Inequalities in Mortality and Access to Hospital Care for Cervical Cancer—An Ecological Study
Abstract
:1. Background
2. Method
2.1. Data Source
2.2. Procedure for Collecting Data
Deaths from Cervical Cancer
- -
- Access to mortality data was based on the following sequence within the DATASUS system:
- Vital statistics;
- Mortality between 2000 and 2012;
- General mortality;
- Geographical coverage.
- -
- The deaths related to each code were extracted and stratified according to the following variables:
- Age group (from 25 to 64 years, divided into 5-year ranges);
- Location (administrative regions);
- Year (2000 to 2012).
2.3. Resident Population
- Demographic and socioeconomic data;
- Resident population data;
- Censuses (1980, 1991, 2000, and 2010), Count (1996), and intercensorial projections (1981 to 2012) according to age, sex, and domiciliary situation;
- Geographical coverage.
2.4. Cervical Cancer Mortality
2.5. Hospital Admissions for Cervical Cancer
- Region;
- Morbidity list code CID-10 (malignant neoplasm of the cervix);
- Age group.
2.6. Data Analysis
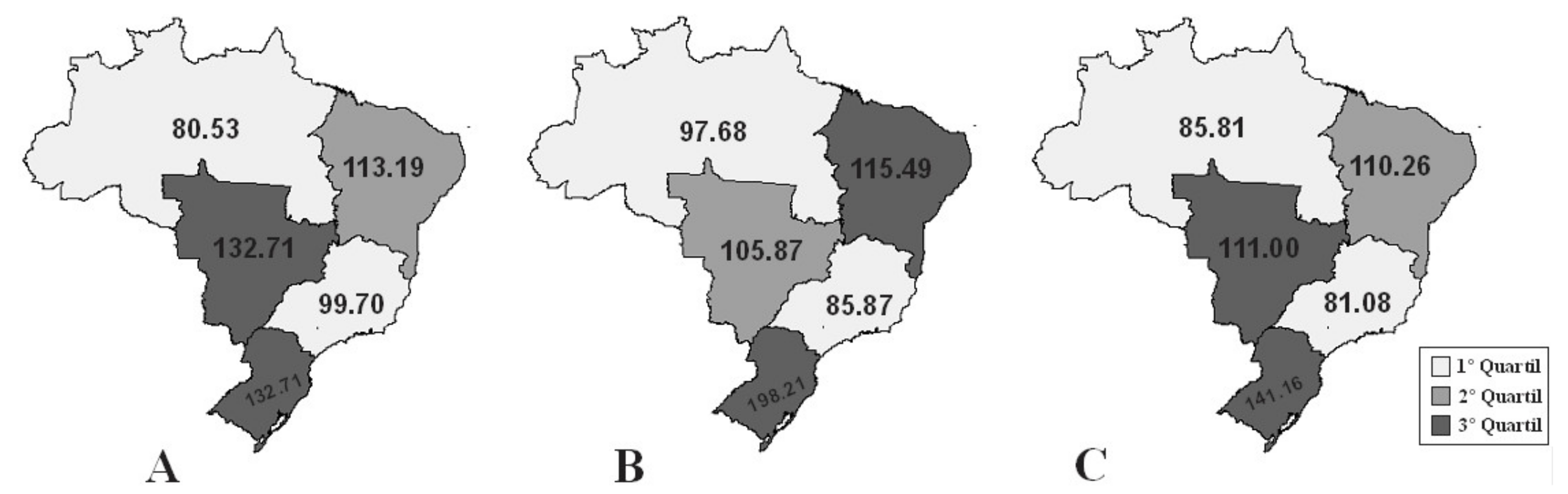
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CC | Cervical cancer |
| CACON | Complexity in Oncology Center |
| SIM | Information system |
| DATASUS | Data from the Department of Informatics of the Unified Health System |
| ICD | International Classification of Diseases |
| IBGE | Brazilian Institute of Geography and Statistics |
| IAH | Hospital Information System (SIH), Hospital Inpatient Authorization |
References
- Castro, E.K.D.; Peuker, A.C.; Lawrenz, P.; Figueiras, M.J. Illness perception, knowledge and self-care about cervical cancer. Psicol. Reflexão Crítica 2015, 28, 483–489. [Google Scholar] [CrossRef] [Green Version]
- Parada, R.; de Assis, M.; da Silva, R.C.F.; Abreu, M.F.; da Silva, M.A.F.; Dias, M.B.K.; Tomazelli, J.G. A Política Nacional de Atenção Oncológica e o papel da Atenção Básica na prevenção e controle do câncer. Rev. APS 2008, 11, 199–206. [Google Scholar]
- Amaral, R.G.; Ribeiro, A.A.; Miranda, F.A.; Tavares, S.; Souza, N.L.A.; Manrique, E.J.C.; Albuquerque, Z.B.P.d.; Fonsechi-Carvasan, G.A. Fatores que podem comprometer a qualidade dos exames citopatológicos no rastreamento do câncer do colo do útero. Rev. Bras. Anal. Clin. 2006, 38, 3–6. [Google Scholar]
- Brasil Ministério da Saúde. DATASUS. Sistema de Informação de Mortalidade (SIM) [Internet]. [Citado 20 December 2017]. 2008. Available online: http://tabnet.datasus.gov.br/cgi/idb2006/matriz.htm (accessed on 20 December 2018).
- Instituto Nacional de Câncer José Alencar Gomes da Silva. Coordenação de Prevenção e Vigilância. Divisão de Detecção Precoce e Apoio à Organização de Rede. In Diretrizes Brasileiras Para o Rastreamento do Câncer do Colo do Útero, 2nd ed.; INCA: Rio de Janeiro, Brasil, 2016. [Google Scholar]
- Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Análise de Situação de Saúde. Plano de Ações Estratégicas Para o Enfrentamento das Doenças Crônicas Não Transmissíveis (DCNT) No Brasil 2011–2022; Ministério da Saúde: Brasília, Brasil, 2011; p. 148.
- Thuler, L.C.S. Mortality due to cancer of the uterine cervix in Brazil. Rev. Bras. Ginecol. Obs. 2008, 30, 216–218. [Google Scholar]
- Da Sousa, L.V.; da Paiva, L.; da Figueiredo, F.W.S.; da Almeida, T.C.C.; Oliveira, F.R.; Adami, F. Trends in Stroke-Related Mortality in the ABC Region, São Paulo, Brazil: An Ecological Study Between 1997 and 2012. Open Cardiovasc. Med. J. 2017, 11, 111. [Google Scholar] [CrossRef] [Green Version]
- Ministério da saúde do Brasil. Coordenação Geral de Informações Sobre Mortalidade; Sistema de Informações Sobre Mortalidade–SIM. Consolidação da Base de Dados de 2011; Ministério da Saúde do Brasil: Brasília, Brasil, 2013; pp. 1–12.
- Rebelo, P.A.P.; Paiva, F.F.S.; Sousa, A.F. Registro Hospitalar de Câncer–Relatório Anual 1994–1998; Instituto Nacional do Câncer, Ministério da Saúde, Instituto Nacional de Câncer: Rio de Janeiro, Brasil, 2004.
- Ahmad, O.B.; Boschi-Pinto, C.; Lopez, A.D.; Murray, C.J.; Lozano, R.; Inoue, M. Age standardization of rates: A new who standard. Geneva World Health Organ. 2001, 9, 1–14. [Google Scholar]
- Allin, S.; Masseria, C.; Mossialos, E. Measuring socioeconomic differences in use of health care services by wealth versus by income. Am. J. Public Health 2009, 99, 1849–1855. [Google Scholar] [CrossRef] [PubMed]
- De Sousa-Muñoz, R.L.; Formiga, M.Y.Q.; Silva, A.E.V.F.; Silva, M.B.d.L.; Vieira, R.C.; Galdino, M.M.; de Morais, M.T.M. Hospitalizações por Neoplasias em Idosos no Âmbito do Sistema Único de Saúde na Paraíba, Brasil. Saúde e Pesqui. 2015, 8, 479–491. [Google Scholar] [CrossRef]
- Instituto Nacional de Câncer. Plano de Ação Para Redução da Incidência e Mortalidade por Câncer do Colo do Útero; (Sumário Executivo); INCA: Rio de Janeiro, Brasil, 2010; p. 40. [Google Scholar]
- Cancer Control: Knowledge into Action: WHO Guide for Effective. Available online: https://pubmed.ncbi.nlm.nih.gov/24716263/ (accessed on 12 April 2019).
- Barbosa, I.R.; de Souza, D.L.B.; Bernal, M.M.; Costa, I.d.C.C. Desigualdades regionais na mortalidade por câncer de colo de útero no Brasil: Tendências e projeções até o ano 2030. Ciência Saúde Coletiva 2016, 21, 253–262. [Google Scholar] [CrossRef] [Green Version]
- Girianelli, V.R.; Gamarra, C.J.; Azevedo, E.S.G. Os grandes contrastes na mortalidade por câncer do colo uterino e de mama no Brasil. Rev. Saude Publica 2014, 48, 459–467. [Google Scholar] [CrossRef] [Green Version]
- Rico, A.M.; Iriart, J.A.B. “Tem mulher, tem preventivo”: Sentidos das práticas preventivas do câncer do colo do útero entre mulheres de Salvador, Bahia, Brasil. Cad. Saúde Pública Rio Jan. 2013, 29, 1763–1773. [Google Scholar] [CrossRef]
- Coimbra, C.; Manuela, C.; Teixeria, L.A. As campanhas educativas contra o câncer. História Ciências Saúde-Manguinhos 2010, 17, 223–241. [Google Scholar]
- Saslow, D.; Castle, P.E.; Cox, J.T.; Davey, D.D.; Einstein, M.H.; Ferris, D.G.; Goldie, S.J.; Harper, D.M.; Kinney, W.; Moscicki, A.-B.; et al. American Cancer Society Guideline for human papillomavirus (HPV) vaccine use to prevent cervical cancer and its precursors. CA Cancer J. Clin. 2007, 57, 7–28. [Google Scholar] [CrossRef] [Green Version]
- De Sousa, A.M.V.; Teixeira, C.C.A.; Medeiros, S.d.; Nunes, S.J.C.; Salvador, P.T.C.d.; de Barros, R.M.B.; de Lima, F.F.S.; Nascimento, G.G.C.d.; Santos, J.d.; de Souza, D.L.B.; et al. Mortalidade por câncer do colo do útero no estado do Rio Grande do Norte, no período de 1996 a 2010: Tendência temporal e projeções até 2030. Epidemiol. Serviços Saúde 2016, 25, 311–322. [Google Scholar]
- Corrêa, D.A.D.; Villela, W.V. O controle do câncer do colo do útero: Desafios para implementação de ações programáticas no Amazonas, Brasil. Rev. Bras. Saúde Matern. Infant. 2008, 8, 491–497. [Google Scholar] [CrossRef] [Green Version]
- Navarro, C.; da Fonseca, A.J.; Sibajev, A.; Souza, C.I.d.; Araújo, D.S.; Teles, D.A.d.; de Carvalho, S.G.L.; Cavalcante, K.W.M.; Rabelo, W.L. Cervical cancer screening coverage in a high-incidence region. Rev. Saude Publica 2015, 49, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nartey, Y.; Hill, P.; Amo-Antwi, K.; Nyarko, K.; Yarney, J.; Cox, B. Characteristics of Women Diagnosed with Invasive Cervical Cancer in Ghana. Asian Pac. J. Cancer Prev. 2018, 19, 357–363. [Google Scholar] [CrossRef]
- Nartey, Y.; Hill, P.C.; Amo-Antwi, K.; Nyarko, K.M.; Yarney, J.; Cox, B. Factors Contributing to the Low Survival Among Women With a Diagnosis of Invasive Cervical Cancer in Ghana. Int. J. Gynecol. Cancer 2017, 27, 1926–1934. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.B.R. Câncer do Colo do Útero No Município de São Gonçalo, RJ: Tendência da Mortalidade e Caracterização Epidemiológica das Neoplasias Intra-Epiteliais Cervicais. Fundação Oswaldo Cruz. Escola Nacional de Saúde Pública Sergio Arouca. Ph.D. Thesis, Escola Nacional de Saúde Pública Sergio Arouca, Rio de Janeiro, Brasil, 2008. [Google Scholar]
- De Albuquerque, M.V.; Viana, A.L.d.; de Lima, L.D.; Ferreira, M.P.; Fusaro, E.R.; Iozzi, F.L. Desigualdades regionais na saúde: Mudanças observadas no Brasil de 2000 a 2016. Ciência Saúde Coletiva 2017, 22, 1055–1064. [Google Scholar] [CrossRef] [Green Version]
- Guerra, M.R.; Bustamante-Teixeira, M.T.; Corrêa, C.S.L.; de Abreu, D.M.X.; Curado, M.P.; Naghavi, M.M.M.; Teixeira, R.; França, E.B.; Malta, D.C. Magnitude e variação da carga da mortalidade por câncer no Brasil e Unidades da Federação, 1990 e 2015. Rev. BRas Epidemiol. 2017, 20, 102–115. [Google Scholar] [CrossRef]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, S.G.D.; Carvalho, C.P.A.L.D.; Silva, R.S.D.; Oliveira, C.M.D.; Bonfim, C.V.D. Decline of mortality from cervical cancer. Rev. Bras. Enferm. 2018, 71, 585–590. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, S.D.A.; Machado, M.D.F.A.S.; Sampaio, N.M.V. Motivos que levam mulheres a não retornarem para receber o resultado de exame Papanicolau. Rev. Lat. -Am. Enferm. 2006, 14, 503–509. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Country Regions | Deaths (n) | Age-Standardized Mortality (95% CI) | Hospital Admissions | Age-Standardized Admissions (95% CI) | Proportional Mortality (95% CI) |
|---|---|---|---|---|---|
| Age group (years) * | |||||
| North | |||||
| 25–29 | 177 | 2.09 (2.08 to 2.09) | 797 | 9.45 (9.44 to 9.46) | 3.55 (3.46 to 3.64) |
| 30–34 | 375 | 5.22 (5.21 to 5.23) | 1587 | 22.10 (22.08 to 22.11) | 7.12 (6.94 to 7.29) |
| 35–39 | 496 | 8.24 (8.23 to 8.24) | 2299 | 38.21 (38.18 to 38.25) | 8.89 (8.68 to 9.10) |
| 40–44 | 677 | 13.59 (13.58 to 13.60) | 2909 | 58.42 (58.37 to 58.48) | 10.61 (10.38 to 10.84) |
| 45–49 | 770 | 19.24 (19.23 to 19.26) | 2616 | 65.36 (65.29 to 65.42) | 9.61 (9.42 to 9.80) |
| 50–54 | 704 | 22.62 (22.60 to 22.64) | 1718 | 55.22 (55.15 to 55.29) | 7.61 (7.48 to 7.75) |
| 55–59 | 617 | 25.37 (25.34 to 25.40) | 1221 | 50.22 (50.15 to 50.29) | 6.19 (6.08 to 6.30) |
| 60–64 | 529 | 28.47 (28.42 to 28.51) | 918 | 49.41 (49.34 to 49.49) | 4.92 (4.84 to 5.01) |
| Northeast | |||||
| 25–29 | 347 | 1.21 (1.21 to 2.65) | 3595 | 12.55 (12.54 to 12.56) | 2.59 (2.55 to 2.62) |
| 30–34 | 679 | 2.66 (2.65 to 2.66) | 7206 | 28.23 (28.21 to 28.24) | 4.43 (4.37 to 4.49) |
| 35–39 | 1083 | 4.81 (4.80 to 4.82) | 12,255 | 54.50 (54.48 to 54.52) | 5.85 (5.78 to 5.93) |
| 40–44 | 1422 | 7.22 (7.21 to 7.22) | 16,134 | 82.02 (81.98 to 82.05) | 6.00 (5.93 to 6.07) |
| 45–49 | 1783 | 10.63 (10.62 to 10.64) | 15,222 | 90.81 (90.77 to 90.85) | 5.96 (5.90 to 6.01) |
| 50–54 | 1719 | 12.28 (12.28 to 12.29) | 9402 | 67.18 (67.14 to 67.22) | 4.91 (4.86 to 4.96) |
| 55–59 | 1683 | 14.54 (14.53 to 14.55) | 6004 | 51.88 (51.86 to 51.90) | 4.31 (4.27 to 4.34) |
| 60–64 | 1549 | 15.73 (15.72 to 15.73) | 4887 | 49.64 (49.61 to 49.67) | 3.33 (3.30 to 3.36) |
| Southeast | |||||
| 25–29 | 363 | 0.81 (0.80 to 0.81) | 5508 | 12.37 (12.37 to 12.37) | 1.61 (1.59 to 1.62) |
| 30–34 | 772 | 1.82 (1.81 to 1.83) | 9593 | 22.70 (22.69 to 22.71) | 2.71 (2.68 to 2.73) |
| 35–39 | 1244 | 3.13 (3.13 to 3.14) | 14,480 | 36.46 (36.44 to 36.47) | 3.36 (3.33 to 3.38) |
| 40–44 | 1961 | 5.35 (5.34 to 5.35) | 20,572 | 56.13 (56.11 to 56.14) | 3.83 (3.80 to 3.86) |
| 45–49 | 2460 | 7.56 (7.55 to 7.57) | 21,140 | 64.99 (64.97 to 65.01) | 3.67 (3.64 to 3.70) |
| 50–54 | 2576 | 9.43 (9.42 to 9.43) | 15,212 | 55.70 (55.67 to 55.72) | 3.33 (3.31 to 3.34) |
| 55–59 | 2380 | 10.99 (10.98 to 10.99) | 10,837 | 55.05 (50.02 to 50.08) | 2.91 (2.89 to 2.91) |
| 60–64 | 2242 | 12.70 (12.69 to 12.71) | 9223 | 52.27 (52.24 to 52.30) | 2.57 (2.55 to 2.58) |
| South | |||||
| 25–29 | 208 | 1.43 (1.42 to 1.43) | 4341 | 29.93 (29.91 to 29.95) | 2.60 (2.55 to 2.66) |
| 30–34 | 414 | 2.96 (2.95 to 2.97) | 6679 | 47.81 (47.78 to 47.84) | 4.39 (4.31 to 4.47) |
| 35–39 | 715 | 5.29 (5.28 to 5.29) | 9998 | 73.98 (73.95 to 74.01) | 5.53 (5.44 to 5.61) |
| 40–44 | 893 | 7.10 (7.09 to 7.10) | 14,092 | 112.17 (112.11 to 112.23) | 5.24 (5.18 to 5.30) |
| 45–49 | 1115 | 9.90 (9.89 to 9.90) | 15,274 | 135.64 (135.57 to 135.71) | 4.95 (4.89 to 5.00) |
| 50–54 | 1073 | 11.45 (11.44 to 11.45) | 9969 | 106.41 (106.35 to 106.48) | 4.02 (3.99 to 4.05) |
| 55–59 | 996 | 13.19 (13.18 to 13.19) | 5722 | 75.83 (75.77 to 75.88) | 3.36 (3.34 to 3.39) |
| 60–64 | 898 | 14.75 (14.73 to 14.76) | 4390 | 72.14 (72.08 to 72.19) | 2.76 (2.73 to 2.78) |
| Central-West | |||||
| 25–29 | 101 | 1.26 (1.26 to 1.27) | 1155 | 14.41 (14.41 to 14.41) | 2.40 (2.33 to 2.47) |
| 30–34 | 211 | 2.82 (2.81 to 2.82) | 2167 | 29.02 (28.99 to 29.04) | 3.99 (3.89 to 4.08) |
| 35–39 | 310 | 4.65 (4.64 to 4.66) | 3503 | 52.58 (52.55 to 52.61) | 4.56 (4.47 to 4.66) |
| 40–44 | 429 | 7.50 (7.49 to 7.50) | 4706 | 82.33 (82.26 to 82.40) | 5.43 (5.32 to 5.54) |
| 45–49 | 546 | 11.55 (11.53 to 11.57) | 4255 | 90.02 (89.94 to 90.10) | 5.41 (5.32 to 5.51) |
| 50–54 | 511 | 13.72 (13.70 to 13.73) | 2565 | 68.87 (68.81 to 68.93) | 4.39 (4.32 to 4.46) |
| 55–59 | 467 | 16.30 (16.28 to 16.32) | 1555 | 54.29 (54.23 to 54.35) | 3.76 (3.71 to 3.82) |
| 60–64 | 397 | 17.93 (17.90 to 17.96) | 1269 | 57.33 (57.25 to 57.41) | 3.06 (3.02 to 3.10) |
| Brazil | |||||
| 25–29 | 1196 | 1.14 (1.13 to 1.15) | 15,396 | 14.79 (14.79 to 14.79) | 2.40 (2.39 to 2.42) |
| 30–34 | 2451 | 2.54 (2.53 to 2.54) | 27,232 | 28.25 (28.24 to 28.25) | 3.99 (3.96 to 4.02) |
| 35–39 | 3848 | 4.35 (4.34 to 4.36) | 42,535 | 48.12 (48.11 to 48.13) | 4.57 (4.54 to 4.59) |
| 40–44 | 5382 | 6.76 (6.75 to 6.76) | 58,413 | 73.40 (73.38 to 73.41) | 5.43 (5.40 to 5.45) |
| 45–49 | 6674 | 9.63 (9.63 to 9.64) | 58,507 | 84.45 (84.44 to 84.47) | 5.41 (5.38 to 5.43) |
| 50–54 | 6583 | 11.44 (11.43 to 11.45) | 38,866 | 67.58 (67.56 to 67.60) | 4.40 (4.38 to 4.41) |
| 55–59 | 6143 | 13.33 (13.32 to 13.33) | 25,339 | 55.01 (55.00 to 55.03) | 3.77 (3.75 to 3.78) |
| 60–64 | 5615 | 14.91 (14.90 to 14.91) | 20,687 | 54.95 (54.94 to 54.97) | 3.07 (3.06 to 3.08) |
| Country Regions | Linear Regression Mortality | Linear Regression Admissions | ||||
|---|---|---|---|---|---|---|
| β | p * | r2 | β | p * | r2 | |
| Age group (years) * | ||||||
| North | ||||||
| 25–29 | 0.03 | 0.38 | 0.07 | −0.27 | 0.135 | 0.19 |
| 30–34 | 0.12 | 0.148 | 0.18 | −0.72 | 0.025 | 0.37 |
| 35–39 | 0.17 | 0.229 | 0.12 | −2.14 | 0.001 | 0.63 |
| 40–44 | 0.44 | 0.036 | 0.34 | −2.45 | 0.026 | 0.38 |
| 45–49 | 0.83 | 0.015 | 0.43 | −2.58 | 0.031 | 0.36 |
| 50–54 | 0.28 | 0.246 | 0.12 | 0.09 | 0.926 | 0.01 |
| 55–59 | 0.80 | 0.071 | 0.26 | 1.23 | 0.108 | 0.21 |
| 60–64 | 0.67 | 0.014 | 0.43 | 1.71 | 0.072 | 0.26 |
| Northeast | ||||||
| 25–29 | 0.05 | 0.031 | 0.35 | −0.05 | 0.838 | 0.01 |
| 30–34 | 0.11 | 0.001 | 0.64 | −0.56 | 0.193 | 0.15 |
| 35–39 | 0.12 | 0.039 | 0.33 | −1.64 | 0.048 | 0.30 |
| 40–44 | 0.05 | 0.241 | 0.12 | −2.30 | 0.078 | 0.26 |
| 45–49 | 0.19 | 0.007 | 0.49 | −2.56 | 0.124 | 0.20 |
| 50–54 | 0.23 | 0.150 | 0.17 | −2.06 | 0.046 | 0.31 |
| 55–59 | 0.38 | 0.014 | 0.43 | −1.20 | 0.060 | 0.29 |
| 60–64 | 0.29 | 0.011 | 0.46 | −1.13 | 0.059 | 0.28 |
| Southeast | ||||||
| 25–29 | 0.01 | 0.088 | 0.24 | −0.08 | 0.692 | 0.02 |
| 30–34 | 0.03 | 0.108 | 0.22 | −0.40 | 0.027 | 0.37 |
| 35–39 | −0.03 | 0.191 | 0.15 | −1.62 | <0.001 | 0.89 |
| 40–44 | −0.12 | 0.001 | 0.65 | −3.23 | <0.001 | 0.94 |
| 45–49 | −0.26 | <0.001 | 0.72 | −4.03 | <0.001 | 0.88 |
| 50–54 | −0.30 | 0.007 | 0.49 | −2.95 | <0.001 | 0.82 |
| 55–59 | −0.38 | <0.001 | 0.81 | −2.33 | <0.001 | 0.78 |
| 60–64 | −0.56 | <0.001 | 0.85 | −2.31 | <0.001 | 0.84 |
| South | ||||||
| 25–29 | 0.03 | 0.350 | 0.08 | −0.34 | 0.656 | 0.02 |
| 30–34 | 0.01 | 0.836 | 0.04 | −0.44 | 0.546 | 0.03 |
| 35–39 | −0.01 | 0.894 | 0.01 | −2.21 | 0.066 | 0.27 |
| 40–44 | −0.28 | 0.001 | 0.62 | −5.90 | 0.024 | 0.38 |
| 45–49 | −0.49 | <0.001 | 0.84 | −8.87 | 0.025 | 0.37 |
| 50–54 | −0.59 | 0.001 | 0.63 | −6.26 | 0.045 | 0.32 |
| 55–59 | −0.53 | 0.001 | 0.68 | −3.89 | 0.014 | 0.44 |
| 60–64 | −0.39 | 0.003 | 0.56 | −1.43 | 0.236 | 0.12 |
| Central-west | ||||||
| 25–29 | −0.01 | 0.814 | 0.01 | −0.47 | 0.008 | 0.48 |
| 30–34 | 0.10 | 0.088 | 0.24 | −1.37 | <0.001 | 0.80 |
| 35–39 | 0.08 | 0.188 | 0.15 | −3.15 | <0.001 | 0.79 |
| 40–44 | −0.02 | 0.790 | 0.01 | −4.55 | 0.001 | 0.68 |
| 45–49 | −0.22 | 0.381 | 0.07 | −6.07 | <0.001 | 0.79 |
| 50–54 | −0.11 | 0.650 | 0.01 | −3.21 | <0.001 | 0.85 |
| 55–59 | −0.36 | 0.131 | 0.19 | −1.82 | 0.004 | 0.54 |
| 60–64 | −0.36 | 0.333 | 0.08 | −1.12 | 0.159 | 0.18 |
| Brazil | ||||||
| 25–29 | 0.03 | 0.006 | 0.50 | −0.16 | 0.505 | 0.04 |
| 30–34 | 0.06 | 0.001 | 0.64 | −0.58 | 0.047 | 0.31 |
| 35–39 | 0.03 | 0.115 | 0.21 | −1.89 | <0.001 | 0.71 |
| 40–44 | −0.05 | 0.092 | 0.23 | −3.43 | 0.001 | 0.68 |
| 45–49 | −0.11 | 0.087 | 0.24 | −4.49 | 0.001 | 0.63 |
| 50–54 | −0.16 | 0.023 | 0.39 | −3.14 | 0.003 | 0.57 |
| 55–59 | −0.15 | 0.050 | 0.31 | −2.08 | 0.002 | 0.60 |
| 60–64 | −0.24 | 0.001 | 0.66 | −1.57 | 0.001 | 0.64 |
| Brazil/Regions | Age-Standardized Mortality * (95% CI) by Cervical Cancer † (×100,000 Inhabitants) | Linear Regression | ||||||||||||||
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | β | p | r2 | |
| North | 4.09 (4.08; 4.10) | 5.20 (5.19; 5.20) | 6.28 (6.27; 6.29) | 6.21 (6.21; 6.22) | 7.32 (7.31; 7.33) | 7.07 (7.06; 7.08) | 7.40 (7.39; 7.41) | 5.84 (5.83; 5.85) | 7.22 (7.21; 7.22) | 7.38 (7.37; 7.38) | 6.88 (6.87; 6.88) | 6.93 (6.92; 6.93) | 7.39 (7.38; 7.39) | 0.18 | 0.008 | 0.48 |
| Northeast | 2.85 (2.84; 2.86) | 3.10 (3.09; 3.10) | 3.40 (3.39; 3.40) | 3.28 (3.27; 3.29) | 3.61 (3.60; 3.61) | 3.92 (3.92; 3.93) | 4.07 (4.06; 4.07) | 3.75 (3.74; 3.75) | 3.84 (3.83; 3.84) | 4.00 (3.99; 4.00) | 3.62 (3.61; 3.62) | 3.73 (3.72; 3.74) | 4.12 (4.12; 4.13) | 0.07 | 0.002 | 0.61 |
| Southeast | 3.17 (3.16; 3.17) | 3.21 (3.21; 3.22) | 2.97 (2.96; 2.97) | 3.04 (3.04; 3.05) | 3.28 (3.27; 3.28) | 2.83 (2.82; 2.83) | 2.69 (2.69; 2.70) | 2.46 (2.46; 2.47) | 2.44 (2.44; 2.45) | 2.37 (2.36; 2.37) | 2.47 (2.46; 2.48) | 2.51 (2.51; 2.52) | 2.41 (2.41; 2.42) | −0.07 | <0.001 | 0.79 |
| South | 4.03 (4.02; 4.04) | 4.62 (4.61; 4.62) | 3.95 (3.95; 3.96) | 4.08 (4.08; 4.09) | 3.99 (3.98; 3.99) | 3.78 (3.78; 3.79) | 3.59 (3.58; 3.59) | 3.14 (3.13; 3.15) | 3.27 (3.26; 3.28) | 3.10 (3.09; 3.10) | 3.02 (3.01; 3.02) | 3.14 (3.13; 3.14) | 3.25 (3.25; 3.25) | −0.11 | <0.001 | 0.79 |
| Central-west | 4.03 (4.02; 4.04) | 3.81 (3.80; 3.81) | 3.50 (3.49; 3.51) | 4.57 (4.57; 4.58) | 4.61 (4.61; 4.61) | 4.68 (4.67; 4.69) | 4.53 (4.53; 4.54) | 3.89 (3.89; 3.90) | 3.81 (3.81; 3.81) | 3.89 (3.89; 3.89) | 4.04 (4.03; 4.05) | 3.49 (3.48; 3.49) | 3.59 (3.58; 3.59) | −0.03 | 0.270 | 0.10 |
| Brazil | 3.34 (3.33; 3.35) | 3.57 (3.57; 3.58) | 3.45 (3.45; 3.45) | 3.55 (3.55; 3.56) | 3.78 (3.77; 3.78) | 3.62 (3.61; 3.63) | 3.56 (3.55; 3.56) | 3.17 (3.17; 3.17) | 3.29 (3.29; 3.30) | 3.28 (3.27; 3.28) | 3.22 (3.21; 3.23) | 3.26 (3.25; 3.26) | 3.36 (3.35; 3.37) | −0.02 | 0.065 | 0.27 |
| Brazil/Regions | Age-Standardized Incidence * (95% CI) of Hospital Admissions for Cervical Câncer (× 100,000 Inhabitants) | Linear Regression | ||||||||||||||
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | β | p | r2 | |
| North | 17.56 (17.54; 17.58) | 18.32 (18.29; 18.35) | 20.39 (20.37; 20.41) | 24.03 (24.01; 24.06) | 28.24 (28.20; 28.280 | 25.64 (25.61; 25.68) | 22.51 (22.49; 22.53) | 22.03 (22.01; 22.06) | 20.02 (19.99; 20.04) | 18.36 (18.35; 18.37) | 15.49 (15.47; 15.50) | 15.99 (15.98; 16.01) | 16.13 (16.12; 16.14) | −0.42 | 0.157 | 0.17 |
| Northeast | 24.60 (24.59; 24.61) | 21.37 (21.36; 21.39) | 29.20 (29.19; 29.21) | 37.77 (37.75; 37.80) | 32.87 (32.86; 32.89) | 27.79 (27.77; 27.81) | 29.22 (29.21; 29.23) | 26.10 (26.08; 26.11) | 25.70 (25.68; 25.71) | 23.51 (23.49; 23.53) | 20.72 (20.71; 20.73) | 20.34 (20.32; 20.35) | 20.33 (20.32; 20.35) | −0.67 | 0.080 | 0.25 |
| Southeast | 24.08 (24.06; 24.09) | 24.16 (24.15; 24.18) | 26.24 (26.23; 26.25) | 25.18 (25.16; 25.19) | 22.59 (22.57; 22.60) | 22.84 (22.82; 22.85) | 21.94 (21.94; 21.95) | 19.00 (18.99; 19.00) | 17.10 (17.09; 17.10) | 16.41 (16.40; 16.42) | 16.93 (16.93; 16.94) | 15.04 (15.04; 15.05) | 15.62 (15.61; 15.62) | −0.95 | <0.001 | 0.88 |
| South | 33.98 (33.95; 34.01) | 30.81 (30.79; 30.84) | 53.69 (53.65; 53.73) | 54.81 (54.76; 54.86) | 53.45 (53.40; 53.50) | 55.37 (55.32; 55.42) | 50.34 (50.30; 50.37) | 40.54 (40.51; 40.57) | 31.93 (31.90; 31.95) | 29.82 (29.79; 29.84) | 28.32 (28.29; 28,35) | 26.45 (26.44; 26.46) | 24.78 (24.76; 24.79) | −1.43 | 0.236 | 0.12 |
| Central-west | 36.96 (36.92; 37.00) | 36.72 (36.67; 36.77) | 28.04 (28.00; 28.08) | 31.21 (31.24; 31.24) | 28.38 (28.34; 28.41) | 27.09 (27.06; 27.13) | 29.31 (29.27; 29.34) | 22.09 (22.06; 22.11) | 24.13 (24.10; 24.15) | 24.99 (24.97; 25.02) | 22.70 (22.67; 22.72) | 20.17 (20.15; 20.19) | 19.34 (19.32; 19.36) | −1.33 | <0.001 | 0.84 |
| Brazil | 26.31 (26.30; 26.32) | 25.07 (25.06; 25.07) | 31.16 (31.15; 31.17) | 33.36 (33.35; 33.38) | 30.75 (30.74; 30.75 | 29.65 (29.64; 29.65) | 28,74 (28.74; 28.75) | 24.51 (24.50; 24.52) | 22.20 (22.19; 22.20) | 20.97 (20.97; 20.97) | 19.90 (19.89; 19.90) | 18.54 (18.53; 18.54) | 18.48 (18.48; 18.48) | −1.01 | 0.002 | 0.59 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sousa, L.V.d.A.; Maciel, E.d.S.; da Silva Paiva, L.; Alcantara, S.d.S.A.; Nascimento, V.B.d.; Fonseca, F.L.A.; Adami, F. Inequalities in Mortality and Access to Hospital Care for Cervical Cancer—An Ecological Study. Int. J. Environ. Res. Public Health 2021, 18, 10966. https://doi.org/10.3390/ijerph182010966
Sousa LVdA, Maciel EdS, da Silva Paiva L, Alcantara SdSA, Nascimento VBd, Fonseca FLA, Adami F. Inequalities in Mortality and Access to Hospital Care for Cervical Cancer—An Ecological Study. International Journal of Environmental Research and Public Health. 2021; 18(20):10966. https://doi.org/10.3390/ijerph182010966
Chicago/Turabian StyleSousa, Luiz Vinicius de Alcantara, Erika da Silva Maciel, Laércio da Silva Paiva, Stefanie de Sousa Antunes Alcantara, Vânia Barbosa do Nascimento, Fernando Luiz Affonso Fonseca, and Fernando Adami. 2021. "Inequalities in Mortality and Access to Hospital Care for Cervical Cancer—An Ecological Study" International Journal of Environmental Research and Public Health 18, no. 20: 10966. https://doi.org/10.3390/ijerph182010966






