Latent Class Analysis of Obesogenic Behaviors among Korean Adolescents: Associations with Weight-Related Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Data and Participants
2.2. Measures
2.2.1. Obesogenic Behaviors
2.2.2. Predictors of LCM
2.2.3. Weight-Related Outcomes
2.3. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Multiple-Group LCA
3.3. Sex-Specific LCMs of Obesogenic Behaviors in Korean Adolescents
3.4. Predictors of LCM
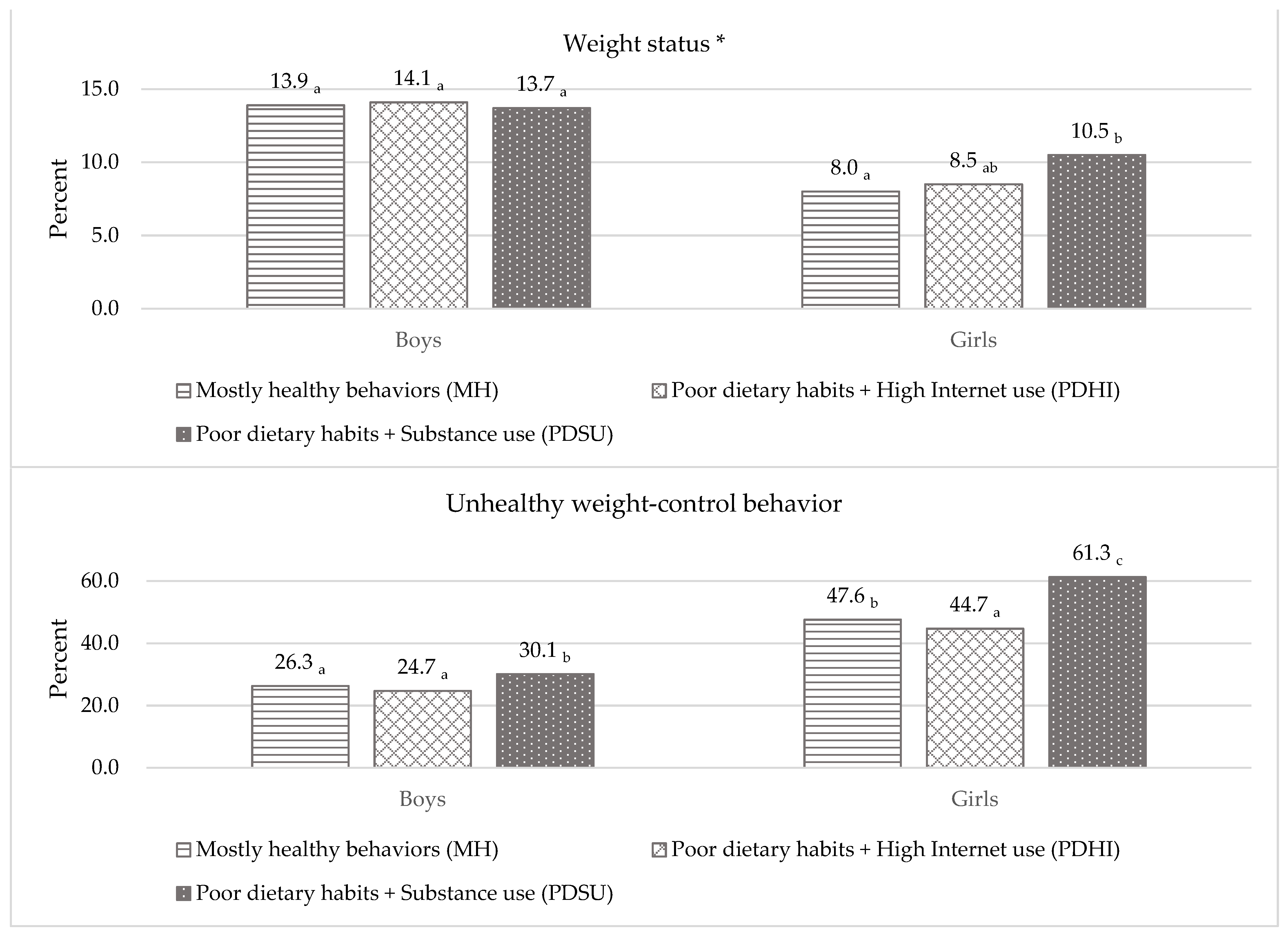
3.5. Class Difference in Weight-Related Outcomes
4. Discussion
4.1. Sex-Specific LCMs of Obesogenic Behaviors
4.2. Predictors of Latent Class Membership
4.3. Class Difference in Weight-Related Outcomes
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Dietz, W.H. Critical periods in childhood for the development of obesity. Am. J. Clin. Nutr. 1994, 59, 955–959. [Google Scholar] [CrossRef]
- Non-communicable Disease Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Fryar, C.D.; Carroll, M.D.; Afful, J. Prevalence of Overweight, Obesity, and Severe Obesity among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 through 2017–2018. Available online: https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/overweight-obesity-child-H.pdf (accessed on 11 July 2021).
- Ministry of Education; Ministry of Health and Welfare; Centers for Disease Control and Prevention. The Statistics on the 14th Korea Youth Risk Behavior Survey in 2018; Centers for Disease Control and Prevention: Sejong, Korea, 2018.
- Daniels, S.R.; Jacobson, M.S.; McCrindle, B.W.; Eckel, R.H.; Sanner, B.M. American Heart Association childhood obesity research summit. Circulation 2009, 119, 2114–2123. [Google Scholar] [CrossRef]
- Sagar, R.; Gupta, T. Psychological aspects of obesity in children and adolescents. Indian J. Pediatr. 2018, 85, 554–559. [Google Scholar] [CrossRef]
- Weihrauch-Blüher, S.; Schwarz, P.; Klusmann, J.-H. Childhood obesity: Increased risk for cardiometabolic disease and cancer in adulthood. Metabolism 2019, 92, 147–152. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Wall, M.; Eisenberg, M.E.; Story, M.; Hannan, P.J. Overweight status and weight control behaviors in adolescents: Longitudinal and secular trends from 1999 to 2004. Prev. Med. 2006, 43, 52–59. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Wall, M.; Story, M.; Standish, A.R. Dieting and unhealthy weight control behaviors during adolescence: Associations with 10-year changes in body mass index. J. Adolesc. Health 2012, 50, 80–86. [Google Scholar] [CrossRef]
- Vidot, D.; Messiah, S.; Prado, G.; Hlaing, W. Relationship between current substance use and unhealthy weight loss practices among adolescents. Matern. Child Health J. 2016, 20, 870–877. [Google Scholar] [CrossRef]
- Kim, J.-S.; Seo, Y. Associations between weight perception, unhealthy weight control behavior, and suicidal ideation and planning among Korean adolescents: A national cross-sectional secondary analysis. J. Pediatr. Nurs. 2021, 56, e62–e69. [Google Scholar] [CrossRef]
- Gonsalves, D.; Hawk, H.; Goodenow, C. Unhealthy weight control behaviors and related risk factors in Massachusetts middle and high school students. Matern. Child Health J. 2014, 18, 1803–1813. [Google Scholar] [CrossRef]
- Division of Epidemiology and Community Health. Project EAT. Available online: https://www.sph.umn.edu/research/projects/project-eat/ (accessed on 11 March 2021).
- Weng, C.-B.; Sheu, J.-J.; Chen, H.-S. Factors associated with unhealthy weight control behaviors among a representative sample of U.S. high school students. J. Sch. Nurs. in press. [CrossRef]
- Niemeier, H.M.; Raynor, H.A.; Lloyd-Richardson, E.E.; Rogers, M.L.; Wing, R.R. Fast food consumption and breakfast skipping: Predictors of weight gain from adolescence to adulthood in a nationally representative sample. J. Adolesc. Health 2006, 39, 842–849. [Google Scholar] [CrossRef] [PubMed]
- Fang, K.; Mu, M.; Liu, K.; He, Y. Screen time and childhood overweight/obesity: A systematic review and meta-analysis. Child Care Health Dev. 2019, 45, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Fan, H.; Zhang, X. Prevalence of and trends in the co-existence of obesogenic behaviors in adolescents from 15 countries. Front. Pediatr. 2021, 9, 664828. [Google Scholar] [CrossRef]
- Boone-Heinonen, J.; Gordon-Larsen, P.; Adair, L.S. Obesogenic clusters: Multidimensional adolescent obesity-related behaviors in the U.S. Ann. Behav. Med. 2008, 36, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Liberali, R.; Del Castanhel, F.; Kupek, E.; de Assis, M.A.A. Latent class analysis of lifestyle risk factors and association with overweight and/or obesity in children and adolescents: Systematic review. Child Obes. 2021, 17, 2–15. [Google Scholar] [CrossRef] [PubMed]
- Fleary, S.A. Combined patterns of risk for problem and obesogenic behaviors in adolescents: A latent class analysis approach. J. Sch. Health 2017, 87, 182–193. [Google Scholar] [CrossRef]
- Collins, L.M.; Lanza, S.T. Latent Class and Latent Transition Analysis with Applications in the Social, Behavioral, and Health Sciences; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar]
- Lanza, S.T.; Rhoades, B.L. Latent class analysis: An alternative perspective on subgroup analysis in prevention and treatment. Prev. Sci. 2013, 14, 157–168. [Google Scholar] [CrossRef]
- Iannotti, R.J.; Wang, J. Patterns of physical activity, sedentary behavior, and diet in U.S. adolescents. J. Adolesc. Health 2013, 53, 280–286. [Google Scholar] [CrossRef]
- Laxer, R.E.; Brownson, R.C.; Dubin, J.A.; Cooke, M.; Chaurasia, A.; Leatherdale, S.T. Clustering of risk-related modifiable behaviours and their association with overweight and obesity among a large sample of youth in the COMPASS study. BMC Public Health 2017, 17, 102. [Google Scholar] [CrossRef]
- Tabacchi, G.; Faigenbaum, A.; Jemni, M.; Thomas, E.; Capranica, L.; Palma, A.; Breda, J.; Bianco, A. Profiles of physical fitness risk behaviours in school adolescents from the ASSO Project: A latent class analysis. Int. J. Environ. Res. Public Health 2018, 15, 1933. [Google Scholar] [CrossRef]
- Sweeting, H.N. Gendered dimensions of obesity in childhood and adolescence. Nutr. J. 2008, 7, 1. [Google Scholar] [CrossRef]
- Ministry of Education; Ministry of Health and Welfare; Centers for Disease Control and Prevention. The Statistics on the 15th Korea Youth Risk Behavior Survey in 2019; Centers for Disease Control and Prevention: Sejong, Korea, 2019.
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Williams, P. Breakfast and the diets of Australian children and adolescents: An analysis of data from the 1995 National Nutrition Survey. Int. J. Food Sci. Nutr. 2007, 58, 201–216. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare; The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2015; Ministry of Health and Welfare: Sejong, Korea, 2016.
- Hoare, E.; Milton, K.; Foster, C.; Allender, S. The associations between sedentary behaviour and mental health among adolescents: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 108. [Google Scholar] [CrossRef]
- Duraccio, K.M.; Krietsch, K.N.; Chardon, M.L.; Van Dyk, T.R.; Beebe, D.W. Poor sleep and adolescent obesity risk: A narrative review of potential mechanisms. Adolesc. Health Med. Ther. 2019, 10, 117–130. [Google Scholar] [CrossRef]
- American Lung Association. Cutting Tobacco’s Rural Roots: Tobacco Use in Rural Communities; American Lung Association: Washington, DC, USA, 2015. [Google Scholar]
- Donath, C.; Gräßel, E.; Baier, D.; Pfeiffer, C.; Karagülle, D.; Bleich, S.; Hillemacher, T. Alcohol consumption and binge drinking in adolescents: Comparison of different migration backgrounds and rural vs. urban residence—A representative study. BMC Public Health 2011, 11, 84. [Google Scholar] [CrossRef]
- Hanson, M.D.; Chen, E. Socioeconomic status and health behaviors in adolescence: A review of the literature. J. Behav. Med. 2007, 30, 263–285. [Google Scholar] [CrossRef]
- Edwards, J.U.; Mauch, L.; Winkelman, M.R. Relationship of nutrition and physical activity behaviors and fitness measures to academic performance for sixth graders in a midwest city school district. J. Sch. Health 2011, 81, 65–73. [Google Scholar] [CrossRef]
- Korean Society for the Study of Obesity. Obesity Treatment Guideline; Korean Society for the Study of Obesity: Seoul, Korea, 2020. [Google Scholar]
- Berglund, P.A. Latent Class Analysis Using PROC LCA. Available online: http://support.sas.com/resources/papers/proceedings16/5500-2016.pdf (accessed on 2 October 2019).
- Dziak, J.J.; Bray, B.C.; Wagner, A.T. LCA_Distal_BCH SAS Macro Users’ Guide (Version 1.1); The Methodology Center, Penn State: University Park, PA, USA, 2017. [Google Scholar]
- Bolck, A.; Croon, M.; Hagenaars, J. Estimating latent structure models with categorical variables: One-step versus three-step estimators. Polit. Anal. 2004, 12, 3–27. [Google Scholar] [CrossRef]
- World Health Organization. Adolescents’ Dietary Habits; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2016. [Google Scholar]
- Kann, L.; McManus, T.; Harris, W.A.; Shanklin, S.L.; Flint, K.H.; Queen, B.; Lowry, r.; Chyen, D.; Whittle, L.; Thornton, J.; et al. Youth Risk Behavior Surveillance—United States, 2017. MMWR Surveill. Summ. 2018, 67, 1–114. [Google Scholar] [CrossRef] [PubMed]
- Ko, Y.-M.; Lim, M.K. The difference of general characteristics, health status and health behavior of Internet over users by Internet use purposes among Korean adolescents. Korea J. Health Edu. Promot. 2015, 32, 1–15. [Google Scholar] [CrossRef][Green Version]
- Mayne, S.L.; Virudachalam, S.; Fiks, A.G. Clustering of unhealthy behaviors in a nationally representative sample of U.S. children and adolescents. Prev. Med. 2020, 130, 105892. [Google Scholar] [CrossRef]
- Reilly, J.J. Descriptive epidemiology and health consequences of childhood obesity. Best Pract. Res. Clin. Endoc. Metab. 2005, 19, 327–341. [Google Scholar] [CrossRef]
- Luszczynska, A.; de Wit, J.B.F.; de Vet, E.; Januszewicz, A.; Liszewska, N.; Johnson, F.; Pratt, M.; Gaspar, T.; de Matos, M.G.; Stok, F.M. At-home environment, out-of-home environment, snacks and sweetened beverages intake in preadolescence, early and mid-adolescence: The interplay between environment and self-regulation. J. Youth Adolesc. 2013, 42, 1873–1883. [Google Scholar] [CrossRef]
- Latimer, W.; Zur, J. Epidemiologic trends of adolescent use of alcohol, tobacco, and other drugs. Child Adolesc. Psychiatr. N. Am. 2010, 19, 451–464. [Google Scholar] [CrossRef]
- Park, E. A comparative study of youth health risk behaviors by region: Focused on metropolitan areas, medium sized and small city areas, and rural areas. J. Korean Acad. Nurs. 2010, 40, 14–23. [Google Scholar] [CrossRef]
- Warren, J.C.; Smalley, K.B.; Barefoot, K.N. Perceived ease of access to alcohol, tobacco and other substances in rural and urban US students. Rural Remote Health 2015, 15, 3397. [Google Scholar]
- Chae, M.; Han, K. Differences in health behavior profiles of adolescents in urban and rural areas in a Korean city. Healthcare 2021, 9, 282. [Google Scholar] [CrossRef]
- Hoare, E.; Skouteris, H.; Fuller-Tyszkiewicz, M.; Millar, L.; Allender, S. Associations between obesogenic risk factors and depression among adolescents: A systematic review. Obes. Rev. 2014, 15, 40–51. [Google Scholar] [CrossRef]
- Khantzian, E.J. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harv. Rev. Psychiatr. 1997, 4, 231–244. [Google Scholar] [CrossRef]
- Rubio-López, N.; Morales-Suárez-Varela, M.; Pico, Y.; Livianos-Aldana, L.; Llopis-González, A. Nutrient intake and depression symptoms in Spanish children: The ANIVA study. Int. J. Environ. Res. Public Health 2016, 13, 352. [Google Scholar] [CrossRef]
- Picciotto, M.R.; Brunzell, D.H.; Caldarone, B.J. Effect of nicotine and nicotinic receptors on anxiety and depression. Neuroreport 2002, 13, 1097–1106. [Google Scholar] [CrossRef]
- Kwon, M.; Park, E.; Dickerson, S.S. Adolescent substance use and its association to sleep disturbances: A systematic review. Sleep Health 2019, 5, 382–394. [Google Scholar] [CrossRef]
- McCabe, M.P.; Ricciardelli, L.A. A prospective study of pressures from parents, peers, and the media on extreme weight change behaviors among adolescent boys and girls. Behav. Res. Ther. 2005, 43, 653–668. [Google Scholar] [CrossRef]
- Jago, R.; Anderson, C.B.; Baranowski, T.; Watson, K. Adolescent patterns of physical activity: Differences by gender, day, and time of day. Am. J. Prev. Med. 2005, 28, 447–452. [Google Scholar] [CrossRef]
- Jessor, R. Problem behavior theory: A half-century of research on adolescent behavior and development. In The Developmental Science of Adolescence: History Through Autobiography; Lerner, R.M., Petersen, A.C., Silbereisen, R.K., Brooks-Gunn, J., Eds.; Psychology Press: New York, NY, USA, 2014; pp. 239–256. [Google Scholar]
- Sim, W.Y.; Cho, Y.G.; Kang, J.H.; Park, H.A.; Kim, K.W.; Hur, Y.I.; Shin, K.E.; Byeon, G.R. The relationship between smoking and unhealthy weight control behaviors among Korean adolescents: The tenth Korea youth risk behavior web-based survey, 2014. Korean J. Fam. Med. 2017, 38, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Chuang, C.-W.I.; Sussman, S.; Stone, M.D.; Pang, R.D.; Chou, C.-P.; Leventhal, A.M.; Kirkpatrick, M.G. Impulsivity and history of behavioral addictions are associated with drug use in adolescents. Addict. Behav. 2017, 74, 41–47. [Google Scholar] [CrossRef]
- Lee, J.; Lee, Y. The association of body image distortion with weight control behaviors, diet behaviors, physical activity, sadness, and suicidal ideation among Korean high school students: A cross-sectional study. BMC Public Health 2016, 16, 39. [Google Scholar] [CrossRef] [PubMed]
- Goodman, E.; Hinden, B.R.; Khandelwal, S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics 2000, 106, 52–58. [Google Scholar] [CrossRef]
| Factor | Frequency (%) * | |||
|---|---|---|---|---|
| Boys (n = 29,841) | Girls (n = 27,462) | |||
| School year | ||||
| Middle school | 15,401 | (47.7) | 13,983 | (48.1) |
| High school | 14,440 | (52.3) | 13,479 | (51.9) |
| Area of residence | ||||
| Suburban or rural | 14,475 | (49.4) | 13,472 | (49.2) |
| Urban | 15,366 | (50.6) | 13,990 | (50.8) |
| Perceived economic status | ||||
| High or middle | 26,146 | (87.8) | 23,816 | (87.2) |
| Low | 3695 | (12.3) | 3646 | (12.9) |
| Perceived academic performance | ||||
| High or middle | 20,530 | (68.5) | 18,647 | (67.9) |
| Low | 9311 | (31.5) | 8815 | (32.1) |
| Stress | ||||
| Low or average | 20,446 | (68.3) | 14,079 | (51.2) |
| High | 9395 | (31.7) | 13,383 | (48.8) |
| Depressive feeling | ||||
| No | 23,346 | (77.8) | 17,929 | (65.4) |
| Yes | 6495 | (22.2) | 9533 | (34.6) |
| Sleep satisfaction | ||||
| Satisfied or average | 18,610 | (61.4) | 12,621 | (45.2) |
| Dissatisfied | 11,231 | (38.6) | 14,841 | (54.8) |
| Breakfast skipping | ||||
| >2 days/week | 14,321 | (48.1) | 14,662 | (52.9) |
| ≤2 days/week | 15,520 | (52.0) | 12,800 | (47.1) |
| Sugar-sweetened beverage intake | ||||
| ≥3 days/week | 19,650 | (66.2) | 15,242 | (55.5) |
| <3 days/week | 10,191 | (33.8) | 12,220 | (44.5) |
| Fast food consumption | ||||
| ≥3 times/week | 8011 | (27.5) | 6381 | (23.4) |
| <3 times/week | 21,830 | (72.5) | 21,081 | (76.6) |
| Fruit and vegetable consumption | ||||
| Non-daily | 26,109 | (87.4) | 24,393 | (88.6) |
| Daily | 3732 | (12.6) | 3069 | (11.4) |
| Total physical activity | ||||
| ≥60 min/day | 26,814 | (90.5) | 26,746 | (97.4) |
| <60 min/day | 3027 | (9.6) | 716 | (2.6) |
| Non-academic Internet use | ||||
| ≥2 h/day | 13,464 | (45.1) | 14,445 | (52.7) |
| <2 h/day | 16,377 | (54.9) | 13,017 | (47.3) |
| Tobacco product use | ||||
| No | 26,952 | (89.7) | 26,323 | (95.9) |
| Yes | 2889 | (10.3) | 1139 | (4.1) |
| Alcohol use | ||||
| No | 25,000 | (83.2) | 23,903 | (87.0) |
| Yes | 4841 | (16.9) | 3559 | (13.0) |
| Weight status | ||||
| Non-obese | 25,004 | (86.2) | 24,439 | (91.9) |
| Obese | 4055 | (13.8) | 2250 | (8.2) |
| Unhealthy weight control behaviors | ||||
| No | 22,046 | (74.0) | 14,464 | (53.3) |
| Yes | 7795 | (26.0) | 12,998 | (46.8) |
| Number of Latent Classes | G2 | Degree of Freedom | AIC | BIC | Adjusted BIC | Entropy | Log-Likelihood | Percentage of Seeds Associated with Best Fitted Model |
|---|---|---|---|---|---|---|---|---|
| Total | ||||||||
| 1 | 13,719.60 | 247 | 13,735.60 | 13,807.25 | 13,781.83 | 1.00 | −223,225.48 | 100.0 |
| 2 | 5055.70 | 238 | 5089.70 | 5241.96 | 5187.93 | 0.75 | −218,893.54 | 100.0 |
| 3 | 1841.57 | 229 | 1893.57 | 2126.43 | 2043.80 | 0.51 | −217,286.47 | 100.0 |
| 4 | 842.81 | 220 | 912.81 | 1226.27 | 1115.04 | 0.48 | −216,787.09 | 50.0 |
| 5 | 591.24 | 211 | 679.24 | 1073.31 | 933.48 | 0.54 | −216,661.30 | 15.0 |
| Boys | ||||||||
| 1 | 7686.18 | 247 | 7702.18 | 7768.61 | 7743.18 | 1.00 | −121,481.34 | 100.0 |
| 2 | 2667.31 | 238 | 2701.31 | 2842.47 | 2788.45 | 0.72 | −118,971.90 | 100.0 |
| 3 | 1135.00 | 229 | 1187.00 | 1402.89 | 1320.26 | 0.54 | −118,205.74 | 100.0 |
| 4 | 585.64 | 220 | 655.64 | 946.27 | 835.04 | 0.51 | −117,931.06 | 45.0 |
| 5 | 411.37 | 211 | 499.37 | 864.73 | 724.90 | 0.55 | −117,843.93 | 20.0 |
| Girls | ||||||||
| 1 | 6044.51 | 247 | 6060.51 | 6126.28 | 6100.85 | 1.00 | −99,990.15 | 100.0 |
| 2 | 2554.12 | 238 | 2588.12 | 2727.87 | 2673.84 | 0.80 | −98,244.95 | 20.0 |
| 3 | 736.18 | 229 | 788.18 | 1001.92 | 919.29 | 0.53 | −97,335.98 | 100.0 |
| 4 | 371.60 | 220 | 441.60 | 729.32 | 618.09 | 0.45 | −97,153.69 | 95.0 |
| 5 | 286.48 | 211 | 374.48 | 736.19 | 596.35 | 0.48 | −97,111.13 | 5.0 |
| Boys (n = 29,841) | Girls (n = 27,462) | |||||
|---|---|---|---|---|---|---|
| Mostly Healthy Behaviors (MH) | Poor Dietary Habits + High Internet Use (PDHI) | Poor Dietary Habits + Substance Use (PDSU) | Mostly Healthy Behaviors (MH) | Poor Dietary Habits + High Internet Use (PDHI) | Poor Dietary Habits + Substance Use (PDSU) | |
| Probability of membership | 0.539 | 0.354 | 0.108 | 0.479 | 0.448 | 0.074 |
| Breakfast skipping (>2 days/wk) | 0.431 | 0.506 | 0.641 | 0.442 | 0.597 | 0.751 |
| SSB intake (≥3 days/wk) | 0.429 | 0.966 | 0.797 | 0.300 | 0.795 | 0.754 |
| Fast food consumption (≥3 days/wk) | 0.104 | 0.476 | 0.409 | 0.034 | 0.415 | 0.413 |
| Fruit and vegetable consumption (non-daily) | 0.866 | 0.873 | 0.924 | 0.857 | 0.914 | 0.936 |
| Total physical activity (non-daily) | 0.091 | 0.115 | 0.113 | 0.028 | 0.022 | 0.038 |
| Non-academic Internet use (≥2 h/day) | 0.408 | 0.512 | 0.469 | 0.457 | 0.605 | 0.491 |
| Smoking during the past 30 days (Yes) | 0.018 | 0.036 | 0.692 | 0.004 | 0.005 | 0.503 |
| Drinking during the past 30 days (Yes) | 0.067 | 0.112 | 0.801 | 0.067 | 0.079 | 0.845 |
| Predictor | Boys (n = 29,841) | Girls (n = 27,462) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| p-Value | Poor Dietary Habits + High Internet Use (PDHI) | Poor Dietary Habits + Substance Use (PDSU) | p-Value | Poor Dietary Habits + High Internet Use (PDHI) | Poor Dietary Habits + Substance Use (PDSU) | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
| School year | ||||||||||
| High school (ref. = middle school) | <0.001 | 0.86 | (0.79, 0.95) | 5.72 | (5.03, 6.50) | <0.001 | 1.00 | (0.91, 1.09) | 3.20 | (2.82, 3.64) |
| Area of residence | ||||||||||
| Urban area (ref. = suburban/rural area) | <0.001 | 1.02 | (0.93, 1.11) | 0.82 | (0.74, 0.89) | <0.001 | 0.96 | (0.88, 1.05) | 0.75 | (0.68, 0.83) |
| Perceived economic status | ||||||||||
| Low (ref. = high or middle) | 0.052 | 0.94 | (0.82, 1.08) | 1.11 | (0.97, 1.26) | <0.001 | 1.11 | (0.97, 1.28) | 1.47 | (1.28, 1.69) |
| Perceived academic performance | ||||||||||
| Low (ref. = high or middle) | <0.001 | 1.62 | (1.47, 1.80) | 2.49 | (2.25, 2.76) | <0.001 | 1.80 | (1.62, 1.99) | 2.53 | (2.26, 2.84) |
| Stress | ||||||||||
| High (ref. = low or average) | <0.001 | 1.22 | (1.10, 1.34) | 1.18 | (1.07, 1.31) | <0.001 | 1.52 | (1.39, 1.67) | 1.71 | (1.53, 1.91) |
| Depressive feeling | ||||||||||
| Yes (ref. = no) | <0.001 | 1.53 | (1.36, 1.72) | 2.80 | (2.50, 3.14) | <0.001 | 1.56 | (1.41, 1.72) | 3.36 | (2.99, 3.77) |
| Sleep satisfaction | ||||||||||
| Dissatisfied (ref. = average or satisfied) | <0.001 | 1.54 | (1.41, 1.69) | 1.89 | (1.71, 2.09) | <0.001 | 1.36 | (1.24, 1.48) | 1.57 | (1.41, 1.75) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.; La, I.-S. Latent Class Analysis of Obesogenic Behaviors among Korean Adolescents: Associations with Weight-Related Outcomes. Int. J. Environ. Res. Public Health 2021, 18, 11059. https://doi.org/10.3390/ijerph182111059
Lee H, La I-S. Latent Class Analysis of Obesogenic Behaviors among Korean Adolescents: Associations with Weight-Related Outcomes. International Journal of Environmental Research and Public Health. 2021; 18(21):11059. https://doi.org/10.3390/ijerph182111059
Chicago/Turabian StyleLee, Haein, and In-Seo La. 2021. "Latent Class Analysis of Obesogenic Behaviors among Korean Adolescents: Associations with Weight-Related Outcomes" International Journal of Environmental Research and Public Health 18, no. 21: 11059. https://doi.org/10.3390/ijerph182111059
APA StyleLee, H., & La, I.-S. (2021). Latent Class Analysis of Obesogenic Behaviors among Korean Adolescents: Associations with Weight-Related Outcomes. International Journal of Environmental Research and Public Health, 18(21), 11059. https://doi.org/10.3390/ijerph182111059






