Evaluating Effectiveness of Outpatient Monitoring in Type 2 Diabetes: The One-Year Experience in an Italian Group of Primary Care
Abstract
1. Introduction
2. Materials and Methods
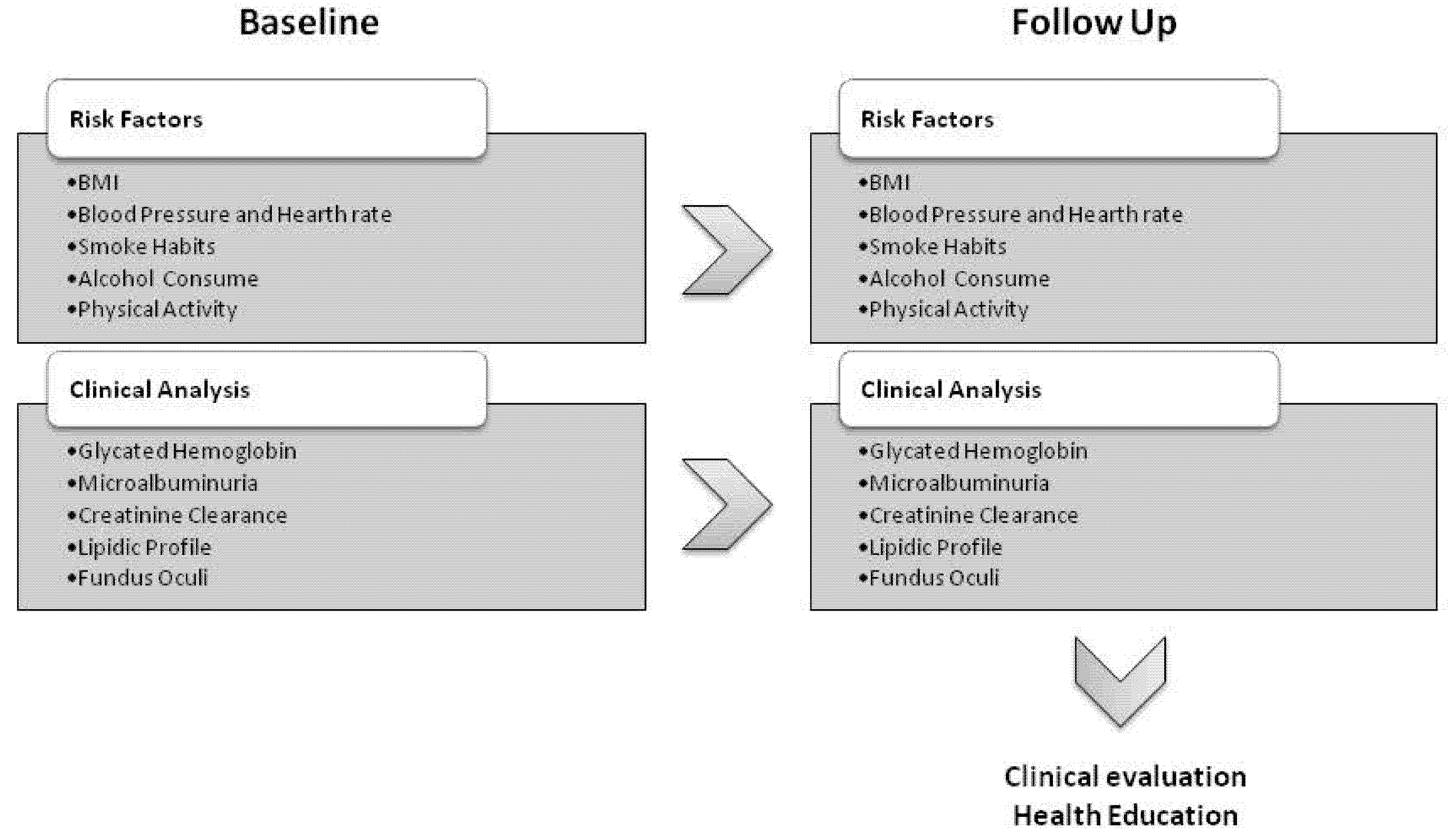
2.1. Study Design and Setting
2.2. Data Collection
2.3. Statistical Analysis
2.4. Sample Size
- The time, CAD and interaction effects were all hypothesized to be equal to 2.6. The effect of 2.6 corresponds to a Cohen d effect size of 0.8 [7] (d = (51 − 53.6)/3.3 = 2.6/3.3 = 0.8);
- Both marginal and interaction terms were considered in the data generation process;
- The baseline glycated hemoglobin value was supposed to be equal to 51 [8];
- The outcome variance was assumed to be equal to 3.3 [8].
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bodenheimer, T.; Wagner, E.H.; Grumbach, K. Improving Primary Care for Patients with Chronic Illness: The Chronic Care Model, Part 2. JAMA 2002, 288, 1909–1914. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. DF Diabetes Atlas, 7th ed.; International Diabetes Federation: Brussels, Belgium, 2015; ISBN 978-2-930229-81-2. [Google Scholar]
- SID Società Italiana di Diabetologia. Il Diabete in Italia. 2012, 1st ed.; Bononia University Press: Bologna, Italy, 2016; ISBN 978-88-6923-146-9. [Google Scholar]
- Marcellusi, A.; Viti, R.; Mecozzi, A.; Mennini, F.S. The Direct and Indirect Cost of Diabetes in Italy: A Prevalence Probabilistic Approach. Eur. J. Health Econ. HEPAC Health Econ. Prev. Care 2016, 17, 139–147. [Google Scholar] [CrossRef] [PubMed]
- SER Sistema Epidemiologico Regionale Relazione Socio Sanitaria Della Regione Del Veneto—Anno 2017 (Dati 2015–2016). Available online: https://www.ser-veneto.it/public/RSSR_Veneto_2016.pdf (accessed on 12 July 2021).
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B Methodol. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Nathan, D.M.; Kuenen, J.; Borg, R.; Zheng, H.; Schoenfeld, D.; Heine, R.J. For the A1c-Derived Average Glucose (ADAG) Study Group Translating the A1C Assay Into Estimated Average Glucose Values. Diabetes Care 2008, 31, 1473–1478. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 2 February 2021).
- Harrell, F.E., Jr. rms: Regression Modeling Strategies. 2020. Available online: https://cran.r-project.org/web/packages/rms/index.html (accessed on 2 February 2021).
- Goldfeld, K. Simulation of Study Data. R Package Version 0.1.15. 2019. Available online: https://CRAN.R-project.org/package=simstudy (accessed on 2 February 2021).
- Elm, E.v.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- European Countries on Their Journey towards National EHealth Infrastructures. Digit. Single Mark. 2011. Available online: https://ec.europa.eu/digital-single-market/en/news/european-countries-their-journey-towards-national-ehealth-infrastructures-0 (accessed on 24 September 2018).
- MacPhail, L.H.; Neuwirth, E.B.; Bellows, J. Coordination of Diabetes Care in Four Delivery Models Using an Electronic Health Record. Med. Care 2009, 47, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Houle, J.; Beaulieu, M.-D.; Chiasson, J.-L.; Lespérance, F.; Côté, J.; Strychar, I.; Bherer, L.; Meunier, S.; Lambert, J. Glycaemic Control and Self-Management Behaviours in Type 2 Diabetes: Results from a 1-Year Longitudinal Cohort Study. Diabet. Med. J. Br. Diabet. Assoc. 2015, 32, 1247–1254. [Google Scholar] [CrossRef] [PubMed]
- Parchman, M.L.; Pugh, J.A.; Noël, P.H.; Larme, A.C. Continuity of Care, Self-Management Behaviors, and Glucose Control in Patients with Type 2 Diabetes. Med. Care 2002, 40, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Windrum, P.; García-Goñi, M.; Coad, H. The Impact of Patient-Centered versus Didactic Education Programs in Chronic Patients by Severity: The Case of Type 2 Diabetes Mellitus. Value Health 2016, 19, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Tsasis, P.; Wu, J.; An, A.; Wong, H.J.; An, X.; Mei, Z.; Hains, T. Conceptualizing Type 2 Diabetes and Its Management. J. Multidiscip. Healthc. 2016, 9, 133–136. [Google Scholar] [CrossRef] [PubMed]
- Karimi Moonaghi, H.; Namdar Areshtanab, H.; Jouybari, L.; Arshadi Bostanabad, M.; McDonald, H. Facilitators and Barriers of Adaptation to Diabetes: Experiences of Iranian Patients. J. Diabetes Metab. Disord. 2014, 13, 17. [Google Scholar] [CrossRef] [PubMed]
- Ganiyu, A.B.; Mabuza, L.H.; Malete, N.H.; Govender, I.; Ogunbanjo, G.A. Non-Adherence to Diet and Exercise Recommendations amongst Patients with Type 2 Diabetes Mellitus Attending Extension II Clinic in Botswana. Afr. J. Prim. Health Care Fam. Med. 2013, 5, 6. [Google Scholar] [CrossRef]
- Parajuli, J.; Saleh, F.; Thapa, N.; Ali, L. Factors Associated with Nonadherence to Diet and Physical Activity among Nepalese Type 2 Diabetes Patients; a Cross Sectional Study. BMC Res. Notes 2014, 7, 758. [Google Scholar] [CrossRef] [PubMed]
- Bertolin, D.C.; Pace, A.E.; Cesarino, C.B.; Ribeiro, R.d.C.H.M.; Ribeiro, R.M.; Bertolin, D.C.; Pace, A.E.; Cesarino, C.B.; Ribeiro, R.d.C.H.M.; Ribeiro, R.M. Psychological Adaptation to and Acceptance of Type 2 Diabetesmellitus. Acta Paul. Enferm. 2015, 28, 440–446. [Google Scholar] [CrossRef]
- Laursen, D.H.; Christensen, K.B.; Christensen, U.; Frølich, A. Assessment of Short and Long-Term Outcomes of Diabetes Patient Education Using the Health Education Impact Questionnaire (HeiQ). BMC Res. Notes 2017, 10, 213. [Google Scholar] [CrossRef] [PubMed]
| N | PDTA (N = 91) | PDTA and CAD (N = 33) | All (N = 124) | p-Value | |
|---|---|---|---|---|---|
| Sex | 124 | 0.459 | |||
| Male | 54 (59%) | 22 (67%) | 76 (61%) | ||
| Female | 37 (41%) | 11 (33%) | 48 (39%) | ||
| Age (years) | 124 | 72.3 (66.5, 77.4) | 69.6 (63.3, 75.0) | 71.5 (66.1, 77.2) | 0.080 |
| Pharmacological treatment | 124 | 0.052 | |||
| Oral hypoglycemic | 82 (90%) | 29 (88%) | 111 (90%) | ||
| Insulin | 1 (1%) | 3 (9%) | 4 (3%) | ||
| None | 8 (9%) | 1 (3%) | 9 (7%) | ||
| Follow-up time (days) | 123 | 367 (314, 403) | 375 (348, 399) | 370 (315, 403) | 0.777 |
| N | PDTA (N = 91) | PDTA and CAD (N = 33) | All (N = 124) | p-Value | |
|---|---|---|---|---|---|
| Glycated Hemoglobin (mmol/mol) | 124 | 51.0 (45.5, 56.0) | 57.0 (49.0, 74.0) | 52.0 (46.0, 59.0) | 0.018 |
| Microalbuminuria (mg/die) | 111 | 10.4 (3.3, 22.7) | 6.5 (3.1, 15.0) | 8.3 (3.1, 21.9) | 0.192 |
| Creatinine Clearance (mL/min) | 120 | 86.7 (69.4, 103.3) | 84.1 (66.5, 99.6) | 85.7 (68.8, 102.8) | 0.539 |
| Total Cholesterol (mg/dL) | 120 | 180 (158, 209) | 176 (150, 222) | 178 (152, 212) | 0.840 |
| LDL Cholesterol (mg/dL) | 124 | 99.0 (77.0, 123.5) | 89.0 (71.0, 139.0) | 96.5 (76.0, 125.5) | 0.902 |
| HDL Cholesterol (mg/dL) | 120 | 56.0 (44.0, 65.0) | 49.0 (42.0, 54.0) | 53.5 (43.0, 63.0) | 0.039 |
| Triglycerides (mg/dL) | 118 | 102.0 (76.0,140.5) | 119.0 (95.5, 178.5) | 105.5 (78.2, 151.0) | 0.043 |
| Weight (kg) | 124 | 80.0 (68.5, 89.0) | 81.0 (75.0, 93.0) | 80.0 (70.0, 90.0) | 0.164 |
| BMI (kg/m2) | 124 | 28.5 (25.8, 30.8) | 29.3 (25.8, 32.4) | 28.7 (25.8, 31.2) | 0.374 |
| Waist Circumference (cm) | 111 | 105 (96, 111) | 107 (99, 114) | 106 (97, 112) | 0.524 |
| Smoke habits | 122 | 0.227 | |||
| Current smokers | 13 (15%) | 3 (9%) | 16 (13%) | ||
| Non-smokers | 50 (56%) | 15 (45%) | 65 (53%) | ||
| Former smokers | 26 (29%) | 15 (45%) | 41 (34%) | ||
| Cigarettes per day (n/day) | 57 | 20.0 (13.5, 27.5) | 20.0 (20.0, 30.0) | 20.0 (15.0, 30.0) | 0.263 |
| Alcohol consume (gr/day) | 124 | 0 (0, 12) | 0 (0, 12) | 0 (0, 12) | 0.159 |
| Physical activity | 124 | 0.579 | |||
| None | 29 (32%) | 15 (45%) | 44 (35%) | ||
| Light physical activity | 52 (57%) | 15 (45%) | 67 (54%) | ||
| Moderate physical activity | 7 (8%) | 2 (6%) | 9 (7%) | ||
| Intense physical activity | 3 (3%) | 1 (3%) | 4 (3%) | ||
| Systolic Blood Pressure (mmHg) | 124 | 150 (140, 160) | 145 (135, 160) | 148 (140, 160) | 0.726 |
| Diastolic Blood Pressure (mmHg) | 124 | 80.0 (70.0, 87.0) | 80.0 (75.0, 90.0) | 80.0 (71.5, 90.0) | 0.208 |
| Heart Rate (bpm) | 119 | 72.0 (66.0, 80.0) | 75.5 (66.0, 80.0) | 73.0 (66.0, 80.0) | 0.752 |
| N | PDTA (N = 91) | PDTA and CAD (N = 33) | All (N = 124) | p-Value | |
|---|---|---|---|---|---|
| Glycated Hemoglobin (mmol/mol) | 123 | 50 (44, 55) | 53 (49, 63) | 51 (44, 57) | 0.010 |
| Microalbuminuria (mg/die) | 107 | 10.6 (3.0, 32.5) | 4.8 (2.3, 9.6) | 7.9 (3.0, 27.2) | 0.046 |
| Creatinine Clearance (mL/min) | 119 | 86.0 (74.1, 104.3) | 78.4 (67.5, 99.2) | 83.9 (71.8, 103.6) | 0.182 |
| Total Cholesterol (mg/dL) | 121 | 173 (154, 199) | 162 (151, 192) | 172 (151, 199) | 0.588 |
| LDL Cholesterol (mg/dL) | 120 | 94.0 (74.5, 118.5) | 87.0 (72.0, 108.0) | 91.5 (73.8, 118.0) | 0.585 |
| HDL Cholesterol (mg/dL) | 120 | 54.0 (45.0, 67.0) | 51.0 (41.0, 57.0) | 52.5 (43.8, 64.5) | 0.087 |
| Triglycerides (mg/dL) | 118 | 100 (74, 143) | 120 (84, 163) | 106 (77, 146) | 0.212 |
| Weight (kg) | 124 | 79 (68, 87) | 84 (74, 93) | 80 (70, 90) | 0.104 |
| BMI (kg/m2) | 124 | 28.0 (25.6, 31.0) | 30.1 (25.5, 31.6) | 28.4 (25.6, 31.4) | 0.458 |
| Waist Circumference (cm) | 117 | 104 (96, 113) | 107 (100, 114) | 105 (96, 114) | 0.322 |
| Smoke habits | 123 | 0.334 | |||
| Current smokers | 11 (12) | 3 (9) | 14 (11) | ||
| Non-smokers | 51 (57) | 15 (45) | 66 (54) | ||
| Former smokers | 28 (31) | 15 (45) | 43 (35) | ||
| Cigarettes per day (n/day) | 57 | 20.0 (11.5, 27.5) | 20.0 (20.0, 30.0) | 20.0 (15.0, 30.0) | 0.164 |
| Alcohol consume (gr/day) | 124 | 0.0 (0.0, 14.4) | 0.0 (0.0, 14.4) | 0.0 (0.0, 14.4) | 0.434 |
| Physical activity | 124 | 0.594 | |||
| None | 40 (44) | 18 (55) | 58 (47) | ||
| Light physical activity | 42 (46) | 12 (36) | 54 (44) | ||
| Moderate physical activity | 8 (9) | 2 (6) | 10 (8) | ||
| Intense physical activity | 1 (1) | 1 (3) | 2 (2) | ||
| Systolic Blood Pressure (mmHg) | 124 | 145 (135, 158) | 140 (130, 160) | 145 (130, 160) | 0.320 |
| Diastolic Blood Pressure (mmHg) | 124 | 75 (70, 80) | 80 (70, 90) | 76 (70, 80) | 0.235 |
| Heart Rate (bpm) | 124 | 73.0 (66.0, 84.0) | 74.0 (68.0, 82.0) | 73.0 (66.0, 83.2) | 0.514 |
| Model 1 | Model 2 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Time Effect) | (CAD Effect) | (CAD × Time Effect) | ||||||||||
| Variable | EE | SE | p-Value | EE | SE | p-Value | EE | SE | p-Value | EE | SE | p-Value |
| Glycated haemoglobin | −0.005 | 0.003 | 0.392 | −0.005 | 0.003 | 0.392 | 8.230 | 2.063 | 0.001 | −0.002 | 0.006 | 0.963 |
| Microalbuminuria | 0.003 | 0.010 | 0.934 | 0.003 | 0.010 | 0.934 | −5.075 | 9.472 | 0.786 | −0.036 | 0.022 | 0.963 |
| Creatinine | 0.009 | 0.009 | 0.658 | 0.009 | 0.009 | 0.658 | −5.205 | 5.285 | 0.599 | 0.000 | 0.020 | 1 |
| Total cholesterol | −0.020 | 0.009 | 0.159 | −0.020 | 0.009 | 0.159 | 2.609 | 7.589 | 0.894 | −0.015 | 0.021 | 0.963 |
| Low density lipoprotein | −0.018 | 0.008 | 0.159 | −0.018 | 0.008 | 0.159 | 3.619 | 6.600 | 0.786 | −0.010 | 0.018 | 0.963 |
| High density lipoprotein | 0.003 | 0.002 | 0.623 | 0.003 | 0.002 | 0.623 | −5.875 | 3.065 | 0.367 | 0.001 | 0.006 | 0.963 |
| Triglycerides | 0.001 | 0.012 | 0.934 | 0.001 | 0.012 | 0.934 | 16.389 | 11.206 | 0.504 | −0.031 | 0.027 | 0.963 |
| Weight | 0.000 | 0.001 | 0.730 | 0.000 | 0.001 | 0.730 | 4.025 | 2.906 | 0.504 | 0.002 | 0.002 | 0.963 |
| Body mass index | 0.000 | 0.000 | 0.644 | 0.000 | 0.000 | 0.644 | 0.580 | 0.870 | 0.786 | 0.000 | 0.001 | 0.963 |
| Waist circumference | 0.000 | 0.001 | 0.735 | 0.000 | 0.001 | 0.735 | 2.496 | 2.325 | 0.599 | 0.000 | 0.002 | 0.966 |
| Number of cigarettes | −0.001 | 0.000 | 0.161 | −0.001 | 0.000 | 0.161 | 4.768 | 3.306 | 0.504 | 0.001 | 0.001 | 0.963 |
| Alcohol | −0.009 | 0.002 | <0.001 | 0.000 | 0.003 | <0.001 | 0.590 | 2.784 | 0.894 | 0.000 | 0.001 | 0.963 |
| Systolic blood pressure | −0.007 | 0.005 | 0.265 | −0.007 | 0.005 | 0.265 | −3.300 | 3.650 | 0.669 | −0.010 | 0.012 | 0.963 |
| Diastolic blood pressure | −0.011 | 0.003 | 0.001 | −0.011 | 0.003 | 0.001 | 2.350 | 1.831 | 0.518 | 0.006 | 0.006 | 0.963 |
| Heart rate | 0.003 | 0.002 | 0.730 | 0.003 | 0.002 | 0.730 | 1.153 | 2.026 | 0.786 | 0.001 | 0.006 | 0.963 |
| Phisical Activity (Moderate-Intense) | −0.001 | 0.001 | 0.309 | −0.001 | 0.001 | 0.309 | 0.182 | 2.247 | 0.935 | 0.001 | 0.007 | 0.963 |
| Smoker (Yes) | −0.002 | 0.003 | 0.481 | −0.002 | 0.003 | 0.481 | 0.483 | 3.502 | 0.890 | 0.002 | 0.011 | 0.963 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lazzarini, F.; Barbacane, L.; Scoleri, G.; Comoretto, R.I.; Cogno, G.; Disarò, B.; Gomirato, L.; Stocco, F.; Suppa, A.; Toninato, G.; et al. Evaluating Effectiveness of Outpatient Monitoring in Type 2 Diabetes: The One-Year Experience in an Italian Group of Primary Care. Int. J. Environ. Res. Public Health 2021, 18, 11540. https://doi.org/10.3390/ijerph182111540
Lazzarini F, Barbacane L, Scoleri G, Comoretto RI, Cogno G, Disarò B, Gomirato L, Stocco F, Suppa A, Toninato G, et al. Evaluating Effectiveness of Outpatient Monitoring in Type 2 Diabetes: The One-Year Experience in an Italian Group of Primary Care. International Journal of Environmental Research and Public Health. 2021; 18(21):11540. https://doi.org/10.3390/ijerph182111540
Chicago/Turabian StyleLazzarini, Francesca, Luca Barbacane, Giuseppe Scoleri, Rosanna I. Comoretto, Gianni Cogno, Benedetta Disarò, Luigi Gomirato, Francesca Stocco, Alessandro Suppa, Gianluca Toninato, and et al. 2021. "Evaluating Effectiveness of Outpatient Monitoring in Type 2 Diabetes: The One-Year Experience in an Italian Group of Primary Care" International Journal of Environmental Research and Public Health 18, no. 21: 11540. https://doi.org/10.3390/ijerph182111540
APA StyleLazzarini, F., Barbacane, L., Scoleri, G., Comoretto, R. I., Cogno, G., Disarò, B., Gomirato, L., Stocco, F., Suppa, A., Toninato, G., Minto, C., Azzolina, D., Iliceto, S., & Gregori, D. (2021). Evaluating Effectiveness of Outpatient Monitoring in Type 2 Diabetes: The One-Year Experience in an Italian Group of Primary Care. International Journal of Environmental Research and Public Health, 18(21), 11540. https://doi.org/10.3390/ijerph182111540







