Pilot Study to Develop and Test Palliative Care Quality Indicators for Nursing Homes
Abstract
:1. Background
2. Methods
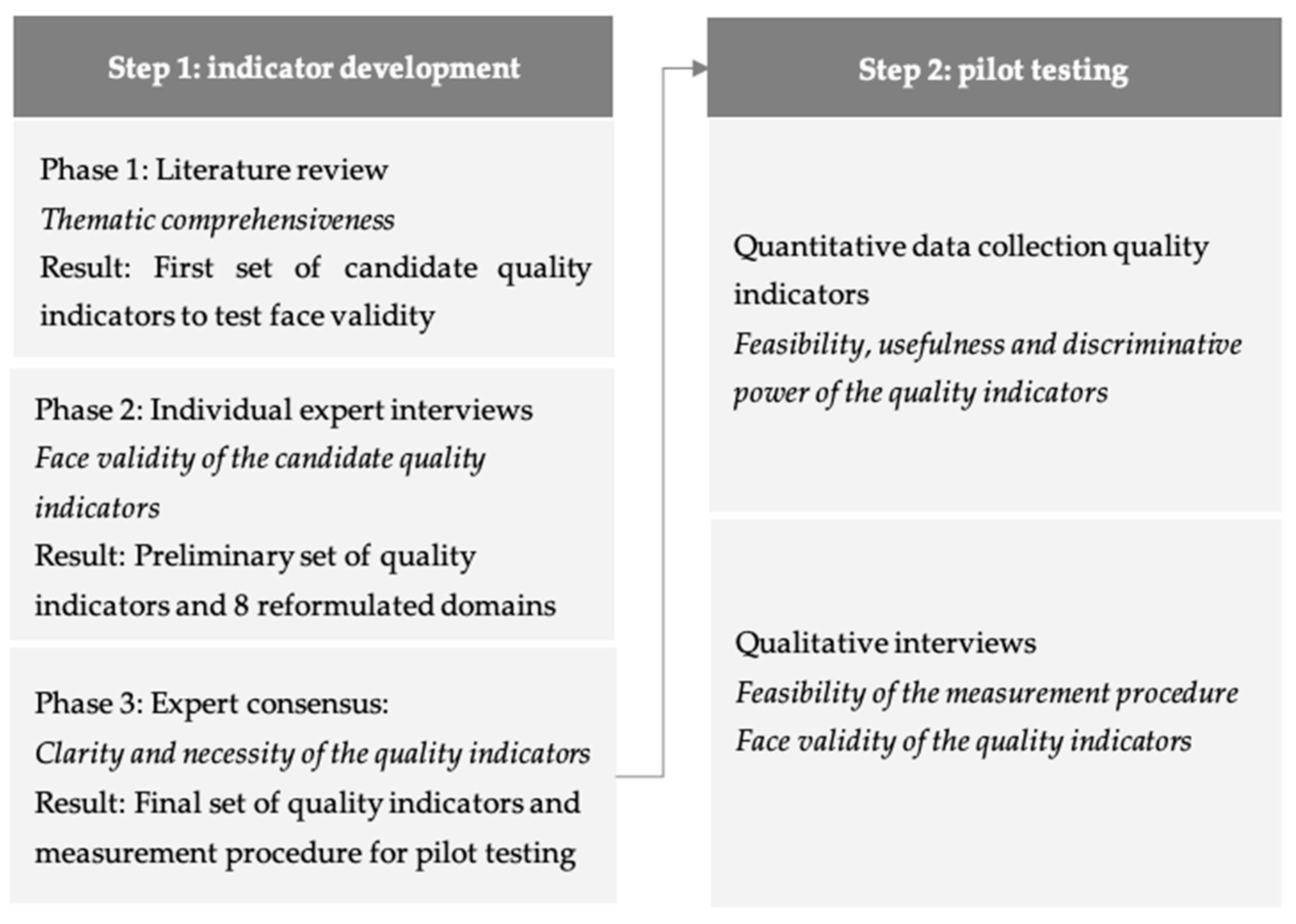
2.1. Design
2.2. Step 1: Indicator and Questionnaire Development
2.2.1. Phase 1 and 2: Literature Study and Expert Interviews
2.2.2. Phase 3: Expert Consensus
2.2.3. Questionnaires to Measure the Quality Indicators
2.3. Step 2: Pilot Testing
2.3.1. Design
2.3.2. Setting and Participants
- lived for a minimum of one month in the facility;
- lived for a minimum of one month in the facility; and,
- passed away four weeks to six months earlier in the nursing home.
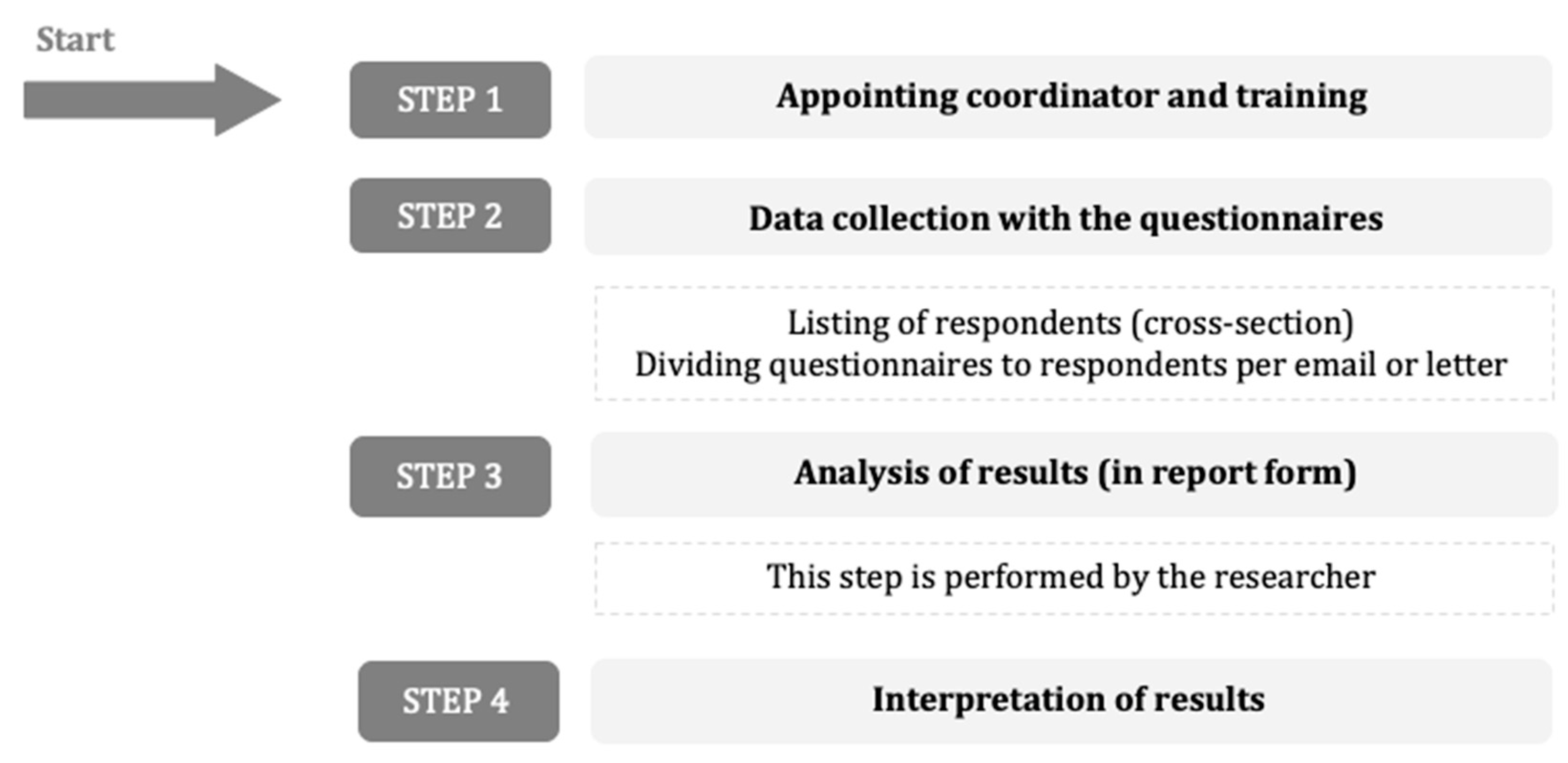
2.3.3. Measurement Procedure
2.3.4. Feedback and Evaluation
2.3.5. Analyses
2.4. Ethical and Language Issues
3. Results
3.1. Step 1: Indicator Development
3.1.1. Phase 1 and 2: Literature Study and Expert Interviews
3.1.2. Phase 3: Expert Consensus
3.2. Step 2: Pilot Test
3.2.1. Responder Characteristics
3.2.2. Psychometric Analyses: Feasibility and Discriminative Power
3.2.3. Qualitative Analyses; Feasibility, Usefulness and Face Validity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Etkind, S.N.; Bone, A.E.; Gomes, B.; Lovell, N.; Evans, C.J.; Higginson, I.J.; Murtagh, F.E.M. How many people will need palliative care in 2040? Past trends, future projections and implications for services. BMC Med. 2017, 15, 102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bone, A.E.; Gomes, B.; Etkind, S.N.; Verne, J.; Murtagh, F.E.M.; Evans, C.J.; Higginson, I.J. What is the impact of population ageing on the future provision of end-of-life care? Population-Based projections of place of death. Palliat. Med. 2018, 32, 329–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kojima, G. Prevalence of Frailty in Nursing Homes: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2015, 16, 940–945. [Google Scholar] [CrossRef] [PubMed]
- Hoben, M.; Chamberlain, S.A.; Gruneir, A.; Knopp-Sihota, J.A.; Sutherland, J.M.; Poss, J.W.; Doupe, M.B.; Bergsrom, V.; Norton, P.G.; Schalm, C.; et al. Nursing Home Length of Stay in 3 Canadian Health Regions: Temporal Trends, Jurisdictional Differences, and Associated Factors. J. Am. Med. Dir. Assoc. 2019, 20, 1121–1128. [Google Scholar] [CrossRef] [PubMed]
- Centeno, C.; Lynch, T.; Donea, O.; Rocafort, J.; Clark, D. EAPC Atlas of Palliative Care in Europe 2013—Full Edition; EAPC Press: Charleroi, Belgium, 2013. [Google Scholar]
- Organisation, W.H. Definition of Palliative Care. Available online: http://www.who.int/cancer/palliative/definition/en/ (accessed on 9 November 2020).
- Ten Koppel, M.; Onwuteaka-Philipsen, B.D.; Van den Block, L.; Deliens, L.; Gambassi, G.; Heymans, M.W.; Kylanen, M.; Pasman, H.R.W.; Payne, S.; Smets, T.; et al. Palliative care provision in long-term care facilities differs across Europe: Results of a cross-sectional study in six European countries (PACE). Palliat. Med. 2019, 33, 1176–1188. [Google Scholar] [CrossRef] [PubMed]
- Honinx, E.; van Dop, N.; Smets, T.; Deliens, L.; Van Den Noortgate, N.; Froggatt, K.; Gambassi, G.; Kylanen, M.; Onwuteaka-Philipsen, B.; Van den Block, L.; et al. Dying in long-term care facilities in Europe: The PACE epidemiological study of deceased residents in six countries. BMC Public Health 2019, 19, 1199. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.-R.; Wang, Y.; Lou, Y.; Li, Y.; Zhang, X.-G. The role of quality control circles in sustained improvement of medical quality. Springerplus 2013, 2, 141. [Google Scholar] [CrossRef] [Green Version]
- Grol, R.; Wensing, M. What drives change? Barriers to and incentives for achieving evidence-based practice. Med. J. Aust. 2004, 180, S57–S60. [Google Scholar] [CrossRef]
- Peters, M.A.J.; Harmsen, M.; Laurant, M.G.H.; Wensing, M. Room for Improvement? Barriers to and Facilitators for Improvement of Patient Care; Centre for Quality of Care Research (WOK): Nijmegen, The Netherlands, 2002.
- Grol, R.P.; Bosch, M.C.; Hulscher, M.E.; Eccles, M.P.; Wensing, M. Planning and studying improvement in patient care: The use of theoretical perspectives. Milbank Q. 2007, 85, 93–138. [Google Scholar] [CrossRef] [Green Version]
- Grol, R.; Wensing, M. Implementatie: Effectieve Verbetering van de Patiëntenzorg; Reed Business: Amsterdam, The Netherlands, 2011. [Google Scholar]
- Ostgathe, C.; Voltz, R. Quality indicators in end-of-life care. Curr. Opin. Support. Palliat. Care 2010, 4, 170–173. [Google Scholar] [CrossRef]
- Teno, J.M.; Coppola, K.M. For every numerator, you need a denominator: A simple statement but key to measuring the quality of care of the “dying”. J. Pain Symptom Manag. 1999, 17, 109–113. [Google Scholar] [CrossRef]
- Cohen, J.; Leemans, K. How can you prove that you are delivering good care? Monitoring the quality of palliative care using quality indicators. Eur. J. Palliat. Care 2014, 21, 228–231. [Google Scholar]
- Eagar, K.; Watters, P.; Currow, D.C.; Aoun, S.M.; Yates, P. The Australian Palliative Care Outcomes Collaboration (PCOC)—Measuring the quality and outcomes of palliative care on a routine basis. Aust. Health Rev. 2009, 34, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Canadian Government D of H. Canadian Strategy on Palliative and End-Of-Life Care. Available online: http://www.hc-sc.gc.ca/hcs-sss/palliat/support-soutien/strateg-eng.php (accessed on 2 September 2014).
- New Zealand Government M of H. The New Zealand Palliative Care Strategy. Available online: http://www.health.govt.nz/publication/new-zealand-palliative-care-strategy (accessed on 2 September 2014).
- Department of Health. End of life Care Strategy: Quality Markers and Measures for End of Life Care; Crown: London, UK, 2009. Available online: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_101684.pdf (accessed on 9 November 2020).
- Lundstrom, S.; Axelsson, B.; Heedman, P.A.; Fransson, G.; Furst, C.J. Developing a national quality register in end-of-life care: The Swedish experience. Palliat. Med. 2012, 26, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Welfare and Sports. Plan van Aanpak Palliatieve Zorg 2008–2010; Ministry of Health, Welfare and Sports: The Hague, The Netherlands, 2008. Available online: http://www.palliatief.nl/Portals/31/Planvanaanpak2008-2010/planvanaanpakpalliatievezorg2008-2010.pdf (accessed on 9 November 2020).
- Martinsson, L.; Furst, C.J.; Lundstrom, S.; Nathanaelsson, L.; Axelsson, B. Registration in a quality register: A method to improve end-of-life care--a cross-sectional study. BMJ Open 2012, 2, e001328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leemans, K.; Deliens, L.; Van den Block, L.; Vander, S.R.; Francke, A.L.; Cohen, J. Systematic Quality Monitoring for Specialized Palliative Care Services: Development of a Minimal Set of Quality Indicators for Palliative Care Study (QPAC). Am. J. Hosp. Palliat Care 2017, 34. [Google Scholar] [CrossRef]
- Plessers, M.; Ghekiere, A.; De Wachter, D.; Deneckere, S.; Tambuyzer, E.; Ramaekers, D. Het ontwikkelen van evidence-based indicatoren van kwaliteit van zorg in Vlaanderen: Een methodologieitle. Preprints 2019, 2020120424. [Google Scholar] [CrossRef]
- Oosterveld-Vlug, M.; Onwuteaka-Philipsen, B.; Ten Koppel, M.; van Hout, H.; Smets, T.; Pivodic, L.; Tanghe, M.; Hockley, J.; Kijowska, V.; Engels, Y.; et al. Evaluating the implementation of the PACE Steps to Success Programme in long-term care facilities in seven countries according to the RE-AIM framework. Implement. Sci. 2019, 14, 107. [Google Scholar] [CrossRef] [Green Version]
- Van Riet Paap, J.; Vissers, K.; Iliffe, S.; Radbruch, L.; Hjermstad, M.J.; Chattat, R.; Vernooij-Dassen, M.; Engels, Y.; IMPACT Research Team. Strategies to implement evidence into practice to improve palliative care: Recommendations of a nominal group approach with expert opinion leaders. BMC Palliat. Care 2015, 14, 47. [Google Scholar] [CrossRef] [Green Version]
- Leemans, K.; Deliens, L.; Francke, A.L.; Vander Stichele, R.; Van Den Block, L.; Cohen, J. Quality indicators for palliative care services: Mixed-method study testing for face validity, feasibility, discriminative power and usefulness. Palliat. Med. 2015, 29. [Google Scholar] [CrossRef] [Green Version]
- Leemans, K.; Cohen, J.; Francke, A.L.; Stichele, R.V.; Claessen, S.J.J.; Block, L.V.D.; Deliens, L. Towards a standardized method of developing quality indicators for palliative care: Protocol of the Quality indicators for Palliative Care (Q-PAC) study. BMC Palliat. Care 2013, 12, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dodd, S.R.; Payne, S.A.; Preston, N.J.; Walshe, C.E. Understanding the Outcomes of Supplementary Support Services in Palliative Care for Older People. A Scoping Review and Mapping Exercise. J. Pain Symptom Manag. 2020, 60, 449–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lood, Q.; Kirkevold, M.; Sjögren, K.; Bergland, Å.; Sandman, P.-O.; Edvardsson, D. Associations between person-centred climate and perceived quality of care in nursing homes: A cross-sectional study of relatives’ experiences. J. Adv. Nurs. 2019, 75, 2526–2534. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.; Kinghorn, P.; Orlando, R.; Armour, K.; Perry, R.; Jones, L.; Coast, J. “The ICECAP-SCM tells you more about what I’m going through”: A think-aloud study measuring quality of life among patients receiving supportive and palliative care. Palliat. Med. 2016, 30, 642–652. [Google Scholar] [CrossRef] [Green Version]
- Brownie, S.; Nancarrow, S. Effects of person-centered care on residents and staff in aged-care facilities: A systematic review. Clin. Interv. Aging 2013, 8, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Smets, T.; Onwuteaka-Philipsen, B.B.D.; Miranda, R.; Pivodic, L.; Tanghe, M.; van Hout, H.; Engels, Y.; Piers, R.; Baranska, I.; Deliens, L.; et al. Integrating palliative care in long-term care facilities across Europe (PACE): Protocol of a cluster randomized controlled trial of the “PACE Steps to Success” intervention in seven countries. BMC Palliat. Care 2018, 17, 47. [Google Scholar] [CrossRef] [Green Version]
- Campbell, S.M.; Kontopantelis, E.; Hannon, K.; Burke, M.; Barber, A.; Lester, H.E. Framework and indicator testing protocol for developing and piloting quality indicators for the UK quality and outcomes framework. BMC Fam. Pract. 2011, 12, 85. [Google Scholar] [CrossRef]
- Fitch, K.; Bernstein, S.J.; Aguilar, M.S.; Burnand, B.; LaCalle, J.R.; Lazaro, P.; van het Loo, M.; McDonnell, J.; Vader, J.; Kahan, J.P. The RAND/UCLA Appropriateness Method User’s Manual; RAND Corporation: Santa Monica, CA, USA, 2001; Available online: http://www.rand.org/pubs/monograph_reports/MR1269 (accessed on 9 November 2020).
- Pasman, H.R.; Brandt, H.E.; Deliens, L.; Francke, A.L. Quality indicators for palliative care: A systematic review. J. Pain Symptom Manag. 2009, 38, 145–156. [Google Scholar] [CrossRef]
- De Roo, M.L.; Leemans, K.; Claessen, S.J.J.; Cohen, J.W.; Pasman, H.R.; Deliens, L.; Francke, A.L.; EURO IMPACT. Quality indicators for palliative care: Update of a systematic review. J. Pain Symptom Manag. 2013, 46, 556–572. [Google Scholar] [CrossRef]
- Pope, C.; Ziebland, S.; Mays, N. Qualitative research in health care. Analysing qualitative data. Br. Med. J. 2000, 320, 114–146. [Google Scholar] [CrossRef]
- Leemans, K.; Van den Block, L.; Vander, S.R.; Francke, A.L.; Deliens, L.; Cohen, J. How to implement quality indicators successfully in palliative care services: Perceptions of team members about facilitators of and barriers to implementation. Support. Care Cancer 2015, 23, 3503–3511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donabedian, A. Quality assurance. Structure, process and outcome. Nurs. Stand. 1992, 7, 4–5. [Google Scholar] [PubMed]
- Mazor, K.M.; Clauser, B.E.; Field, T.; Yood, R.A.; Gurwitz, J.H. A demonstration of the impact of response bias on the results of patient satisfaction surveys. Health Serv. Res. 2002, 37, 1403–1417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shekelle, P.G.; Maclean, C.H.; Morton, S.C.; Wenger, N.S. Assessing care of vulnerable elders: Methods for developing quality indicators. Ann. Intern. Med. 2001, 135, 647–652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorenz, K.A.; Rosenfeld, K.; Wenger, N. Quality indicators for palliative and end-of-life care in vulnerable elders. J. Am. Geriatr. Soc. 2007, 55, S318–S326. [Google Scholar] [CrossRef] [PubMed]
- Hall, S.; Goddard, C.; Stewart, F.; Higginson, I.J. Implementing a quality improvement programme in palliative care in care homes: A qualitative study. BMC Geriatr. 2011, 11, 31. [Google Scholar] [CrossRef] [Green Version]
- Amin, A.; Besdine, R.C.; Blazer, D.G.; Cohen, H.; Fulmer, T.; Ganz, P.A.; Grunwald, M.; Hall, W.J.; Katz, P.R.; Kitzman, D.W.; et al. Assessing care of vulnerable elders-3 quality indicators. J. Am. Geriatr. Soc. 2007, 55, S464–S487. [Google Scholar]
- Detering, K.M.; Hancock, A.D.; Reade, M.C.; Silvester, W. The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. Br. Med. J. 2010, 340, 1345. [Google Scholar] [CrossRef] [Green Version]
- Van den Block, L.; Honinx, E.; Pivodic, L.; Miranda, R.; Onwuteaka-Philipsen, B.D.; van Hout, H.; Pasman, R.W.; Piers, R.; Froggatt, K.; Payne, S.; et al. Evaluation of a Palliative Care Program for Nursing Homes in 7 Countries: The PACE Cluster-Randomized Clinical Trial. JAMA Intern. Med. 2020, 180, 233–242. [Google Scholar] [CrossRef]
- Van Soest-Poortvliet, M.C.; van der Steen, J.T.; Zimmerman, S.; Cohen, L.W.; Reed, D.; Achterberg, W.P.; Ribbe, M.W.; de Vet, H.C.W. Selecting the best instruments to measure quality of end-of-life care and quality of dying in long term care. J. Am. Med. Dir. Assoc. 2013, 14, 179–186. [Google Scholar] [CrossRef]
- Hall, S.; Kolliakou, A.; Petkova, H.; Froggatt, K.; Higginson, I.J. Interventions for improving palliative care for older people living in nursing care homes. Cochrane Database Syst. Rev. 2011, CD007132. [Google Scholar] [CrossRef]
- Sawatzky, R.; Laforest, E.; Schick-Makaroff, K.; Stajduhar, K.; Reimer-Kirkham, S.; Krawczyk, M.; Ohlen, J.; McLeod, B.; Hilliard, N.; Cohen, R.; et al. Design and introduction of a quality of life assessment and practice support system: Perspectives from palliative care settings. J. Patient Rep. Outcomes 2017, 2, 36. [Google Scholar] [CrossRef] [PubMed]
- De Vos, M.L.; van der Veer, S.N.; Graafmans, W.C.; de Keizer, N.F.; Jager, K.J.; Westert, G.P.; van der Vort, P.H.J. Process evaluation of a tailored multifaceted feedback program to improve the quality of intensive care by using quality indicators. Br. Med. J. Qual. Saf. 2013, 22, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Van Riet Paap, J.; Vernooij-Dassen, M.; Brouwer, F.; Meiland, F.; Iliffe, S.; Davies, N.; Leppert, W.; Jaspers, B.; Mariani, E.; Vissers, K.; et al. Improving the organization of palliative care: Identification of barriers and facilitators in five European countries. Implement. Sci. 2014, 9, 130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antunes, B.; Harding, R.; Higginson, I.J. Implementing patient-reported outcome measures in palliative care clinical practice: A systematic review of facilitators and barriers. Palliat. Med. 2014, 28, 158–175. [Google Scholar] [CrossRef] [Green Version]
- Bunn, F.; Goodman, C.; Corazzini, K.; Sharpe, R.; Handley, M.; Lynch, J.; Meyer, J.; Dening, T.; Gordon, A.L. Setting Priorities to Inform Assessment of Care Homes’ Readiness to Participate in Healthcare Innovation: A Systematic Mapping Review and Consensus Process. Int. J. Environ. Res. Public Health 2020, 17, 987. [Google Scholar] [CrossRef] [Green Version]
| Aspect | Definition | Evaluation Method | Criterion to Judge Aspect as Adequate |
|---|---|---|---|
| Individual quality indicators (QI’s) | |||
| Face validity | The extent to which QI’s are subjectively viewed as covering the concept it purports to measure | Qualitative: interview: feedback on every single quality indicator was asked in terms of face validity | Subjective confirmation of validity of quality indicator scores |
| Feasibility | The extent to which the QI’s are measurable | Quantitative: psychometric analyses | Not more than 10% missing values per question |
| Discriminative power | The extent to which a QI discriminates between good and bad quality | Quantitative: psychometric analyses | Not more that 95% of answers in an extreme category Meaningful range between QI scores (min–max ≥20%) |
| Usefulness | The extent to which the QI scores can be used to improve care | Qualitative: interview question “Were you able to define improvement point based on the quality indicator scores and feedback report?” | Subjective confirmation of usefulness |
| Overall quality indicator measurement | |||
| Feasibility | The extent to which the measurement procedure is feasible for caregivers in nursing homes | Qualitative: interview question “Do you have the feeling you are able to measure the quality indicators without any support in the future?” | Subjective information on work-load for caregivers |
| Qualitative: interview question “How did you feel about the length of the questionnaire?” | Subjective information on survey completion time for caregivers | ||
| Original QPAC Set [24] | QPAC for Nursing Homes | ||
|---|---|---|---|
| 1 | Physical aspects of care | Physical aspects of care | 1 |
| 2 | Psychological, social and spiritual aspects of care | Psychological, social and spiritual aspects of care | 2 |
| 3 | Care planning, information and communication with patients | Autonomy and dignity | 3 |
| Care planning and communication with residents | 4 | ||
| 4 | Care planning, information and communication with family | Communication with family | 5 |
| 5 | Care planning, information and communication between caregivers | Communication between caregivers | 6 |
| 6 | Circumstances surrounding death | Care and circumstances surrounding death | 7 |
| 7 | Coordination and continuity of care | ||
| 8 | Support for family | Care for family | 8 |
| Total | |
|---|---|
| Professional caregivers from care homes | 7 |
| Head nurse/Referent nurse | 3 |
| Paramedic | 1 |
| Care personnel | 1 |
| Physician | 1 |
| Quality coordinator | 1 |
| Representatives from residents and next-of-kin | 3 |
| Flemish Expertise Centre for Dementia | 1 |
| Alzheimer League, family council | 1 |
| Flemish elderly council | 1 |
| Palliative care research and policy | 5 |
| KU Leuven—LUCAS research group | 2 |
| Flemish Federation Palliative Care | 1 |
| Local Palliative home care network Westhoek-Oostende | 1 |
| Flemish agency for care and health | 1 |
| Domain: Physical Aspects of Care | |||||
| N | Short title | Description of the indicator | Respondent | Mean score (%) | Range (min–max) |
| PC-1 | Being in pain | Percentage of residents with a pain score of 3 or more in the last three days | Residents | 30.7 | 37.1 (19.1–56.3) |
| Domain: Psychological, Social and Spiritual Aspects of Care | |||||
| N | Short title | Description of the indicator | Respondent | Mean score (%) | Range (min–max) |
| PC-2 | Feeling worried or anxious, or a burden | Percentage of residents who indicate they were most of the times or always feeling worried or anxious, or a burden to others | Residents | 9.2 | 23 (4.3–27.3) |
| PC-3 | Being around people who care about you | Percentage of residents who indicate that they were most of the times or always able to be around people who cared about them | Residents | 57.1 | 42.9 (29.8–72.7) |
| Domain: Autonomy and Dignity | |||||
| N | Short title | Description of the indicator | Respondent | Mean score (%) | Range (min–max) |
| PC-4 | Personal wishes and beliefs respected | Percentage of residents who indicate that their caregivers most of the times or always respecting their personal wishes and beliefs | Residents | 63.3 | 55.7 (35.2–90.9) |
| PC-5 | Decisions about life and care | Percentage of residents who indicate that they most of the times or always can make their own decisions about their life and care | Residents | 44.2 | 35.4 (31.3–66.7) |
| PC-6 | Treated with respect | Percentage of residents who indicate that they most of the times or always were treated with respect | Residents | 68.6 | 47.2 (43.8–90.9) |
| Domain: Care Planning and Communication with Residents | |||||
| N | Short title | Description of the indicator | Respondent | Mean score (%) | Range (min–max) |
| ACP-1 | Information comprehensible and not contradictory | Percentage of residents who indicate that they most of the times or always receive comprehensible information and almost never of never contradictory information | Residents | 79.5 | 21.4 (72.3–93.8) |
| ACP-2 | Conversation with family | Percentage of residents for whom the next-of-kin indicates that more than once a conversation took place with the caregivers, the next-of-kin and, when possible, the resident | Next-of-kin | 47.6 | 100 (0–100) |
| ACP-3 | Knowledge about care goals and life wishes | Percentage of residents for whom their professional caregiver indicates that they have knowledge about the residents’ care goals and life wishes. | Professional caregiver | 63.8 | 40 (47.1–87.1) |
| ACP-4 | Encouraging ACP | Percentage of residents for whom their professional caregiver indicates that they often or very often encourage residents and their next-of-kins to involve in advance care planning. | Professional caregiver | 37.7 | 72.5 (10.8–83.3) |
| Domain: Communication with Family | |||||
| N | Short title | Description of the indicator | Respondent | Mean score (%) | Range (min–max) |
| ACP-5 | Next-of-kin involved in decisions | Percentage of next-of-kin who indicate that they often or very often felt involved in the decisions taken about the resident. | Next-of-kin | 64.7 | 75 (25–100) |
| EOL-1 | Information about approaching death | Percentage of next-of-kin who indicate that they received the right amount of information on the approaching death of the resident. | Next-of-kin | 73.5 | 35.7 (64.3–100) |
| Domain: Communication between Caregivers | |||||
| N | Short title | Description of the indicator | Respondent | Mean score (%) | Range (min–max) |
| PC-8 | Information in resident file | Percentage of residents for whom the professional caregiver finds sufficient information in the resident file when needed. | Professional caregiver | 69.3 | 37.6 (52.7–90.3) |
| Domain: Care and Circumstances Surrounding Death | |||||
| N | Short title | Description of the indicator | Respondent | Mean score (%) | Range (min–max) |
| EOL-3 | Comfortable in last week of life | Percentage of next-of-kin who indicate that many or a lot of measures were taken to make the resident comfortable in the last week of life. | Next-of-kin | 67.6 | 100 (0–100) |
| EOL-4 | Recognizing the approaching death | Percentage of residents for whom the professional caregiver indicates they could recognize the approaching death well or very well by physical changes. | Professional caregiver | 91.7 | 16.7 (83.3–100) |
| EOL-5 | Satisfied by care delivered | Percentage of residents for whom the professional caregiver indicates they are satisfied with the care delivered to the resident. | Professional caregiver | 95.8 | 16.7 (83.3–100) |
| EOL-6 | Support by specialized palliative care | Percentage of residents for whom the professional caregiver indicates a palliative care referent or specialized team was involved in the care for the resident. | Professional caregiver | 68.8 | 100 (0–100) |
| Domain: Care for Family | |||||
| PC-7 | Attention for wishes and feelings of next-of-kin | Percentage of next-of-kin who indicate that the professional caregivers had attention for their wishes and feelings. | Next-of-kin | 67.6 | 30 (50–80) |
| EOL-2 | Supported immediate after death | Percentage of next-of-kin who indicate that they felt sufficiently supported by the professional caregivers immediate after the death of the resident. | Next-of-kin | 85.3 | 66.7 (33.3–100) |
| Response Type | Total | Female (%) | Age of Resident | Dementia B (%) | Length of Stay C | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| <75 (%) | 75–84 (%) | 85–94 (%) | >94 (%) | <12 (%) | 12–24 (%) | >24 (%) | ||||
| Residents | 294 | 214 (73) | 26 (9) | 74 (25) | 157 (53) | 37 (13) | NA | NA | NA | NA |
| Resident him/herself | 114 | 83 (73) | 11 (10) | 24 (21) | 67 (59) | 12 (11) | NA | NA | NA | NA |
| Together with family caregiver | 63 | 43 (68) | 5 (8) | 14 (22) | 38 (60) | 6 (10) | NA | NA | NA | NA |
| Family caregivers in the name of the resident | 116 A | 87 (75) | 10 (9) | 35 (30) | 52 (45) | 19 (16) | 56 (48) | 37 (33) | 22 (20) | 52 (47) |
| Professional caregivers | 393 | 305 (73) | 27 (7) | 97 (25) | 218 (55) | 51 (13) | 204 (49) | 125 (32) | 60 (15) | 208 (53) |
| Residents who lived in the facility | 345 | 257 (74) | 25 (7) | 88 (26) | 193 (56) | 39 (11) | 162 (47) | 109 (32) | 54 (16) | 182 (53) |
| Deceased residents | 48 | 31 (65) | 2 (4) | 9 (19) | 25 (52) | 12 (25) | 29 (60) | 16 (33) | 6 (13) | 26 (54) |
| Family caregivers | 34 | 22 (65) | 1 (3) | 7 (21) | 17 (50) | 9 (26) | 16 (47) | 14 (41) | 5 (15) | 15 (44) |
| Barrier (b) or Facilitator (f) | Quote from Caregivers or Field Notes | Diary by Coordinator | Interview with Coordinator |
|---|---|---|---|
| The use of the instrument in general terms | |||
| Lack of time and staff to perform quality measurement (b) | “To sell the instrument: make it a sort of an obligation, otherwise it will not happen, I think. So much extra is added [next to the regular work], and also many projects that are already there anyway” (coordinator nursing home) | X | X |
| Readiness of the team to perform quality monitoring together (f) | “[experience with implementation of the quality assessment] it was ok. It also depends on the enthusiasm and commitment of the persons who are doing it.” (coordinator nursing home) | X | |
| Step 1: Appointing coordinator | |||
| Presence of a good coordinator to guide the quality measurement (f) | “Appointment of the coordinator: one is not enough. Depends on the size of the nursing home.” (coordinator nursing home) “Announced [the quality assessment] during team meeting. They [coordinators] had made a step-by-step plan and mailed it to the staff, how they could easily find it and fill it in … everything went smoothly” (coordinator nursing home) | X | X |
| Step 2: Data collection with the quality indicators | |||
| Bad timing regarding the start of measurement (i.e., sick staff, loss of coordinator) (b) | Some of the coordinators became absent during the procedure and the person who took over didn’t have all the needed paperwork. (field notes researchers). Some nursing homes forgot to record the total of included participants, didn’t sent out the recruited number of questionnaires or didn’t sent questionnaires to family caregivers. The reason they indicated was the moment of the measurement was not convenient (field notes researchers). | X | |
| Lack of computer literacy in all participants (b) | “They [family and residents] had no e-mail and some [family] had to come to the nursing home to fill it [the questionnaire] in.” In some nursing homes professional caregivers didn’t had a work email and in one of these homes, the coordinator had to aid each included professional caregivers with opening the link [which made available on the desktop] to the questionnaire (field notes researchers). | X | |
| Lack of technology in the nursing homes (b) | “It was a lot of time investment, there was only one iPad available in the nursing home, so we had to arrange a lot. WIFI connection was also not reliable, which limited usability.” (coordinator nursing home) | X | X |
| Feasible workload (f) | All coordinators found the overall workload feasible (field notes researchers) “A lot of work in preparation by the coordinator so the coordinator should certainly have time to prepare. Once it runs [there is] little follow-up work.” (coordinator nursing home) | X | X |
| Step 3: Analysis of results by researchers | |||
| Low(er) response rate because of measurement procedure (b) AND Inclusion of deceased residents due to low mortality (b) | “With a longer measurement period, they [respondents] could fill in more” (coordinator nursing home) | X | X |
| Fast (within two weeks) analysis of questionnaires because of the use of digital data (f) | Because we used online questionnaires the researchers didn’t need to input any data but could directly analyse resulting in fast feed-back to the nursing homes | X | |
| Step 4: Interpretation of results by coordinator and nursing home team | |||
| Easy to interpret results (f) | “The results indicate clear work points. Results are recognizable” (coordinator nursing home) | X | |
| Struggle to go from interpretation to establishing improvement goals (b) | Most coordinators indicate they recognize the results, but they cannot (yet) make clear improvement goals. (field notes researchers) | X | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dupont, C.; De Schreye, R.; Cohen, J.; De Ridder, M.; Van den Block, L.; Deliens, L.; Leemans, K. Pilot Study to Develop and Test Palliative Care Quality Indicators for Nursing Homes. Int. J. Environ. Res. Public Health 2021, 18, 829. https://doi.org/10.3390/ijerph18020829
Dupont C, De Schreye R, Cohen J, De Ridder M, Van den Block L, Deliens L, Leemans K. Pilot Study to Develop and Test Palliative Care Quality Indicators for Nursing Homes. International Journal of Environmental Research and Public Health. 2021; 18(2):829. https://doi.org/10.3390/ijerph18020829
Chicago/Turabian StyleDupont, Charlèss, Robrecht De Schreye, Joachim Cohen, Mark De Ridder, Lieve Van den Block, Luc Deliens, and Kathleen Leemans. 2021. "Pilot Study to Develop and Test Palliative Care Quality Indicators for Nursing Homes" International Journal of Environmental Research and Public Health 18, no. 2: 829. https://doi.org/10.3390/ijerph18020829
APA StyleDupont, C., De Schreye, R., Cohen, J., De Ridder, M., Van den Block, L., Deliens, L., & Leemans, K. (2021). Pilot Study to Develop and Test Palliative Care Quality Indicators for Nursing Homes. International Journal of Environmental Research and Public Health, 18(2), 829. https://doi.org/10.3390/ijerph18020829






