Association between Lifetime Tobacco Use and Alcohol Consumption Trajectories and Cardiovascular and Chronic Respiratory Diseases among Older People
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.2. Measures
2.2.1. Tobacco Use and Alcohol Consumption Trajectories
2.2.2. CVDs and CRDs
2.2.3. Control Variables
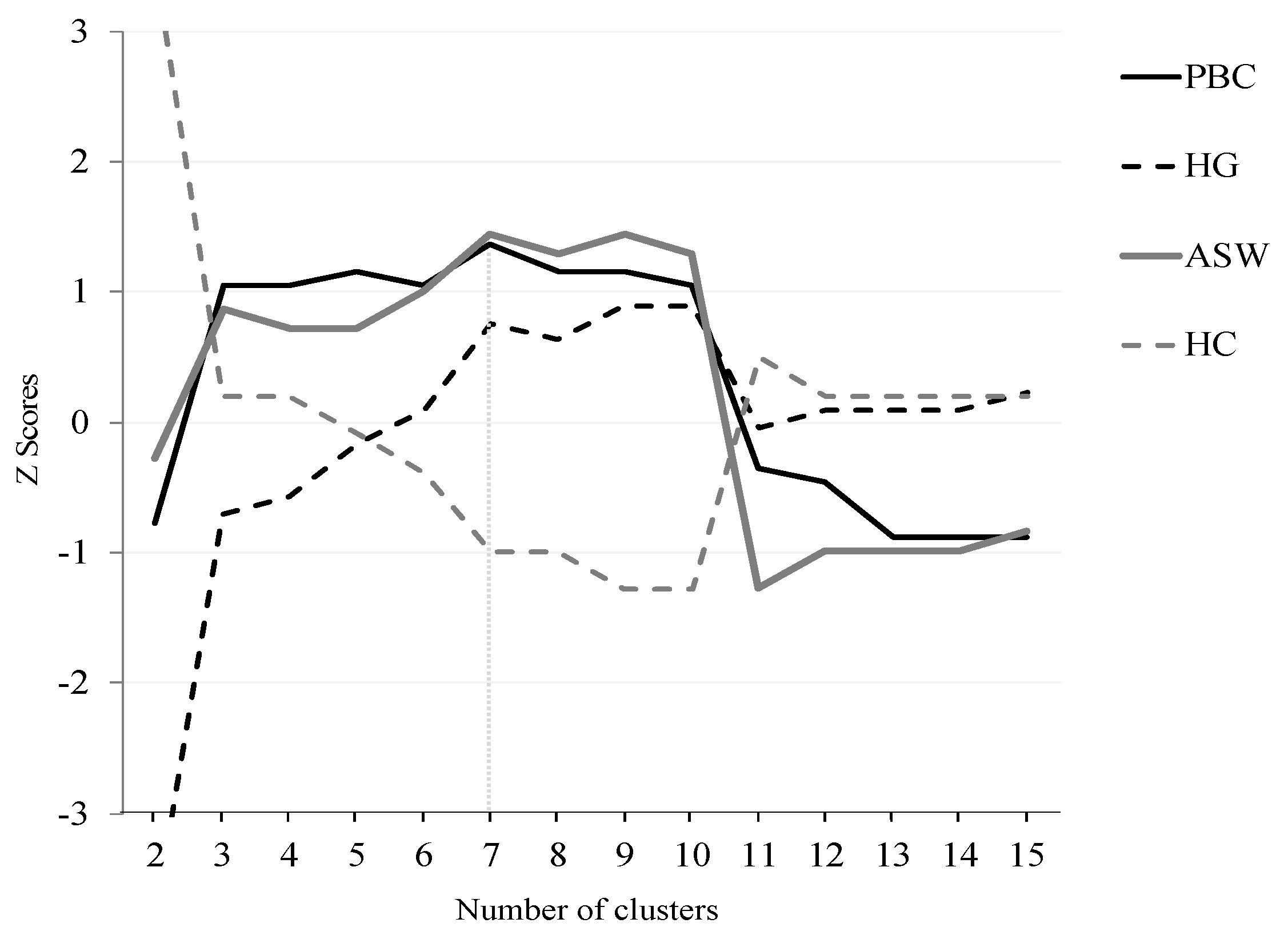
2.3. Statistical Analysis
3. Results
3.1. Weighted Univariate Descriptives
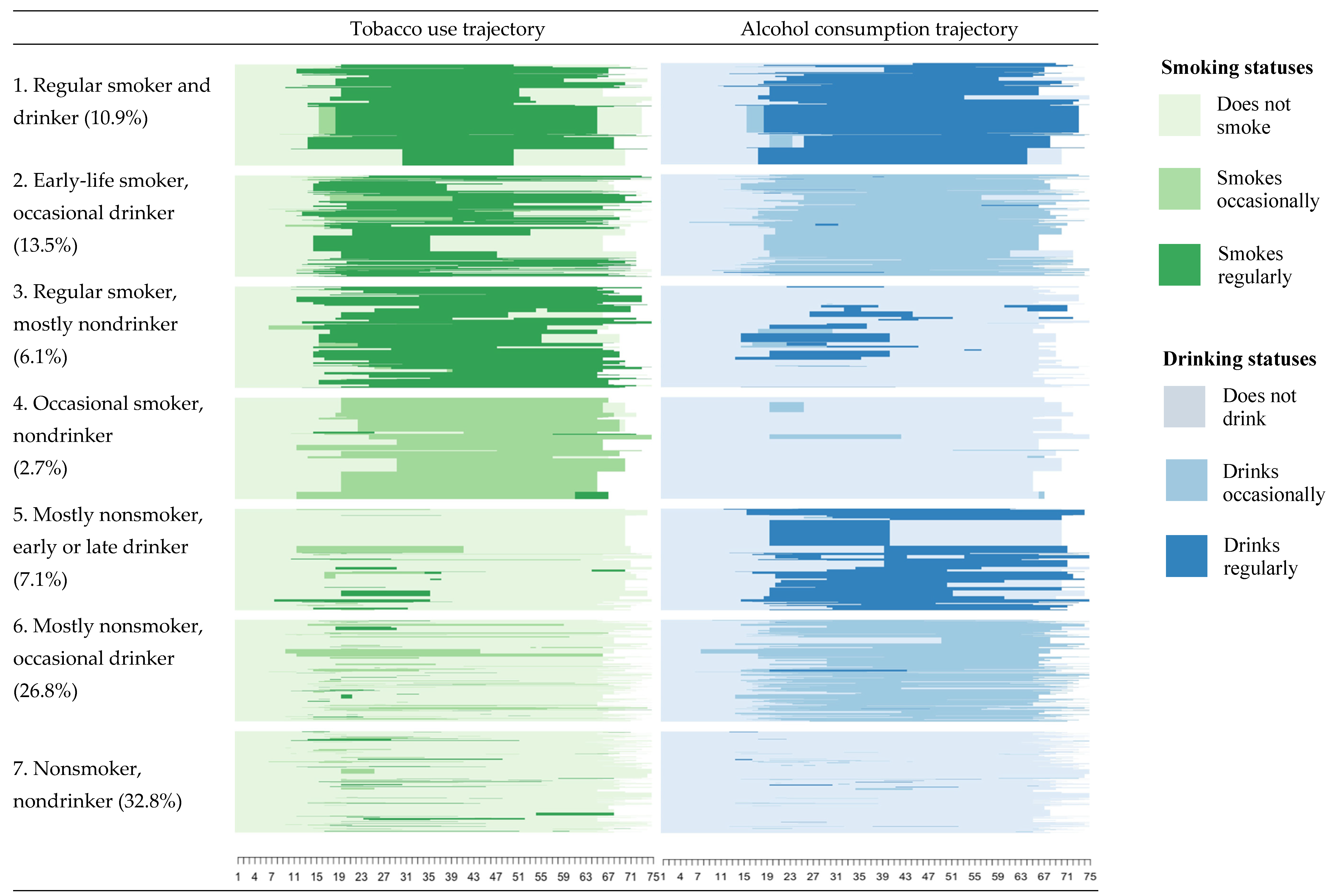
3.2. Tobacco Use and Alcohol Consumption Trajectories
3.3. Tobacco–Alcohol Trajectories and CVDs and CRDs among Older People
4. Discussion
5. Conclusions
Author Contributions
Funding
- -
- ANID/FONDECYT/INICIACION/Nº11180360
- -
- ANID/FONDAP/Nº15130009
- -
- ANID/FONDAP/Nº15130011
- -
- ANID/Millennium Science Initiative/Grant NCS17_062 “Millennium Nucleus for the Study of the Life Course and Vulnerability (MLIV)”.
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Matus-Lopez, M.; Chaverri-Carvajal, A. Population with Long-Term Care Needs in Six Latin American Countries: Estimation of Older Adults Who Need Help Performing ADLs. Int. J. Environ. Res. Public Health 2021, 18, 7935. [Google Scholar] [CrossRef]
- Knott, C.S.; Bell, S.; Britton, A. The stability of baseline-defined categories of alcohol consumption during the adult life-course: A 28-year prospective cohort study. Addiction 2017, 113, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Mayyas, F.; Alzoubi, K. Cardiac effects of cigarette tobacco smoking in rat model of diabetes. Life Sci. 2018, 211, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Parry, C.D.; Patra, J.; Rehm, J. Alcohol consumption and non-communicable diseases: Epidemiology and policy implications. Addiction 2011, 106, 1718–1724. [Google Scholar] [CrossRef]
- Britton, A.; Ben-Shlomo, Y.; Benzeval, M.; Kuh, D.; Bell, S. Life course trajectories of alcohol consumption in the United Kingdom using longitudinal data from nine cohort studies. BMC Med. 2015, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gémes, K.; Moeller, J.; Engström, K.; Sidorchuk, A. Alcohol consumption trajectories and self-rated health: Findings from the Stockholm Public Health Cohort. BMJ Open 2019, 9, e028878. [Google Scholar] [CrossRef]
- Jandackova, V.K.; Scholes, S.; Britton, A.; Steptoe, A. Healthy Lifestyle and Cardiac Vagal Modulation Over 10 Years: Whitehall II Cohort Study. J. Am. Heart Assoc. 2019, 8, e012420. [Google Scholar] [CrossRef]
- Clennell, S.; Kuh, D.; Guralnik, J.M.; Patel, K.V.; Mishra, G.D. Characterisation of smoking behaviour across the life course and its impact on decline in lung function and all-cause mortality: Evidence from a British birth cohort. J. Epidemiol. Community Health 2008, 62, 1051–1056. [Google Scholar] [CrossRef] [PubMed]
- Frosch, Z.A.; Dierker, L.C.; Rose, J.S.; Waldinger, R.J. Smoking trajectories, health, and mortality across the adult lifespan. Addict. Behav. 2009, 34, 701–704. [Google Scholar] [CrossRef]
- Chen, S.; Kawasaki, Y.; Hu, H.; Kuwahara, K.; Yamamoto, M.; Uehara, A.; Honda, T.; Yamamoto, S.; Nakagawa, T.; Miyamoto, T.; et al. Smoking Cessation, Weight Gain, and the Trajectory of Estimated Risk of Coronary Heart Disease: 8-Year Follow-up From a Prospective Cohort Study. Nicotine Tob. Res. 2021, 23, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Zong, G.; Liu, G.; Wang, M.; Rosner, B.; Pan, A.; Willett, W.C.; Manson, J.E.; Hu, F.B.; Sun, Q. Smoking Cessation, Weight Change, Type 2 Diabetes, and Mortality. N. Engl. J. Med. 2018, 379, 623–632. [Google Scholar] [CrossRef]
- Liu, G.; Hu, Y.; Zong, G.; Pan, A.; Manson, J.E.; Rexrode, K.M.; Rimm, E.B.; Hu, F.B.; Sun, Q. Smoking cessation and weight change in relation to cardiovascular disease incidence and mortality in people with type 2 diabetes: A population-based cohort study. Lancet Diabetes Endocrinol. 2020, 8, 125–133. [Google Scholar] [CrossRef]
- Bell, S.; Daskalopoulou, M.; Rapsomaniki, E.; George, J.; Britton, A.; Bobak, M.; Casas, J.P.; Dale, C.E.; Denaxas, S.; Shah, A.D.; et al. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: Population based cohort study using linked health records. BMJ 2017, 356, j909. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, D.; Britton, A.; Brunner, E.J.; Bell, S. Twenty-Five-Year Alcohol Consumption Trajectories and Their Association With Arterial Aging: A Prospective Cohort Study. J. Am. Heart Assoc. 2017, 6, e005288. [Google Scholar] [CrossRef] [PubMed]
- Ruidavets, J.-B.; Ducimetière, P.; Evans, A.; Montaye, M.; Haas, B.; Bingham, A.; Yarnell, J.; Amouyel, P.; Arveiler, D.; Kee, F.; et al. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: The Prospective Epidemiological Study of Myocardial Infarction (PRIME). BMJ 2010, 341, c6077. [Google Scholar] [CrossRef] [PubMed]
- Britton, A.; Hardy, R.; Kuh, D.; Deanfield, J.; Charakida, M.; Bell, S. Twenty-year trajectories of alcohol consumption during midlife and atherosclerotic thickening in early old age: Findings from two British population cohort studies. BMC Med. 2016, 14, 111. [Google Scholar] [CrossRef] [PubMed]
- Romelsjö, A.; Allebeck, P.; Andréasson, S.; Leifman, A. Alcohol, Mortality and Cardiovascular Events in a 35 Year Follow-up of a Nationwide Representative Cohort of 50,000 Swedish Conscripts up to Age 55. Alcohol Alcohol. 2012, 47, 322–327. [Google Scholar] [CrossRef]
- Griswold, M.G.; Fullman, N.; Hawley, C.; Arian, N.; Zimsen, S.R.M.; Tymeson, H.D.; Venkateswaran, V.; Tapp, A.D.; Forouzanfar, M.H.; Salama, J.S.; et al. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 392, 1015–1035. [Google Scholar] [CrossRef]
- Ortolá, R.; García-Esquinas, E.; López-García, E.; León-Muñoz, L.M.; Banegas, J.R.; Rodríguez-Artalejo, F. Alcohol consumption and all-cause mortality in older adults in Spain: An analysis accounting for the main methodological issues. Addiction 2019, 114, 59–68. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf (accessed on 26 October 2021).
- US Department of Health and Human Services. Review Alcohol and Tobacco. 2007. Available online: https://pubs.niaaa.nih.gov/publications/aa71/aa71.htm (accessed on 26 October 2021).
- Balakumar, P.; Maung, U.K.; Jagadeesh, G. Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol. Res. 2016, 113, 600–609. [Google Scholar] [CrossRef]
- World Health Organization. WHO Reveals Leading Causes of Death and Disability Worldwide: 2000–2019. 2020. Available online: https://www.paho.org/en/news/9-12-2020-who-reveals-leading-causes-death-and-disability-worldwide-2000-2019 (accessed on 26 October 2021).
- Simet, S.M.; Sisson, J.H. Alcohol’s effects on lung health and immunity. Alcohol Res. Curr. Rev. 2015, 37, 199–208. [Google Scholar]
- Dintrans, P.V. Health Systems, Aging, and Inequity: An Example from Chile. Int. J. Environ. Res. Public Health 2020, 17, 6546. [Google Scholar] [CrossRef]
- Pan American Health Organization. Health in the Americas+, 2017: Regional Outlook and Country Profiles. 2017. Available online: https://iris.paho.org/handle/10665.2/34321 (accessed on 26 October 2021).
- Ministerio de Salud de Chile. Encuesta Nacional de Salud 2016–2017. Primeros resultados. 2017. Available online: https://www.minsal.cl/wp-content/uploads/2017/11/ENS-2016-17_PRIMEROS-RESULTADOS.pdf (accessed on 26 October 2021).
- Ministerio de Salud de Chile. Ministerio de Salud de Chile. Encuesta Nacional de Salud 2016-2017. Segunda Entrega de Re-Sultados. 2018. Available online: https://www.minsal.cl/wp-content/uploads/2018/01/2-Resultados-ENS_MINSAL_31_01_2018.pdf (accessed on 26 October 2021).
- OECD. Overweight or Obese Population. 2020. Available online: https://data.oecd.org/healthrisk/overweight-or-obese-population.htm (accessed on 26 October 2021).
- Paraje, G.; Araya, D.; Drope, J. Illicit cigarette trade in Metropolitan Santiago de Chile. Tob. Control. 2020, 29, 68–73. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2019.
- Bambs, C.; Bravo-Sagua, R.; Margozzini, P.; Lavandero, S. Science and Health Policies to Tackle Chronic Diseases in Chile. Trends Endocrinol. Metab. 2020, 31, 67–70. [Google Scholar] [CrossRef]
- Peruga, A.; Molina, X.; Delgado, I.; Matute, I.; Olea, A.; Hirmas, M.; González, C.; Aguilera, X. Compliance with the smoking ban in enclosed, semiopen and open areas of workplaces and public places in Chile. Tob. Control. 2021, 30, 570–573. [Google Scholar] [CrossRef]
- Paraje, G.; Araya, D. Relationship between smoking and health and education spending in Chile. Tob. Control. 2017, 27, 560–567. [Google Scholar] [CrossRef]
- Vidal, C.; Padilla, O.; Bambs, C. Tabaquismo en el adulto mayor: Un freno al envejecimiento saludable en la población chilena. Rev. Médica de Chile 2020, 148, 939–946. [Google Scholar] [CrossRef]
- American Association for Public Opinion Research (AAPOR). Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 2016. Available online: https://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169thEditionfinal.pdf (accessed on 26 October 2021).
- Morselli, D.; Dasoki, N.; Gabriel, R.; Gauthier, J.-A.; Henke, J.; Le Goff, J.-M. Using Life History Calendars to Survey Vulnerability. In Surveying Human Vulnerabilities across the Life Course; Springer: Cham, Switzerland, 2016; pp. 179–201. [Google Scholar]
- Conway, M.A. Autobiographical knowledge and autobiographical memories. In Remembering our Past: Studies in Autobiographical Memory; Cambridge University Press: New York, NY, USA, 1996; pp. 67–93. [Google Scholar]
- Gauthier, J.-A.; Widmer, E.D.; Bucher, P.; Notredame, C. Multichannel Sequence Analysis Applied to Social Science Data. Sociol. Methodol. 2010, 40, 1–38. [Google Scholar] [CrossRef]
- Ritschard, G.; Studer, M. Sequence Analysis: Where Are We, Where Are We Going? In Sequence Analysis and Related Approaches; Springer: Cham, Switzerland, 2018; pp. 1–11. [Google Scholar]
- Macindoe, H.; Abbott, A. Sequence Analysis and Optimal Matching Techniques for Social Science Data. In Handbook of Data Analysis; SAGE: London, UK, 2012; pp. 386–406. [Google Scholar]
- Gabadinho, A.; Ritschard, G.; Müller, N.S.; Studer, M. Analyzing and Visualizing State Sequences inRwithTraMineR. J. Stat. Softw. 2011, 40, 1–37. [Google Scholar] [CrossRef]
- Zhang, Q.-L.; Zhao, L.-G.; Zhang, W.; Li, H.-L.; Gao, J.; Han, L.-H.; Zheng, W.; Shu, X.-O.; Xiang, Y.-B. Combined Impact of Known Lifestyle Factors on Total and Cause-Specific Mortality among Chinese Men: A Prospective Cohort Study. Sci. Rep. 2017, 7, 5293. [Google Scholar] [CrossRef] [PubMed]
- Khaw, K.-T.; Wareham, N.; Bingham, S.; Welch, A.; Luben, R.; Day, N. Combined Impact of Health Behaviours and Mortality in Men and Women: The EPIC-Norfolk Prospective Population Study. PLoS Med. 2008, 5, e12. [Google Scholar] [CrossRef]
- van Dam, R.M.; Li, T.; Spiegelman, D.; Franco, O.H.; Hu, F.B. Combined impact of lifestyle factors on mortality: Prospective cohort study in US women. BMJ 2008, 337, a1440. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.; Wang, X.; Lam, T.H.; Kim, H.C.; Suzanne Asia Pacific Cohort Studies Collaboration; Ninomiya, T.; Knuiman, M.; Vaartjes, I.; Bots, M.L.; Woodward, M. Clustering of risk factors and the risk of incident cardiovascular disease in Asian and Caucasian populations: Results from the Asia Pacific Cohort Studies Collaboration. BMJ Open 2018, 8, e019335. [Google Scholar] [CrossRef] [PubMed]
- Berg, C.J.; Thrasher, J.F.; Barnoya, J.; Cohen, J.E.; Maziak, W.; Lando, H.; Drope, J.; Mejía, R.; Foley, K.; Nakkash, R.; et al. Strengthening Policy-Relevant Tobacco Research Capacity in Low- and Middle-Income Countries: Challenges, Opportunities, and Lessons Learned. Nicotine Tob. Res. 2018, 21, 1140–1143. [Google Scholar] [CrossRef] [PubMed]
| Variable | % | Variable | % | ||
|---|---|---|---|---|---|
| CVD | Presence | 17.34 | Body mass index | Obese | 30.20 |
| Absence | 82.65 | Not obese | 69.80 | ||
| CRD | Presence | 6.16 | Physical activity | 1 or less a week | 35.97 |
| Absence | 93.84 | >1 a week | 64.03 | ||
| Gender | Women | 56.77 | Portion of fruits or vegetables | Every day | 78.91 |
| Men | 43.23 | <6 times a week | 21.09 | ||
| Education | Primary or none | 38.51 | Mean (SD) | Min–Max | |
| Secondary | 38.89 | Age | 69.83 (3.14) | 65–75 | |
| Tertiary | 22.60 |
| CVD | CRD | Education (%) | Gender (%) | Body Mass Index (%) | Physical Activity (%) | Portion of Fruits or Vegetables (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tobacco and Alcohol Trajectories Types | Primary or None | Secon Dary | Tertiary | Women | Men | Obese | Not Obese | 1 or Less a Week | >1 a Week | <6 Times a Week | Every Day | Total | ||
| 1. Regular smoker and drinker | 53.1 | 12.5 | 13.0 | 47.5 | 39.5 | 12.6 | 87.4 | 6.5 | 93.5 | 45.6 | 54.4 | 40.2 | 59.7 | 10.9 |
| 2. Early-life smoker, occasional drinker | 5.6 | 11.2 | 39.2 | 36.1 | 24.7 | 53.9 | 46.1 | 31.7 | 68.3 | 47.8 | 52.2 | 21.9 | 78.1 | 13.5 |
| 3. Regular smoker, mostly nondrinker | 11.7 | 6.8 | 59.7 | 29.4 | 10.9 | 52.6 | 47.4 | 19.1 | 80.9 | 71.8 | 28.2 | 30.9 | 69.1 | 6.1 |
| 4. Occasional smoker, nondrinker | 9.9 | 5.0 | 22.4 | 53.4 | 24.2 | 80.0 | 20.0 | 14.9 | 85.1 | 80.9 | 19.1 | 14.1 | 85.9 | 2.7 |
| 5. Mostly nonsmoker, early or late drinker | 4.0 | 3.1 | 25.0 | 30.3 | 44.7 | 18.8 | 81.2 | 19.0 | 81.0 | 41.1 | 58.9 | 4.9 | 95.1 | 7.1 |
| 6. Mostly nonsmoker, occasional drinker | 20.3 | 3.3 | 37.8 | 45.3 | 16.9 | 60.0 | 40.0 | 31.0 | 69.0 | 55.7 | 33.3 | 17.4 | 82.6 | 26.8 |
| 7. Nonsmoker, nondrinker | 12.4 | 4.9 | 47.6 | 34.5 | 18.0 | 76.7 | 23.3 | 43.0 | 57.0 | 63.2 | 36.8 | 19.7 | 80.3 | 32.8 |
| Total | 17.3 | 6.2 | 38.5 | 38.9 | 22.6 | 56.7 | 43.3 | 30.3 | 69.7 | 56.6 | 43.4 | 21.1 | 78.9 | 100.0 |
| CVD | CRD | |||||
|---|---|---|---|---|---|---|
| RRR | CI 95% | AME | RRR | CI 95% | AME | |
| Tobacco and alcohol trajectories types | ||||||
| (ref = Type 1. Regular smoker and drinker) | ||||||
| 2. Early-life smoker, occasional drinker | 0.06 *** | (0.01–0.24) | –0.44 | 0.60 | (0.11–3.06) | −0.06 |
| 3. Regular smoker, mostly nondrinker | 0.13 * | (0.03–0.65) | –0.38 | 0.28 | (0.05–1.58) | −0.12 |
| 4. Occasional smoker, nondrinker | 0.13 * | (0.02–0.86) | –0.38 | 0.21 * | (0.05–0.85) | −0.14 |
| 5. Mostly nonsmoker, early or late drinker | 0.03 ** | (0.00–0.24) | –0.47 | 0.19 + | (0.03–1.14) | −0.14 |
| 6. Mostly nonsmoker, occasional drinker | 0.24 + | (0.06–1.08) | –0.30 | 0.14 * | (0.03–0.66) | −0.15 |
| 7. Nonsmoker, nondrinker | 0.12 ** | (0.03–0.46) | –0.39 | 0.17 * | (0.04–0.87) | −0.14 |
| Socio-demographics | ||||||
| Age | 1.08 | (0.98–1.20) | 1.08 | (0.93–1.26) | ||
| Gender (ref = Men) | ||||||
| Women | 0.70 | (0.28–1.75) | 2.23 + | (0.90–5.54) | ||
| Educational level (ref = Primary or none) | ||||||
| Secondary | 0.72 | (0.34–1.56) | 0.93 | (0.41–2.08) | ||
| Tertiary | 1.06 | (0.35–3.24) | 0.28 * | (0.09–0.89) | ||
| Health risks | ||||||
| Body mass index (ref = Not Obese) | ||||||
| Obese | 1.06 * | (1.00–1.12) | 0.93 | (0.86–1.01) | ||
| Physical activity (ref = More than once a week) | ||||||
| Once a week or less | 0.80 | (0.35–1.85) | 0.77 | (0.30–1.93) | ||
| Frequency fruits and vegetables (ref = Six times a week or less) | ||||||
| Every day | 0.80 | (0.37–1.72) | 1.13 | (0.51–2.48) | ||
| Intercept | 0.00 | 0.00 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Madero-Cabib, I.; Bambs, C. Association between Lifetime Tobacco Use and Alcohol Consumption Trajectories and Cardiovascular and Chronic Respiratory Diseases among Older People. Int. J. Environ. Res. Public Health 2021, 18, 11275. https://doi.org/10.3390/ijerph182111275
Madero-Cabib I, Bambs C. Association between Lifetime Tobacco Use and Alcohol Consumption Trajectories and Cardiovascular and Chronic Respiratory Diseases among Older People. International Journal of Environmental Research and Public Health. 2021; 18(21):11275. https://doi.org/10.3390/ijerph182111275
Chicago/Turabian StyleMadero-Cabib, Ignacio, and Claudia Bambs. 2021. "Association between Lifetime Tobacco Use and Alcohol Consumption Trajectories and Cardiovascular and Chronic Respiratory Diseases among Older People" International Journal of Environmental Research and Public Health 18, no. 21: 11275. https://doi.org/10.3390/ijerph182111275







