, 35, 1427–1434. [Google Scholar] [CrossRef]
- Hardy, S.T.; Loehr, L.R.; Butler, K.R.; Chakladar, S.; Chang, P.P.; Folsom, A.R.; Heiss, G.; MacLehose, R.F.; Matsushita, K.; Avery, C.L. Reducing the Blood Pressure-Related Burden of Cardiovascular Disease: Impact of Achievable Improvements in Blood Pressure Prevention and Control. J. Am. Heart Assoc. 2015, 4, e002276. [Google Scholar] [CrossRef] [Green Version]
- Muntner, P.; Einhorn, P.T.; Cushman, W.C.; Whelton, P.K.; Bello, N.A.; Drawz, P.E.; Green, B.B.; Jones, D.W.; Juraschek, S.P.; Margolis, K.L.; et al. Blood Pressure Assessment in Adults in Clinical Practice and Clinic-Based Research. J. Am. Coll. Cardiol. 2019, 73, 317–335. [Google Scholar] [CrossRef]
- Choi, Y.J.; Kim, S.H.; Kang, S.H.; Kim, S.Y.; Kim, O.J.; Yoon, C.H.; Lee, H.Y.; Youn, T.J.; Chae, I.H.; Kim, C.H. Short-term effects of air pollution on blood pressure. Sci. Rep. 2019, 9, 20298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klompmaker, J.O.; Janssen, N.A.H.; Bloemsma, L.D.; Gehring, U.; Wijga, A.H.; van den Brink, C.; Lebret, E.; Brunekreef, B.; Hoek, G. Associations of Combined Exposures to Surrounding Green, Air Pollution, and Road Traffic Noise with Cardiometabolic Diseases. Environ. Health Perspect. 2019, 127, 87003. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Characteristic | Total | Township Residents | Borough Residents | City Residents | p-Value |
|---|---|---|---|---|---|
| Number of individuals | 9593 | 5853 | 2786 | 954 | n/a |
| Number of communities | 724 | 424 | 200 | 100 | n/a |
| Sex, female, n (%) | 4757 (49.6) | 2772 (47.4) | 1450 (52.1) | 535 (56.1) | <0.001 |
| Age, years, mean (SD) | 56.9 (14.0) | 57.7 (13.5) | 56.0 (14.5) | 54.6 (14.9) | <0.001 |
| Race, white, n (%) | 9346 (97.4) | 5723 (97.8) | 2729 (98.0) | 894 (93.7) | <0.001 |
| Non-Hispanic ethnicity, n (%) | 9385 (97.8) | 5750 (98.2) | 2737 (98.2) | 898 (94.1) | <0.001 |
| Medical Assistance, ever, n (%) | 2365 (13.2) | 1090 (10.0) | 868 (16.5) | 407 (23.2) | <0.001 |
| Smoking status, n (%) | <0.001 | ||||
| Current | 1666 (17.4) | 867 (14.8) | 572 (20.5) | 227 (23.8) | |
| Former | 3635 (37.9) | 2205 (37.7) | 1068 (38.3) | 362 (38.0) | |
| Never | 4239 (44.2) | 2738 (46.8) | 1137 (40.8) | 364 (38.2) | |
| Unknown | 53 (0.6) | 43 (0.7) | 9 (0.3) | 1 (0.1) | |
| Body mass index (kg/m2), 1 mean (SD) | 35.3 (7.9) | 35.0 (7.7) | 35.6 (8.2) | 35.9 (8.3) | <0.001 |
| SBP (mmHg), mean (SD) | 126.3 (14.1) | 126.5 (14.2) | 126.3 (14.0) | 125.0 (14.1) | 0.01 |
| DBP (mmHg), mean (SD) | 74.9 (9.4) | 75.0 (9.4) | 74.9 (9.3) | 74.4 (9.8) | 0.24 |
| Blood pressure category, 2 n (%) | 0.26 | ||||
| Normal | 2414 (25.2) | 1458 (24.9) | 692 (24.8) | 264 (27.7) | |
| Elevated | 2260 (23.6) | 1372 (23.4) | 662 (23.8) | 226 (23.7) | |
| Hypertension stage 1 | 3152 (32.9) | 1916 (32.7) | 921 (33.1) | 315 (33.0) | |
| Hypertension stage 2 | 1767 (18.4) | 1107 (18.9) | 511 (18.3) | 149 (15.6) | |
| Season of blood pressure measurement, n (%) | |||||
| Winter (December–February) | 2250 (23.5) | 1401 (23.9) | 646 (23.2) | 203 (21.3) | 0.18 |
| Non-winter (March–November) | 7343 (76.6) | 4452 (76.1) | 2140 (76.8) | 751 (78.7) | |
| Current blood pressure medication usage, n (%) | 7009 (73.1) | 4287 (73.2) | 2060 (73.9) | 662 (69.4) | 0.02 |
| Primary hypertension, n (%) | 7000 (73.0) | 4316 (73.7) | 2027 (72.8) | 657 (68.9) | 0.01 |
| Duration of hypertension to blood pressure measurement, 3 years, mean (SD) | 7.2 (4.5) | 7.4 (4.5) | 7.0 (4.5) | 6.6 (4.5) | <0.001 |
| NDVI, mean (SD) | 0.55 (0.17) | 0.59 (0.16) | 0.50 (0.15) | 0.42 (0.14) | <0.001 |
| Percent forest, mean (SD) | 29.9 (25.3) | 38.8 (25.5) | 18.6 (18.4) | 8.2 (11.9) | <0.001 |
| CSD, SD units, mean (SD) | 0.3 (2.7) | −0.6 (2.4) | 1.1 (2.5) | 3.3 (2.3) | <0.001 |
| Townships Beta (95% CI) | Boroughs Beta (95% CI) | City Census Tracts Beta (95% CI) | |
|---|---|---|---|
| Systolic blood pressure | |||
| NDVI, 75th versus 25th quartile | −0.87 (−1.43, −0.30) | −0.76 (−1.64, 0.12) | −0.17 (−1.88, 1.53) |
| Primary hypertension diagnosis | 6.21 (5.28, 7.14) | 7.21 (5.87, 8.56) | 4.76 (2.51, 7.01) |
| Current blood pressure medication | −0.76 (−1.75, 0.23) | −1.38 (−2.80, 0.04) | −0.95 (−3.57, 1.67) |
| Diastolic blood pressure | |||
| NDVI, 75th versus 25th quartile | −0.41 (−0.78, −0.05) | −0.32 (−0.92, 0.28) | 0.02 (−1.14, 1.17) |
| Primary hypertension diagnosis | 3.82 (3.21, 4.43) | 4.17 (3.33, 5.02) | 3.14 (1.57, 4.70) |
| Current blood pressure medication | −1.15 (−1.79, −0.51) | −1.19 (−2.11, −0.27) | −1.18 (−2.84, 0.49) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poulsen, M.N.; Schwartz, B.S.; Nordberg, C.; DeWalle, J.; Pollak, J.; Imperatore, G.; Mercado, C.I.; Siegel, K.R.; Hirsch, A.G. Association of Greenness with Blood Pressure among Individuals with Type 2 Diabetes across Rural to Urban Community Types in Pennsylvania, USA. Int. J. Environ. Res. Public Health 2021, 18, 614. https://doi.org/10.3390/ijerph18020614
Poulsen MN, Schwartz BS, Nordberg C, DeWalle J, Pollak J, Imperatore G, Mercado CI, Siegel KR, Hirsch AG. Association of Greenness with Blood Pressure among Individuals with Type 2 Diabetes across Rural to Urban Community Types in Pennsylvania, USA. International Journal of Environmental Research and Public Health. 2021; 18(2):614. https://doi.org/10.3390/ijerph18020614
Chicago/Turabian StylePoulsen, Melissa N., Brian S. Schwartz, Cara Nordberg, Joseph DeWalle, Jonathan Pollak, Giuseppina Imperatore, Carla I. Mercado, Karen R. Siegel, and Annemarie G. Hirsch. 2021. "Association of Greenness with Blood Pressure among Individuals with Type 2 Diabetes across Rural to Urban Community Types in Pennsylvania, USA" International Journal of Environmental Research and Public Health 18, no. 2: 614. https://doi.org/10.3390/ijerph18020614





