Vaping and COVID-19: Insights for Public Health and Clinical Care from Twitter
Abstract
:1. Introduction
2. Methods and Materials
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix A.1. COVID-19-Related Search Terms
Appendix A.2. Vaping-Related Search Terms
References
- Volkow, N.D. Collision of the COVID-19 and Addiction Epidemics. Ann. Intern. Med. 2020, 173, 61–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farsalinos, K.; Barbouni, A.; Niaura, R. Systematic review of the prevalence of current smoking among hospitalized COVID-19 patients in China: Could nicotine be a therapeutic option? Intern. Emerg. Med. 2020, 15, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Pew Research Center. Social Media Use in 2021. 2021. Available online: https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ (accessed on 3 August 2020).
- Majmundar, A.; Allem, J.-P.; Cruz, T.B.; Unger, J.B. Where Do People Vape? Insights from Twitter Data. Int. J. Environ. Res. Public Health 2019, 16, 3056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allem, J.-P.; Escobedo, P.; Chu, K.-H.; Soto, D.W.; Cruz, T.B.; Unger, J. Campaigns and counter campaigns: Reactions on Twitter to e-cigarette education. Tob. Control. 2017, 26, 226–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allem, J.-P.; Ferrara, E.; Uppu, S.P.; Cruz, T.B.; Unger, J.B. E-Cigarette Surveillance with Social Media Data: Social Bots, Emerging Topics, and Trends. JMIR Puclic Health Surveill. 2017, 3, e98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrara, E.; Varol, O.; Davis, C.B.; Menczer, F.; Flammini, A. The Rise of Social Bots. Commun. ACM 2016, 59, 96–104. [Google Scholar] [CrossRef] [Green Version]
- Pennington, J.; Socher, R.; Manning, C. Glove: Global Vectors for Word Representation. In Proceedings of the 2014 Conference on Empirical Methods in Natural Language Processing, Doha, Qatar, 25–29 October 2014. [Google Scholar]
- Cai, G. Tobacco-use disparity in gene expression of ace2, the receptor of 2019-ncov. Preprints 2020. [Google Scholar] [CrossRef]
- Yang, Y.; Lu, Q.; Liu, M.; Wang, Y.; Zhang, A.; Jalali, N.; Dean, N.E.; Longini, I.; Halloran, M.E.; Xu, B.; et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Kopeki, D. World Health Organization Offers Tips for Living under Coronavirus Quarantine: Don’t Drink, Smoke or Watch Too Much News. CNBC. 2020. Available online: https://www.cnbc.com/2020/03/20/who-offers-tips-for-living-under-coronavirus-quarantine-dont-drink-smoke-or-watch-too-much-news.html (accessed on 3 August 2020).
- Morbidity Mortality Weekly Report. Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions among Patients with Coronavirus Disease 2019—United States, 12 February–28 March. 2020. Available online: https://www.cdc.gov/mmwr/volumes/69/wr/mm6913e2.htm (accessed on 3 August 2020).
- California Smokers’ Helpline. Protect Your Lungs. 2020. Available online: https://www.nobutts.org/covid (accessed on 3 August 2020).
- Law, T. Surgeon General Adams Warns of ‘Saddest Week of Most Americans’ Lives’ as Covid-19 Pandemic Spreads. Time. 2020. Available online: https://time.com/5815870/jerome-adams-surgeon-general-saddest-week-covid-19/ (accessed on 3 August 2020).
- Sebag, G. France to Test Nicotine Substitutes as Treatment for Covid-19. Bloomberg. 2020. Available online: https://www.bloomberg.com/news/articles/2020-04-24/france-to-test-nicotine-substitutes-as-treatment-for-covid-19 (accessed on 3 August 2020).
- Kaur, G.; Lungarella, G.; Rahman, I. SARS-CoV-2 COVID-19 susceptibility and lung inflammatory storm by smoking and vaping. J. Inflamm. 2020, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kouzy, R.; Jaoude, J.A.; Kraitem, A.; El Alam, M.B.; Karam, B.; Adib, E.; Zarka, J.; Traboulsi, C.; Akl, E.W.; Baddour, K. Coronavirus Goes Viral: Quantifying the COVID-19 Misinformation Epidemic on Twitter. Cureus 2020, 12, e7255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Majmundar, A.; Allem, J.-P.; Cruz, T.B.; Unger, J.B. Public Health Concerns and Unsubstantiated Claims at the Intersection of Vaping and COVID-19. Nicotine Tob. Res. 2020, 22, 1667–1668. [Google Scholar] [CrossRef] [Green Version]
- Armatas, C.; Heinzerling, A.; Wilken, J.A. Notes from the Field: E-cigarette, or Vaping, Product Use–Associated Lung Injury Cases during the COVID-19 Response—California, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 801–802. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Xie, Z.; Li, D. Electronic Cigarette Users’ Perspective on the COVID-19 Pandemic: Observational Study Using Twitter Data. JMIR Public Health Surveill. 2021, 7, e24859. [Google Scholar] [CrossRef] [PubMed]
- Miotke, M. From Camping to Dining Out: Here’s How Experts Rate the Risks of 14 Summer Activities. NPR. 2020. Available online: https://www.wabe.org/from-camping-to-dining-out-heres-how-experts-rate-the-risks-of-14-summer-activit-2/ (accessed on 4 August 2020).
- Guidry, J.P.; Jin, Y.; Orr, C.A.; Messner, M.; Meganck, S. Ebola on Instagram and Twitter: How health organizations address the health crisis in their social media engagement. Public Relat. Rev. 2017, 43, 477–486. [Google Scholar] [CrossRef]
| Topic Label | Definition | Paraphrased Posts | n | % |
|---|---|---|---|---|
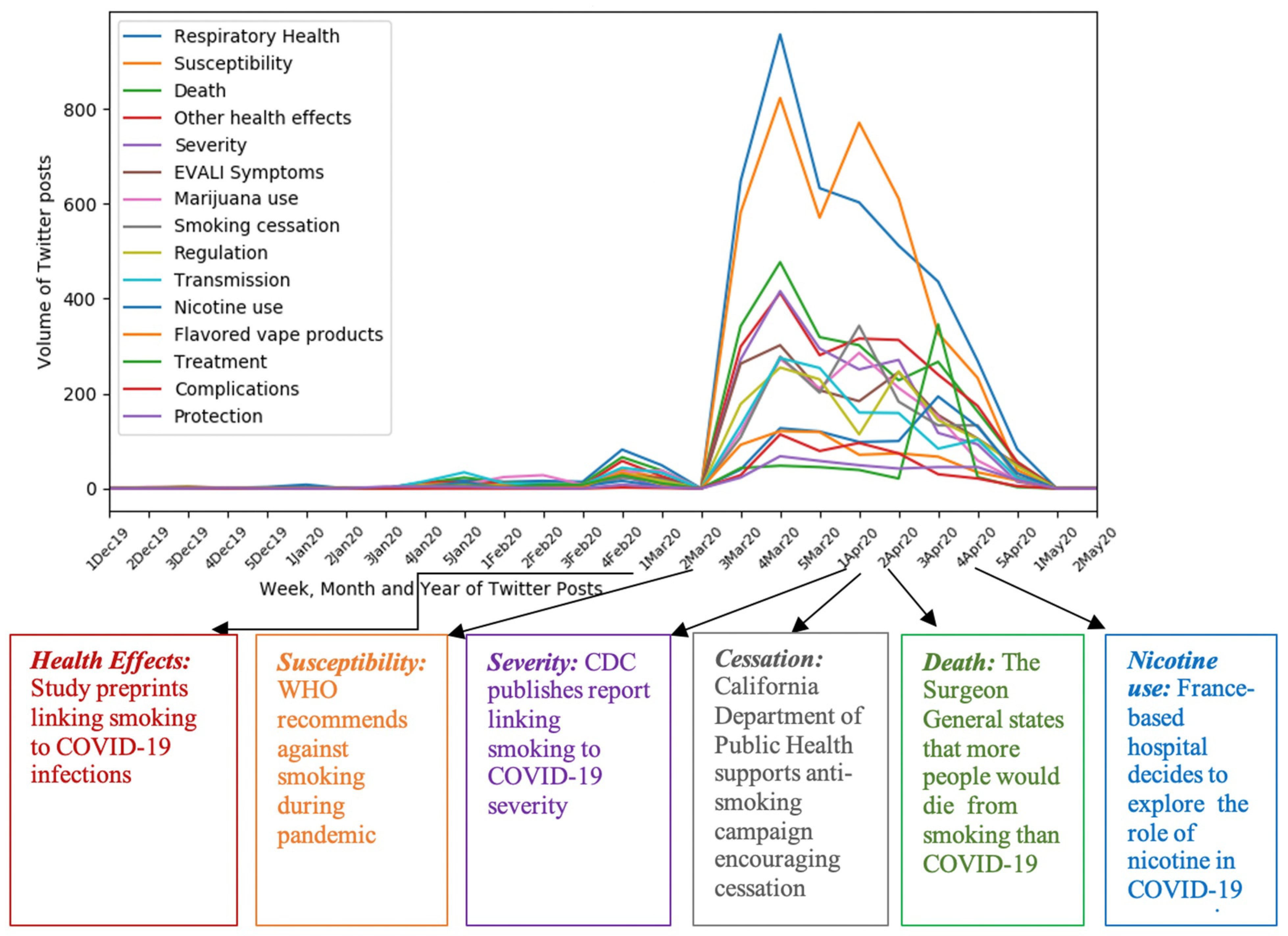
| COVID-19 Respiratory Health | Posts discussed COVID-19 respiratory problems and concerns due to vaping | Vaping perhaps causes pulmonary inflammation. Perfect recipe for covid19 infection. My parents freak out cause I vape cause there is a connection between COVID and vaping and how vaping weakens your respiratory system. | 4359 | 18.87 |
| COVID-19 Susceptibility | Posts discussed fear or risk of contracting COVID-19 as a result of vaping | Those who vape are more at likely to get coronavirus. Because they vape nicotine makes them 5x to 10x less likely to catch the covid disease. | 4049 | 17.53 |
| Death | Posts discussed concerns about dying from COVID-19 and vaping | Guys, go ahead and continue vaping if you want to die from COVID-19. You’ll get yourself and us killed from coronavirus if you keep vaping. | 2326 | 10.07 |
| Other COVID-19 Health Effects | Posts discussed other COVID-19 health effects besides respiratory and death-related outcomes as a result of vaping | I have chest pain–should I blame vaping or covid? I had flu-like symptoms from covid19 and my mom thinks it’s because of vaping. | 2222 | 9.62 |
| COVID-19 Severity | Posts discussed the degree of severity of COVID-19 symptoms among those who vape | Do you all realize that vaping causes more severe COVID-19? Scientists see vaping as a possible risk factor for severe covid19 coronavirus infection | 1784 | 7.72 |
| EVALI Symptoms | Posts discussed the similarity of symptoms related to COVID-19 and EVALI (E-cigarette, or vaping, product use-associated lung injury) and potential misdiagnosis | We dropped the ball on a hoax because COVID-19 might have been EVALI. The death rate of EVALI is 44 CVOID19 is 5 at first and down to 2. Now I am pretty sure for the EVALI cases they did not check the virus DNA assay. | 1603 | 6.94 |
| Marijuana Use | Posts discussed use or purchase of marijuana and/or cannabis during the COVID-19 pandemic | I have a sore throat from being at home weed vaping during covid. I guess I it a bit too much. So you allow alcohol shops to remain during covid but not weed or vape shops? | 1481 | 6.41 |
| Smoking Cessation | Posts discussed challenges and opportunities in smoking cessation due to lockdowns during the COVID-19 pandemic | All vape shops are shutdown. How am I expected to quit smoking during covid19 lockdown? Now is the time to quit smoking and switch to vaping! #covid | 1465 | 6.34 |
| Regulation | Posts discussed the role of, or mentions of, regulatory agencies, such as the FDA or CDC, during the COVID-19 pandemic. | The FDA will bankrupt thousands of vape shops inspite of this coronavirus pandemic. CDC hasn’t found one case of a vaper having covid so far. | 1404 | 6.08 |
| COVID-19 Transmission | Posts discussed ways people believe the COVID-19 virus is transmitted as a result of vaping | Is it possible that COVID can spread from person to person by vaping products? Can covid19 spread through secondhand smoke if an individual is close to a person smoking? | 1343 | 5.81 |
| Nicotine Use | Posts discussed use of, or the role of, nicotine-containing substances during the COVID-19 pandemic. | How do I get my fill of nicotine when everything is shutdown? #covid. Does anyone know if vaping nicotine really decreases chances of getting covid? | 898 | 3.89 |
| Flavored Vape Products | Posts discussed flavored vape product use and bans in the COVID-19 pandemic. | If you could have the same compassion for us as you would for someone with covid, please allow us to still purchase flavors and products online. You guys I know lots of people are sick and dying right now but do not worry some folks have the solution: banning flavored vapes during covid19. | 662 | 2.87 |
| COVID-19 Treatment | Posts discussed how vaping could aid in the treatment of COVID-19 | Are you guys aware that vaping vaping can treat all symptoms of COVID-19? Vape pens could directly deliver covid meds to the lung for treatment. | 636 | 2.75 |
| COVID-19 Complications | Posts discussed COVID-19-related complications among those who vape | Vaping can worsen infections from COVID-19. These youngsters who are now having complications from covid19 use vape pens the most. | 450 | 1.95 |
| Protection | Posts discussed potential protective effects of vaping in COVID-19 | Propylene glycol found in vaping liquids has shown to have protected people from COVID-19. The e-liquid and vape salts have antiviral properties that can prevent covid. | 375 | 1.62 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Majmundar, A.; Allem, J.-P.; Unger, J.B.; Cruz, T.B. Vaping and COVID-19: Insights for Public Health and Clinical Care from Twitter. Int. J. Environ. Res. Public Health 2021, 18, 11231. https://doi.org/10.3390/ijerph182111231
Majmundar A, Allem J-P, Unger JB, Cruz TB. Vaping and COVID-19: Insights for Public Health and Clinical Care from Twitter. International Journal of Environmental Research and Public Health. 2021; 18(21):11231. https://doi.org/10.3390/ijerph182111231
Chicago/Turabian StyleMajmundar, Anuja, Jon-Patrick Allem, Jennifer B. Unger, and Tess Boley Cruz. 2021. "Vaping and COVID-19: Insights for Public Health and Clinical Care from Twitter" International Journal of Environmental Research and Public Health 18, no. 21: 11231. https://doi.org/10.3390/ijerph182111231







