Development and Evaluation of a Preceptor Education Program Based on the One-Minute Preceptor Model: Participatory Action Research
Abstract
:1. Introduction
- What is the implementation process for the development and application of the OMP model-based PEP through PAR?
- What effect does the PEP that is based on the OMP model through PAR have on preceptor nurses?
- What are the experiences of preceptor nurses who participated in the development and application of the OMP model-based PEP through PAR?
2. Materials and Methods
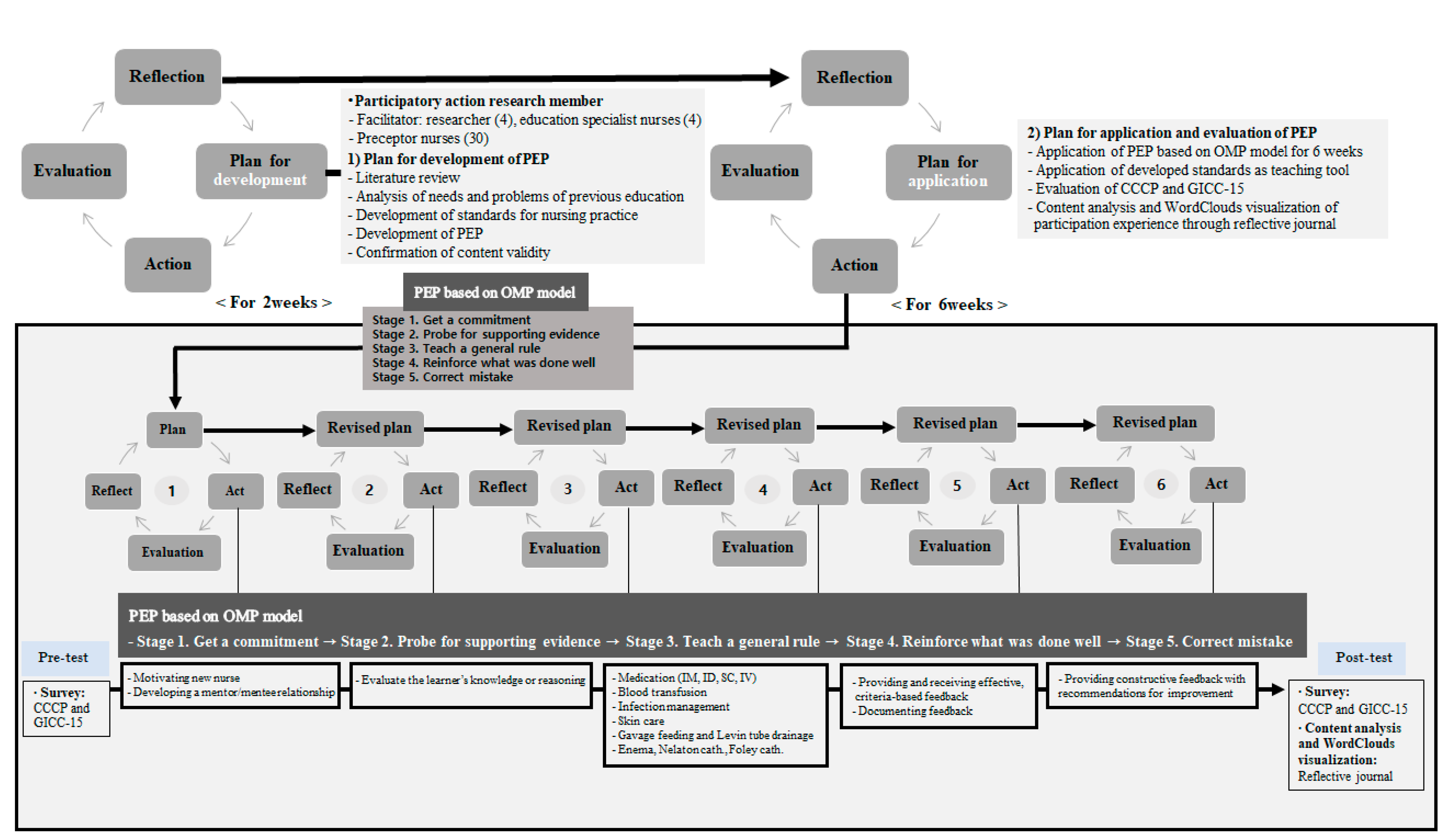
2.1. Study Design
2.2. Participants
2.3. Research Procedure
2.3.1. Development of the PEP
2.3.2. Application of PEP
2.4. Data Collection and Analysis
2.4.1. Data Collection
2.4.2. Data Analysis
2.5. Rigor
2.6. Ethical Consideration
3. Results
3.1. General Characteristics of the Participants
3.2. The OMP-Based PEP’s Effect
3.3. The Experience of Participants throughout Content Analysis of the Reflective Journals
3.4. Feelings and Thoughts about Preceptorship throughout Frequency Analysis of Keywords about Reflective Journals
4. Discussion
4.1. PAR Approach for Development and Application of OMP-Based PEP
4.2. Evaluation of OMP-Based PEP throughout Quantitative and Qualitative Analysis
4.3. Participation Experience of OMP-Based PEP
4.4. Implications for Practice
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kyunghyang Newspaper. Available online: https://m.khan.co.kr/national/health-welfare/article/202101130600015#c2b (accessed on 8 August 2021).
- Hussein, R.; Everett, B.; Ramjan, L.M.; Hu, W.; Salamonson, Y. New graduate nurses’ experiences in a clinical specialty: A follow up study of newcomer perceptions of transitional support. BMC Nurs. 2017, 16, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Welfare MoHa. Ministry of Health and Welfare Announced Measures for Improving Working Environment and Treatment of Nurses. Korea Policy Briefing. 2018. Available online: https://www.korea.kr/news/pressReleaseView.do?newsId=156259453 (accessed on 8 August 2021).
- Salyers, M.P.; Bonfils, K.A.; Luther, L.; Firmin, R.L.; White, D.A.; Adams, E.L.; Rollins, A.L. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis. J. Gen. Intern. Med. 2017, 32, 475–482. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, J.K.; Park, K.O. The Role Experience of Preceptor Nurses in Hospitals. J. Korean Acad. Nurs. Adm. 2012, 18, 33–45. [Google Scholar] [CrossRef] [Green Version]
- Ward, A.E.; McComb, S.A. Formalising the precepting process: A concept analysis of preceptorship. J. Clin. Nurs. 2018, 27, e873–e881. [Google Scholar] [CrossRef] [PubMed]
- Clipper, B.; Cherry, B. From Transition Shock to Competent Practice: Developing Preceptors to Support New Nurse Transition. J. Contin. Educ. Nurs. 2015, 46, 448–454. [Google Scholar] [CrossRef] [Green Version]
- Ji, E.A.; Kim, J.S. Factor Influencing New Graduate Nurses’ Turnover Intention according to Length of Service. J. Korean Acad. Nurs. Adm. 2018, 24, 51–60. [Google Scholar] [CrossRef]
- Cho, Y.S.; Sohn, S.K.; Han, M.Y.; Kim, M.S.; Bang, B.K.; Lee, K.M. Nurses’ lived Experience of Preceptorship for Newly Graduated Nurses in Hospital. J. East-West Nurs. Res. 2014, 20, 37–47. [Google Scholar] [CrossRef]
- Omansky, G.L. Staff nurses’ experiences as preceptors and mentors: An integrative review. J. Nurs. Manag. 2010, 18, 697–703. [Google Scholar] [CrossRef]
- Shin, S.; Kim, J.; Kang, Y.; Roh, Y.; Jeong, S.; Hwang, E. The experiences of difficulties for nurses in clinical education. J. Qual. Res. 2018, 19, 40–47. [Google Scholar] [CrossRef]
- Han, J.; Yoo, E.K. The study of preceptor nurses’ occupational stress and burden. Korean J. Stress Res. 2018, 26, 38–45. [Google Scholar] [CrossRef] [Green Version]
- Kang, C.M.; Chiu, H.T.; Lin, Y.K.; Chang, W.Y. Development of a situational initiation training program for preceptors to retain new graduate nurses: Process and initial outcomes. Nurse Educ. Today 2016, 37, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Baltimore, J.J. The hospital clinical preceptor: Essential preparation for success. J. Contin. Educ. Nurs. 2004, 35, 133–140. [Google Scholar] [CrossRef] [Green Version]
- Shin, N.Y.; Lee, S.S.; Park, M.J.; Park, Y.M.; Kim, S.K.; Nam, G.H. Development and Validation of a Education Nurse Specialist-Led Education Satisfaction Scale for Nurses Working at Comprehensive Nursing Care Service Wards. J. Korean Clin. Nurs. Res. 2020, 26, 285–295. [Google Scholar] [CrossRef]
- Kwon, S.H.; Kim, S.H.; Jung, S.Y.; Mo, M.H.; Chun, Y.M.; Hong, S.Y.; lee, W.S.; Park, J.; Park, J.H.; Son, J.T.; et al. Core nursing skills and suggestions for improvement in clinical teaching for new graduate nurses as recognized by clinical nurse educators. J. Korean Data Inf. Sci. Soc. 2021, 32, 309–324. [Google Scholar] [CrossRef]
- Salerno, S.M.; O’Malley, P.G.; Pangaro, L.N.; Wheeler, G.A.; Moores, L.K. Jackson, J.L. Faculty development seminars based on the one-minute preceptor improve feedback in the ambulatory setting. J. Gen. Intern. Med. 2002, 17, 779–787. [Google Scholar] [CrossRef] [Green Version]
- Gallagher, P.; Tweed, M.; Hanna, S.; Winter, H.; Hoare, K. Developing the One-Minute Preceptor. Clin. Teach. 2012, 9, 358–362. [Google Scholar] [CrossRef]
- Neher, J.O.; Gordon, K.C.; Meyer, B.; Stevens, N. A five-step “microskills” model of clinical teaching. J. Am. Board Fam. Pract. 1992, 5, 419–424. [Google Scholar]
- Irby, D.M.; Aagaard, E.; Teherani, A. Teaching points identified by preceptors observing one-minute preceptor and traditional preceptor encounters. Acad. Med. 2004, 79, 50–55. [Google Scholar] [CrossRef]
- Shagholi, R.; Abadi, S.E.; Moghaddasi, A.; Sayyadee, T.; Tayefi, M. Teaching Strategy of One Minute Preceptor and its Approaches in the Past Two Decades: Systematic Review. Rev. Clin. Med. 2018, 5, 123–131. [Google Scholar] [CrossRef]
- Toulmin, S.; Gustavsen, B. Beyond Theory: Changing Organizations through Participation; Toulmin, S., Gustavsen, B., Eds.; John Benjamins North America: Herndon, VA, USA, 1996; Volume viii, p. 233. ISBN 9789027217721. [Google Scholar]
- Bate, P. Synthesizing Research and Practice: Using the Action Research Approach in Health Care Settings. Soc. Policy Adm. 2000, 34, 478–493. [Google Scholar] [CrossRef]
- Pine, L.; Patricia, M. The Domain of Nursing: Developing Practice through Action Research in the Intensive Care Unit. 2008. Available online: http://hdl.handle.net/10063/903 (accessed on 8 August 2021).
- Shin, S.; Park, Y.W.; Kim, M.; Kim, J.; Lee, I. Survey on the Education System for New Graduate Nurses in Hospitals: Focusing on the Preceptorship. Korean Med. Educ. Rev. 2019, 21, 112–122. [Google Scholar] [CrossRef]
- Kim, H.Y.; Park, J.; Ryu, S.Y.; Choi, S.W.; Han, M.A. The effects of preceptors’ transformational leadership on job stress and clinical performance among new graduate nurses. Health Policy Manag. 2012, 22, 347–364. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.Y.; Kim, I.S. Experience of Preceptorship for Newly Employed Nurses. J. Korean Clin. Nurs. Res. 2005, 10, 75–88. [Google Scholar]
- Zuber-Skerritt, O.; Fletcher, M.A. The quality of an action research thesis in the social sciences. Qual. Assur. Educ. 2007, 15, 413–416. [Google Scholar] [CrossRef]
- Zuber-Skerritt, O.; Perry, C. Action research within organisations and university thesis writing. Learn. Organ. 2002, 9, 171–179. [Google Scholar] [CrossRef]
- Kwon, I.G.; Jung, K.H.; Cho, H.S.; Hwang, J.W.; Kim, J.Y.; Jeon, K.O.; Sung, Y.H. Development and Validation of the Core Competency Evaluation Tool for New Graduate Nurse’s Preceptor. J. Korean Acad. Nurs. Adm. 2002, 8, 535–549. [Google Scholar]
- Rubin, R.B.; Martin, M.M.; Bruning, S.S.; Powers, D.E. Test of a self-efficacy model of interpersonal communication competence. Commun. Q 1993, 41, 210–220. [Google Scholar] [CrossRef]
- Hur, G.H. Construction and validation of a global interpersonal communication competence scale. Korean J. Commun. Stud. 2003, 47, 380–408. [Google Scholar]
- Krippendorff, K. Content Analysis: An. Introduction to Its Methodology, 4th ed.; Sage Publications: Thousand Oaks, CA, USA, 2018; ISBN 9781506395661. [Google Scholar]
- Guba, E.G.; Lincoln, Y.S. Effective Evaluation: Improving the Usefulness of Evaluation Results through Responsive and Naturalistic Approaches; Jossey Bass Inc.: San Francisco, CA, USA, 1981; ISBN 1555424422. [Google Scholar]
- Moon, J.E.; Song, M.O.; Kim, H.Y.; Park, H.Y.; Kim, E.A.; Kim, Y.M.; Jang, K.S. Action Research in Hospital Settings: A Literature Review of International Nursing Journals. J. Korean Acad. Nurs. Adm. 2013, 19, 95–107. [Google Scholar] [CrossRef] [Green Version]
- Lingard, L.; Albert, M.; Levinson, W. Grounded theory, mixed methods, and action research. BMJ 2008, 337, a567. [Google Scholar] [CrossRef]
- Kang, Y.M.; Eun, Y. The Effects of Self-efficacy, Critical Thinking Disposition, Self-leadership, and Communication Competency on the Core Competencies of the Preceptor in Advanced General Hospitals. J. Korean Acad. Soc. Nurs. Educ. 2018, 24, 279–289. [Google Scholar] [CrossRef] [Green Version]
- Im, S.; Kim, E.K. Interpersonal Communication Competence and Difficult Communication Experiences of Preceptor Nurses. J. Korean Acad. Psychiatr. Ment. Health Nurs. 2008, 17, 471–480. [Google Scholar]
- Gatewood, E.; De Gagne, J.C. The one-minute preceptor model: A systematic review. J. Am. Assoc. Nurse Pract. 2019, 31, 46–57. [Google Scholar] [CrossRef] [PubMed]
- Jeoung, Y.O.; Park, S.C.; Jin, J.K.; Kim, J.Y.; Lee, J.U.; Park, S.Y.; Sok, S. Content Analysis of Communication between Nurses during Preceptorship. J. Korean Acad. Psychiatr. Ment. Health Nurs. 2014, 23, 82–92. [Google Scholar] [CrossRef] [Green Version]
- Korea Nurses Association. Guideline on the Education System for New Graduate Nurses in Hospitals; Korean Nurses Association: Seoul, Korea, 2019; Available online: http://www.nursenews.co.kr/main/ArticleDetailView.asp?sSection=57&idx=24574&intPage=21 (accessed on 8 August 2021).
- Kim, J.Y.; Kim, Y.S.; Kim, C.S.; Park, H.S.; Sin, M.Y.; Yun, Y.S.; Jo, Y.S.; Park, M.M.; Yoo, M.S. A Comparison of Preceptors’ and New Graduate Nurses’ Perception of Teaching Effectiveness. J. Korean Acad. Nurs. Adm. 2009, 15, 193–202. [Google Scholar]
- Dosser, I.; Kennedy, C. Improving family carers’ experiences of support at the end of life by enhancing communication: An action research study. Int. J. Palliat. Nurs. 2014, 20, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Coghlan, D. Doing Action Research in Your Own Organization, 5th ed.; SAGE Publications Ltd.: London, UK, 2019; 240p, ISBN 9781526458827. [Google Scholar]

| Characteristics | Categories | N (%) | Mean (SD) |
|---|---|---|---|
| Age (years) | <30 | 20 (66.7) | 28.8 ± 2.30 |
| ≥30 | 10 (33.3) | ||
| Sex | Men | 1 (3.3) | |
| Women | 29 (96.7) | ||
| Marital status | Single | 26 (86.7) | |
| Married | 4 (13.3) | ||
| Types of religion | Protestantism | 5 (16.7) | |
| Catholicism | 3 (10.0) | ||
| None | 21 (70.0) | ||
| Others | 1 (3.3) | ||
| Total working career (years) | ≤3 | 10 (33.3) | |
| 4–5 | 11 (36.7) | ||
| ≥6 | 9 (30.0) | ||
| Present unit career (years) | <3 | 6 (20.0) | |
| 3–4 | 12 (40.0) | ||
| ≥5 | 12 (40.0) | ||
| Work unit | Ward | 13 (43.3) | |
| Intensive care unit | 17 (56.7) | ||
| Preceptor experience | Yes | 17 (56.7) | |
| No | 13 (43.3) | ||
| Reason of preceptor | Recommendation from unit manager | 30 (100.0) | |
| Voluntary | 0 (0) |
| Variables | Pre-Test Mean (SD) | Post-Test Mean (SD) | t | p |
|---|---|---|---|---|
| Clinical Core Competency of Preceptors (CCCP) | 3.74 ± 0.42 | 3.76 ± 0.32 | 0.29 | 0.777 |
| Role model | 3.91 ± 0.43 | 3.89 ± 0.34 | 0.35 | 0.733 |
| Facilitator | 3.65 ± 0.50 | 3.69 ± 0.42 | 0.45 | 0.655 |
| Educator | 3.69 ± 0.40 | 3.72 ± 0.35 | 0.42 | 0.675 |
| Learning needs assessment | 3.76 ± 0.50 | 3.78 ± 0.35 | 0.26 | 0.794 |
| Learning experience planning | 3.52 ± 0.56 | 3.53 ± 0.53 | 0.06 | 0.954 |
| Learning plan implementation | 3.75 ± 0.42 | 3.83 ± 0.39 | 0.84 | 0.410 |
| Job performance evaluation | 3.55 ± 0.62 | 3.50 ± 0.54 | 0.45 | 0.655 |
| General Interpersonal Communication Competence (GICC-15) | 3.46 ± 0.45 | 3.43 ± 0.30 | 0.44 | 0.666 |
| Category | Subcategory | Quotation |
|---|---|---|
| Designated as a preceptor without preparation | Designated preceptor owing to the sudden resignation of a fellow nurse | Rather than participating voluntarily; I got the preceptor job really suddenly. As a fellow nurse who was supposed to be a preceptor resigned, I was designated owing to similarity in age with the previous preceptor.—Participant 3 |
| Designated preceptor owing to turnover | Since it was my turn, I had no choice but to become a preceptor.—Participant 8 | |
| Designated preceptor owing to same work duties as new nurses | The preceptor had the rotation of departments, and I had to fill the vacant position. That day, I was assigned because I had the same work schedule as a new nurse.—Participant 2 | |
| Designated preceptor owing to the suggestion of the unit manager | The head nurse told me to do it by designation, but I could not refuse. A preceptor is not something you can do selectively.—Participant 6 | |
| Commitment to do well | Commitment within the PAR team | The pledge within the practice research team to help for my preceptorship made me resolve to work even harder.—Participant 4 |
| Pledge with the preceptor | Not a promise I made alone, but a promise I made with someone made me teach more responsibly.—Participant 10 | |
| Camaraderie | Strong support team | When we got together concurrently every week and had time to look back on our preceptor activities for the week, I thought we were going together, not alone.—Participant 23 |
| Formation of consensus among preceptors | Listening to the stories of nurses doing preceptor with me, it was comforting to know that it was not just my problem, but that everyone faces the same difficulties.—Participant 8 | |
| Growth | Opportunities for learning | I was able to have time to look back on the week by writing a reflection journal every week, and I think I learn as I teach.—Participant 1 |
| Check of direction | While checking whether I was teaching properly, I checked the direction for correct preceptor education. And when I found something was lacking, I made an effort to make up for it.—Participant 16 | |
| Awareness of limitation | Lack of training | I knew I had to provide short, positive, and constructive feedback with the essentials, but I regretted not doing it because I wasn’t trained.—Participant 14 |
| Difficulties providing positive feedback | I was taught to provide positive feedback to new nurses, but that didn’t work out well in an urgent clinical situation. It was really hard to praise.—Participant 20 | |
| Lack of critical thinking | I had to teach new nurses to think critically about why this happens, but it didn’t work out. I think we have to practice deliberately and consciously.—Participant 18 | |
| Exhaustion | Repeated feedback for new nurses | I was tired of seeing a new nurse who learned from me and who I gave feedback repeatedly to several times but who still couldn’t do it.—Participant 15 |
| Interference by senior nurses | Even if I try to teach systematically according to the standards, if a higher-year nurse gives a different way to a new nurse, I have to follow it.—Participant 12 | |
| Self-blame | It was not easy to teach as I was taught from the PAR team, so I didn’t teach well. So, it seems that new nurses can’t learn to work.—Participant 25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, H.W.; Ju, D.; Choi, M.L.; Kim, S. Development and Evaluation of a Preceptor Education Program Based on the One-Minute Preceptor Model: Participatory Action Research. Int. J. Environ. Res. Public Health 2021, 18, 11376. https://doi.org/10.3390/ijerph182111376
Jeong HW, Ju D, Choi ML, Kim S. Development and Evaluation of a Preceptor Education Program Based on the One-Minute Preceptor Model: Participatory Action Research. International Journal of Environmental Research and Public Health. 2021; 18(21):11376. https://doi.org/10.3390/ijerph182111376
Chicago/Turabian StyleJeong, Hye Won, Deok Ju, Myoung Lee Choi, and Suhyun Kim. 2021. "Development and Evaluation of a Preceptor Education Program Based on the One-Minute Preceptor Model: Participatory Action Research" International Journal of Environmental Research and Public Health 18, no. 21: 11376. https://doi.org/10.3390/ijerph182111376
APA StyleJeong, H. W., Ju, D., Choi, M. L., & Kim, S. (2021). Development and Evaluation of a Preceptor Education Program Based on the One-Minute Preceptor Model: Participatory Action Research. International Journal of Environmental Research and Public Health, 18(21), 11376. https://doi.org/10.3390/ijerph182111376






