Moving Forward: Understanding Correlates of Physical Activity and Sedentary Behaviour during COVID-19—An Integrative Review and Socioecological Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Review Methodology
2.2. Quality Assessment
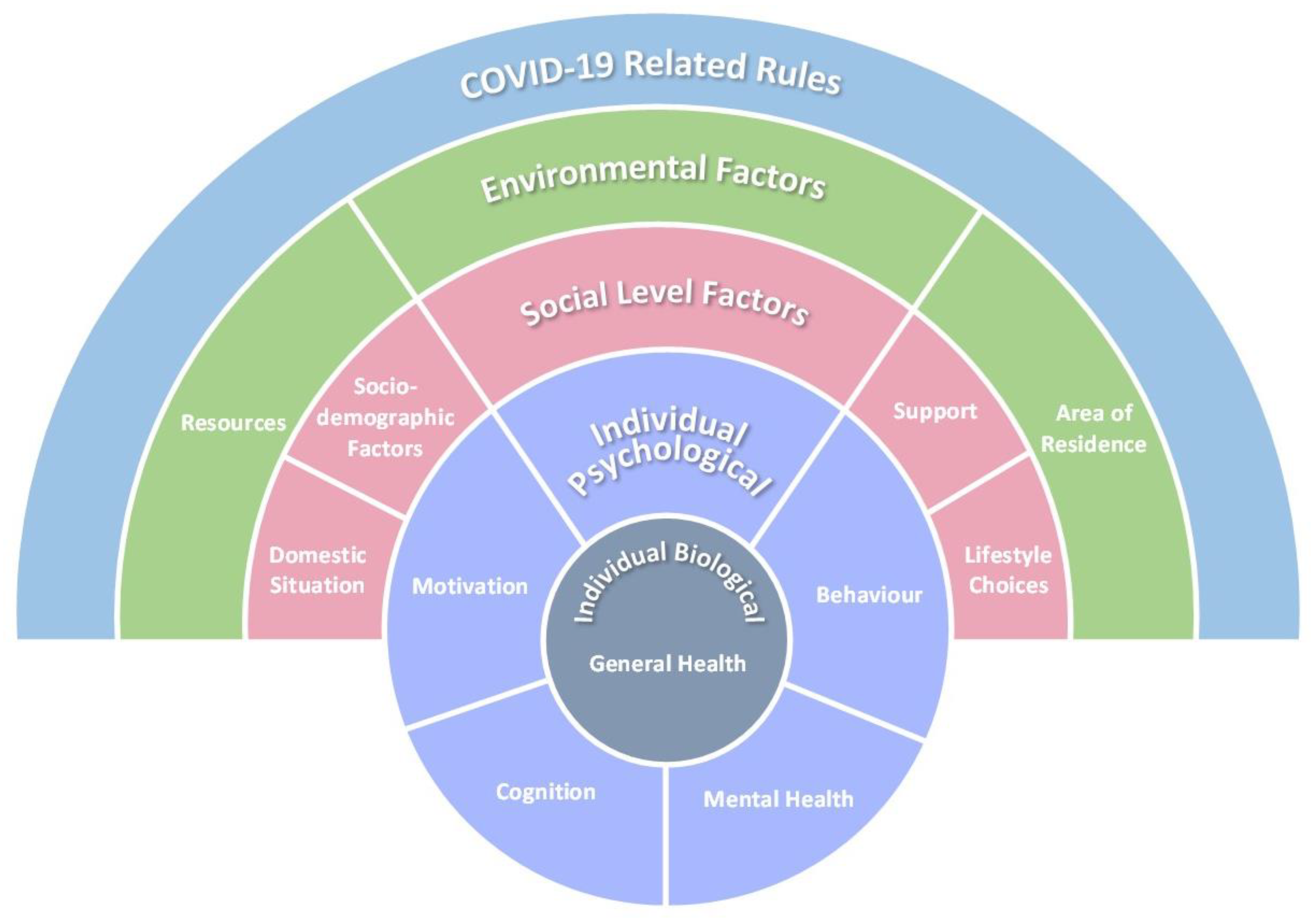
2.3. Data Analysis and Model Development
3. Results
3.1. Individual—Biological Factors
3.1.1. Age and Sex
3.1.2. General Health
3.2. Individual—Psychological Factors
3.2.1. Mental Health
3.2.2. Personality Traits
3.2.3. Motivation
3.2.4. Cognition
3.2.5. Behaviour
3.3. Social Level Factors
3.3.1. Sociodemographics
3.3.2. Support
3.3.3. Domestic Situation
3.3.4. Lifestyle Choices
3.4. Environmental Factors
3.4.1. Area of Residence
3.4.2. Resources
3.5. COVID-19-Related Rules
4. Discussion
4.1. Recommendations for Policy: Mapping to the COM-B
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rhodes, R.E.; Janssen, I.; Bredin, S.S.D.; Warburton, D.E.R.; Bauman, A. Physical activity: Health impact, prevalence, correlates and interventions. Psychol Health 2017, 32, 942–975. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- Sedentary Behaviour Research, N. Letter to the editor: Standardized use of the terms “sedentary” and “sedentary behaviours”. Appl. Physiol. Nutr. Metab. 2012, 37, 540–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too much sitting: The population health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef]
- Matthews, C.E.; Chen, K.Y.; Freedson, P.S.; Buchowski, M.S.; Beech, B.M.; Pate, R.R.; Troiano, R.P. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008, 167, 875–881. [Google Scholar] [CrossRef] [Green Version]
- Hamer, M.; Kivimäki, M.; Gale, C.R.; Batty, G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav. Immun. 2020, 87, 184–187. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19—Weekly Epidemiological Update. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---20-july-2021 (accessed on 22 July 2021).
- World Health Organization. Critical Preparedness, Readiness and Response Actions for COVID-19. Available online: https://apps.who.int/iris/handle/10665/336373 (accessed on 11 November 2020).
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [Green Version]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [Green Version]
- Van Kasteren, Y.F.; Lewis, L.K.; Maeder, A. Office-based physical activity: Mapping a social ecological model approach against COM-B. BMC Public Health 2020, 20, 163. [Google Scholar] [CrossRef]
- Toronto, C.E.; Remington, R. A Step-by-Step Guide to Conducting an Integrative Review, 1st ed.; Springer: Berlin/Heidelberg, Germany, 2020; ISBN 978-3-030-37503-4. [Google Scholar]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT); Version 2018; Registration of Copyright (#1148552); Canadian Intellectual Property Office: Gatineau, QC, Canada, 2018. [Google Scholar]
- Hong, Q.N. Reporting the rResults of the MMAT. Available online: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/140056890/Reporting%20the%20results%20of%20the%20MMAT.pdf (accessed on 9 February 2021).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Smith, B.; McGannon, K.R. Developing rigor in qualitative research: Problems and opportunities within sport and exercise psychology. Int. Rev. Sport Exerc. Psychol. 2018, 11, 101–121. [Google Scholar] [CrossRef]
- Acs, P.; Premusz, V.; Morvay-Sey, K.; Palvolgyi, A.; Trpkovici, M.; Elbert, G.; Melczer, C.; Makai, A. Effects of COVID-19 on physical activity behavior among university students: Results of a Hungarian online survey. Health Probl. Civiliz. 2020, 14, 174–182. [Google Scholar] [CrossRef]
- Alomari, M.A.; Khabour, O.F.; Alzoubi, K.H. Changes in physical activity and sedentary behavior amid confinement: The BKSQ-COVID-19 Project. Risk Manag. Healthc Policy 2020, 13, 1757–1764. [Google Scholar] [CrossRef] [PubMed]
- Angosto, S.; Berengüí, R.; Vegara-Ferri, J.M.; López-Gullón, J.M. Motives and commitment to sport in amateurs during confinement: A segmentation study. Int. J. Environ. Res. Public Health 2020, 17, 7398. [Google Scholar] [CrossRef]
- Asiamah, N.; Opuni, F.F.; Mends-Brew, E.; Mensah, S.W.; Mensah, H.K.; Quansah, F. Short-term changes in behaviors resulting from COVID-19-related social isolation and their influences on mental health in Ghana. Community Ment. Health. J. 2020, 57, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Barwais, F.A. Physical activity at home during the covid-19 pandemic in the two most affected cities in Saudi Arabia. Open Public Health, J. 2020, 13, 470–476. [Google Scholar] [CrossRef]
- Belgen Kaygısız, B.; Güçhan Topcu, Z.; Meriç, A.; Gözgen, H.; Çoban, F. Determination of exercise habits, physical activity level and anxiety level of postmenopausal women during COVID-19 pandemic. Health Care Women Int. 2020, 41, 1240–1254. [Google Scholar] [CrossRef]
- Brady, S.M.; Fenton, S.A.M.; Metsios, G.S.; Bosworth, A.; Duda, J.L.; Kitas, G.D.; Veldhuijzen van Zanten, J.J.C.S. Different types of physical activity are positively associated with indicators of mental health and psychological wellbeing in rheumatoid arthritis during COVID-19. Rheumatol. Int. 2020, 41, 335–344. [Google Scholar] [CrossRef]
- Cancello, R.; Soranna, D.; Zambra, G.; Zambon, A.; Invitti, C. Determinants of the lifestyle Changes during COVID-19 pandemic in the residents of Northern Italy. Int. J. Environ. Res. Public Health 2020, 17, 6287. [Google Scholar] [CrossRef] [PubMed]
- Carriedo, A.; Cecchini, J.A.; Fernandez-Rio, J.; Méndez-Giménez, A. COVID-19, psychological well-being and physical activity levels in older adults during the nationwide lockdown in Spain. Am. J. Geriatr. Psychiatry 2020, 28, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Carriedo, A.; Cecchini, J.A.; Fernandez-Rio, J.; Mendez-Gimenez, A. Resilience and physical activity in people under home isolation due to COVID-19: A preliminary evaluation. Ment. Health Phys. Act. 2020, 19, 100361. [Google Scholar] [CrossRef] [PubMed]
- Castaneda-Babarro, A.; Arbillaga-Etxarri, A.; Gutierrez-Santamaria, B.; Coca, A. Physical activity change during COVID-19 confinement. Int. J. Environ. Res. Public Health 2020, 17, 6878. [Google Scholar] [CrossRef] [PubMed]
- Cecchini, J.A.; Carriedo, A.; Fernandez-Rio, J.; Mendez-Gimenez, A.; Gonzalez, C.; Sanchez-Martinez, B.; Rodriguez-Gonzalez, P. A longitudinal study on depressive symptoms and physical activity during the Spanish lockdown. Int. J. Clin. Health Psychol. 2021, 21, 100200. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-K.; Hung, C.-L.; Timme, S.; Nosrat, S.; Chu, C.-H. Exercise behavior and mood during the COVID-19 pandemic in Taiwan: Lessons for the future. Int. J. Environ. Res. Public Health 2020, 17, 7092. [Google Scholar] [CrossRef] [PubMed]
- Chirico, A.; Lucidi, F.; Galli, F.; Giancamilli, F.; Vitale, J.; Borghi, S.; La Torre, A.; Codella, R. COVID-19 outbreak and physical activity in the Italian population: A cross-sectional analysis of the underlying psychosocial mechanisms. Front. Psychol. 2020, 11, 2100. [Google Scholar] [CrossRef]
- Colley, R.C.; Bushnik, T.; Langlois, K. Exercise and screen time during the COVID-19 pandemic. Health Rep. 2020, 31, 3–11. [Google Scholar] [CrossRef]
- Constant, B.; Thibaut, E.; De Bosscher, V.; Scheerder, J.; Ricour, M.; Willem, A. Exercising in times of lockdown: An analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. Int. J. Environ. Res. Public Health 2020, 17, 4144. [Google Scholar] [CrossRef]
- Coughenour, C.; Gakh, M.; Pharr, J.R.; Bungum, T.; Jalene, S. Changes in depression and physical activity among college students on a diverse campus after a COVID-19 stay-at-home order. J. Community Health 2020, 46, 758–766. [Google Scholar] [CrossRef]
- Dunca, G.E.; Aver, A.R.; Seto, E.; Tsang, S. Perceived change in physical activity levels and mental health during COVID-19: Findings among adult twin pairs. PLoS ONE 2020, 15, e0237695. [Google Scholar] [CrossRef]
- Fallon, N.; Brown, C.; Twiddy, H.; Brian, E.; Frank, B.; Nurmikko, T.; Stancak, A. Adverse effects of COVID-19-related lockdown on pain, physical activity and psychological well-being in people with chronic pain. Br. J. Pain 2020, 15, 357–368. [Google Scholar] [CrossRef]
- Fearnbach, S.N.; Flanagan, E.W.; Höchsmann, C.; Beyl, R.A.; Altazan, A.D.; Martin, C.K.; Redman, L.M. Factors protecting against a decline in physical activity during the COVID-19 pandemic. Med. Sci. Sports Exerc. 2021, 53, 1391–1399. [Google Scholar] [CrossRef] [PubMed]
- Gallè, F.; Sabella, E.A.; Ferracuti, S.; De Giglio, O.; Caggiano, G.; Protano, C.; Valeriani, F.; Parisi, E.A.; Valerio, G.; Liguori, G.; et al. Sedentary behaviors and physical activity of Italian undergraduate students during lockdown at the time of COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6171. [Google Scholar] [CrossRef] [PubMed]
- Gildner, T.E.; Laugier, E.J.; Thayer, Z.M. Exercise routine change is associated with prenatal depression scores during the COVID-19 pandemic among pregnant women across the United States. PLoS ONE 2021, 15, e0243188. [Google Scholar] [CrossRef]
- Ingram, J.; Maciejewski, G.; Hand, C.J. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front. Psychol. 2020, 11, 588604. [Google Scholar] [CrossRef] [PubMed]
- Jacob, L.; Tully, M.A.; Barnett, Y.; Lopez-Sanchez, G.F.; Butler, L.; Schuch, F.; Lopez-Bueno, R.; McDermott, D.; Firth, J.; Grabovac, I.; et al. The relationship between physical activity and mental health in a sample of the UK public: A cross-sectional study during the implementation of COVID-19 social distancing measures. Ment. Health Phys. Act. 2020, 19, 100345. [Google Scholar] [CrossRef] [PubMed]
- Karuc, J.; Soric, M.; Radman, I.; Misigoj-Durakovic, M. Moderators of change in physical activity levels during restrictions due to COVID-19 pandemic in young urban adults. Sustainability 2020, 12, 6392. [Google Scholar] [CrossRef]
- Katewongsa, P.; Widyastari, D.A.; Saonuam, P.; Haemathulin, N.; Wongsingha, N. The effects of the COVID-19 pandemic on the physical activity of the Thai population: Evidence from Thailand’s Surveillance on Physical Activity 2020. J. Sport Health Sci. 2020, 10, 341–348. [Google Scholar] [CrossRef]
- Kaur, H.; Singh, T.; Arya, Y.K.; Mittal, S. Physical fitness and exercise during the COVID-19 pandemic: A qualitative enquiry. Front. Psychol. 2020, 11, 590172. [Google Scholar] [CrossRef]
- Kaushal, N.; Keith, N.; Aguiñaga, S.; Hagger, M.S. Social cognition and socioecological predictors of home-based physical activity intentions, planning, and habits during the COVID-19 pandemic. Behav. Sci. 2020, 10, 133. [Google Scholar] [CrossRef]
- Khan, A.H.; Sultana, M.S.; Hossain, S.; Hasan, M.T.; Ahmed, H.U.; Sikder, M.T. The impact of COVID-19 pandemic on mental health and wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. J. Affect. Disord. 2020, 277, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Knell, G.; Robertson, M.C.; Dooley, E.E.; Burford, K.; Mendez, K.S. Health behavior changes during COVID-19 pandemic and subsequent “stay-at-home” orders. Int. J. Environ. Res. Public Health 2020, 17, 6268. [Google Scholar] [CrossRef] [PubMed]
- Lebel, C.; MacKinnon, A.; Bagshawe, M.; Tomfohr-Madsen, L.; Giesbrecht, G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect Disord. 2020, 277, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Lesser, I.A.; Nienhuis, C.P. The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef] [PubMed]
- Limbers, C.A.; McCollum, C.; Greenwood, E. Physical activity moderates the association between parenting stress and quality of life in working mothers during the COVID-19 pandemic. Ment. Health Phys. Act. 2020, 19, 100358. [Google Scholar] [CrossRef]
- Lin, J.Y.; Guo, T.Y.; Becker, B.; Yu, Q.; Chen, S.T.; Brendon, S.; Hossain, M.M.; Cunha, P.M.; Soares, F.C.; Veronese, N.; et al. Depression is associated with moderate-intensity physical activity among college students during the COVID-19 pandemic: Differs by activity level, gender and gender role. Psychol. Res. Behav. Manag. 2020, 13, 1123–1134. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Bueno, R.; Calatayud, J.; Andersen, L.L.; Balsalobre-Fernandez, C.; Casana, J.; Casajus, J.A.; Smith, L.; Lopez-Sanchez, G.F. Immediate impact of the COVID-19 confinement on physical activity levels in Spanish adults. Sustainability 2020, 12, 5708. [Google Scholar] [CrossRef]
- Lopez-Bueno, R.; Calatayud, J.; Ezzatvar, Y.; Casajus, J.A.; Smith, L.; Andersen, L.L.; Lopez-Sanchez, G.F. Association between current physical activity and current perceived anxiety and mood in the initial phase of COVID-19 confinement. Front. Psychiatry 2020, 11, 729. [Google Scholar] [CrossRef]
- Luciano, F.; Cenacchi, V.; Vegro, V.; Pavei, G. COVID-19 lockdown: Physical activity, sedentary behaviour and sleep in Italian medicine students. Eur. J. Sport Sci. 2020, 21, 1459–1468. [Google Scholar] [CrossRef]
- Maher, J.P.; Hevel, D.J.; Reifsteck, E.J.; Drollette, E.S. Physical activity is positively associated with college students’ positive affect regardless of stressful life events during the COVID-19 pandemic. Psychol. Sport Exerc. 2021, 52, 101826. [Google Scholar] [CrossRef]
- Martinez, E.Z.; Silva, F.M.; Morigi, T.Z.; Zucoloto, M.L.; Silva, T.L.; Joaquim, A.G.; Dall’Agnol, G.; Galdino, G.; Martinez, M.O.Z.; da Silva, W.R. Physical activity in periods of social distancing due to COVID-19: A cross-sectional survey. Ciencia Saude Coletiva 2020, 25, 4157–4168. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef] [PubMed]
- McDowell, C.P.; Herring, M.P.; Lansing, J.; Brower, C.; Meyer, J.D. Working from home and job loss due to the COVID-19 pandemic are associated with greater time in sedentary behaviors. Front. Public Health 2020, 8, 597619. [Google Scholar] [CrossRef] [PubMed]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef] [PubMed]
- Munekawa, C.; Hosomi, Y.; Hashimoto, Y.; Okamura, T.; Takahashi, F.; Kawano, R.; Nakajima, H.; Osaka, T.; Okada, H.; Majima, S.; et al. Effect of coronavirus disease 2019 pandemic on the lifestyle and glycemic control in patients with type 2 diabetes: A cross-section and retrospective cohort study. Endocr. J. 2020, 68, 201–210. [Google Scholar] [CrossRef]
- Nienhuis, C.P.; Lesser, I.A. The impact of COVID-19 on women’s physical activity behavior and mental well-being. Int. J. Environ. Res. Public Health 2020, 17, 9036. [Google Scholar] [CrossRef] [PubMed]
- Oliva, J.L.; Johnston, K.L. Puppy love in the time of Corona: Dog ownership protects against loneliness for those living alone during the COVID-19 lockdown. Int. J. Soc. Psychiatry 2021, 67, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, F.; Cansel, N.; Kizilay, F.; Guldogan, E.; Ucuz, I.; Sinanoglu, B.; Colak, C.; Cumurcu, H.B. The role of physical activity on mental health and quality of life during COVID-19 outbreak: A cross-sectional study. Eur. J. Integr. Med. 2020, 40, 101248. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.E.; Islam, M.S.; Bishwas, M.S.; Moonajilin, S.; Gozal, D. Physical inactivity and sedentary behaviors in the Bangladeshi population during the COVID-19 pandemic: An online cross-sectional survey. Heliyon 2020, 6, e05392. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Olavarría, D.; Latorre-Román, P.Á.; Guzmán-Guzmán, I.P.; Jerez-Mayorga, D.; Caamaño-Navarrete, F.; Delgado-Floody, P. Positive and negative changes in food habits, physical activity patterns, and weight status during COVID-19 confinement: Associated factors in the Chilean population. Int. J. Environ. Res. Public. Health 2020, 17, 5431. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Liu, S.; Lithopoulos, A.; Garcia-Barrera, M.A.; Zhang, C.Q.; Garcia-Barrera, M.A. Correlates of Perceived Physical Activity Transitions during the COVID-19 Pandemic among Canadian Adults. Appl. Psychol. Health Well Being 2020, 12, 1157–1182. [Google Scholar] [CrossRef]
- Richardson, D.L.; Duncan, M.J.; Clarke, N.D.; Myers, T.D.; Tallis, J. The influence of COVID-19 measures in the United Kingdom on physical activity levels, perceived physical function and mood in older adults: A survey-based observational study. J. Sports Sci. 2021, 39, 887–899. [Google Scholar] [CrossRef]
- Robinson, E.; Boyland, E.; Chisholm, A.; Harrold, J.; Maloney, N.G.; Marty, L.; Mead, B.R.; Noonan, R.; Hardman, C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite 2021, 156, 104853. [Google Scholar] [CrossRef]
- Rogers, N.T.; Waterlow, N.R.; Brindle, H.; Enria, L.; Eggo, R.M.; Lees, S.; Roberts, C.H. Behavioral change towards reduced intensity physical activity is disproportionately prevalent among adults with serious health issues or self-perception of high risk during the UK COVID-19 lockdown. Front. Public Health 2020, 8, 575091. [Google Scholar] [CrossRef]
- Rogowska, A.M.; Pavlova, I.; Kusnierz, C.; Ochnik, D.; Bodnar, I.; Petrytsa, P. Does physical activity matter for the mental health of university students during the COVID-19 pandemic? J. Clin. Med. 2020, 9, 3494. [Google Scholar] [CrossRef] [PubMed]
- Romero-Blanco, C.; Rodríguez-Almagro, J.; Onieva-Zafra, M.D.; Parra-Fernández, M.L.; Prado-Laguna, M.D.C.; Hernández-Martínez, A. Physical activity and sedentary lifestyle in university students: Changes during confinement due to the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6567. [Google Scholar] [CrossRef] [PubMed]
- Rossinot, H.; Fantin, R.; Venne, J. Behavioral changes during COVID-19 confinement in France: A web-based study. Int. J. Environ. Res. Public Health 2020, 17, 8444. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.R.B.; Seguro, C.S.; de Oliveira, C.G.A.; Santos, P.O.S.; de Oliveira, J.C.M.; de Souza, L.F.M.; de Paula, C.A.; Gentil, P.; Rebelo, A.C.S. Physical inactivity is associated with increased levels of anxiety, depression, and stress in Brazilians during the COVID-19 pandemic: A cross-sectional study. Front. Psychiatry 2020, 11, 565291. [Google Scholar] [CrossRef]
- Smith, L.; Jacob, L.; Butler, L.; Schuch, F.; Barnett, Y.; Grabovac, I.; Veronese, N.; Caperchione, C.; Lopez-Sanchez, G.F.; Meyer, J.; et al. Prevalence and correlates of physical activity in a sample of UK adults observing social distancing during the COVID-19 pandemic. BMJ Open Sport Exerc. Med. 2020, 6, e000850. [Google Scholar] [CrossRef]
- Spence, J.C.; Rhodes, R.E.; McCurdy, A.; Mangan, A.; Hopkins, D.; Mummery, W.K. Determinants of physical activity among adults in the United Kingdom during the COVID-19 pandemic: The DUK-COVID study. Br. J. Health Psychol. 2021, 26, 588–605. [Google Scholar] [CrossRef]
- Stephan, Y.; Terracciano, A.; Luchetti, M.; Aschwen, D.; Lee, J.H.; Sesker, A.A.; Strickhouser, J.E.; Sutin, A.R. Physical activity and sedentary behavior during COVID-19: Trajectory and moderation by personality. Soc. Psychol. Personal Sci. 2020, 12, 1103–1109. [Google Scholar] [CrossRef]
- Suzuki, Y.; Maeda, N.; Hirado, D.; Shirakawa, T.; Urabe, Y. Physical activity changes and its risk factors among community-dwelling Japanese older adults during the COVID-19 epidemic: Associations with subjective well-being and health-related quality of life. Int. J. Environ. Res. Public Health 2020, 17, 6591. [Google Scholar] [CrossRef]
- Weaver, R.H.; Jackson, A.; Lanigan, J.; Power, T.G.; Anderson, A.; Cox, A.E.; Eddy, L.; Parker, L.; Sano, Y.; Weybright, E. Health behaviors at the onset of the COVID-19 pandemic. Am. J. Health Beha 2021, 45, 44–61. [Google Scholar] [CrossRef]
- Werneck, A.O.; Silva, D.R.; Malta, D.C.; Lima, M.G.; Souza-Júnior, P.R.B.; Azevedo, L.O.; Barros, M.B.A.; Szwarcwald, C.L. The mediation role of sleep quality in the association between the incidence of unhealthy movement behaviors during the COVID-19 quarantine and mental health. Sleep Med. 2020, 76, 10–15. [Google Scholar] [CrossRef]
- Yang, Y.; Koenigstorfer, J. Determinants of physical activity maintenance during the Covid-19 pandemic: A focus on fitness apps. Transl. Behav. Med. 2020, 10, 835–842. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
- World Health Organization. Motion for your mind: Physical Activity for Mental Health Promotion, Protection and Care. Available online: https://www.euro.who.int/__data/assets/pdf_file/0018/403182/WHO-Motion-for-your-mind-ENG.pdf (accessed on 10 April 2021).
- Caputo, E.L.; Reichert, F.F. Studies of physical activity and COVID-19 during the pandemic: A scoping review. J. Phys. Act. Health 2020, 17, 1275–1284. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.; Martin, B.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- O’Donoghue, G.; Perchoux, C.; Mensah, K.; Lakerveld, J.; van der Ploeg, H.; Bernaards, C.; Chastin, S.F.; Simon, C.; O’Gorman, D.; Nazare, J.A. A systematic review of correlates of sedentary behaviour in adults aged 18–65 years: A socio-ecological approach. BMC Public Health 2016, 16, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Connell, S.E.; Griffiths, P.L.; Clemes, S.A. Seasonal variation in physical activity, sedentary behaviour and sleep in a sample of UK adults. Ann. Hum. Biol. 2014, 41, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; Chaput, J.P.; Giangregorio, L.M.; Janssen, I.; Saunders, T.J.; Kho, M.E.; Poitras, V.J.; Tomasone, J.R.; El-Kotob, R.; McLaughlin, E.C.; et al. Canadian 24-Hour Movement Guidelines for Adults aged 18-64 years and Adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 2020, 45 (Suppl. 2), S57–S102. [Google Scholar] [CrossRef]
- Boulton, E.R.; Horne, M.; Todd, C. Multiple influences on participating in physical activity in older age: Developing a social ecological approach. Health Expect. 2018, 21, 239–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Devereux-Fitzgerald, A.; Powell, R.; Dewhurst, A.; French, D.P. The acceptability of physical activity interventions to older adults: A systematic review and meta-synthesis. Soc. Sci. Med. 2016, 158, 14–23. [Google Scholar] [CrossRef] [PubMed]
- French, D.P.; Olander, E.K.; Chisholm, A.; Mc Sharry, J. Which behaviour change techniques are most effective at increasing older adults’ self-efficacy and physical activity behaviour? A systematic review. Ann. Behav. Med. 2014, 48, 225–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. CMAJ 2006, 174, 801–809. [Google Scholar] [CrossRef] [Green Version]
- Prince, S.A.; Cardilli, L.; Reed, J.L.; Saunders, T.J.; Kite, C.; Douillette, K.; Fournier, K.; Buckley, J.P. A comparison of self-reported and device measured sedentary behaviour in adults: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act 2020, 17, 31. [Google Scholar] [CrossRef]

| Variable | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population or participants and condition or interest | Adults aged 18 years or older Any sex/gender Not restricted to the UK | Studies including children and adolescents (aged less than 18 years) |
| Intervention or exposures | Exposure to the COVID-19 pandemic, containment, and mitigation strategies | Studies that involve non-COVID-19 related pandemics, such as SARS or MERS |
| Comparison or control groups | No restrictions | |
| Outcomes of interest | Data/information, qualitative or quantitative, relating to correlates of PA and/or sedentary time/behaviour during the COVID-19 pandemic | No data relating to the pandemic phase or restrictions in place available Studies only including empirical data on volume of or changes in volume of PA or sedentary time/behaviour Data pooled from multiple different countries |
| Setting | Any community setting | |
| Study designs | Any randomized, non-randomized, qualitative, or mixed methods study design providing original results | Studies not providing original results, such as systematic reviews, meta-analysis, general reviews, or editorials |
| Number of Studies | ||
|---|---|---|
| Country of study | Australia | 1 [62] |
| Austria | 1 [64] | |
| Bangladesh | 2 [46,65] | |
| Belgium | 1 [33] | |
| Brazil | 3 [56,74,80] | |
| Canada | 5 [32,48,49,61,67] | |
| Chile | 1 [66] | |
| China | 1 [51] | |
| Croatia | 1 [42] | |
| France | 1 [73] | |
| Ghana | 1 [21] | |
| Hungary | 1 [18] | |
| Japan | 2 [60,78] | |
| Jordan | 1 [19] | |
| KSA | 1 [22] | |
| India | 1 [44] | |
| Italy | 5 [25,31,38,54,57] | |
| Northern Cyprus | 1 [23] | |
| Spain | 8 [20,26,27,28,29,52,53,72] | |
| Taiwan | 1 [30] | |
| Thailand | 1 [43] | |
| Turkey | 1 [63] | |
| United Kingdom | 9 [24,36,40,41,68,69,70,75,76] | |
| Ukraine | 1 [71] | |
| USA | 13 [34,35,37,39,45,47,50,55,58,59,77,79,81] | |
| Study design | Observational | |
| Cross-sectional | 59 [18,19,20,21,22,23,24,25,26,27,28,30,31,32,33,34,35,36,37,38,40,41,42,43,45,46,47,48,49,50,51,52,53,54,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,73,74,75,76,77,78,79,80,81] | |
| Longitudinal | 4 [29,39,55,72] | |
| Phenomenological | 1 [44] | |
| Correlated behaviour | Physical activity | 64 [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81] |
| Sedentary behaviour | ||
| Active breaks | 1 [66] | |
| Screen time | 5 [19,32,58,59,80] | |
| Sitting time | 11 [18,24,26,54,58,59,65,68,72,77,79] | |
| Sedentary time | 4 [21,28,51,81] | |
| Primary COVID-19 restrictions | Stay-at-home order | 47 [18,19,20,21,22,23,24,25,26,27,28,29,31,34,35,36,38,40,41,42,43,44,45,46,51,52,53,54,55,56,57,60,62,63,64,65,68,69,70,71,72,73,74,75,76,78,80] |
| Social distancing | 4 [30,58,59,66] | |
| Varied by state/region | 12 [32,37,39,47,48,49,50,61,67,77,79,81] | |
| Lockdown light | 1 [33] | |
| Overall study quality | * | 1 [77] |
| ** | 10 [31,55,56,57,59,60,71,73,74,75] | |
| *** | 29 [19,21,22,24,25,27,29,30,32,33,35,37,39,40,41,43,46,58,61,63,64,65,66,68,70,72,76,79,81] | |
| **** | 21 [18,20,23,26,28,34,38,42,45,47,48,49,50,51,52,53,54,67,69,78,80] | |
| ***** | 3 [36,44,62] | |
| Framework Theme | Theme | COM-B Component |
|---|---|---|
| Individual (biological) | General health | Capability (physical) |
| Individual (psychological) | Mental health | Capability (psychological) |
| Individual (psychological) | Motivation | Motivation (automatic) |
| Individual (psychological) | Cognitions | Capability (psychological) |
| Individual (psychological) | Behaviour | Motivation (reflexive) |
| Social | Sociodemographic factors | Opportunity (physical) |
| Social | Support | Opportunity (social) |
| Social | Domestic situation | Opportunity (social) |
| Social | Lifestyle choices | Capability (psychological) |
| Environment | Resources | Opportunity (physical) |
| Environment | Area of residence | Opportunity (physical) |
| Policy | COVID-19 related factors | Opportunity (physical) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knight, R.L.; McNarry, M.A.; Sheeran, L.; Runacres, A.W.; Thatcher, R.; Shelley, J.; Mackintosh, K.A., on behalf of the Welsh Institute of Physical Activity, Health, and Sport (WIPAHS). Moving Forward: Understanding Correlates of Physical Activity and Sedentary Behaviour during COVID-19—An Integrative Review and Socioecological Approach. Int. J. Environ. Res. Public Health 2021, 18, 10910. https://doi.org/10.3390/ijerph182010910
Knight RL, McNarry MA, Sheeran L, Runacres AW, Thatcher R, Shelley J, Mackintosh KA on behalf of the Welsh Institute of Physical Activity, Health, and Sport (WIPAHS). Moving Forward: Understanding Correlates of Physical Activity and Sedentary Behaviour during COVID-19—An Integrative Review and Socioecological Approach. International Journal of Environmental Research and Public Health. 2021; 18(20):10910. https://doi.org/10.3390/ijerph182010910
Chicago/Turabian StyleKnight, Rachel L., Melitta A. McNarry, Liba Sheeran, Adam W. Runacres, Rhys Thatcher, James Shelley, and Kelly A. Mackintosh on behalf of the Welsh Institute of Physical Activity, Health, and Sport (WIPAHS). 2021. "Moving Forward: Understanding Correlates of Physical Activity and Sedentary Behaviour during COVID-19—An Integrative Review and Socioecological Approach" International Journal of Environmental Research and Public Health 18, no. 20: 10910. https://doi.org/10.3390/ijerph182010910
APA StyleKnight, R. L., McNarry, M. A., Sheeran, L., Runacres, A. W., Thatcher, R., Shelley, J., & Mackintosh, K. A., on behalf of the Welsh Institute of Physical Activity, Health, and Sport (WIPAHS). (2021). Moving Forward: Understanding Correlates of Physical Activity and Sedentary Behaviour during COVID-19—An Integrative Review and Socioecological Approach. International Journal of Environmental Research and Public Health, 18(20), 10910. https://doi.org/10.3390/ijerph182010910








