Effects of 1 MHz Therapeutic Ultrasound on Limb Blood Flow and Microvascular Reactivity: A Randomized Pilot Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participant Characteristics and Inclusion Criteria
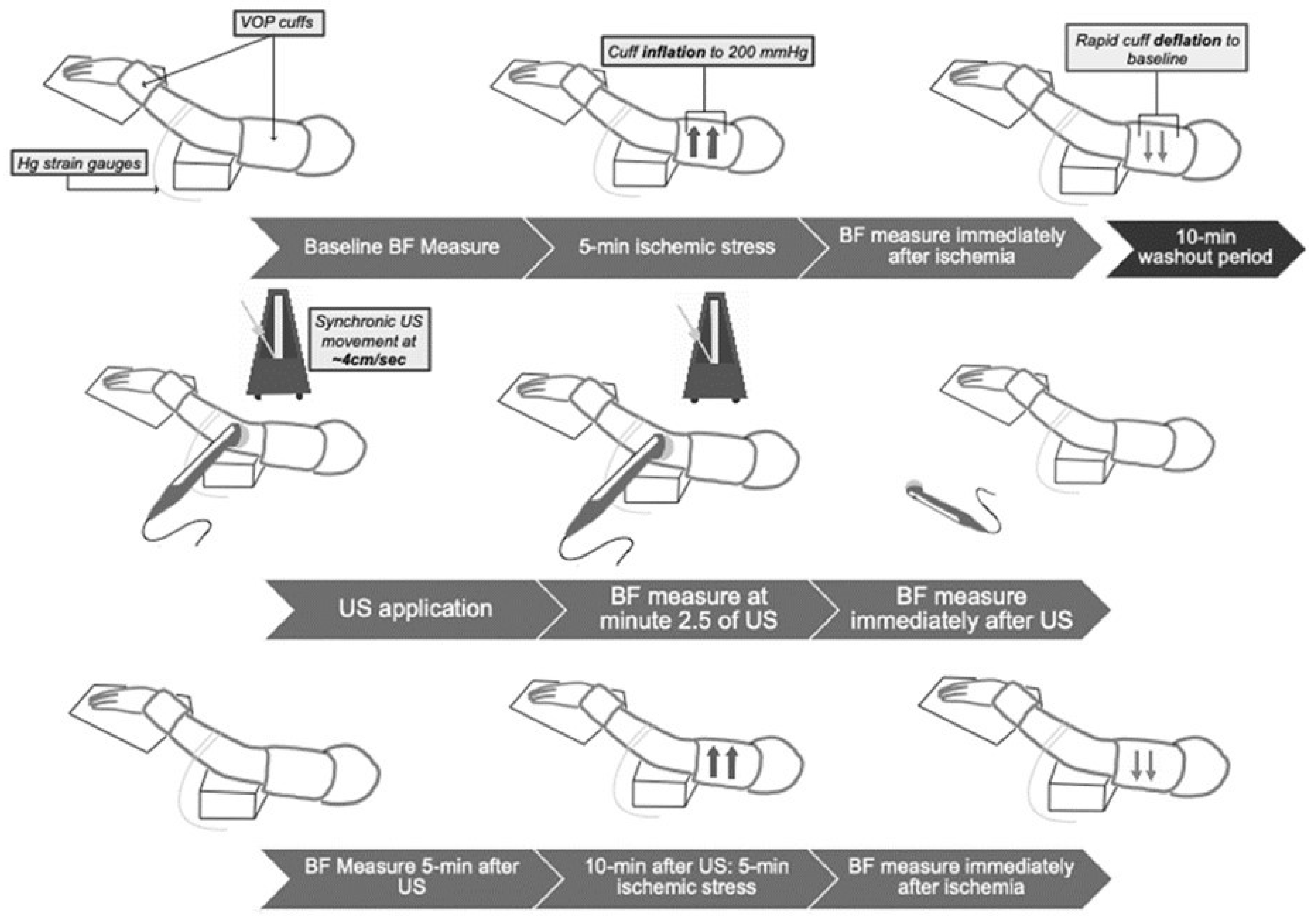
2.2. Experimental Design
2.3. Experimental Procedures
2.4. Statistical Analysis
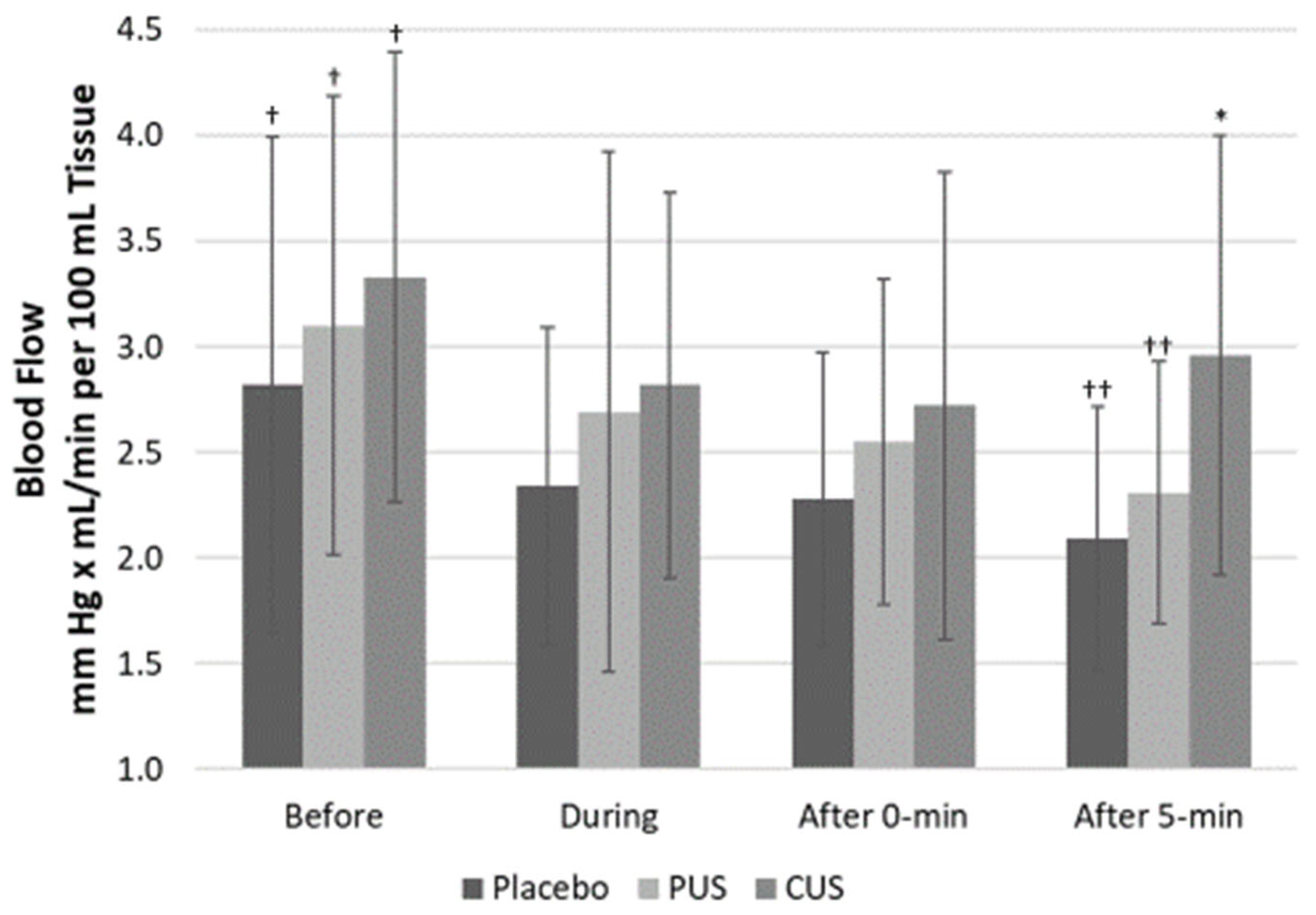
3. Results
4. Discussion
Limitations and Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huether, S.; McCance, K. Understanding Pathophysiology; Elsevier Mosby: St. Louis, MO, USA, 2012; pp. 134–137. [Google Scholar]
- Teller, P.; White, T.K. The Physiology of Wound Healing: Injury through Maturation. Surg. Clin. N. Am. 2009, 89, 599–610. [Google Scholar] [CrossRef]
- Cruz, J.M.; Hauck, M.; Pereira, A.P.C.; Moraes, M.B.; Martins, C.N.; da Silva Paulitsch, F.; Plentz, R.D.M.; Peres, W.; da Silva, A.M.V.; Signori, L.U. Effects of different therapeutic ultrasound waveforms on endothelial function in healthy vol-unteers: A randomized clinical trial. J. Ultras Med. Biol. 2016, 42, 471–480. [Google Scholar] [CrossRef]
- Vanhoutte, P.M.; Shimokawa, H.; Tang, E.H.C.; Feletou, M. Endothelial dysfunction and vascular disease. Acta Physiol. 2009, 196, 193–222. [Google Scholar] [CrossRef] [Green Version]
- Higashi, Y.; Noma, K.; Yoshizumi, M.; Kihara, Y. Endothelial Function and Oxidative Stress in Cardiovascular Diseases. Circ. J. 2009, 73, 411–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajendran, P.; Rengarajan, T.; Thangavel, J.; Nishigaki, Y.; Sakthisekaran, D.; Sethi, G.; Nishigaki, I. The Vascular Endothelium and Human Diseases. Int. J. Biol. Sci. 2013, 9, 1057–1069. [Google Scholar] [CrossRef] [Green Version]
- Poredos, P.; Jezovnik, M.K. Testing endothelial function and its clinical relevance. J. Atheroscler. Thromb. 2013, 20, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Cameron, M. Physical Agents in Rehabilitation: From Research to Practice, 4th ed.; Saunders Elsevier: St. Louis, MO, USA, 2012. [Google Scholar]
- Gurovich, A.N. Controlled Re-Injury of a Thigh Muscle Tear in a Soccer Player: A Case Study. J. Phys. Ther. Sci. 2012, 24, 295–299. [Google Scholar] [CrossRef] [Green Version]
- Harvey, E.N. Biological Aspects of Ultrasonic Waves, a General Survey. Biol. Bull. 1930, 59, 306–325. [Google Scholar] [CrossRef]
- Lehmann, J.F.; DeLateur, B.J.; Stonebridge, J.B.; Warren, C.G. Therapeutic temperature distribution produced by ultrasound as modified by dosage and volume of tissue exposed. Arch. Phys. Med. Rehabil. 1967, 48, 662–666. [Google Scholar]
- Lehmann, J.; DeLateur, B.; Warren, G.; Stonebridge, J. Bone and soft tissue heating produced by ultrasound. Arch. Phys. Med. Rehabil. 1967, 48, 397–401. [Google Scholar] [PubMed]
- Wong, R.; Schumann, B.; Townsend, R.; Phelps, C. A Survey of Therapeutic Ultrasound Use by Physical Therapists Who Are Orthopaedic Certified Specialists. Phys. Ther. 2007, 87, 986–994. [Google Scholar] [CrossRef] [Green Version]
- Pye, S.; Milford, C. The performance of ultrasound physiotherapy machines in Lothian region, Scotland, 1992. Ultrasound Med. Biol. 1994, 20, 347–359. [Google Scholar] [CrossRef]
- Young, S.; Dyson, M. Effect of therapeutic ultrasound on the healing of full-thickness excised skin lesions. Ultrasonics 1990, 28, 175–180. [Google Scholar] [CrossRef]
- Harpaz, D.; Chen, X.; Francis, C.W.; Marder, V.J.; Meltzer, R.S. Ultrasound enhancement of thrombolysis and reperfusion in vitro. J. Am. Coll. Cardiol. 1993, 21, 1507–1511. [Google Scholar] [CrossRef] [Green Version]
- Young, S.; Dyson, M. The effect of therapeutic ultrasound on angiogenesis. Ultrasound Med. Biol. 1990b, 16, 261–269. [Google Scholar] [CrossRef]
- Speed, C.A. Therapeutic ultrasound in soft tissue lesions. Rheumatology 2001, 40, 1331–1336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hauck, M.; Martins, C.N.; Moraes, M.B.; Aikawa, P.; da Silva Paulitsch, F.; Plentz, R.; Da Costa, S.T.; Da Silva, A.V.; Signori, L. Comparison of the effects of 1 MHz and 3 MHz therapeutic ultrasound on endothelium-dependent vasodilation of humans: A randomised clinical trial. Physiotherapy 2017, 105, 120–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regres-sion analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Adkisson, E.J.; Casey, D.; Beck, D.; Gurovich, A.N.; Martin, J.S.; Braith, R.W. Central, peripheral and resistance arterial reactivity: Fluctuates during the phases of the menstrual cycle. Exp. Biol. Med. 2010, 235, 111–118. [Google Scholar] [CrossRef] [Green Version]
- Mattu, A.; MacInnis, M.; Doyle-Baker, P.; Murias, J. Effects of the menstrual and oral contraceptive cycle phases on micro-vascular reperfusion. Exp. Phsyiol. 2020, 105, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Joyner, M.J.; Dietz, N.M.; Shepherd, J.T. From Belfast to Mayo and beyond: The use and future of plethysmography to study blood flow in human limbs. J. Appl. Physiol. 2001, 91, 2431–2441. [Google Scholar] [CrossRef]
- Larkin, K.A.; Martin, J.S.; Zeanah, E.H.; True, J.M.; Braith, R.W.; Borsa, P. Limb Blood Flow After Class 4 Laser Therapy. J. Athl. Train. 2012, 47, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Beck, D.; Martin, J.S.; Casey, D.; Braith, R.W. Exercise training improves endothelial function in resistance arteries of young prehypertensives. J. Hum. Hypertens. 2013, 28, 303–309. [Google Scholar] [CrossRef] [Green Version]
- McMackin, C.J.; Vita, J.A. Update on Nitric Oxide–Dependent Vasodilation in Human Subjects. Methods Enzym. 2005, 396, 541–553. [Google Scholar] [CrossRef] [Green Version]
- Abay, T.Y.; Kyriacou, P. Comparison of NIRS, laser Doppler flowmetry, photoplethysmography, and pulse oximetry during vascular occlusion challenges. Physiol. Meas. 2016, 37, 503–514. [Google Scholar] [CrossRef] [Green Version]
- Francis, C.W.; Onundarson, P.T.; Carstensen, E.L.; Blinc, A.; Meltzer, R.S.; Schwarz, K.; Marder, V.J. Enhancement of fibrinolysis in vitro by ultrasound. J. Clin. Investig. 1992, 90, 2063–2068. [Google Scholar] [CrossRef]
- Young, S.; Dyson, M. Macrophage responsiveness to therapeutic ultrasound. Ultrasound Med. Biol. 1990, 16, 809–816. [Google Scholar] [CrossRef]
- Chang, Y.-P.; Chiang, H.; Shih, K.-S.; Ma, H.-L.; Lin, L.-C.; Hsu, W.-L.; Huang, Y.-C.; Wang, H.-K. Effects of Therapeutic Physical Agents on Achilles Tendon Microcirculation. J. Orthop. Sports Phys. Ther. 2015, 45, 563–569. [Google Scholar] [CrossRef]
- Maegawa, Y.; Itoh, T.; Hosokawa, T.; Yaegashi, K.; Nishi, M. Effects of near-infrared low-level laser irradiation on microcir-culation. Lasers Surg. Med. 2000, 27, 427–437. [Google Scholar] [CrossRef]

| Demographics | Mean | Std. Deviation |
|---|---|---|
| Age (years) | 25.90 | 3.90 |
| Weight (kg) | 72.25 | 10.37 |
| Height (cm) | 163.87 | 8.27 |
| Body Mass Index (kg/m2) | 26.83 | 2.54 |
| Systolic BP (mm Hg) | 122.97 | 11.88 |
| Diastolic BP (mm Hg) | 76.5 | 9.24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Waters, M.; Miljkovic, B.; Rascon, J.; Gomez, M.; Gurovich, A.N. Effects of 1 MHz Therapeutic Ultrasound on Limb Blood Flow and Microvascular Reactivity: A Randomized Pilot Trial. Int. J. Environ. Res. Public Health 2021, 18, 11444. https://doi.org/10.3390/ijerph182111444
Waters M, Miljkovic B, Rascon J, Gomez M, Gurovich AN. Effects of 1 MHz Therapeutic Ultrasound on Limb Blood Flow and Microvascular Reactivity: A Randomized Pilot Trial. International Journal of Environmental Research and Public Health. 2021; 18(21):11444. https://doi.org/10.3390/ijerph182111444
Chicago/Turabian StyleWaters, Megan, Branko Miljkovic, Jozelyn Rascon, Manuel Gomez, and Alvaro N. Gurovich. 2021. "Effects of 1 MHz Therapeutic Ultrasound on Limb Blood Flow and Microvascular Reactivity: A Randomized Pilot Trial" International Journal of Environmental Research and Public Health 18, no. 21: 11444. https://doi.org/10.3390/ijerph182111444
APA StyleWaters, M., Miljkovic, B., Rascon, J., Gomez, M., & Gurovich, A. N. (2021). Effects of 1 MHz Therapeutic Ultrasound on Limb Blood Flow and Microvascular Reactivity: A Randomized Pilot Trial. International Journal of Environmental Research and Public Health, 18(21), 11444. https://doi.org/10.3390/ijerph182111444







