Validation of the COVID-19 Transmission Misinformation Scale and Conditional Indirect Negative Effects on Wearing a Mask in Public
Abstract
:1. Introduction
1.1. Theory of Rumor Dissemination
1.2. Persistence of Rumors in Society despite Evidence-Based Facts
1.3. Fear of COVID-19 and Behavioral Changes
1.4. COVID-19 Transmission Misinformation
1.5. Callousness and Social Interactions
1.6. Overview of Studies
2. Method
2.1. Overview of Studies
2.2. Phase 1 Initial Item Generation
2.3. Participant Inclusion
2.4. Inter-Item Correlations and Reduction
2.5. Factor Loadings
2.6. COVID-19 Transmission Misinformation Consensus
2.7. Demographic Variables
3. Results
3.1. Phase 2 Reliability
3.2. Convergent and Discriminant Validity
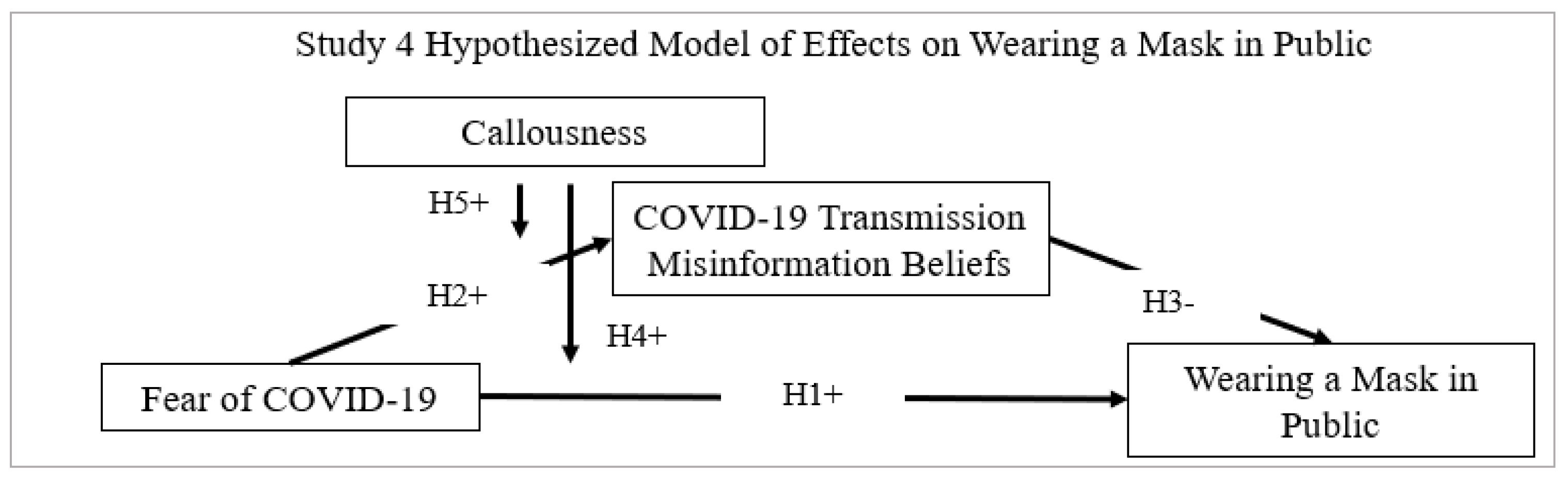
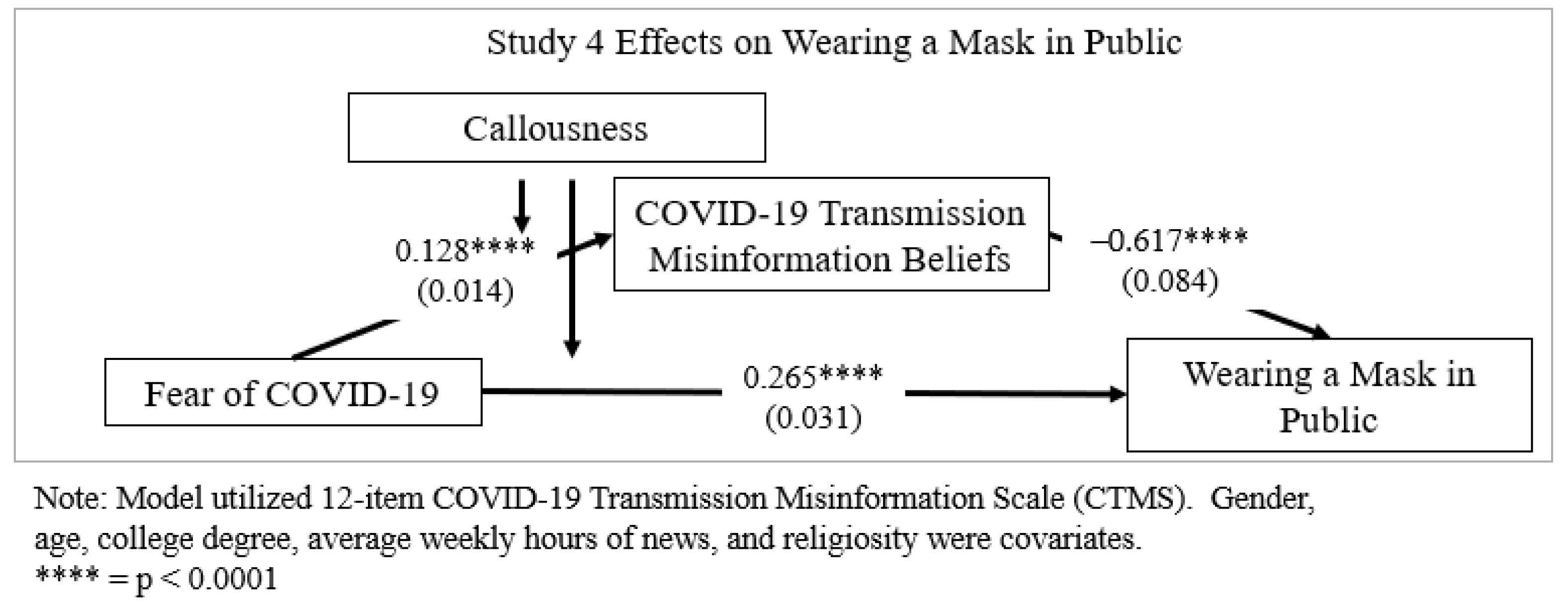
3.3. Study 4 Moderated Mediation Analysis
Phase 3 Measures
3.4. Predictive Validity Results
3.5. Moderated Mediation Results
4. Discussion
5. Implications
6. Limitations
7. Future Research
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahmed, W.; Seguí, F.L.; Vidal-Alaball, J.; Katz, M.S. COVID-19 and the “Film Your Hospital” Conspiracy Theory: Social Network Analysis of Twitter Data. J. Med. Internet Res. 2020, 22, e22374. [Google Scholar] [CrossRef]
- Bitan, D.T.; Grossman-Giron, A.; Bloch, Y.; Mayer, Y.; Shiffman, N.; Mendlovic, S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020, 289, 113100. [Google Scholar] [CrossRef]
- Aiyewumi, O.; Okeke, M.I. The myth that Nigerians are immune to SARS-CoV-2 and that COVID-19 is a hoax are putting lives at risk. J. Glob. Health 2020, 10. [Google Scholar] [CrossRef]
- Ali, S.; Asaria, M.; Stranges, S. COVID-19 and inequality: Are we all in this together? Can. J. Public Health 2020, 111, 415–416. [Google Scholar] [CrossRef]
- Lee, A.M.; Allport, G.W.; Postman, L. The Psychology of Rumor. Am. Sociol. Rev. 1948, 13, 361. [Google Scholar] [CrossRef]
- Allport, G.W.; Postman, L.J. The basic psychology of rumor. Trans. N. Y. Acad. Sci. 1945, 8, 61–81. [Google Scholar] [CrossRef] [PubMed]
- Atrubin, D.; Wiese, M.; Bohinc, B. An outbreak of COVID-19 associated with a recreational hockey game—Florida, June. Morb. Mortal. Wkly. Rep. 2020, 69, 1492–1493. [Google Scholar] [CrossRef]
- Avalos, L.; Tylka, T.L.; Wood-Barcalow, N. The Body Appreciation Scale: Development and psychometric evaluation. Body Image 2005, 2, 285–297. [Google Scholar] [CrossRef]
- Bai, Y.; Yao, L.; Wei, T.; Tian, F.; Jin, D.-Y.; Chen, L.; Wang, M. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA 2020, 323, 1406. [Google Scholar] [CrossRef] [Green Version]
- Basch, C.H.; Kecojevic, A.; Wagner, V.H. Coverage of the COVID-19 Pandemic in the Online Versions of Highly Circulated U.S. Daily Newspapers. J. Community Health 2020, 45, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Beitler, J.R.; Mittel, A.M.; Kallet, R.; Kacmarek, R.; Hess, D.; Branson, R.; Olson, M.; Garcia, I.; Powell, B.; Wang, D.S.; et al. Ventilator Sharing during an Acute Shortage Caused by the COVID-19 Pandemic. Am. J. Respir. Crit. Care Med. 2020, 202, 600–604. [Google Scholar] [CrossRef]
- Bendau, A.; Petzold, M.B.; Pyrkosch, L.; Maricic, L.M.; Betzler, F.; Rogoll, J.; Große, J.; Ströhle, A.; Plag, J. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 283–291. [Google Scholar] [CrossRef]
- Bentzen, J. In crisis, we pray: Religiosity and the COVID-19 pandemic. CEPR Press 2020, 20, 52–108. [Google Scholar]
- Bode, L.; Vraga, E.K. See Something, Say Something: Correction of Global Health Misinformation on Social Media. Health Commun. 2017, 33, 1131–1140. [Google Scholar] [CrossRef]
- Bowleg, L. We’re not all in this together: On COVID-19, intersectionality, and structural inequality. Am. Public Health Assoc. 2020, 110, 917. [Google Scholar] [CrossRef] [PubMed]
- Brennen, J.S.; Simon, F.; Howard, P.N.; Nielsen, R.K. Types, sources, and claims of COVID-19 misinformation. Reuters Inst. 2020, 7, 1–13. [Google Scholar]
- Brezina, T.; Phipps, H.E., Jr. False news reports, folk devils, and the role of public officials: Notes on the social con-struction of law and order in the aftermath of Hurricane Katrina. Deviant Behav. 2009, 31, 97–134. [Google Scholar] [CrossRef]
- Briggs, C.L.; Hallin, D.C. Making Health Public: How News Coverage is Remaking Media, Medicine, and Contemporary Life; Routledge: Oxford, UK, 2016. [Google Scholar]
- Brotherton, R.; French, C.C.; Pickering, A.D. Measuring Belief in Conspiracy Theories: The Generic Conspiracist Beliefs Scale. Front. Psychol. 2013, 4, 279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, T.S.; Walensky, R.P. Serosurveillance and the COVID-19 Epidemic in the US: Undetected, Uncertain, and Out of Control. JAMA 2020, 324, 749–751. [Google Scholar] [CrossRef] [PubMed]
- Buhrmester, M.; Kwang, T.; Gosling, S.D. Amazon’s Mechanical Turk: A New Source of Inexpensive, Yet High-Quality Data? American Psychological Association: Washington, DC, USA, 2016. [Google Scholar]
- Byambasuren, O.; Cardona, M.; Bell, K.; Clark, J.; McLaws, M.-L.; Glasziou, P. Estimating the extent of asymptomatic COVID-19 and its potential for community transmission: Systematic review and meta-analysis. Off. J. Assoc. Med. Microbiol. Infect. Dis. Can. 2020, 5, 223–234. [Google Scholar] [CrossRef]
- Calvillo, D.P.; Ross, B.J.; Garcia, R.J.B.; Smelter, T.J.; Rutchick, A.M. Political Ideology Predicts Perceptions of the Threat of COVID-19 (and Susceptibility to Fake News About It). Soc. Psychol. Pers. Sci. 2020, 11, 1119–1128. [Google Scholar] [CrossRef]
- Cardinale, E.M.; Marsh, A.A. The reliability and validity of the Inventory of Callous Unemotional Traits: A meta-analytic review. Assessment 2020, 27, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, S. Ten Steps in Scale Development and Reporting: A Guide for Researchers. Commun. Methods Meas. 2017, 12, 25–44. [Google Scholar] [CrossRef]
- Castaneda, M.A.; Saygili, M. The Effect of Shelter-in-Place Orders on Social Distancing and the Spread of the COVID-19 Pandemic: A Study of Texas. Front. Public Health 2020, 8, 596607. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention. About Cloth Face Coverings. Coronavirus Disease 2019 (COVID-19). Available online: https://www.google.com.hk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwj9-sHRxOzzAhXRc94KHex7CE0QFnoECAgQAQ&url=https%3A%2F%2Fstacks.cdc.gov%2Fview%2Fcdc%2F89934%2Fcdc_89934_DS1.pdf%3F&usg=AOvVaw1eud3bEOijh9iHTx2nmyxg (accessed on 28 June 2020).
- Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Frequently Asked Questions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/faq.html (accessed on 12 February 2020).
- Chilimuri, S.; Sun, H.; Alemam, A.; Manthri, N.; Shehi, E.; Tejada, J.; Yugay, A.; Nayudu, S.K. Predictors of Mortality in Adults Admitted with COVID-19: Retrospective Cohort Study from New York City. West. J. Emerg. Med. 2020, 21, 779–784. [Google Scholar] [CrossRef]
- Christianson, S.; Goodman, J.; Loftus, E.F. Eyewitness memory for stressful events: Methodological quandaries and ethical dilemmas. In The Handbook of Emotion and Memory: Research and Theory; Psychology Press: London, UK, 1992; pp. 217–241. [Google Scholar]
- Chua, A.Y.; Banerjee, S. To share or not to share: The role of epistemic belief in online health rumors. Int. J. Med. Inform. 2017, 108, 36–41. [Google Scholar] [CrossRef]
- Chua, A.Y.; Banerjee, S. Intentions to trust and share online health rumors: An experiment with medical profes-sionals. Comput. Hum. Behav. 2018, 87, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Chyung, S.Y.; Winiecki, D.; Hunt, G.; Sevier, C.M. Measuring Learners’ Attitudes Toward Team Projects: Scale Development Through Exploratory and Confirmatory Factor Analyses. Am. J. Eng. Educ. AJEE 2017, 8, 61–82. [Google Scholar] [CrossRef] [Green Version]
- Cinelli, M.; Quattrociocchi, W.; Galeazzi, A.; Valensise, C.M.; Brugnoli, E.; Schmidt, A.L.; Zola, P.; Zollo, F.; Scala, A. The COVID-19 social media infodemic. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Clark, L.A.; Watson, D. Constructing validity: Basic issues in objective scale development. Psychol. Assess. 1995, 7, 309–319. [Google Scholar] [CrossRef]
- Cohen, S. Folk Devils and Moral Panics: The Creation of the Mods and Rockers; Taylor & Francis: Abingdon, UK, 1972. [Google Scholar]
- Colins, O.F.; Andershed, H.; Hawes, S.W.; Bijttebier, P.; Pardini, D.A. Psychometric Properties of the Original and Short Form of the Inventory of Callous-Unemotional Traits in Detained Female Adolescents. Child. Psychiatry Hum. Dev. 2015, 47, 679–690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dbouk, T.; Drikakis, D. On respiratory droplets and face masks. Phys. Fluids 2020, 32, 063303. [Google Scholar] [CrossRef]
- Ellis, B.; Degh, L. Legend and Belief: Dialectics of a Folklore Genre. West. Folk. 2001, 60, 227. [Google Scholar] [CrossRef]
- Dégh, L.; Vázsonyi, A. Does the word “Dog” bite? Ostensive action: A means of legend-telling. J. Folk. Res. 1983, 20, 5–34. [Google Scholar]
- Desjardins, M.; Hohl, A.; Delmelle, E. Rapid surveillance of COVID-19 in the United States using a prospective space-time scan statistic: Detecting and evaluating emerging clusters. Appl. Geogr. 2020, 118, 102202. [Google Scholar] [CrossRef]
- DiFonzo, N.; Bourgeois, M.J.; Suls, J.; Homan, C.; Stupak, N.; Brooks, B.P.; Ross, D.S.; Bordia, P. Rumor clustering, consensus, and polarization: Dynamic social impact and self-organization of hearsay. J. Exp. Soc. Psychol. 2013, 49, 378–399. [Google Scholar] [CrossRef]
- Donnellan, M.B.; Oswald, F.L.; Baird, B.M.; Lucas, R. The Mini-IPIP Scales: Tiny-yet-effective measures of the Big Five Factors of Personality. Psychol. Assess. 2006, 18, 192–203. [Google Scholar] [CrossRef]
- Donovan, P. How Idle is Idle Talk? One Hundred Years of Rumor Research. Diogenes 2007, 54, 59–82. [Google Scholar] [CrossRef]
- Duncan, L.A.; Schaller, M.; Park, J.H. Perceived vulnerability to disease: Development and validation of a 15-item self-report instrument. Pers. Individ. Differ. 2009, 47, 541–546. [Google Scholar] [CrossRef]
- Dunn, S.C.; Seaker, R.F.; Waller, M.A. Latent variables in business logistics research: Scale development and val-idation. J. Bus. Logist. 1994, 15, 145–172. [Google Scholar]
- Dutta, S.; Acharya, S.; Shukla, S.; Acharya, N. COVID-19 Pandemic-revisiting the myths. SSRG Int. J. Med. Sci. 2020, 7, 7–10. [Google Scholar] [CrossRef]
- Ellis, B. “Fake news” in the contemporary legend dynamic. J. Am. Folk. 2018, 131, 398–404. [Google Scholar] [CrossRef]
- Faasse, K.; Newby, J. Public Perceptions of COVID-19 in Australia: Perceived Risk, Knowledge, Health-Protective Behaviors, and Vaccine Intentions. Front. Psychol. 2020, 11, 551004. [Google Scholar] [CrossRef]
- Feng, S.; Shen, C.; Xia, N.; Song, W.; Fan, M.; Cowling, B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020, 8, 434–436. [Google Scholar] [CrossRef]
- Fine, G.A. Rumor, Trust and Civil Society: Collective Memory and Cultures of Judgment. Diogenes 2007, 54, 5–18. [Google Scholar] [CrossRef]
- Fine, G.A.; Heath, C. Rumor Mills: The Social Impact of Rumor and Legend; Transaction Publishers: Piscataway, NJ, USA, 2009. [Google Scholar]
- Gibbons, R.D.; Clark, D.C.; Cavanaugh, S.V.; Davis, J.M. Application of modern psychometric theory in psychiatric research. J. Psychiatr. Res. 1985, 19, 43–55. [Google Scholar] [CrossRef]
- Goldberg, L.R. The development of markers for the Big-Five factor structure. Psychol. Assess. 1992, 4, 26–42. [Google Scholar] [CrossRef]
- Fine, G.A.; Goldstein, D.E. Once upon a Virus: AIDS Legends and Vernacular Risk Perception. J. Am. Folk. 2009, 122, 102. [Google Scholar] [CrossRef]
- Golmaryami, F.N.; Vaughan, E.P.; Frick, P.J. Callous-unemotional traits and romantic relationships. Pers. Individ. Differ. 2020, 168, 110408. [Google Scholar] [CrossRef]
- Goode, E.; Ben-Yehuda, N. Moral Panics: The Social Construction of Deviance; Wiley Online Library: Hoboken, NJ, USA, 2010. [Google Scholar]
- Grubaugh, N.D.; Hanage, W.P.; Rasmussen, A.L. Making Sense of Mutation: What D614G Means for the COVID-19 Pandemic Remains Unclear. Cell 2020, 182, 794–795. [Google Scholar] [CrossRef]
- Gruzd, A.; Mai, P. Going viral: How a single tweet spawned a COVID-19 conspiracy theory on Twitter. Big Data Soc. 2020, 7, 2053951720938405. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Black William, C.; Babin Barry, J.; Anderson Rolph, E. Multivariate Data Analysis, 7th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2010. [Google Scholar]
- Haischer, M.H.; Beilfuss, R.; Hart, M.R.; Opielinski, L.; Wrucke, D.; Zirgaitis, G.; Uhrich, T.D.; Hunter, S.K. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLoS ONE 2020, 15, e0240785. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. PROCESS: A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling. 2012. Available online: http://www.afhayes.com/public/process2012.pdf (accessed on 8 August 2020).
- Hayes, A.F. An Index and Test of Linear Moderated Mediation. Multivar. Behav. Res. 2015, 50, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Hayes, A. Partial, conditional, and moderated moderated mediation: Quantification, inference, and interpretation. Commun. Monogr. 2017, 85, 4–40. [Google Scholar] [CrossRef]
- Heaven, P.C.L.; Bucci, S. Right-wing authoritarianism, social dominance orientation and personality: An analysis using the IPIP measure. Eur. J. Pers. 2001, 15, 49–56. [Google Scholar] [CrossRef]
- Heller, J. Rumors and Realities: Making Sense of HIV/AIDS Conspiracy Narratives and Contemporary Legends. Am. J. Public Health 2015, 105, e43–e50. [Google Scholar] [CrossRef]
- Highhouse, S.; Bottrill, K.V. The Influence of Social (Mis)Information on Memory for Behavior in an Employment Interview. Organ. Behav. Hum. Decis. Process. 1995, 62, 220–229. [Google Scholar] [CrossRef]
- Hilbert, M. Toward a synthesis of cognitive biases: How noisy information processing can bias human decision making. Psychol. Bull. 2012, 138, 211–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, T.D.; Gonzalez, K.; Burdette, A.M. The Blood of Christ Compels Them: State Religiosity and State Population Mobility During the Coronavirus (COVID-19) Pandemic. J. Relig. Health 2020, 59, 2229–2242. [Google Scholar] [CrossRef] [PubMed]
- Hinkin, T.R. A review of scale development practices in the study of organizations. J. Manag. 1995, 21, 967–988. [Google Scholar] [CrossRef]
- Hinkin, T.R. Scale development principles and practices. In Research in Organizations: Foundations and Methods of Inquiry; Berrett Koehler: Oakland, CA, USA, 2005; pp. 161–179. [Google Scholar]
- Hulland, J. Use of partial least squares (PLS) in strategic management research: A review of four recent studies. Strateg. Manag. J. 1999, 20, 195–204. [Google Scholar] [CrossRef]
- Huynh, T.D. The more I fear about COVID-19, the more I wear medical masks: A survey on risk perception and medical masks uses. MedRxiv 2020. [Google Scholar] [CrossRef]
- Jaja, I.F.; Anyanwu, M.U.; Jaja, C.-J.I. Social distancing: How religion, culture and burial ceremony undermine the effort to curb COVID-19 in South Africa. Emerg. Microbes Infect. 2020, 9, 1077–1079. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, K.H.; Albarracin, D. The Relation between Media Consumption and Misinformation at the Outset of the SARS-CoV-2 Pandemic in the US; The Harvard Kennedy School Misinformation Review: 2020. Available online: https://misinforeview.hks.harvard.edu/article/the-relation-between-media-consumption-and-misinformation-at-the-outset-of-the-SARS-CoV-2-pandemic-in-the-us/ (accessed on 24 August 2021).
- Jöbges, S.; Vinay, R.; Luyckx, V.A.; Biller-Andorno, N. Recommendations on COVID-19 triage: International comparison and ethical analysis. Bioethics 2020, 34, 948–959. [Google Scholar] [CrossRef]
- Johansson, M.A.; Quandelacy, T.M.; Kada, S.; Prasad, P.V.; Steele, M.; Brooks, J.T.; Slayton, R.B.; Biggerstaff, M.; Butler, J.C. SARS-CoV-2 Transmission from People Without COVID-19 Symptoms. JAMA Netw. Open 2021, 4, e2035057. [Google Scholar] [CrossRef]
- Johnson, J.A. Measuring thirty facets of the Five Factor Model with a 120-item public domain inventory: Development of the IPIP-NEO-120. J. Res. Pers. 2014, 51, 78–89. [Google Scholar] [CrossRef]
- Kavish, N.; Sellbom, M.; Anderson, J.L. Implications for the Measurement of Psychopathy in the DSM–5 Using the Computerized Adaptive Test of Personality Disorder. J. Pers. Assess. 2018, 101, 468–480. [Google Scholar] [CrossRef] [PubMed]
- Keith, M.G.; Tay, L.; Harms, P.D. Systems perspective of Amazon Mechanical Turk for organizational research: Review and recommendations. Front. Psychol. 2017, 8, 1359. [Google Scholar] [CrossRef]
- Khalid, Z.; Yousaf, M.A.; Khan, A.T.-A.; Shakoori, F.R.; Munir, M.; Shakoori, A.R. Debunking Myths about COVID-19, Paranoiac Misconceptions, Recent Developments and its Current Stance. Pak. J. Zool. 2020, 52, 2377. [Google Scholar] [CrossRef]
- Kim, H.-Y. Statistical notes for clinical researchers: Assessing normal distribution (2) using skewness and kurtosis. Restor. Dent. Endod. 2013, 38, 52–54. [Google Scholar] [CrossRef]
- Kitta, A. Alternative Health Websites and Fake News: Taking a Stab at Definition, Genre, and Belief. J. Am. Folk. 2018, 131, 405–412. [Google Scholar] [CrossRef]
- Kitta, A. The Kiss of Death: Contagion, Contamination, and Folklore; University Press of Colorado: Boulder, CO, USA, 2019. [Google Scholar] [CrossRef]
- Kitta, A.; Goldberg, D.S. The significance of folklore for vaccine policy: Discarding the deficit model. Crit. Public Health 2016, 27, 506–514. [Google Scholar] [CrossRef]
- Kline, R.B. Response to Leslie Hayduk’s Review of Principles and Practice of Structural Equation Modeling, 4th Edition. Can. Stud. Popul. 2018, 45, 188–195. [Google Scholar] [CrossRef]
- Klompas, M. Coronavirus Disease 2019 (COVID-19): Protecting Hospitals from the Invisible. Ann. Intern. Med. 2020, 172, 619–620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwon, M.; Kim, D.-J.; Cho, H.; Yang, S. The Smartphone Addiction Scale: Development and Validation of a Short Version for Adolescents. PLoS ONE 2013, 8, e83558. [Google Scholar] [CrossRef] [Green Version]
- Lasisi, T.T.; Eluwole, K.K. Is the weather-induced COVID-19 spread hypothesis a myth or reality? Evidence from the Russian Federation. Environ. Sci. Pollut. Res. 2020, 28, 4840–4844. [Google Scholar] [CrossRef] [PubMed]
- Lelieveld, J.; Helleis, F.; Borrmann, S.; Cheng, Y.; Drewnick, F.; Haug, G.; Klimach, T.; Sciare, J.; Su, H.; Pöschl, U. Model Calculations of Aerosol Transmission and Infection Risk of COVID-19 in Indoor Environments. Int. J. Environ. Res. Public Health 2020, 17, 8114. [Google Scholar] [CrossRef]
- Li, T.; Liu, Y.; Li, M.; Qian, X.; Dai, S.Y. Mask or no mask for COVID-19: A public health and market study. PLoS ONE 2020, 15, e0237691. [Google Scholar] [CrossRef]
- Lobato, E.J.; Powell, M.; Padilla, L.M.; Holbrook, C. Factors predicting willingness to share COVID-19 misinfor-mation. Front. Psychol. 2020, 11, 2413. [Google Scholar] [CrossRef]
- Loftus, E.F. Leading questions and the eyewitness report. Cogn. Psychol. 1975, 7, 560–572. [Google Scholar] [CrossRef]
- Lucas, R.E.; Diener, E.; Suh, E. Discriminant validity of well-being measures. J. Personal. Soc. Psychol. 1996, 71, 616. [Google Scholar] [CrossRef]
- MacCallum, R.C.; Browne, M.W.; Sugawara, H.M. Power analysis and determination of sample size for covariance structure modeling. Psychol. Methods 1996, 1, 130. [Google Scholar] [CrossRef]
- Mahale, P.; Rothfuss, C.; Bly, S.; Kelley, M.; Bennett, S.; Huston, S.L.; Robinson, S. Multiple COVID-19 outbreaks linked to a wedding reception in rural Maine—7 August–14 September 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1686. [Google Scholar] [CrossRef]
- Majra, D.; Benson, J.; Pitts, J.; Stebbing, J. SARS-CoV-2 (COVID-19) superspreader events. J. Infect. 2020, 82, 36–40. [Google Scholar] [CrossRef]
- Maloney, P.W.; Grawitch, M.; Barber, L. The multi-factor structure of the Brief Self-Control Scale: Discriminant validity of restraint and impulsivity. J. Res. Pers. 2012, 46, 111–115. [Google Scholar] [CrossRef]
- Marsh, A.A.; Finger, E.; Mitchell, D.G.V.; Reid, M.E.; Sims, C.; Kosson, D.S.; Towbin, K.E.; Leibenluft, E.; Pine, D.S.; Blair, R.J.R. Reduced Amygdala Response to Fearful Expressions in Children and Adolescents with Callous-Unemotional Traits and Disruptive Behavior Disorders. Am. J. Psychiatry 2008, 165, 712–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathieu, J.E.; Farr, J.L. Further evidence for the discriminant validity of measures of organizational commitment, job involvement, and job satisfaction. J. Appl. Psychol. 1991, 76, 127. [Google Scholar] [CrossRef]
- Maves, R.C.; Downar, J.; Dichter, J.R.; Hick, J.L.; Devereaux, A.; Geiling, J.A.; Kissoon, N.; Hupert, N.; Niven, A.S.; King, M.A. Triage of scarce critical care resources in COVID-19: An implementation guide for regional allocation an expert panel report of the Task Force for Mass Critical Care and the American College of Chest Physicians. Chest 2020, 158, 212–225. [Google Scholar] [CrossRef]
- Mazzoni, G.; Vannucci, M. Hindsight Bias, the Misinformation Effect, and False Autobiographical Memories. Soc. Cogn. 2007, 25, 203–220. [Google Scholar] [CrossRef]
- Papakyriakopoulos, O.; Serrano, J.C.M.; Hegelich, S. The Spread of COVID-19 Conspiracy Theories on Social Media and the Effect of Content Moderation. Harvard Kennedy School Misinformation Review, 2020; p. 1. [CrossRef]
- Paul, S.K.; Chowdhury, P. Strategies for Managing the Impacts of Disruptions During COVID-19: An Example of Toilet Paper. Glob. J. Flex. Syst. Manag. 2020, 21, 283–293. [Google Scholar] [CrossRef]
- Pechorro, P.; Hawes, S.W.; Gonçalves, R.A.; Ray, J.V. Psychometric properties of the inventory of callous-unemotional traits short version (ICU-12) among detained female juvenile offenders and community youths. Psychol. Crime Law 2017, 23, 221–239. [Google Scholar] [CrossRef]
- Petersen, M.B.; Osmundsen, M.; Arceneaux, K. The “need for chaos” and motivations to share hostile political rumors. PsyArXiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Peterson, R.A. A Meta-Analysis of Variance Accounted for and Factor Loadings in Exploratory Factor Analysis. Mark. Lett. 2000, 11, 261–275. [Google Scholar] [CrossRef]
- Porzio, G.; Cortellini, A.; Bruera, E.; Verna, L.; Ravoni, G.; Peris, F.; Spinelli, G. Home Care for Cancer Patients During COVID-19 Pandemic: The Double Triage Protocol. J. Pain Symptom Manag. 2020, 60, e5–e7. [Google Scholar] [CrossRef]
- Preacher, K.J.; Rucker, D.D.; Hayes, A. Addressing Moderated Mediation Hypotheses: Theory, Methods, and Prescriptions. Multivar. Behav. Res. 2007, 42, 185–227. [Google Scholar] [CrossRef]
- QC, I.F. COVID-19: Fear, quackery, false representations and the law. Int. J. Law Psychiatry 2020, 72, 101611. [Google Scholar]
- Ranney, M.L.; Griffeth, V.; Jha, A.K. Critical Supply Shortages—The Need for Ventilators and Personal Protective Equipment during the COVID-19 Pandemic. N. Engl. J. Med. 2020, 382, e41. [Google Scholar] [CrossRef]
- Rasmussen, S.; Sperling, P.; Poulsen, M.S.; Emmersen, J.; Andersen, S. Medical students for health-care staff shortages during the COVID-19 pandemic. Lancet 2020, 395, e79–e80. [Google Scholar] [CrossRef]
- Raykov, T.; Marcoulides, G.A. Introduction to Psychometric Theory; Routlegde: London, UK, 2011. [Google Scholar] [CrossRef]
- Raymond, J.R. The Great Mask Debate: A Debate That Shouldn’t Be a Debate at All. WMJ 2020, 119, 229–239. [Google Scholar] [PubMed]
- Rieger, M.O. To wear or not to wear? Factors influencing wearing face masks in Germany during the COVID-19 pandemic. Soc. Health Behav. 2020, 3, 50. [Google Scholar] [CrossRef]
- Robbins, M.; Francis, L.J.; Edwards, B. Happiness as Stable Extraversion: Internal Consistency Reliability and Construct Validity of the Oxford Happiness Questionnaire Among Undergraduate Students. Curr. Psychol. 2010, 29, 89–94. [Google Scholar] [CrossRef] [Green Version]
- Rosnow, R.L. Rumor as Communication: A Contextualist Approach. J. Commun. 1988, 38, 12–28. [Google Scholar] [CrossRef]
- Rosnow, R.L. Inside rumor: A personal journey. Am. Psychol. 1991, 46, 484. [Google Scholar] [CrossRef]
- Sahoo, S.; Padhy, S.K.; Ipsita, J.; Mehra, A.; Grover, S. Demystifying the myths about COVID-19 infection and its societal importance. Asian J. Psychiatry 2020, 54, 102244. [Google Scholar] [CrossRef]
- Samore, T.; Fessler, D.M.T.; Sparks, A.M.; Holbrook, C. Of pathogens and party lines: Social conservatism positively associates with COVID-19 precautions among U.S. Democrats but not Republicans. PLoS ONE 2021, 16, e0253326. [Google Scholar] [CrossRef]
- Sanfilippo, F.; Bignami, E.; Lorini, L.F.; Astuto, M. The importance of a “socially responsible” approach during COVID-19: The invisible heroes of science in Italy. Crit. Care 2020, 24, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Satici, B.; Gocet-Tekin, E.; Deniz, M.E.; Satici, S.A. Adaptation of the Fear of COVID-19 Scale: Its Association with Psychological Distress and Life Satisfaction in Turkey. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef]
- Schmidt, F.L.; Le, H.; Ilies, R. Beyond alpha: An empirical examination of the effects of different sources of meas-urement error on reliability estimates for measures of individual-differences constructs. Psychol. Methods 2003, 8, 206–224. [Google Scholar] [CrossRef] [Green Version]
- Sell, T.K.; Hosangadi, D.; Trotochaud, M. Misinformation and the US Ebola communication crisis: Analyzing the veracity and content of social media messages related to a fear-inducing infectious disease outbreak. BMC Public Health 2020, 20, 1–10. [Google Scholar] [CrossRef]
- Shahsavari, S.; Holur, P.; Wang, T.; Tangherlini, T.R.; Roychowdhury, V. Conspiracy in the time of corona: Auto-matic detection of emerging COVID-19 conspiracy theories in social media and the news. J. Comput. Soc. Sci. 2020, 3, 279–317. [Google Scholar] [CrossRef]
- Singh, L.; Bansal, S.; Bode, L.; Budak, C.; Chi, G.; Kawintiranon, K.; Padden, C.; Vanarsdall, R.; Vraga, E.; Wang, Y. A first look at COVID-19 information and misinformation sharing on Twitter. arXiv 2020, arXiv:2003.13907. [Google Scholar]
- Sobering, K. Watercooler Democracy: Rumors and Transparency in a Cooperative Workplace. Work. Occup. 2019, 46, 411–440. [Google Scholar] [CrossRef]
- Steffens, M.S.; Dunn, A.G.; Wiley, K.E.; Leask, J. How organisations promoting vaccination respond to misinfor-mation on social media: A qualitative investigation. BMC Public Health 2019, 19, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stephens, M. A geospatial infodemic: Mapping Twitter conspiracy theories of COVID-19. Dialogues Hum. Geogr. 2020, 10, 276–281. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2007; Volume 5. [Google Scholar]
- Tang, J.W.; Bahnfleth, W.P.; Bluyssen, P.M.; Buonanno, G.; Jimenez, J.L.; Kurnitski, J.; Li, Y.; Miller, S.; Sekhar, C.; Morawska, L. Dismantling myths on the airborne transmission of severe acute respiratory syndrome coronavirus (SARS-CoV-2). J. Hosp. Infect. 2021, 110, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Tangherlini, T.R.; Shahsavari, S.; Shahbazi, B.; Ebrahimzadeh, E.; Roychowdhury, V. An automated pipeline for the discovery of conspiracy and conspiracy theory narrative frameworks: Bridgegate, Pizzagate and storytelling on the web. PLoS ONE 2020, 15, e0233879. [Google Scholar] [CrossRef]
- Taylor, L. COVID-19 misinformation sparks threats and violence against doctors in Latin America. BMJ 2020, 370, m3088. [Google Scholar] [CrossRef]
- Celenay, S.T.; Karaaslan, Y.; Mete, O.; Kaya, D.O. Coronaphobia, musculoskeletal pain, and sleep quality in stay-at home and continued-working persons during the 3-month COVID-19 pandemic lockdown in Turkey. Chronobiol. Int. 2020, 37, 1778–1785. [Google Scholar] [CrossRef]
- Truog, R.D.; Mitchell, C.; Daley, G.Q. The Toughest Triage—Allocating Ventilators in a Pandemic. N. Engl. J. Med. 2020, 382, 1973–1975. [Google Scholar] [CrossRef]
- Van Der Linden, S.; Roozenbeek, J.; Compton, J. Inoculating Against Fake News About COVID-19. Front. Psychol. 2020, 11, 566790. [Google Scholar] [CrossRef] [PubMed]
- Van Mulukom, V.; Pummerer, L.; Alper, S.; Cavojova, V.; Farias, J.E.M.; Kay, C.S.; Lazarevic, L.; Lobato, E.J.C.; Marinthe, G.; Banai, I.P. Antecedents and consequences of COVID-19 conspiracy theories: A rapid review of the evidence. PsyArXiv 2020. [Google Scholar] [CrossRef]
- Van Trijp, H.C.; Steenkamp, J.-B.E. Consumers’ variety seeking tendency with respect to foods: Measurement and managerial implications. Eur. Rev. Agric. Econ. 1992, 19, 181–195. [Google Scholar] [CrossRef]
- Wang, P.-W.; Hsiao, R.C.; Chen, L.M.; Sung, Y.-H.; Hu, H.-F.; Yen, C.-F. Associations between callous-unemotional traits and various types of involvement in school bullying among adolescents in Taiwan. J. Formos. Med. Assoc. 2018, 118, 50–56. [Google Scholar] [CrossRef]
- Wang, Y.; McKee, M.; Torbica, A.; Stuckler, D. Systematic literature review on the spread of health-related misin-formation on social media. Soc. Sci. Med. 2019, 240, 1–12. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Personal. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- West, S.G.; Finch, J.F.; Curran, P.J. Structural equation models with nonnormal variables: Problems and remedies. In Structural Equation Modeling: Concepts, Issues, and Applications; Sage Publications: Thousand Oaks, CA, USA, 1995; pp. 56–75. [Google Scholar]
- White, D.B.; Lo, B. A Framework for Rationing Ventilators and Critical Care Beds During the COVID-19 Pandemic. JAMA 2020, 323, 1773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Coronavirus Disease (COVID-19) Advice for the Public. Mythbusters. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters (accessed on 23 November 2020).
- Worthington, R.L.; Whittaker, T.A. Scale development research: A content analysis and recommendations for best practices. Couns. Psychol. 2006, 34, 806–838. [Google Scholar] [CrossRef]
- Wright, A.G.C.; Simms, L.J. On the structure of personality disorder traits: Conjoint analyses of the CAT-PD, PID-5, and NEO-PI-3 trait models. Pers. Disord. Theory Res. Treat. 2014, 5, 43–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, S.; Jiang, J.; Pal, A.; Yu, K.; Chen, F.; Yu, S. Analysis and Insights for Myths Circulating on Twitter During the COVID-19 Pandemic. IEEE Open J. Comput. Soc. 2020, 1, 209–219. [Google Scholar] [CrossRef]

| Study 1 | Study 2 | Study 3 | Study 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Kaiser–Meyer–Olkin Measure of Sampling Adequacy | 0.974 | 0.970 | 0.971 | 0.973 | ||||
| Bartlett’s Test of Sphericity | χ2(66) = 6889.146 | *** | χ2(66) = 7019.133 | *** | χ2(66) = 6270.147 | *** | χ2(66) = 7460.664 | *** |
| Study 1 (N = 597) | Study 2 (N = 651) | Study 3 (N = 583) | Study 4 (N = 602) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alpha = 0.964 | Alpha = 0.959 | Alpha = 0.960 | Alpha = 0.965 | ||||||||||
| Item | M | (SD) | Factor Loading | M | (SD) | Factor Loading | M | (SD) | Factor Loading | M | (SD) | Factor Loading | |
| (1) | 5G mobile networks spread COVID-19 | 1.70 | (1.20) | 0.850 | 1.61 | (1.06) | 0.815 | 1.73 | (1.19) | 0.831 | 1.61 | (1.14) | 0.881 |
| (2) | COVID-19 will go away with cold weather | 1.79 | (1.20) | 0.871 | 1.74 | (1.13) | 0.878 | 1.85 | (1.24) | 0.862 | 1.65 | (1.13) | 0.893 |
| (3) | As a foreign disease, only foreigners can catch COVID-19 | 1.63 | (1.20) | 0.895 | 1.53 | (1.08) | 0.894 | 1.71 | (1.21) | 0.899 | 1.49 | (1.11) | 0.926 |
| (4) | Drinking bleach will prevent COVID-19 infection | 1.61 | (1.19) | 0.875 | 1.57 | (1.12) | 0.888 | 1.71 | (1.18) | 0.862 | 1.49 | (1.09) | 0.893 |
| (5) | Consuming garlic will prevent COVID-19 contraction | 1.95 | (1.28) | 0.867 | 1.90 | (1.20) | 0.840 | 2.02 | (1.27) | 0.832 | 1.81 | (1.20) | 0.865 |
| (6) | Adding pepper to meals will prevent COVID-19 infection | 1.78 | (1.21) | 0.892 | 1.75 | (1.15) | 0.869 | 1.86 | (1.25) | 0.862 | 1.64 | (1.14) | 0.881 |
| (7) | Hydroxychloroquine is a sure defense from COVID-19 contraction | 2.25 | (1.31) | 0.720 | 2.29 | (1.25) | 0.701 | 2.30 | (1.29) | 0.705 | 2.12 | (1.23) | 0.700 |
| (8) | Drinking hard liquor protects you from COVID-19 infection | 1.79 | (1.24) | 0.877 | 1.71 | (1.15) | 0.874 | 1.81 | (1.22) | 0.880 | 1.61 | (1.12) | 0.875 |
| (9) | Hand dryers kill the COVID-19 virus | 2.03 | (1.21) | 0.790 | 2.04 | (1.17) | 0.756 | 2.06 | (1.21) | 0.775 | 1.94 | (1.14) | 0.774 |
| (10) | If you do not believe COVID-19 exists you will not contract it | 1.66 | (1.17) | 0.877 | 1.62 | (1.17) | 0.886 | 1.80 | (1.22) | 0.877 | 1.57 | (1.16) | 0.921 |
| (11) | If you can hold your breath for a prolonged period, you are COVID-19 virus-free | 1.77 | (1.23) | 0.875 | 1.73 | (1.15) | 0.832 | 1.88 | (1.20) | 0.846 | 1.65 | (1.10) | 0.854 |
| (12) | Houseflies spread COVID-19 | 2.06 | (1.20) | 0.772 | 2.06 | (1.15) | 0.708 | 2.10 | (1.26) | 0.777 | 1.99 | (1.13) | 0.728 |
| Frequency Believe Not True | Percent Believe Not True | Mean | SD | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|
| Item 1 | 2155 | 88.57% | 1.66 | (1.15) | 1.59 | 1.30 |
| Item 2 | 2114 | 86.89% | 1.76 | (1.17) | 1.31 | 0.44 |
| Item 3 | 2132 | 87.63% | 1.59 | (1.15) | 1.76 | 1.67 |
| Item 4 | 2139 | 87.92% | 1.59 | (1.14) | 1.77 | 1.71 |
| Item 5 | 2043 | 83.97% | 1.92 | (1.24) | 1.03 | −0.27 |
| Item 6 | 2113 | 86.85% | 1.76 | (1.19) | 1.36 | 0.58 |
| Item 7 | 1973 | 81.09% | 2.24 | (1.27) | 0.53 | −0.93 |
| Item 8 | 2119 | 87.09% | 1.73 | (1.18) | 1.44 | 0.82 |
| Item 9 | 2082 | 85.57% | 2.02 | (1.18) | 0.86 | −0.40 |
| Item 10 | 2124 | 87.30% | 1.66 | (1.18) | 1.66 | 1.40 |
| Item 11 | 2122 | 87.22% | 1.76 | (1.17) | 1.34 | 0.46 |
| Item 12 | 2105 | 86.52% | 2.05 | (1.18) | 0.78 | −0.47 |
| Demographic Characteristics | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Male | 839 | 34.48 |
| Female | 1594 | 65.52 |
| Age range (years) | ||
| 18–29 | 467 | 19.19 |
| 30–39 | 762 | 31.34 |
| 40–49 | 519 | 21.33 |
| 50–59 | 399 | 16.4 |
| 60 and over | 286 | 11.76 |
| Household Income | ||
| Less than $10,000 | 111 | 4.56 |
| $10,000–19,999 | 172 | 7.07 |
| $20,000–29,999 | 240 | 9.86 |
| $30,000–39,999 | 325 | 13.36 |
| $40,000–49,999 | 276 | 11.34 |
| $50,000–59,999 | 349 | 14.34 |
| $60,000–69,999 | 186 | 7.64 |
| $70,000–79,999 | 177 | 7.27 |
| $80,000–89,999 | 152 | 6.25 |
| $90,000–99,999 | 131 | 5.38 |
| $100,000 and over | 314 | 12.91 |
| Ethnicity | ||
| Caucasian | 1915 | 78.71 |
| Hispanic/Latino | 118 | 4.85 |
| African American | 208 | 8.55 |
| Native American | 26 | 1.07 |
| Asian | 126 | 5.18 |
| Other | 40 | 1.64 |
| Study 1 | Study 2 | Study 3 | Study 4 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | M | (SD) | r | M | (SD) | r | M | (SD) | r | M | (SD) | r | ||||
| Fear of COVID-19 | 3.52 | −1.72 | 0.506 | *** | 3.37 | −1.64 | 0.487 | *** | 3.56 | −1.61 | 0.565 | *** | 3.3 | −1.61 | 0.486 | *** |
| Callousness | – | – | – | – | – | – | 3.03 | −1.26 | 0.789 | *** | 2.35 | −1.43 | 0.736 | *** | ||
| Conscientious | 5.06 | −1.05 | −0.408 | *** | 5 | −0.96 | −0.422 | *** | – | – | – | – | – | – | – | |
| Conservatism | 4.43 | −0.95 | 0.164 | *** | 4.37 | −0.92 | 0.139 | *** | – | – | – | – | – | – | – | |
| Generic Conspiracy Belief Scale | 2.82 | −1.01 | 0.605 | *** | 2.88 | −0.99 | 0.556 | *** | – | – | – | – | – | – | – | |
| PANAS | – | – | – | 1.25 | −1.38 | −0.168 | *** | – | – | – | – | – | – | – | ||
| Perceived Vulnerability to Disease | – | 4.31 | −0.8 | −0.092 | *** | 4.33 | −0.84 | −0.106 | *** | |||||||
| Variety Seeking | – | 4.51 | −1.08 | −0.186 | *** | – | – | – | ||||||||
| Risk Taking | – | 2.73 | −1.54 | 0.75 | *** | 2.37 | −1.45 | 0.678 | *** | |||||||
| Compassion | – | 5.46 | −1.1 | −0.55 | *** | |||||||||||
| Wearing a Mask in Public | – | 6.36 | −1.19 | −0.301 | *** | |||||||||||
| Demographic Characteristics | ||||||||||||||||
| Gender (Female) | 1.66 | −0.48 | −0.265 | *** | 1.66 | −0.47 | −0.172 | *** | 1.64 | −0.48 | −0.284 | *** | 1.66 | −0.48 | −0.279 | *** |
| Age | 42.34 | −13.45 | −0.158 | *** | 41.25 | −12.93 | −0.123 | *** | 41.97 | −13.34 | −0.183 | *** | 41.06 | −13.28 | −0.077 | *** |
| College Degree | 0.71 | −0.45 | 0.218 | *** | 0.69 | −0.46 | 0.147 | *** | 0.72 | −0.45 | 0.258 | *** | 0.69 | −0.46 | 0.121 | ** |
| Average Weekly News (Hours) | 4.13 | −2.65 | 0.166 | *** | 3.68 | −2.64 | 0.242 | *** | 3.99 | −2.62 | 0.233 | *** | 3.62 | −2.66 | 0.184 | *** |
| Religiosity | 4.58 | −1.93 | 0.339 | *** | 4.25 | −1.93 | 0.339 | *** | 4.63 | −1.85 | 0.295 | *** | 4.22 | −1.99 | 0.317 | *** |
| Outcome | ||||||||
|---|---|---|---|---|---|---|---|---|
| COVID-19 Transmission Misinformation Beliefs | Wearing a Mask in Public | |||||||
| Antecedent | Coeff. | SE | t | p | Coeff. | SE | t | p |
| Fear of COVID-19 | 0.128 | 0.014 | 8.973 | <0.0001 | 0.265 | 0.031 | 8.456 | <0.0001 |
| COVID-19 Transmission Misinformation Scale (CTMS) | — | — | — | — | −0.617 | 0.084 | −7.315 | <0.0001 |
| Callousness | 0.295 | 0.018 | 16.223 | <0.0001 | −0.156 | 0.045 | −3.486 | <0.001 |
| Fear of COVID−19 x Callousness | 0.124 | 0.009 | 14.202 | <0.0001 | 0.118 | 0.021 | 5.678 | <0.0001 |
| Covariates | ||||||||
| Gender (female) | −0.16 | 0.047 | −3.407 | <0.001 | 0.139 | 0.097 | 1.429 | 0.154 |
| Age | −0.001 | 0.002 | −0.46 | 0.645 | 0 | 0.003 | −0.096 | 0.924 |
| College Degree | −0.044 | 0.046 | −0.954 | 0.34 | 0.07 | 0.094 | 0.747 | 0.456 |
| Weekly Hours of News (Average) | −0.008 | 0.009 | −0.964 | 0.336 | 0.023 | 0.018 | 1.321 | 0.187 |
| Religiosity | 0.057 | 0.011 | 5.11 | <0.0001 | −0.051 | 0.023 | −2.21 | <0.05 |
| Model Summary | R2 = 0.727 | R2 = 0.246 | ||||||
| F(8, 593) = 197.227, p < 0.0001 | F(9, 592) = 21.502, p < 0.0001 | |||||||
| Left-Leaning | Average | Right-Leaning | |
|---|---|---|---|
| Low (−1 SD) | Mean | High (+1 SD) | |
| Fear of COVID-19 → Wearing a Mask in Public | −0.040 (LLCI − 0.077 ULCI − 0.002) | 0.085 (LLCI 0.056 ULCI 0.114) | .333 (LLCI 0.295 ULCI 0.372) |
| Fear of COVID-19 → CTMS | 0.106 (LLCI 0.029 ULCI 0.183) | 0.224 (LLCI 0.163 ULCI 0.285) | .460 (LLCI 0.363 ULCI 0.557) |
| Fear of COVID-19 → CTMS → Wearing a Mask in Public | 0.024 (LLCI 0.003 ULCI 0.051) | −0.052 (LLCI − 0.077 ULCI − 0.032) | −0.206 (LLCI − 0.287 ULCI − 0.143) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bok, S.; Martin, D.E.; Acosta, E.; Lee, M.; Shum, J. Validation of the COVID-19 Transmission Misinformation Scale and Conditional Indirect Negative Effects on Wearing a Mask in Public. Int. J. Environ. Res. Public Health 2021, 18, 11319. https://doi.org/10.3390/ijerph182111319
Bok S, Martin DE, Acosta E, Lee M, Shum J. Validation of the COVID-19 Transmission Misinformation Scale and Conditional Indirect Negative Effects on Wearing a Mask in Public. International Journal of Environmental Research and Public Health. 2021; 18(21):11319. https://doi.org/10.3390/ijerph182111319
Chicago/Turabian StyleBok, Stephen, Daniel E. Martin, Erik Acosta, Maria Lee, and James Shum. 2021. "Validation of the COVID-19 Transmission Misinformation Scale and Conditional Indirect Negative Effects on Wearing a Mask in Public" International Journal of Environmental Research and Public Health 18, no. 21: 11319. https://doi.org/10.3390/ijerph182111319






