Development and Validation of 3 Min Incremental Step-In-Place Test for Predicting Maximal Oxygen Uptake in Home Settings: A Submaximal Exercise Study to Assess Cardiorespiratory Fitness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Maximal Oxygen Consumption
2.4. MISP Test
2.5. Statistical Analysis
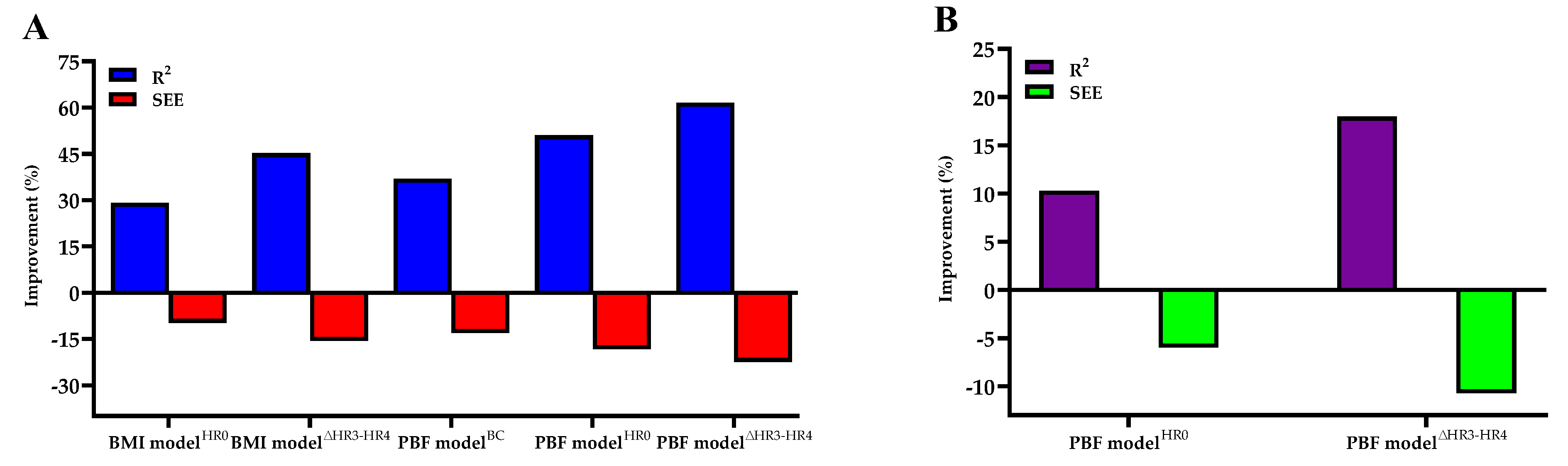
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Hong, S.H.; Yang, H.I.; Kim, D.I.; Gonzales, T.I.; Brage, S.; Jeon, J.Y. Validation of Submaximal Step Tests and the 6-Min Walk Test for Predicting Maximal Oxygen Consumption in Young and Healthy Participants. Int. J. Environ. Res. Public Health 2019, 16, 4858. [Google Scholar] [CrossRef] [Green Version]
- Chung, Y.-C.; Huang, C.-Y.; Wu, H.-J.; Kan, N.-W.; Ho, C.-S.; Huang, C.-C.; Chen, H.-T. Predicting maximal oxygen uptake from a 3-minute progressive knee-ups and step test. PeerJ 2021, 9, e10831. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, T.; So, R.; Takahashi, M. Estimating cardiorespiratory fitness from heart rates both during and after stepping exercise: A validated simple and safe procedure for step tests at worksites. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 120, 2445–2454. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Després, J.-P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; et al. Importance of assessing cardiorespiratory fitness in clinical practice: A case for fitness as a clinical vital sign: A scientific statement from the american heart association. Circulation 2016, 134, e653–e699. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.; Phadke, A.; Patil, P.; Joshi, A. Comparison Of Non-exercise Test and Step Test In Estimation of Aerobic Capacity (VO2max) In Young Adults. Natl. J. Physiol. Pharm. Pharmacol. 2014, 4, 1. [Google Scholar] [CrossRef]
- Beutner, F.; Ubrich, R.; Zachariae, S.; Engel, C.; Sandri, M.; Teren, A.; Gielen, S. Validation of a brief step-test protocol for estimation of peak oxygen uptake. Eur. J. Prev. Cardiol. 2015, 22, 503–512. [Google Scholar] [CrossRef]
- Nes, B.M.; Janszky, I.; Vatten, L.J.; Nilsen, T.I.; Aspenes, S.T.; Wisløff, U. Estimating VO2 peak from a nonexercise prediction model: The HUNT Study, Norway. Med. Sci. Sports Exerc. 2011, 43, 2024–2030. [Google Scholar] [CrossRef]
- Sui, X.; LaMonte, M.J.; Blair, S.N. Cardiorespiratory fitness as a predictor of nonfatal cardiovascular events in asymptomatic women and men. Am. J. Epidemiol. 2007, 165, 1413–1423. [Google Scholar] [CrossRef]
- De Sousa, N.; Bertucci, D.R.; de Sant’Ana, G.M.; Padua, P.; da Rosa, D.M. Incremental and decremental cardiopulmonary exercise testing protocols produce similar maximum oxygen uptake in athletes. Sci. Rep. 2021, 11, 13118. [Google Scholar] [CrossRef]
- Cooney, J.K.; Moore, J.P.; Ahmad, Y.A.; Jones, J.G.; Lemmey, A.B.; Casanova, F.; Maddison, P.J.; Thom, J.M. A simple step test to estimate cardio-respiratory fitness levels of rheumatoid arthritis patients in a clinical setting. Int. J. Rheumatol. 2013, 2013, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Cooper, K.H. A means of assessing maximal oxygen intake. Correlation between field and treadmill testing. JAMA 1968, 203, 201–204. [Google Scholar] [CrossRef]
- Léger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef]
- Noonan, V.; Dean, E. Submaximal exercise testing: Clinical application and interpretation. Phys. Ther. 2000, 80, 782–807. [Google Scholar] [CrossRef]
- Elsaidy, W.S.I.M. Evaluating the validity and reliability of Harvard step test to predict VO2max in terms of the step height according to the knee joint angle. Theor. Appl. Int. Ed. 2011, 1, 126–132. [Google Scholar]
- Sopalard, M.; Leelarungrayub, J.; Klaphajone, J. Variation of knee angle and leg length for predicting VO2max in healthy male volunteers using the Queen’s College step test. J. Phys. Educ. Sport 2016, 16, 275–280. [Google Scholar]
- Van Kieu, N.T.; Jung, S.-J.; Shin, S.-W.; Jung, H.-W.; Jung, E.-S.; Won, Y.H.; Kim, Y.-G.; Chae, S.-W. The Validity of the YMCA 3-Minute Step Test for Estimating Maximal Oxygen Uptake in Healthy Korean and Vietnamese Adults. J. Lifestyle Med. 2020, 10, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Lee, O.; Lee, S.; Kang, M.; Mun, J.; Chung, J. Prediction of maximal oxygen consumption using the Young Men’s Christian Association-step test in Korean adults. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 119, 1245–1252. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Bubela, D.J.; Wang, Y.C.; Magasi, S.S.; Gershon, R.C. Six-minute walk test versus three-minute step test for measuring functional endurance. J. Strength Cond. Res. 2015, 29, 3240–3244. [Google Scholar] [CrossRef] [Green Version]
- Bohannon, R.W.; Crouch, R.H. Two-minute step test of exercise capacity: Systematic review of procedures, performance, and clinimetric properties. J. Geriatr. Phys. Ther. 2019, 42, 105–112. [Google Scholar] [CrossRef]
- Miller, R.M.; Chambers, T.L.; Burns, S.P.; Godard, M.P. Validating inbody® 570 multi-frequency bioelectrical impedance analyzer versus DXA for body fat percentage analysis. Med. Sci. Sports Exerc. 2016, 48, 991. [Google Scholar] [CrossRef] [Green Version]
- Riebe, D.; Ehrman, J.K.; Liguori, G.; Magal, M. Clinical exercise testing and interpretation. In ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2016; pp. 93–142. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation coefficients: Appropriate use and interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef] [PubMed]
- Holiday, D.B.; Ballard, J.; McKeown, B.C. PRESS-related statistics: Regression tools for cross-validation and case diagnostics. Med. Sci. Sports Exerc. 1995, 27, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Giavarina, D. Understanding bland altman analysis. Biochem. Med. 2015, 25, 141–151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García, R.C.F.; De Oliveira, R.M.; Martínez, E.C.; Neves, E.B. VO2 estimation equation accuracy to young adults. Arch. Med. 2019, 20, 33–39. [Google Scholar] [CrossRef]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef] [Green Version]
- Jiménez-Pavón, D.; Lavie, C.J.; Blair, S.N. The role of cardiorespiratory fitness on the risk of sudden cardiac death at the population level: A systematic review and meta-analysis of the available evidence. Prog. Cardiovasc. Dis. 2019, 62, 279–287. [Google Scholar] [CrossRef]
- Christensen, R.A.G.; Arneja, J.; Cyr, K.S.; Sturrock, S.L.; Brooks, J.D. The association of estimated cardiorespiratory fitness with COVID-19 incidence and mortality: A cohort study. PLoS ONE 2021, 16, e0250508. [Google Scholar] [CrossRef] [PubMed]
- Strauss, M.; Foshag, P.; Jehn, U.; Brzęk, A.; Littwitz, H.; Leischik, R. Higher cardiorespiratory fitness is strongly associated with lower cardiovascular risk factors in firefighters: A cross-sectional study in a German fire brigade. Sci. Rep. 2021, 11, 1–7. [Google Scholar] [CrossRef]
- Schwendinger, F.; Pocecco, E. Counteracting physical inactivity during the COVID-19 pandemic: Evidence-based recommendations for home-based exercise. Int. J. Environ. Res. Public Health 2020, 17, 3909. [Google Scholar] [CrossRef]
- Ahmed, I. COVID-19–does exercise prescription and maximal oxygen uptake (VO2max) have a role in risk-stratifying patients? Clin. Med. 2020, 20, 282–284. [Google Scholar] [CrossRef]
- Berglund, I.J.; Sørås, S.E.; Relling, B.E.; Lundgren, K.M.; Kiel, I.A.; Moholdt, T. The relationship between maximum heart rate in a cardiorespiratory fitness test and in a maximum heart rate test. J. Sci. Med. Sport 2019, 22, 607–610. [Google Scholar] [CrossRef]
- Facioli, T.P.; Philbois, S.V.; Gastaldi, A.C.; Almeida, D.S.; Maida, K.D.; Rodrigues, J.A.L.; Sánchez-Delgado, J.C.; Souza, H.C.D. Study of heart rate recovery and cardiovascular autonomic modulation in healthy participants after submaximal exercise. Sci. Rep. 2021, 11, 1–9. [Google Scholar] [CrossRef]
- Grant, C.C.; Murray, C.; Van Rensburg, D.C.J.; Fletcher, L. A comparison between heart rate and heart rate variability as indicators of cardiac health and fitness. Front. Physiol. 2013, 4, 337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chatterjee, S.; Mukherjee, P.S.; Bandyopadhyay, A. Validity of Queen’s College step test for use with young Indian men. Br. J. Sports Med. 2004, 38, 289–291. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Chatterjee, P.; Bandyopadhyay, A. Validity of Queen’s College Step Test for estimation of maximum oxygen uptake in female students. Indian J. Med. Res. 2005, 121, 32–35. [Google Scholar] [PubMed]
- Ekblom-Bak, E.; Bjorkman, F.; Hellenius, M.; Ekblom, B. A new submaximal cycle ergometer test for prediction of VO2max. Scand. J. Med. Sci. Sports 2014, 24, 319–326. [Google Scholar] [CrossRef] [Green Version]
- Ibikunle, P.O.; Enumah, U.G. Maximum oxygen uptake and cardiovascular response of Professional male football and Basketball players to Chester step test. IOSR J. Sports Phys. Educ. 2016, 3, 1–5. [Google Scholar] [CrossRef]
- Matsuo, T.; So, R.; Takahashi, M. Workers’ physical activity data contribute to estimating maximal oxygen consumption: A questionnaire study to concurrently assess workers’ sedentary behavior and cardiorespiratory fitness. BMC Public Health 2020, 20, 22. [Google Scholar] [CrossRef]
- Cao, Z.-B.; Miyatake, N.; Aoyama, T.; Higuchi, M.; Tabata, I. Prediction of maximal oxygen uptake from a 3-minute walk based on gender, age, and body composition. J. Phys. Act. Health 2013, 10, 280–287. [Google Scholar] [CrossRef]
- Elliott, D.; Abt, G.; Barry, T. The effect of an active arm action on heart rate and predicted VO2max during the Chester step test. J. Sci. Med. Sport 2008, 11, 112–115. [Google Scholar] [CrossRef]
- Cheung, P.P. Review of Various Step Test Protocols for Use in Assessing Aerobic Fitness in Schools. Asian J. Phys. Educ. Recreat. 2012, 18, 74–81. [Google Scholar] [CrossRef]
- Yan, L.; Croce, R.; Horvat, M.; Roswal, G.; Fallaize, A.; Love, K. Determination of Cardiovascular Functioning in Chinese Adults with Intellectual Disabilities using the 3-Minute Step Test. Clin. Kinesiol. 2019, 73, 8–14. [Google Scholar]


| Training Group | Testing Group | ES | |||||
|---|---|---|---|---|---|---|---|
| Women (n = 69) | Men (n = 74) | Total (n = 143) | Women (n = 31) | Men (n = 31) | Total (n = 62) | ||
| Age (years) | 43.36 ± 9.51 | 43.24 ± 10.52 | 43.30 ± 10.01 | 44.94 ± 10.36 | 43.52 ± 10.13 | 44.23 ± 10.19 | −0.09 |
| Height (cm) | 160.30 ± 4.95 | 171.78 ± 5.48 | 166.24 ± 7.77 | 159.74 ± 5.50 | 173.40 ± 6.66 | 166.57 ± 9.17 | −0.04 |
| Body weight (kg) | 59.40 ± 8.41 | 75.57 ± 10.72 | 67.77 ± 12.60 | 59.47 ± 10.59 | 75.90 ± 11.78 | 67.69 ± 13.86 | 0.01 |
| BMI (kg/m2) | 23.08 ± 2.74 | 25.61 ± 3.32 | 24.39 ± 3.30 | 23.22 ± 3.24 | 25.22 ± 3.50 | 24.22 ± 3.49 | 0.05 |
| PBF (%) | 28.94 ± 6.25 | 22.32 ± 6.43 | 25.51 ± 7.14 | 29.79 ± 6.20 | 23.06 ± 5.59 | 26.42 ± 6.77 | −0.13 |
| O2max (mL·kg−1·min−1) | 31.85 ± 5.70 | 37.85 ± 6.90 | 34.96 ± 7.01 | 29.40 ± 5.54 | 36.31 ± 6.42 | 32.86 ± 6.89 * | 0.30 |
| HR0 (bpm) | 85 ± 12 | 80 ± 12 | 82 ± 12 | 86 ± 9 | 84 ± 9 | 85 ± 9 | −0.28 |
| ΔHR3 − HR4 (bpm) | 28 ± 8 | 31 ± 8 | 29 ± 8 | 26 ± 8 | 30 ± 7 | 28 ± 8 | 0.13 |
| O2max | Age | Gender | BMI | PBF | HR0 | HR3 | ∆HR3 − HR4 | |
|---|---|---|---|---|---|---|---|---|
| Age | −0.239 ** | |||||||
| Gender (women = 0, men = 1) | 0.430 ** | −0.006 | ||||||
| BMI | −0.191 * | −0.044 | 0.385 ** | |||||
| PBF | −0.706 ** | 0.084 | −0.465 ** | 0.334 ** | ||||
| HR0 | −0.516 ** | 0.007 | −0.203 * | 0.170 * | 0.439 ** | |||
| HR3 | −0.198 * | −0.177 * | −0.184 * | 0.007 | 0.198 * | 0.562 ** | ||
| ∆HR3 − HR4 | 0.563 ** | −0.102 | 0.187 * | −0.128 | −0.406 ** | −0.551 ** | −0.116 | |
| HRpeak | 0.308 ** | −0.676 ** | 0.015 | −0.057 | −0.190 * | −0.065 | 0.061 | 0.064 |
| O2max (mL·kg−1·min−1) | PBF Model (%) | p Value | BMI Model (kg·m−2) | p Value | ||||
|---|---|---|---|---|---|---|---|---|
| B | Standard Error | β | B | Standard Error | β | |||
| ModelBC | ||||||||
| Constant | 55.261 | 2.484 | <0.001 | 60.719 | 4.163 | <0.001 | ||
| Age (years) | −0.130 | 0.040 | −0.186 | 0.002 | −0.178 | 0.046 | −0.255 | <0.001 |
| Gender (women = 0, men = 1) | 1.925 | 0.903 | 0.138 | 0.035 | 8.299 | 0.996 | 0.594 | <0.001 |
| Body composition | −0.614 | 0.064 | −0.626 | <0.001 | −0.916 | 0.152 | −0.431 | <0.001 |
| F | 55.583 | 30.686 | ||||||
| p | <0.001 | <0.001 | ||||||
| R2 | 0.545 | 0.398 | ||||||
| Adjusted R2 | 0.536 | 0.385 | ||||||
| SEE (mL·kg−1·min−1) | 4.7757 | 5.4936 | ||||||
| SEE% | 13.662 | 15.716 | ||||||
| R2p | 0.534 | 0.396 | ||||||
| SEEp | 4.8772 | 5.7061 | ||||||
| ModelHR0 | ||||||||
| Constant | 65.240 | 3.262 | <0.001 | 73.265 | 4.348 | <0.001 | ||
| Age (years) | −0.135 | 0.038 | −0.194 | <0.001 | −0.174 | 0.042 | −0.248 | <0.001 |
| Gender (0 = women, 1 = men) | 1.932 | 0.849 | 0.138 | 0.024 | 6.707 | 0.941 | 0.480 | <0.001 |
| Body composition | −0.500 | 0.065 | −0.510 | <0.001 | −0.691 | 0.142 | −0.325 | <0.001 |
| HR0 (bpm) | −0.154 | 0.035 | −0.262 | <0.001 | −0.212 | 0.037 | −0.361 | <0.001 |
| F | 51.952 | 36.465 | ||||||
| p | <0.001 | <0.001 | ||||||
| R2 | 0.601 | 0.514 | ||||||
| Adjusted R2 | 0.589 | 0.500 | ||||||
| SEE (mL·kg−1·min−1) | 4.4905 | 4.9564 | ||||||
| SEE% | 12.847 | 14.179 | ||||||
| R2p | 0.587 | 0.507 | ||||||
| SEEp | 4.5226 | 4.9852 | ||||||
| Model∆HR3−HR4 | ||||||||
| Constant | 51.312 | 4.650 | <0.001 | 55.761 | 5.596 | <0.001 | ||
| Age (years) | −0.121 | 0.036 | −0.173 | 0.001 | −0.152 | 0.039 | −0.217 | <0.001 |
| Gender (0 = women, 1 = men) | 1.927 | 0.806 | 0.138 | 0.018 | 6.204 | 0.887 | 0.444 | <0.001 |
| Body composition | −0.452 | 0.063 | −0.461 | <0.001 | −0.632 | 0.134 | −0.297 | <0.001 |
| HR0 (bpm) | −0.085 | 0.038 | −0.145 | 0.025 | −0.120 | 0.040 | −0.203 | 0.003 |
| ∆HR3 − HR4 (bpm) | 0.220 | 0.055 | 0.253 | <0.001 | 0.267 | 0.059 | 0.308 | <0.001 |
| F | 49.338 | 37.494 | ||||||
| p | <0.001 | <0.001 | ||||||
| R2 | 0.643 | 0.578 | ||||||
| Adjusted R2 | 0.630 | 0.562 | ||||||
| SEE (mL·kg−1·min−1) | 4.2631 | 4.6358 | ||||||
| SEE% | 12.196 | 13.262 | ||||||
| R2p | 0.651 | 0.587 | ||||||
| SEEp | 4.1861 | 4.6178 | ||||||
| Subgroup | N (%) | PBF ModelBC | PBF ModelHR0 | PBF Model∆HR3 − HR4 | BMI ModelBC | BMI ModelHR0 | BMI Model∆HR3 − HR4 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CE | SD | CE | SD | CE | SD | CE | SD | CE | SD | CE | SD | ||
| Gender | |||||||||||||
| Women | 100 (48.8) | −0.53 | 4.42 | −0.51 | 4.30 | −0.46 | 4.00 | −0.63 | 5.32 | −0.58 | 4.91 | −0.50 | 4.55 |
| Men | 105 (51.2) | −0.31 | 5.07 | −0.13 | 4.59 | −0.23 | 4.35 | −0.55 | 5.67 | −0.24 | 4.91 | −0.35 | 4.57 |
| Age (years) | |||||||||||||
| <40 | 71 (34.6) | −0.35 | 5.11 | −0.28 | 4.47 | −0.37 | 4.15 | −0.39 | 6.16 | −0.28 | 5.16 | −0.39 | 4.78 |
| 40–50 | 72 (35.1) | −1.30 | 4.48 | −1.10 | 4.31 | −0.96 | 4.16 | −1.33 | 5.17 | −1.05 | 4.73 | −0.91 | 4.51 |
| ≥50 | 62 (30.2) | 0.52 | 4.52 | 0.54 | 4.48 | 0.42 | 4.16 | 0.05 | 5.00 | 0.19 | 4.76 | 0.10 | 4.35 |
| O2max (mL·kg−1·min−1) | |||||||||||||
| <32 | 73 (35.6) | −3.21 | 4.00 | −2.94 | 3.73 | −2.57 | 3.53 | −4.57 | 4.57 | −3.84 | 4.07 | −3.26 | 3.97 |
| 32–38 | 75 (36.6) | −1.00 | 3.86 | −0.78 | 3.80 | −0.79 | 3.86 | −0.83 | 3.67 | −0.57 | 3.79 | −0.62 | 3.84 |
| ≥38 | 57 (27.8) | 3.91 | 3.51 | 3.64 | 3.12 | 3.11 | 2.99 | 4.83 | 3.80 | 4.21 | 3.17 | 3.47 | 3.14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, F.; Chang, C.-H.; Chung, Y.-C.; Wu, H.-J.; Kan, N.-W.; ChangChien, W.-S.; Ho, C.-S.; Huang, C.-C. Development and Validation of 3 Min Incremental Step-In-Place Test for Predicting Maximal Oxygen Uptake in Home Settings: A Submaximal Exercise Study to Assess Cardiorespiratory Fitness. Int. J. Environ. Res. Public Health 2021, 18, 10750. https://doi.org/10.3390/ijerph182010750
Li F, Chang C-H, Chung Y-C, Wu H-J, Kan N-W, ChangChien W-S, Ho C-S, Huang C-C. Development and Validation of 3 Min Incremental Step-In-Place Test for Predicting Maximal Oxygen Uptake in Home Settings: A Submaximal Exercise Study to Assess Cardiorespiratory Fitness. International Journal of Environmental Research and Public Health. 2021; 18(20):10750. https://doi.org/10.3390/ijerph182010750
Chicago/Turabian StyleLi, Fang, Chun-Hao Chang, Yu-Chun Chung, Huey-June Wu, Nai-Wen Kan, Wen-Sheng ChangChien, Chin-Shan Ho, and Chi-Chang Huang. 2021. "Development and Validation of 3 Min Incremental Step-In-Place Test for Predicting Maximal Oxygen Uptake in Home Settings: A Submaximal Exercise Study to Assess Cardiorespiratory Fitness" International Journal of Environmental Research and Public Health 18, no. 20: 10750. https://doi.org/10.3390/ijerph182010750
APA StyleLi, F., Chang, C. -H., Chung, Y. -C., Wu, H. -J., Kan, N. -W., ChangChien, W. -S., Ho, C. -S., & Huang, C. -C. (2021). Development and Validation of 3 Min Incremental Step-In-Place Test for Predicting Maximal Oxygen Uptake in Home Settings: A Submaximal Exercise Study to Assess Cardiorespiratory Fitness. International Journal of Environmental Research and Public Health, 18(20), 10750. https://doi.org/10.3390/ijerph182010750







