Social Capital and COVID-19 Deaths: An Ecological Analysis in Japan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Measures
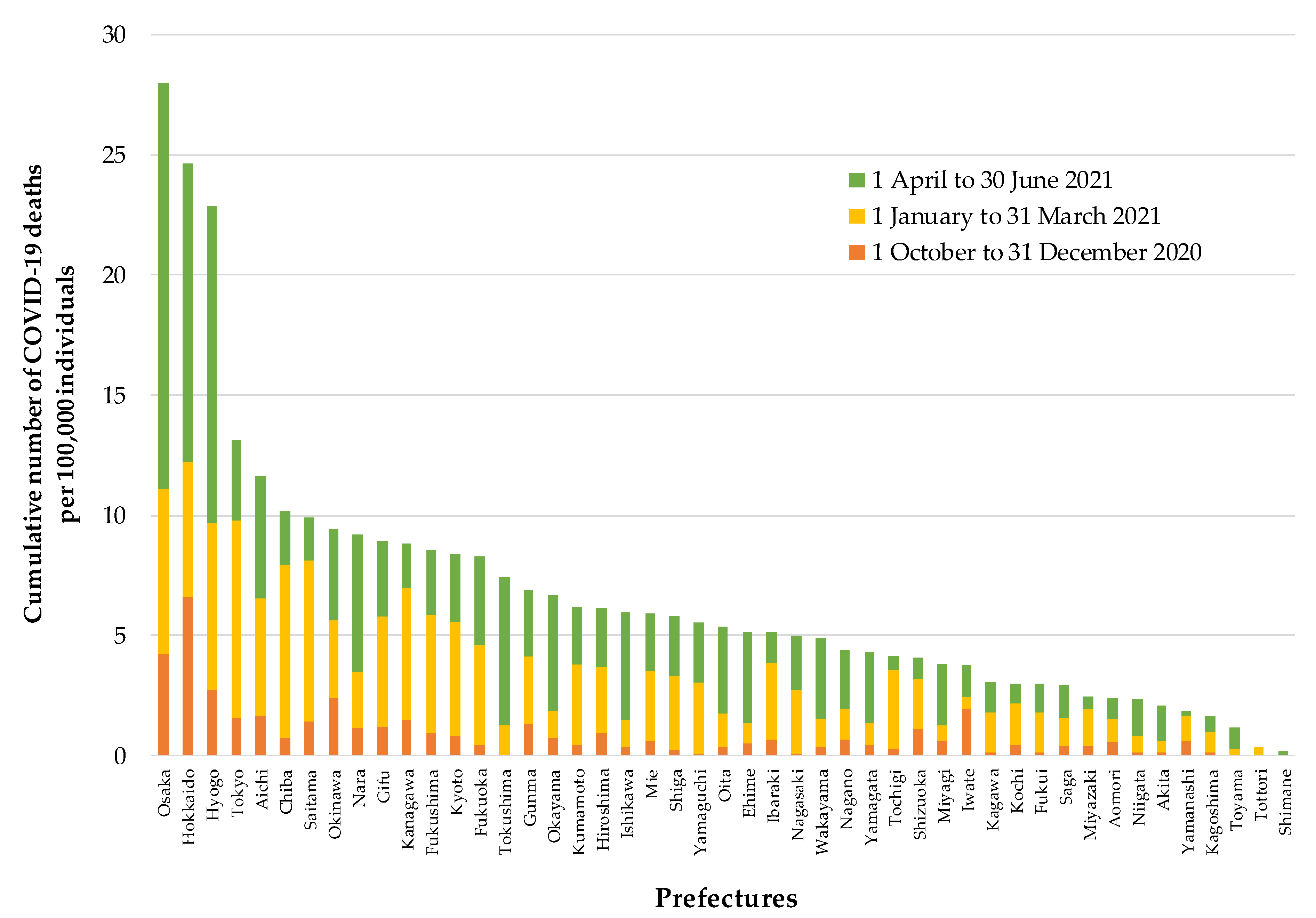
2.2.1. Death by COVID-19
2.2.2. Social Capital
2.2.3. Covariates
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johns Hopkins Coronavirus Resource Center. COVID-19 Map. Available online: https://coronavirus.jhu.edu/map.html (accessed on 1 September 2021).
- Du, P.; Li, D.; Wang, A.; Shen, S.; Ma, Z.; Li, X. A Systematic Review and Meta-Analysis of Risk Factors Associated with Severity and Death in COVID-19 Patients. Can. J. Infect. Dis. Med. Microbiol. 2021, 2021, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Guerrero, L.R.; Wallace, S.P. The Impact of COVID-19 on Diverse Older Adults and Health Equity in the United States. Front. Public Health 2021, 9, 661592. [Google Scholar] [CrossRef] [PubMed]
- Prats-Uribe, A.; Xie, J.; Prieto-Alhambra, D.; Petersen, I. Smoking and COVID-19 infection and related mortality: A prospective cohort analysis of UK Biobank data. Clin. Epidemiol. 2021, 13, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Gesesew, H.A.; Koye, D.N.; Fetene, D.M.; Woldegiorgis, M.; Kinfu, Y.; Geleto, A.B.; Melaku, Y.A.; Mohammed, H.; Alene, K.A.; Awoke, M.A.; et al. Risk factors for COVID-19 infection, disease severity and related deaths in Africa: A systematic review. BMJ Open 2021, 11, e044618. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef]
- Kastora, S.; Kounidas, G.; Perrott, S.; Carter, B.; Hewitt, J.; Myint, P.K. Clinical frailty scale as a point of care prognostic indicator of mortality in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 2021, 36, 100896. [Google Scholar] [CrossRef] [PubMed]
- James, N.; Menzies, M. Trends in COVID-19 prevalence and mortality: A year in review. Phys. D. Nonlinear Phenom. 2021, 425, 132968. [Google Scholar] [CrossRef]
- Elsayed, H.H.; Hassaballa, A.S.; Ahmed, T.A.; Gumaa, M.; Sharkawy, H.Y.; Moharram, A.A. Variation in outcome of invasive mechanical ventilation between different countries for patients with severe COVID-19: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0252760. [Google Scholar] [CrossRef] [PubMed]
- Putnam, R.D. Making Democracy Work: Civic Traditions in Modern Italy; Princeton University Press: Princeton, NJ, USA, 1993. [Google Scholar]
- Kawachi, I.; Berkman, L.F. Social Capital, Social Cohesion, and Health. In Social Epidemiology, 2nd ed.; Berkman, L.F., Kawachi, I., Glymour, M.M., Eds.; Oxford University Press: New York, NY, USA, 2014; pp. 290–319. [Google Scholar]
- Aldrich, D.P.; Meyer, M.A. Social Capital and Community Resilience. Am. Behav. Sci. 2015, 59, 254–269. [Google Scholar] [CrossRef]
- Makridis, C.A.; Wu, C. How social capital helps communities weather the COVID-19 pandemic. PLoS ONE 2021, 16, e0245135. [Google Scholar]
- Yanagisawa, M.; Kawachi, I.; Scannell, C.A.; Oronce, C.I.A.; Tsugawa, Y. Association between county-level social capital and the burden of COVID-19 cases and deaths in the United States. Ann. Epidemiol. 2021, 59, 21–23. [Google Scholar] [CrossRef]
- Arachchi, J.I.; Managi, S. The role of social capital in COVID-19 deaths. BMC Public Health 2021, 21, 1–9. [Google Scholar] [CrossRef]
- Borgonovi, F.; Andrieu, E.; Subramanian, S. The evolution of the association between community level social capital and COVID-19 deaths and hospitalizations in the United States. Soc. Sci. Med. 2021, 278, 113948. [Google Scholar] [CrossRef] [PubMed]
- Elgar, F.J.; Stefaniak, A.; Wohl, M.J.A. The trouble with trust: Time-series analysis of social capital, income inequality, and COVID-19 deaths in 84 countries. Soc. Sci. Med. 2020, 263, 113365. [Google Scholar] [CrossRef] [PubMed]
- Fraser, T.; Aldrich, D.P.; Page-Tan, C. Bowling alone or distancing together? The role of social capital in excess death rates from COVID19. Soc. Sci. Med. 2021, 284, 114241. [Google Scholar] [CrossRef]
- Bartscher, A.K.; Seitz, S.; Siegloch, S.; Slotwinski, M.; Wehrhöfer, N. Social capital and the spread of covid-19: Insights from european countries. J. Health Econ. 2021, 80, 102531. [Google Scholar] [CrossRef] [PubMed]
- Story, W.T.; Glanville, J.L. Comparing the association between social capital and self-rated health in poor and affluent nations. SSM-Popul. Health 2019, 9, 100508. [Google Scholar] [CrossRef]
- Islam, M.K.; Merlo, J.; Kawachi, I.; Lindström, M.; Gerdtham, U.-G. Social capital and health: Does egalitarianism matter? A literature review. Int. J. Equity Health 2006, 5, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakane, C. Japanese Society; University of California Press: Los Angeles, CA, USA, 1970. [Google Scholar]
- Yamagishi, T.; Cook, K.S.; Watabe, M. Uncertainty, Trust, and Commitment Formation in the United States and Japan. Am. J. Sociol. 1998, 104, 165–194. [Google Scholar] [CrossRef]
- Yamagishi, T.; Yamagishi, M. Trust and commitment in the United States and Japan. Motiv. Emot. 1994, 18, 129–166. [Google Scholar] [CrossRef]
- Ministry of Health, Labour, and Welfare. Visualizing the Data: Information on COVID-19 Infections. Available online: https://covid19.mhlw.go.jp/en/ (accessed on 1 September 2021).
- Statistics Bureau. Population Estimates. Available online: https://www.stat.go.jp/english/data/jinsui/index.html (accessed on 1 September 2021).
- Ministry of Health, Labour, and Welfare. Basic Survey on Wage Structure. Available online: https://www.mhlw.go.jp/toukei/list/chinginkouzou.html (accessed on 1 September 2021).
- Ministry of Health, Labour, and Welfare. Hospital Report. Available online: https://www.mhlw.go.jp/toukei/list/80-1.html (accessed on 1 September 2021).
- Ministry of Health, Labour, and Welfare. Comprehensive Survey of Living Conditions 2016. Available online: https://www.mhlw.go.jp/english/database/db-hss/cslc-report2016.html (accessed on 1 September 2021).
- Feter, N.; Caputo, E.; Doring, I.; Leite, J.; Cassuriaga, J.; Reichert, F.; da Silva, M.; Coombes, J.; Rombaldi, A. Sharp increase in depression and anxiety among Brazilian adults during the COVID-19 pandemic: Findings from the PAMPA cohort. Public Health 2021, 190, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Maffly-Kipp, J.; Eisenbeck, N.; Carreno, D.F.; Hicks, J. Mental health inequalities increase as a function of COVID-19 pandemic severity levels. Soc. Sci. Med. 2021, 285, 114275. [Google Scholar] [CrossRef]
- Blair, R.A.; Morse, B.S.; Tsai, L.L. Public health and public trust: Survey evidence from the Ebola Virus Disease epidemic in Liberia. Soc. Sci. Med. 2017, 172, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Vinck, P.; Pham, P.N.; Bindu, K.K.; Bedford, J.; Nilles, E. Institutional trust and misinformation in the response to the 2018–19 Ebola outbreak in North Kivu, DR Congo: A population-based survey. Lancet Infect. Dis. 2019, 19, 529–536. [Google Scholar] [CrossRef] [Green Version]
- Gotanda, H.; Miyawaki, A.; Tabuchi, T.; Tsugawa, Y. Association between trust in government and practice of preventive measures during the COVID-19 pandemic in Japan. J. Gen. Intern. Med. 2021, in press. [Google Scholar] [CrossRef]
- The Asahi Shimbun. Survey: Suga Cabinet Approval Rating Sinks to Record Low of 31% (19 July 2021). Available online: https://www.asahi.com/ajw/articles/14398503 (accessed on 1 September 2021).
- Zmerli, S. Social capital and norms of citizenship: An ambiguous relationship? Am. Behav. Sci. 2010, 53, 657–676. [Google Scholar] [CrossRef]
- Putnam, R.D. Bowling Alone: The Collapse and Revival of American Community; Simon & Schuster: New York, NY, USA, 2000. [Google Scholar]
| Author, Year | Data (Analytic Sample) | Outcome | Social Capital Variable | Findings |
|---|---|---|---|---|
| Borgonovi et al., 2021 [16] | United States (2284 counties) | Death cases | Relational social capital | ↓ |
| Cognitive social capital | ↓ (early period)/↑ (middle/late period) | |||
| Fraser et al., 2021 [18] | United States (947 counties) | Excess death cases | Bonding social capital | ↓ (early period) |
| Bridging social capital | ↓ (middle period)/↑ (late period) | |||
| Linking social capital | ↓ (middle period) | |||
| Makridis & Wu, 2021 [13] | United States (over 2700 counties) | Death cases | Aggregated indicator (including social trust, community cohesion, volunteerism, facility interaction and investment, etc.) | ↓ |
| Yanagisawa et al., 2021 [14] | United States (nationwide counties; no description on the number) | Death cases | Social/emotional support | ↓ |
| Engagement in voluntary organizations | No association | |||
| Civic engagement | ↑ (only on voter turnout) | |||
| Bartscher et al., 2020 [19] | European nations (over 800 areas from four countries) | Excess death cases | Voter turnout | ↓ |
| Elgar et al., 2021 [17] | Worldwide (84 countries) | Death cases | Social trust | ↑ |
| Group affiliation | ↑ | |||
| Civic engagement | ↓ | |||
| Confidence in institution | ↓ | |||
| Imbulana Arachchi & Managi, 2021 [15] | Worldwide (29 countries and 265 province/state from eight countries) | Death cases | Community attachment | ↑ |
| Social trust | ↑ | |||
| Family bond | ↓ | |||
| Neighborhood security | ↓ |
| Variable | Mean ± SD (Min–Max; Median) | Pearson’s r | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| a | b | c | d | e | f | g | h | i | ||
| a. Trust in neighbors (%) | 65.9 ± 2.9 (61.1–72.5; 65.4) | 0.759 * | 0.349 * | 0.365 * | 0.235 | 0.353 * | −0.349 * | −0.042 | 0.210 | |
| b. Norm of reciprocity in the neighborhood (%) | 56.2 ± 3.2 (51.1–63.7; 55.5) | 0.457 * | 0.403 * | 0.035 | 0.394 * | −0.397* | −0.181 | 0.226 | ||
| c. Trust in the national government (%) | 44.3 ± 3.3 (37.4–53.7; 44.2) | 0.297 * | 0.091 | 0.348 * | −0.227 | −0.175 | 0.287 | |||
| d. Neighborhood ties (%) | 12.3 ± 2.7 (7.3–18.6; 12.3) | 0.542 * | 0.440 * | −0.422 * | −0.211 | 0.181 | ||||
| e. Social participation (%) | 23.9 ± 2.7 (17.9–29.5; 24.0) | 0.115 | −0.078 | −0.160 | 0.088 | |||||
| f. Proportion of people aged ≥65 years (%) | 30.5 ± 3.1 (22.2–37.3; 30.8) | −0.609 * | −0.184 | 0.633 * | ||||||
| g. Population density (persons/km2) | 656.2 ± 1216.5 (66.9–6354.8; 265.9) | 0.395 * | −0.417 * | |||||||
| h. Average monthly income (thousand yen) | 280.5 ± 27.8 (239–379; 280.6) | −0.135 | ||||||||
| i. Number of hospital beds (per 100,000 individuals) | 1398.6 ± 360.8 (805–2508; 1366) | |||||||||
| Variable | Category | COVID-19 Deaths from 1 October to 31 December 2020 | COVID-19 Deaths from 1 January to 31 March 2021 | COVID-19 Deaths from 1 April to 30 June 2021 |
|---|---|---|---|---|
| b (95% CI) | b (95% CI) | b (95% CI) | ||
| Trust in neighbors | 1st tertile (low) | Reference | Reference | Reference |
| 2nd tertile (middle) | 0.09 (−0.79, 0.98) | 0.28 (−1.06, 1.62) | 0.93 (−1.55, 3.40) | |
| 3rd tertile (high) | −0.65 (−1.54, 0.25) | −0.66 (−2.00, 0.69) | −1.15 (−3.64, 1.34) | |
| Norm of reciprocity | 1st tertile (low) | Reference | Reference | Reference |
| 2nd tertile (middle) | −0.89 (−17.60, −0.19) | −0.38 (−1.70, 0.94) | −1.64 (−4.13, 0.86) | |
| 3rd tertile (high) | −1.10 (−2.03, −0.17) | −1.43 (−2.84, −0.03) | −2.54 (−5.20, −0.02) | |
| Trust in the national government | 1st tertile (low) | Reference | Reference | Reference |
| 2nd tertile (middle) | −0.29 (−1.16, 0.58) | −1.24 (−2.53, −0.05) | 1.09 (−1.38, 3.57) | |
| 3rd tertile (high) | −0.84 (−1.73, −0.04) | −1.20 (−2.51, −0.01) | −0.73 (−3.24, 1.79) | |
| Neighborhood ties | 1st tertile (low) | Reference | Reference | Reference |
| 2nd tertile (middle) | −0.28 (−1.21, 0.64) | −0.56 (−1.87, 0.75) | 1.74 (−0.83, 4.31) | |
| 3rd tertile (high) | −0.81 (−1.71, 0.10) | −1.23 (−3.01, 0.45) | −0.33 (−2.85, 2.19) | |
| Social participation | 1st tertile (low) | Reference | Reference | Reference |
| 2nd tertile (middle) | −0.72 (−1.60, 0.17) | −0.83 (−2.15, 0.48) | −0.22 (−2.77, 2.33) | |
| 3rd tertile (high) | −0.53 (−1.43, 0.38) | −1.18 (−2.53, 0.16) | −0.57 (−3.18, 2.03) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murayama, H.; Nakamoto, I.; Tabuchi, T. Social Capital and COVID-19 Deaths: An Ecological Analysis in Japan. Int. J. Environ. Res. Public Health 2021, 18, 10982. https://doi.org/10.3390/ijerph182010982
Murayama H, Nakamoto I, Tabuchi T. Social Capital and COVID-19 Deaths: An Ecological Analysis in Japan. International Journal of Environmental Research and Public Health. 2021; 18(20):10982. https://doi.org/10.3390/ijerph182010982
Chicago/Turabian StyleMurayama, Hiroshi, Isuzu Nakamoto, and Takahiro Tabuchi. 2021. "Social Capital and COVID-19 Deaths: An Ecological Analysis in Japan" International Journal of Environmental Research and Public Health 18, no. 20: 10982. https://doi.org/10.3390/ijerph182010982
APA StyleMurayama, H., Nakamoto, I., & Tabuchi, T. (2021). Social Capital and COVID-19 Deaths: An Ecological Analysis in Japan. International Journal of Environmental Research and Public Health, 18(20), 10982. https://doi.org/10.3390/ijerph182010982







