Dietary Fiber Intake and Risk of Pancreatic Cancer: Systematic Review and Meta-Analysis of Observational Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion/Exclusion Criteria
2.2. Selection Process and Data Extraction
2.3. Strategy for Data Synthesis
2.4. Critical Appraisal
2.5. Statistical Analysis
2.6. Subgroup and Sensitivity Analysis
2.7. Cumulative Analysis
3. Results
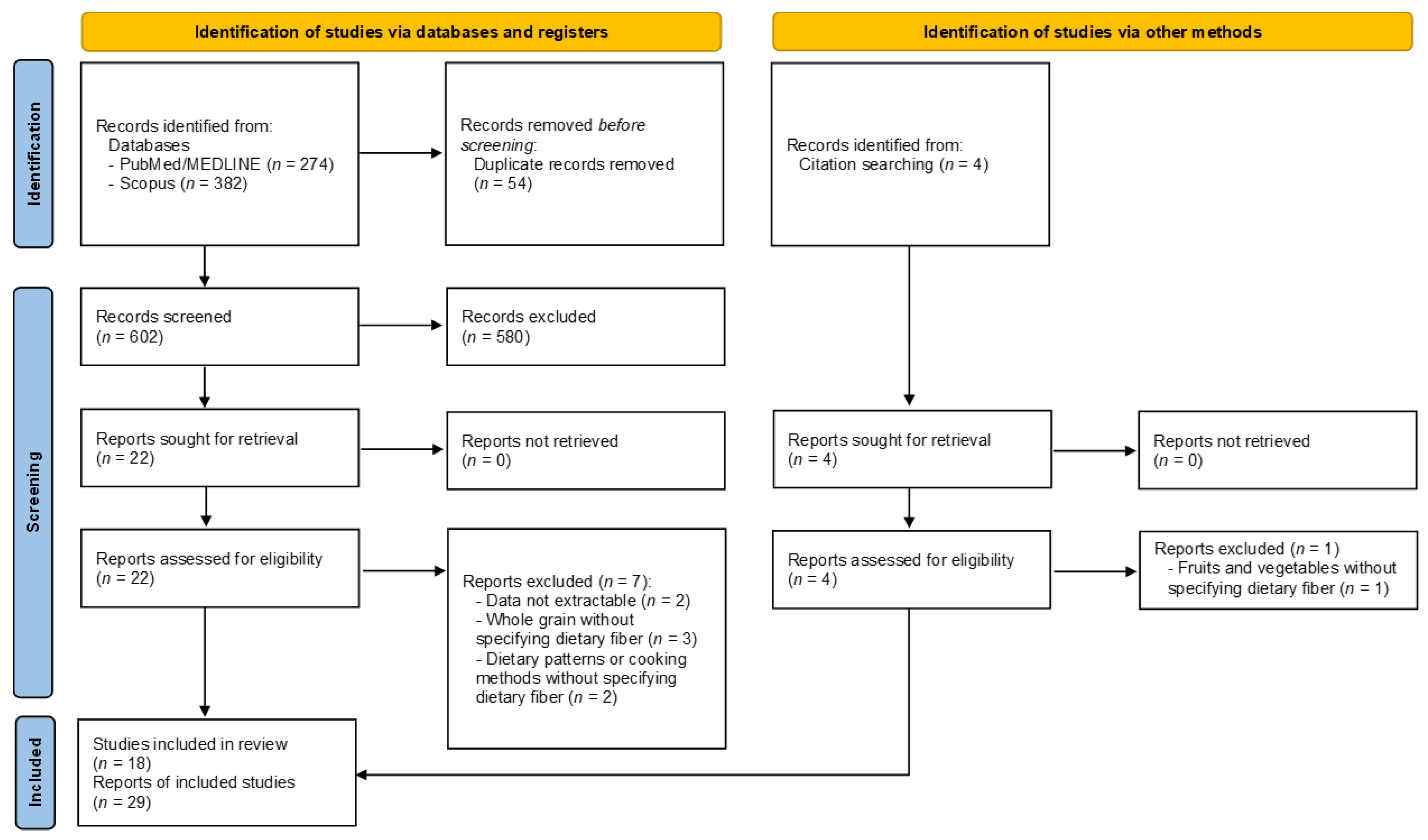
3.1. Literature Search
3.2. Characteristics of Included Studies
3.3. Quality Assessment of Included Studies
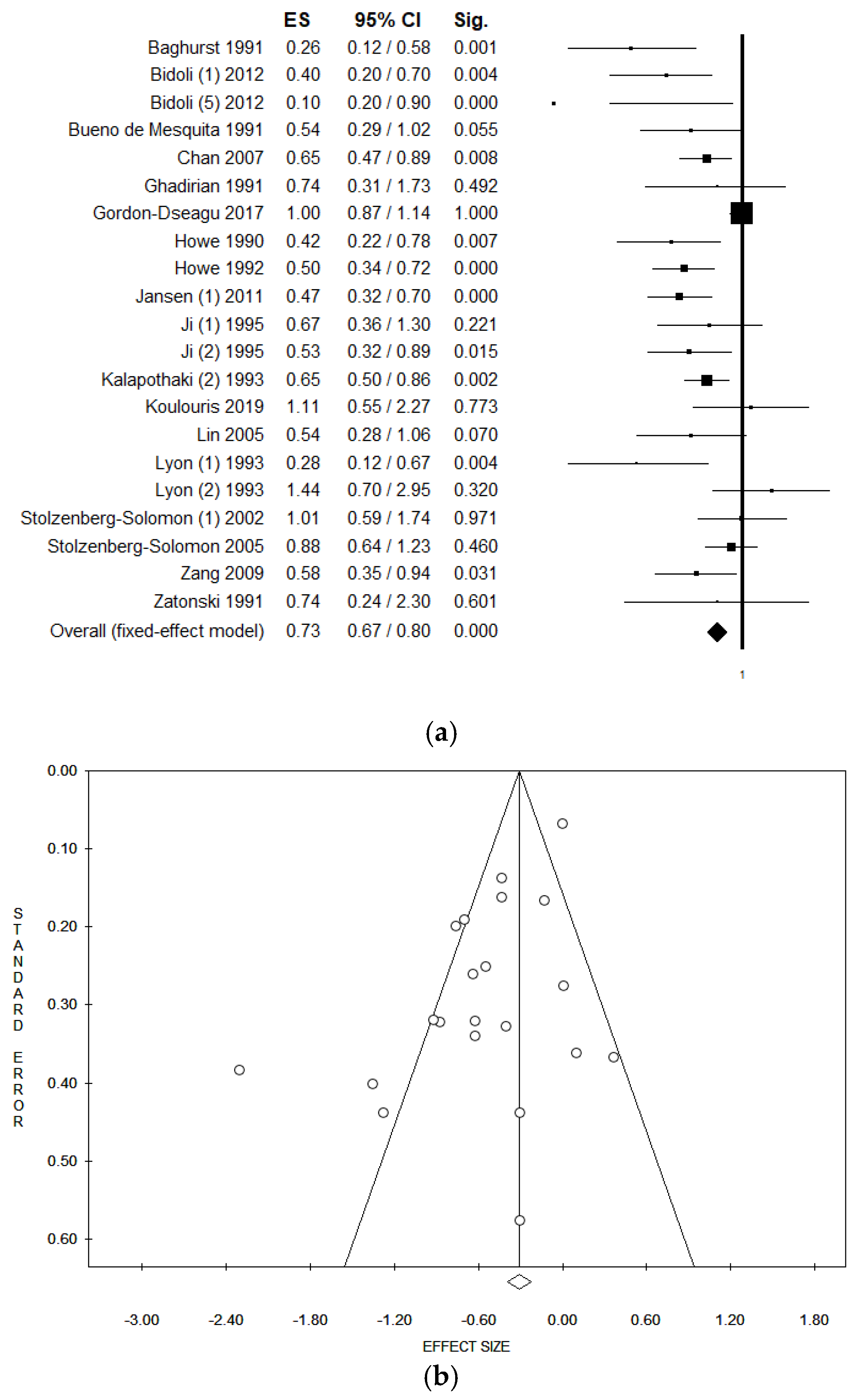
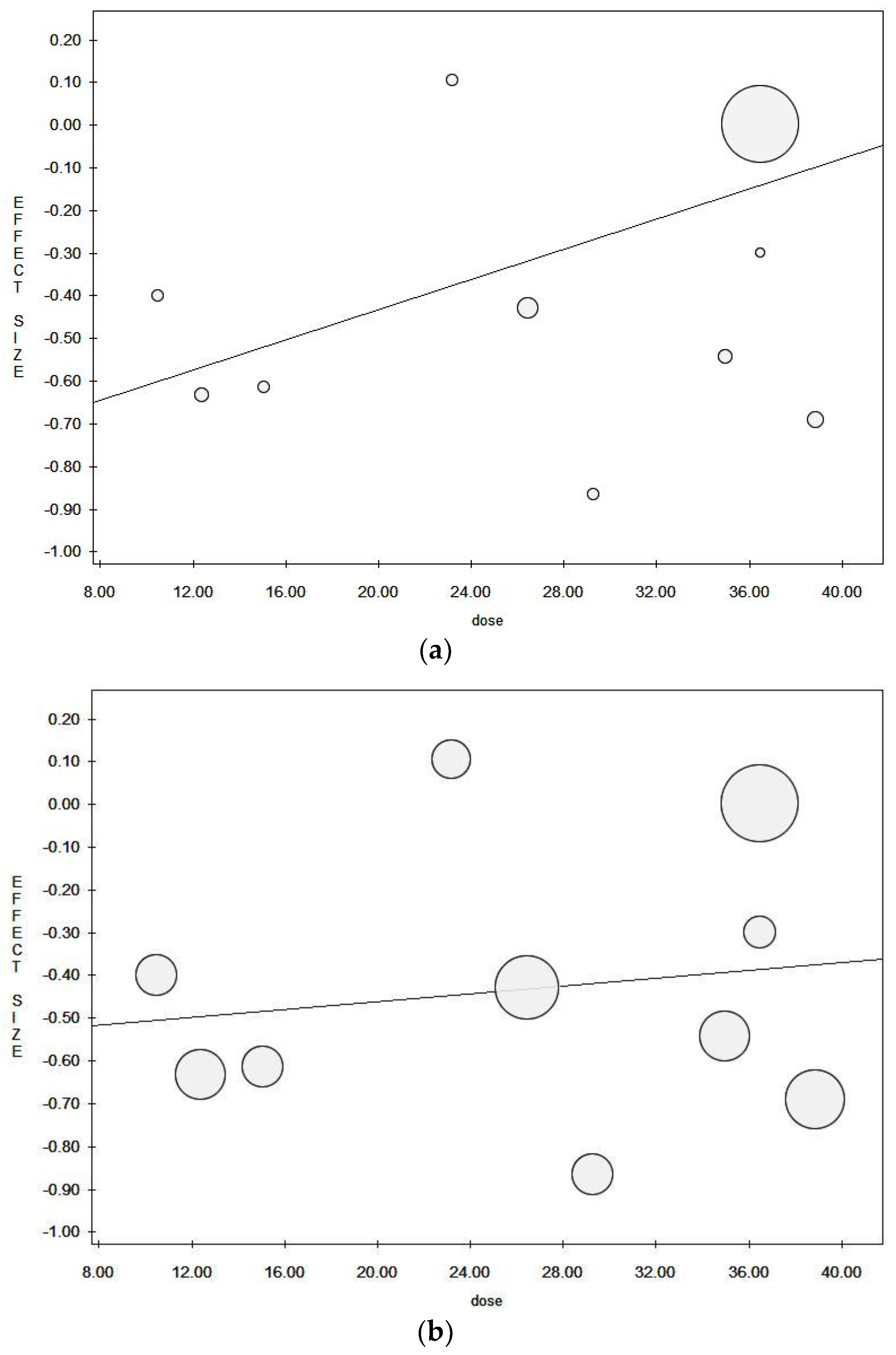
3.4. Results of the Meta-Analysis and Sensitivity Analyses
3.5. Subgroup Analysis
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McGuigan, A.; Kelly, P.; Turkington, R.C.; Jones, C.; Coleman, H.G.; McCain, R.S. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J. Gastroenterol. 2018, 24, 4846–4861. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2016. CA Cancer J. Clin. 2016, 66, 7–30. [Google Scholar] [CrossRef] [Green Version]
- GBD 2017 Pancreatic Cancer Collaborators. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2019, 4, 934–947. [Google Scholar] [CrossRef] [Green Version]
- Capasso, M.; Franceschi, M.; Rodriguez-Castro, K.I.; Crafa, P.; Cambie, G.; Miraglia, C.; Barchi, A.; Nouvenne, A.; Leandro, G.; Meschi, T.; et al. Epidemiology and risk factors of pancreatic cancer. Acta Biomed. 2018, 89, 141–146. [Google Scholar] [CrossRef]
- Zheng, J.; Guinter, M.A.; Merchant, A.T.; Wirth, M.D.; Zhang, J.; Stolzenberg-Solomon, R.Z.; Steck, S.E. Dietary patterns and risk of pancreatic cancer: A systematic review. Nutr. Rev. 2017, 75, 883–908. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund/American Institute for Cancer Research. Continuos Update Project Expert Report 2018. Diet, Nutrition, Physical Activity and Pancreatic Cancer; WCRF/AICR: London, UK, 2018. [Google Scholar]
- Bosetti, C.; Turati, F.; Dal Pont, A.; Ferraroni, M.; Polesel, J.; Negri, E.; Serraino, D.; Talamini, R.; La Vecchia, C.; Zeegers, M.P. The role of Mediterranean diet on the risk of pancreatic cancer. Br. J. Cancer 2013, 109, 1360–1366. [Google Scholar] [CrossRef] [Green Version]
- Katagiri, R.; Goto, A.; Sawada, N.; Yamaji, T.; Iwasaki, M.; Noda, M.; Iso, H.; Tsugane, S. Dietary fiber intake and total and cause-specific mortality: The Japan Public Health Center-based prospective study. Am. J. Clin. Nutr. 2020, 111, 1027–1035. [Google Scholar] [CrossRef]
- Barber, T.M.; Kabisch, S.; Pfeiffer, A.F.H.; Weickert, M.O. The health benefits of dietary fibre. Nutrients 2020, 12, 3209. [Google Scholar] [CrossRef] [PubMed]
- Nucci, D.; Fatigoni, C.; Salvatori, T.; Nardi, M.; Realdon, S.; Gianfredi, V. Association between dietary fibre intake and colorectal adenoma: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 4168. [Google Scholar] [CrossRef]
- Gianfredi, V.; Nucci, D.; Salvatori, T.; Dallagiacoma, G.; Fatigoni, C.; Moretti, M.; Realdon, S. Rectal cancer: 20% risk reduction thanks to dietary fibre intake. Systematic review and meta-analysis. Nutrients 2019, 11, 1579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gianfredi, V.; Salvatori, T.; Villarini, M.; Moretti, M.; Nucci, D.; Realdon, S. Is dietary fibre truly protective against colon cancer? A systematic review and meta-analysis. Int. Food Sci. Nutr. 2018, 69, 904–915. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, G.T.; Macfarlane, S. Bacteria, colonic fermentation, and gastrointestinal health. J. AOAC Int. 2012, 95, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Gianfredi, V.; Nucci, D.; Vannini, S.; Villarini, M.; Moretti, M. In vitro biological effects of sulforaphane (SFN), Epigallocatechin-3-gallate (EGCG), and Curcumin on Breast Cancer Cells: A systematic review of the literature. Nutr. Cancer 2017, 69, 969–978. [Google Scholar] [CrossRef]
- Gianfredi, V.; Albano, L.; Basnyat, B.; Ferrara, P. Does age have an impact on acute mountain sickness? A systematic review. J. Travel Med. 2020, 27, taz104. [Google Scholar] [CrossRef]
- Nucci, D.; Fatigoni, C.; Amerio, A.; Odone, A.; Gianfredi, V. Red and processed meat consumption and risk of depression: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 6686. [Google Scholar] [CrossRef]
- Gianfredi, V.; Blandi, L.; Cacitti, S.; Minelli, M.; Signorelli, C.; Amerio, A.; Odone, A. Depression and objectively measured physical activity: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 3738. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Paterson, J.; Welch, V.; Losos, M. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 1 October 2021).
- Ferrara, P.; Masuet-Aumatell, C.; Aguero, F.; Ramon-Torrell, J.M. The use of stand-by emergency treatment (SBET) for malaria in travellers: A systematic review and meta-analysis of observational studies. J. Infect. 2018, 77, 455–462. [Google Scholar] [CrossRef]
- Perego, G.; Vigezzi, G.P.; Cocciolo, G.; Chiappa, F.; Salvati, S.; Balzarini, F.; Odone, A.; Signorelli, C.; Gianfredi, V. Safety and efficacy of spray intranasal live attenuated influenza vaccine: Systematic review and meta-analysis. Vaccines 2021, 9, 998. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Duval, S.; Tweedie, R. A nonparametric “Trim and Fill” method of accounting for Publication Bias in Meta-Analysis. J. Am. Stat. Assoc. 2000, 95, 89–98. [Google Scholar] [CrossRef]
- Leimu, R.; Koricheva, J. Cumulative meta-analysis: A new tool for detection of temporal trends and publication bias in ecology. Proc. Biol. Sci. 2004, 271, 1961–1966. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silverman, D.T.; Swanson, C.A.; Gridley, G.; Wacholder, S.; Greenberg, R.S.; Brown, L.M.; Hayes, R.B.; Swanson, G.M.; Schoenberg, J.B.; Pottern, L.M.; et al. Dietary and nutritional factors and pancreatic cancer: A case-control study based on direct interviews. J. Natl. Cancer Inst. 1998, 90, 1710–1719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarosz, M.; Sekuła, W.; Rychlik, E. Influence of diet and tobacco smoking on pancreatic cancer incidence in poland in 1960–2008. Gastroenterol. Res. Pract. 2012, 2012, 682156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chatenoud, L.; Tavani, A.; La Vecchia, C.; Jacobs, D.R., Jr.; Negri, E.; Levi, F.; Franceschi, S. Whole grain food intake and cancer risk. Int. J. Cancer 1998, 77, 24–28. [Google Scholar] [CrossRef]
- La Vecchia, C.; Chatenoud, L.; Negri, E.; Franceschi, S. Session: Whole cereal grains, fibre and human cancer wholegrain cereals and cancer in Italy. Proc. Nutr. Soc. 2003, 62, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Schacht, S.R.; Olsen, A.; Dragsted, L.O.; Overvad, K.; Tjønneland, A.; Kyrø, C. Whole-grain intake and pancreatic cancer risk—The danish, diet, cancer and health cohort. J. Nutr. 2021, 151, 666–674. [Google Scholar] [CrossRef]
- Zheng, W.; McLaughlin, J.K.; Gridley, G.; Bjelke, E.; Schuman, L.M.; Silverman, D.T.; Wacholder, S.; Co-Chien, H.T.; Blot, W.J.; Fraumeni, J.F., Jr. A cohort study of smoking, alcohol consumption, and dietary factors for pancreatic cancer (United States). Cancer Causes Control 1993, 4, 477–482. [Google Scholar] [CrossRef]
- Fraser, G.E. Associations between diet and cancer, ischemic heart disease, and all-cause mortality in non-Hispanic white California Seventh-day Adventists. Am. J. Clin. Nutr. 1999, 70, 532s–538s. [Google Scholar] [CrossRef] [PubMed]
- Ghorbani, Z.; Hekmatdoost, A.; Zinab, H.E.; Farrokhzad, S.; Rahimi, R.; Malekzadeh, R.; Pourshams, A. Dietary food groups intake and cooking methods associations with pancreatic cancer: A case-control study. Indian J. Gastroenterol. Off. J. Indian Soc. Gastroenterol. 2015, 34, 225–232. [Google Scholar] [CrossRef]
- Baghurst, P.A.; McMichael, A.J.; Slavotinek, A.H.; Baghurst, K.I.; Boyle, P.; Walker, A.M. A case-control study of diet and cancer of the pancreas. Am. J. Epidemiol. 1991, 134, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Bidoli, E.; Pelucchi, C.; Zucchetto, A.; Negri, E.; Dal Maso, L.; Polesel, J.; Boz, G.; Montella, M.; Franceschi, S.; Serraino, D.; et al. Fiber intake and pancreatic cancer risk: A case-control study. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2012, 23, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Bueno de Mesquita, H.B.; Maisonneuve, P.; Runia, S.; Moerman, C.J. Intake of foods and nutrients and cancer of the exocrine pancreas: A population-based case-control study in The Netherlands. Int. J. Cancer 1991, 48, 540–549. [Google Scholar] [CrossRef]
- Chan, J.M.; Wang, F.; Holly, E.A. Whole grains and risk of pancreatic cancer in a large population-based case-control study in the San Francisco Bay Area, California. Am. J. Epidemiol. 2007, 166, 1174–1185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghadirian, P.; Thouez, J.P.; PetitClerc, C. International comparisons of nutrition and mortality from pancreatic cancer. Cancer Detect. Prev. 1991, 15, 357–362. [Google Scholar]
- Gordon-Dseagu, V.L.Z.; Thompson, F.E.; Subar, A.F.; Ruder, E.H.; Thiébaut, A.C.M.; Potischman, N.; Stolzenberg-Solomon, R. A cohort study of adolescent and midlife diet and pancreatic cancer risk in the nih-aarp diet and health study. Am. J. Epidemiol. 2017, 186, 305–317. [Google Scholar] [CrossRef] [Green Version]
- Howe, G.R.; Ghadirian, P.; de Mesquita, H.B.B.; Zatonski, W.A.; Baghurst, P.A.; Miller, A.B.; Simard, A.; Baillargeon, J.; de Waard, F.; Przewozniak, K.; et al. A collaborative case-control study of nutrient intake and pancreatic cancer within the search programme. Int. J. Cancer 1992, 51, 365–372. [Google Scholar] [CrossRef]
- Howe, G.R.; Jain, M.; Miller, A.B. Dietary factors and risk of pancreatic cancer: Results of a Canadian population-based case-control study. Int. J. Cancer 1990, 45, 604–608. [Google Scholar] [CrossRef]
- Jansen, R.J.; Robinson, D.P.; Stolzenberg-Solomon, R.Z.; Bamlet, W.R.; de Andrade, M.; Oberg, A.L.; Hammer, T.J.; Rabe, K.G.; Anderson, K.E.; Olson, J.E.; et al. Fruit and vegetable consumption is inversely associated with having pancreatic cancer. Cancer Causes Control 2011, 22, 1613–1625. [Google Scholar] [CrossRef]
- Ji, B.T.; Dai, Q.; Hatch, M.C.; Gao, Y.T.; Chow, W.H.; Gridley, G.; McLaughlin, J.K.; Wacholder, S.; Fraumeni, J.F., Jr. Dietary factors and the risk of pancreatic cancer: A case-control study in Shanghai, China. Cancer Epidemiol. Biomark. Prev. 1995, 4, 885–893. [Google Scholar]
- Kalapothaki, V.; Tzonou, A.; Hsieh, C.-c.; Karakatsani, A.; Trichopoulou, A.; Toupadaki, N.; Trichopoulos, D. Nutrient intake and cancer of the pancreas: A case-control study in Athens, Greece. Cancer Causes Control 1993, 4, 383–389. [Google Scholar] [CrossRef]
- Koulouris, A.I.; Luben, R.; Banim, P.; Hart, A.R. Dietary fiber and the risk of pancreatic cancer. Pancreas 2019, 48, 121–125. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.; Tamakoshi, A.; Hayakawa, T.; Naruse, S.; Kitagawa, M.; Ohno, Y. Nutritional factors and risk of pancreatic cancer: A population-based case-control study based on direct interview in Japan. J. Gastroenterol. 2005, 40, 297–301. [Google Scholar] [CrossRef]
- Lyon, J.L.; Slattery, M.L.; Mahoney, A.W.; Robison, L.M. Dietary intake as a risk factor for cancer of the exocrine pancreas. Cancer Epidemiol. Biomark. Prev. 1993, 2, 513–518. [Google Scholar]
- Stolzenberg-Solomon, R.Z.; Graubard, B.I.; Chari, S.; Limburg, P.; Taylor, P.R.; Virtamo, J.; Albanes, D. Insulin, glucose, insulin resistance, and pancreatic cancer in male smokers. JAMA 2005, 294, 2872–2878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stolzenberg-Solomon, R.Z.; Pietinen, P.; Taylor, P.R.; Virtamo, J.; Albanes, D. Prospective study of diet and pancreatic cancer in male smokers. Am. J. Epidemiol. 2002, 155, 783–792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zatonski, W.; Przewozniak, K.; Howe, G.R.; Maisonneuve, P.; Walker, A.M.; Boyle, P. Nutritional factors and pancreatic cancer: A case-control study from South-West Poland. Int. J. Cancer 1991, 48, 390–394. [Google Scholar] [CrossRef]
- Zhang, J.; Dhakal, I.B.; Gross, M.D.; Lang, N.P.; Kadlubar, F.F.; Harnack, L.J.; Anderson, K.E. Physical activity, diet, and pancreatic cancer: A population-based, case-control study in Minnesota. Nutr. Cancer 2009, 61, 457–465. [Google Scholar] [CrossRef] [Green Version]
- Izquierdo, J.N.; Schoenbach, V.J. The potential and limitations of data from population-based state cancer registries. Am. J. Public Health 2000, 90, 695–698. [Google Scholar] [CrossRef] [Green Version]
- EFSA Panel on Dietetic Products Nutrition and Allergies (NDA). Scientific opinion on dietary reference values for carbohydrates and dietary fibre. EFSA J. 2010, 8, 77. [Google Scholar] [CrossRef] [Green Version]
- Mao, Q.Q.; Lin, Y.W.; Chen, H.; Qin, J.; Zheng, X.Y.; Xu, X.; Xie, L.P. Dietary fiber intake is inversely associated with risk of pancreatic cancer: A meta-analysis. Asia Pac. J. Clin. Nutr. 2017, 26, 89–96. [Google Scholar] [CrossRef]
- McRae, M.P. The benefits of dietary fiber intake on reducing the risk of cancer: An umbrella review of meta-analyses. J. Chiropr. Med. 2018, 17, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Campos-Perez, W.; Martinez-Lopez, E. Effects of short chain fatty acids on metabolic and inflammatory processes in human health. Biochim. Biophys Acta Mol. Cell Biol. Lipids 2021, 1866, 158900. [Google Scholar] [CrossRef]
- Li, Q.; Jin, M.; Liu, Y.; Jin, L. Gut microbiota: Its potential roles in pancreatic cancer. Front. Cell Infect. Microbiol. 2020, 10, 572492. [Google Scholar] [CrossRef]
- Fujii, H.; Iwase, M.; Ohkuma, T.; Ogata-Kaizu, S.; Ide, H.; Kikuchi, Y.; Idewaki, Y.; Joudai, T.; Hirakawa, Y.; Uchida, K.; et al. Impact of dietary fiber intake on glycemic control, cardiovascular risk factors and chronic kidney disease in Japanese patients with type 2 diabetes mellitus: The Fukuoka Diabetes Registry. Nutr. J. 2013, 12, 159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gianfredi, V.; Nucci, D.; Balzarini, M.; Acito, M.; Moretti, M.; Villarini, A.; Villarini, M. E-Coaching: The DianaWeb study to prevent breast cancer recurrences. Clin. Ter. 2020, 170, e59–e65. [Google Scholar] [CrossRef]
- Villarini, M.; Acito, M.; Gianfredi, V.; Berrino, F.; Gargano, G.; Somaini, M.; Nucci, D.; Moretti, M.; Villarini, A. Validation of self-reported anthropometric measures and body mass index in a subcohort of the DianaWeb population study. Clin. Breast Cancer 2019, 19, e511–e518. [Google Scholar] [CrossRef]
- Villarini, M.; Lanari, C.; Nucci, D.; Gianfredi, V.; Marzulli, T.; Berrino, F.; Borgo, A.; Bruno, E.; Gargano, G.; Moretti, M.; et al. Community-based participatory research to improve life quality and clinical outcomes of patients with breast cancer (DianaWeb in Umbria pilot study). BMJ Open 2016, 6, e009707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, D.K.; Korc, M.; Petersen, G.M.; Eibl, G.; Li, D.; Rickels, M.R.; Chari, S.T.; Abbruzzese, J.L. Diabetes, pancreatogenic diabetes, and pancreatic cancer. Diabetes 2017, 66, 1103–1110. [Google Scholar] [CrossRef] [Green Version]
- Hadrevi, J.; Sogaard, K.; Christensen, J.R. Dietary fiber intake among normal-weight and overweight female health care workers: An exploratory nested case-control study within FINALE-Health. J. Nutr. Metab. 2017, 2017, 1096015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferravante, C.; Gianfredi, V.; Bietta, C. Nutrition in Umbria: Adherence to five-a-day. Recenti. Prog. Med. 2020, 111, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Gianfredi, V.; Grisci, C.; Nucci, D.; Parisi, V.; Moretti, M. Communication in health. Recenti. Prog. Med. 2018, 109, 374–383. [Google Scholar] [CrossRef]
- Gianfredi, V.; Monarca, S.; Moretti, M.; Villarini, M. Health education, what is the role for pharmacist? Results from a cross sectional study in Umbria, Italy. Recenti. Prog. Med. 2017, 108, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.H.; Qiao, C.; Wang, R.C.; Zhou, W.P. Dietary fiber intake and pancreatic cancer risk: A meta-analysis of epidemiologic studies. Sci. Rep. 2015, 5, 10834. [Google Scholar] [CrossRef] [Green Version]
| Author, Year [Ref.] | Country | Study Period | Study Design | Population Characteristics | Tool | Diagnostic Assessment | Cancer Type | Funds | Conflicts of Interest |
|---|---|---|---|---|---|---|---|---|---|
| Baghurst, 1991 [35] | Australia | 1984–1987 | Case-controls | Patients from major hospitals in Adelaide and from the cancer registry; controls selected from the electoral roll, matched by sex and age. | Personal dietary interview with no info on validation. Subjects’ proxies were also allowed to be interviewed. The food interview refered to 10 years previously (179 food items) | Cancer registry | Not specified | n.a. | n.a. |
| Bidoli, 2012 [36] | Italy | 1991–2008 | Hospital-based case-controls | Patients from two major hospitals in northen Italy; controls were selected from hospital patients and matched by sex, age, and study center | Personal interview by means of a validated 78-item FFQ referring to 2 years previously | Histology or cytology in 54.9% of cases, the others by ultrasound or tomography | Adenocarcinoma of the exocrine pancreas | yes | no |
| Bueno de Mesquita, 1991 [37] | The Netherlands | 1984–1987 | Case-controls | Live and dead patients residing in 70 municipalities; controls were selected from the general population and matched by sex and age | Personal dietary interview with no info on validation. Subjects’ proxies were also allowed to be interviewed. The food interview refered to 1 year previously | Clinical diagnosis retrieved from several medical records, including the cancer registry | Adenocarcinoma of the exocrine pancreas | n.a. | n.a. |
| Chan, 2007 [38] | USA | 1995–1999 | Case-controls | Live patients residing in six Bay Area counties able to complete an in-person interview; controls were selected from the general population and matched by sex and age | Validated 131-item semi-quantitative FFQ referring to 1 year previously | Cancer registry | Adenocarcinoma of the exocrine pancreas | yes | no |
| Ghadirian, 1991 [39] | Canada | 1984–1988 | Case-controls | Live patients from 19 hospitals in Montreal; controls were selected from the general population and matched for sex, age, and residency | Personal interview by means of NCIC 200-item validated FFQ | Histological, clinical, or radiological diagnosis | Not specified | yes | n.a. |
| Gordon-Dseagu, 2017 [40] | USA | 1995–2006 | Cohort | NIH-AARP Diet and Health study | Validated self-administered 37-item FFQ referring to 10 years previously | Cancer registry | Adenocarcinoma of the exocrine pancreas | n.a. | no |
| Howe, 1990 [42] | Canada | 1983–1986 | Case-controls | Live and dead patients diagnosed in 20 Toronto hospitals; controls were selected from the general population and matched by sex and age | Personal dietary interview with no info on validation. Subjects’ proxies were also allowed to be interviewed. The food interview refered to 1–2 years previously (200 food items) | Histology in 69% of cases, the rest were clinically or radiology confirmed | Not specified | n.a. | n.a. |
| Howe, 1992 [41] | Australia, Canada, the Netherlands, Poland | n.a. | Combination of data from 5 different case-control strudies | Live and dead patients; controls were selected from the general population and matched by sex and age | Personal dietary interview with no info on validation. Subjects’ proxies were also allowed to be interviewed. Different questionnaires among the studies | n.a. | Not specified | n.a. | n.a. |
| Jansen, 2011 [43] | USA | 2004–2009 | Case-controls | Live and dead patients; unrelated controls were selected from primary medical care | Validated self-administered 144-item FFQ referring to 5 years previously | Histology in 88%, medical records in 10%, and death certificate in 1% | Adenocarcinoma | yes | no |
| Ji, 1995 [44] | China | 1990–1993 | Case-controls | Live patients residing in Shangai; controls were selected from the general population and matched by sex and age | Personal dietary interview with no info on validation. The food interview refered to 5 years previously (86 food items) | Histology in 37%, surgery in 20%, and radiology in 43% | Not specified | n.a. | n.a. |
| Kalapothaki, 1993 [45] | Greece | 1991–1992 | Case-controls | Live patients diagnosed in 8 major teaching hospitals, with two control series. First control group hospitalized at the same hospital for other reasons; the second control group made up of residents who visited hospitalized patients and matched by sex and age | Personal dietary interview with no info on validation. The food interview refered to 1–2 years previously (110 food items) | Histological confirmation of cases | Not specified | yes | n.a. |
| Koulouris, 2019 [46] | UK | 1993–2010 | Cohort | EPIC-Norfolk | 6-days food diary | Health records and cancer registry data reviewed by gastroenterologist | Pancreatic ductal adenocarcinoma | yes | n.a. |
| Lin, 2005 [47] | Japan | 2000–2002 | Case-controls | Patients 40–79 years of age, who lived in Aichi or Gifu Prefectures; controls were selected from the general population matched by sex, age, and residency | Personal dietary interview, validated. The food interview refered to 1–5 years before (97 food items) | Clinical symptoms, laboratory findings, and imaging | Not specified | yes | n.a. |
| Lyon, 1993 [48] | USA | 1984–1987 | Case-controls | Patients alive or death; controls were selected from US Health Care Financing Administration aged below 65 years | Personal dietary interview, no info on validation (32-item FFQ). Subjects’ proxies were also allowed to be interviewed. | Cancer registry | Not specified | yes | n.a. |
| Stolzenberg-Solomon, 2002 [50] | Finland | 1985–1998 | Case-controls from a subcohort study | ATBC Study | Self-administered, validated, 200-item DHQ | Medical records | Malignant neoplasm of the exocrine pancreas | yes | n.a. |
| Stolzenberg-Solomon, 2005 [49] | Finland | 1985–2001 | Cohort | ATBC Study | Self-administered, validated, 200-item DHQ | Medical records | Malignant neoplasm of the exocrine pancreas | yes | no |
| Zatonski, 1991 [51] | Poland | 1985–1988 | Case-controls | Live or dead patients residing in southwest Poland; controls were selected from electoral rolls and matched by sex, age, and residency | Personal dietary interview, validated. The food interview refered to 1–2 years previously (80 food items) | Medical and pathology records supported by cancer registry data | Malignant neoplasm of the exocrine pancreas | yes | n.a. |
| Zhang, 2009 [52] | USA | 1994–1998 | Case-controls | Live patients form all hospitals in 7 county metropolitan areas of Minnesota. Controls were selected from the general population of the same age, and matched by sex and age | Personal interview by means of a validated 153-item Willet FFQ referring to 1 year previously | Pathological confirmation | Malignant neoplasm of the exocrine pancreas | yes | n.a. |
| Author, Year [Ref.] (Number of Stratified Analyses) | Total Sample ^ | Sex | Age (in Years) Mean ± SD | Dietary Fiber Intake Mean ± SD | No. Subjects at the Highest Fiber Intake | Highest Dietary Fiber Intake g/d | Effect Size (95% CI) p | Adjustment | QS/9 |
|---|---|---|---|---|---|---|---|---|---|
| Baghurst, 1991 [35] | Ca: 104 Co: 253 | Ca: F = 52 Co: F = 111 | ≥50 | n.a. | n.a. | n.a. | RR: 0.26 (0.12–0.58) p < 0.001 | TEn, alcohol, smoking | 6 |
| Bidoli, 2012 (1) [36] | Ca: 326 Co: 652 | Ca: F = 152 Co: F = 304 | Ca: 63 Co: 63 | 16.1 ± 5.7 | n.a. | n.a. | OR 0.4 (0.2–0.7) p < 0.001 | BMI, education, smoking, alcohol, DM, folate intake, TEn | 6 |
| Bidoli, 2012 (2) [36] | 8.1 ± 2.7 Soluble fiber | OR 0.4 (0.2–0.7) p < 0.001 | 6 | ||||||
| Bidoli, 2012 (3) [36] | 7.9 ± 3.2 Insoluble fiber | OR 0.5 (0.3–0.8) p < 0.003 | 6 | ||||||
| Bidoli, 2012 (4) [36] | Only F | Ca: F = 152 Co: F = 304 | n.a. | n.a. | OR 0.3 (0.1–0.8) p = n.a. | 6 | |||
| Bidoli, 2012 (5) [36] | Only M | Ca: M = 174 Co: M = 348 | OR 0.1 (0.2–0.9) p = n.a. | 6 | |||||
| Bueno de Mesquita, 1991 [37] | Ca:164 Co: 480 | Ca: F = 74 Co: F = 248 | Ca: 66.9 Co: 64.8 | n.a. | n.a. | n.a. | OR 0.54 (0.29–1.02) p = 0.75 | Age, sex, response status, smoking, TEn | 6 |
| Chan, 2007 [38] | Ca: 532 Co: 1701 | Ca: F = 241 Co: F = 818 | 21–85 (range for both groups) | n.a. | 81 | 26.5 | OR 0.65 (0.47–0.89) p = 0.02 | Age, sex, TEn, BMI, race, education, smoking, DM | 9 |
| Ghadirian, 1991 [39] | Ca:179 Co: 239 | Ca: F = 82 Co: F = 198 | 35–79 (range for both groups) | Ca: 24.0 ± 11.9 g/d Co: 26.4 ± 14.4 g/d | n.a. | 36.6 | RR: 0.74 (0.31–1.73) p = n.a. | Age, sex, smoking, response status, TEn | 6 |
| Gordon-Dseagu, 2017 [40] | 301,772 Ca: 1322 | Ca: F = 36.6% no Ca: F = 42% | Ca: 66.0 no Ca: 63.5 | n.a. | Ca: 438 | 9.2–54.6 | HR: 1.00 (0.87–1.14) p = 0.92 | Sex, TEn, smoking, BMI, DM | 8 |
| Howe, 1990 [42] | Ca:249 Co: 505 | n.a. | n.a. | n.a. | n.a. | >29.3 | RR: 0.42 (0.22–0.78) p < 0.001 | TEn, fiber intake, smoking | 6 |
| Howe, 1992 [41] | Ca: 808 Co: 1669 | n.a. | n.a. | n.a. | n.a. | 38.9 | RR: 0.50 (0.34–0.72) p < 0.001 | Nutrient variables, smoking | 4 |
| Jansen, 2011 (1) [43] | Ca: 384 Co: 983 | Ca: F = 163 Co: F = 500 | Ca: 67.0 Co: 65.8 | n.a. | Ca:.56 | n.a. | OR: 0.47 (0.32–0.70) p < 0.001 Total dietary fiber | Age, sex, TEn, BMI, smoking, alcohol | 7 |
| Jansen, 2011 (2) [43] | Ca:.60 | OR: 0.58 (0.39–0.86) p < 0.001 Soluble fiber | 7 | ||||||
| Jansen, 2011 (3) [43] | Ca:.57 | OR: 0.48 (0.33–0.71) p < 0.001 Insoluble fiber | 7 | ||||||
| Ji, 1995 (1) [44] | Ca: 325 Co: 1552 | n.a. | F: Ca: 65 Co: 61 | n.a. | n.a. | ≥10.5 | F: OR: 0.67 (0.36–1.30) p = 0.26 | Age, income, smoking, green tea, response status, TEn | 7 |
| Ji, 1995 (2) [44] | M: Ca: 63 Co: 62 | ≥12.4 | M: OR: 0.53 (0.32–0.89) p = 0.01 | 7 | |||||
| Kalapothaki, 1993 (1) [45] | Ca: 181 Co: 181 | n.a. | n.a. | n.a. | Ca: 38 Hospital Co: 43 | n.a. | OR: 0.80 (0.64–1.00) p < 0.005 | Age, sex, hospital, past residence, education, smoking, DM, TEn, nutrient variables | 6 |
| Kalapothaki, 1993 (2) [45] | Ca: 181 Co: 181 | Resident controls: 55 | OR: 0.65 (0.50–0.86) p < 0.001 | 6 | |||||
| Koulouris, 2019 [46] | Ca: 88 n Ca: 3970 | Ca: F = 48 n Ca: F = 2230 | Ca: 64.2 ± 7.8 n Ca: 59.3 ± 9.4 | Ca: 14.8 ± 5.1 g/d n Ca: 15.0 ± 5.4 g/d | Ca: 18 | 23.2 | HR: 1.11 (0.55–2.27) p = n.a. | Age, sex, smoking, DM, TEn | 9 |
| Lin, 2005 [47] | Ca: 109 Co: 218 | n.a. | Ca: 64.7 ± 8.3 Co: 65.1 ± 8.6 | n.a. | n.a. | >15.1 | OR: 0.54 (0.28–1.06) p = 0.07 | Age, smoking, nutrient variables | 8 |
| Lyon, 1993 (1) [48] | Ca: 60 Co: 166 | Only F | n.a. | n.a. | Ca: 10 | n.a. | OR 0.28 (0.12–0.67) p = 0.002 | Age, smoking, coffee, alcohol | 7 |
| Lyon, 1993 (2) [48] | Ca: 85 Co: 191 | Only M | Ca: 30 | OR 1.44 (0.70–2.95) p = 0.90 | 7 | ||||
| Stolzenberg-Solomon, 2002 (1) [50] | Ca: 163 n Ca: 26,948 | Only M | Ca: 58 n Ca: 57 | Ca: 24 n Ca: 24 total dietary fiber | n.a. | n.a. | HR: 1.01 (0.59–1.74) p = 0.70 | Age, smoking, TEn | 9 |
| Stolzenberg-Solomon, 2002 (2) [50] | Ca: 5.3 n Ca: 5.4 Soluble fiber | HR: 1.02 (0.56–1.70) p = 0.90 | Age, smoking, TEn, energy-adjusted folate intake | 9 | |||||
| Stolzenberg-Solomon, 2002 (3) [50] | Ca: 10.4 n Ca: 10.7 Insoluble fiber | HR: 0.95 (0.57–1.60) p = 0.99 | Age, smoking, TEn, energy-adjusted folate intake | 9 | |||||
| Stolzenberg-Solomon, 2005 [49] | Ca: 169 n Ca: 400 | Only M | Ca: 58 n Ca: 56 | Ca: 24.5 n Ca: 25.3 | n.a. | n.a. | OR *: 0.88 (0.64–1.23) p = 0.460 | None | 7 |
| Zatonski, 1991 [51] | Ca: 110 Co: 195 | Ca: F = 42 Co: F = 106 | Ca: 62.2 Co: 63.2 | n.a. | n.a. | n.a. | RR: 0.74 (0.24–2.30) p = 0.87 | Smoking, TEn | 7 |
| Zhang, 2009 [52] | Ca: 186 Co: 554 | Ca: F = 75 Co: F = 240 | Ca: 65.8 ± 10.9 Co: 66.5 ± 12.0 | Ca: 22.4 ± 11.3 Co: 24.0 ± 10.4 | Ca: 37 Co: 138 | 35.0 | OR 0.58 (0.35–0.94) p = 0.021 | Age, sex, race, education, smoking, alcohol | 7 |
| Analysis | Model | N. Studies Included | ES | 95% CI | p | Sample Size | I2 | p | Intercept | Tau (t) | p |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Excluding potential overlapping cohort | Fixed | 19 | 0.74 | 0.67–0.80 | <0.001 | 78.24 | <0.001 | −2.35 | −3.29 | 0.004 | |
| Random | 0.58 | 0.46–0.72 | <0.001 | ||||||||
| Excluding studies with estimated OR | Fixed | 19 | 0.72 | 0.66–0.79 | <0.001 | 78.63 | <0.001 | −2.40 | −3.47 | 0.003 | |
| Random | 0.55 | 0.43–0.69 | <0.001 | ||||||||
| Soluble fiber | Fixed | 3 | 0.62 | 0.47–0.83 | 0.001 | 29,456 | 60.60 | 0.079 | −0.11 | −0.22 | 0.990 |
| Random | 0.62 | 0.39–1.01 | 0.053 | ||||||||
| Insoluble fiber | Fixed | 3 | 0.58 | 0.45–0.75 | <0.001 | 29,456 | 58.34 | 0.091 | 6.72 | 1.01 | 0.498 |
| Random | 0.60 | 0.40–0.90 | 0.014 | ||||||||
| Validated dietary assessment | Fixed | 11 | 0.84 | 0.76–0.93 | 0.001 | 336,147 | 64.07 | 0.002 | −1.60 | −2.16 | 0.059 |
| Random | 0.72 | 0.57–0.89 | 0.003 | ||||||||
| Diagnosis by cancer registry | Fixed | 7 | 0.90 | 0.80–1.01 | 0.086 | 305,496 | 76.04 | <0.001 | −1.51 | −1.42 | 0.214 |
| Random | 0.70 | 0.48–1.04 | 0.079 | ||||||||
| Quality score ≥ 7 | Fixed | 13 | 0.84 | 0.76–0.92 | <0.001 | 65.09 | 0.001 | −1.50 | −2.07 | 0.063 | |
| Random | 0.72 | 0.58–0.89 | 0.003 | ||||||||
| Cohort studies (incidence) | Fixed | 3 | 0.99 | 0.87–1.11 | 0.819 | 302,668 | 0.00 | 0.749 | −0.13 | −0.17 | 0.894 |
| Random | 0.99 | 0.87–1.11 | 0.819 | ||||||||
| Case-Control (prevalence) | Fixed | 17 | 0.58 | 0.51–0.66 | <0.001 | 30.57 | 0.113 | −0.46 | −0.56 | 0.583 | |
| Random | 0.57 | 0.49–0.67 | <0.001 | ||||||||
| Women | Fixed | 3 | 0.45 | 0.28–0.71 | 0.001 | 38.04 | 0.199 | −4.71 | −2.04 | 0.290 | |
| Random | 0.42 | 0.23–0.77 | 0.005 | ||||||||
| Men | Fixed | 5 | 0.71 | 0.57–0.89 | 0.006 | 88.38 | <0.001 | −3.66 | −0.83 | 0.468 | |
| Random | 0.60 | 0.30–1.21 | 0.154 | ||||||||
| No Proxy respondent | Fixed | 14 | 0.80 | 0.73–0.88 | <0.001 | 61.59 | 0.001 | −1.65 | −2.48 | 0.029 | |
| Random | 0.69 | 0.58–0.83 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nucci, D.; Santangelo, O.E.; Provenzano, S.; Fatigoni, C.; Nardi, M.; Ferrara, P.; Gianfredi, V. Dietary Fiber Intake and Risk of Pancreatic Cancer: Systematic Review and Meta-Analysis of Observational Studies. Int. J. Environ. Res. Public Health 2021, 18, 11556. https://doi.org/10.3390/ijerph182111556
Nucci D, Santangelo OE, Provenzano S, Fatigoni C, Nardi M, Ferrara P, Gianfredi V. Dietary Fiber Intake and Risk of Pancreatic Cancer: Systematic Review and Meta-Analysis of Observational Studies. International Journal of Environmental Research and Public Health. 2021; 18(21):11556. https://doi.org/10.3390/ijerph182111556
Chicago/Turabian StyleNucci, Daniele, Omar Enzo Santangelo, Sandro Provenzano, Cristina Fatigoni, Mariateresa Nardi, Pietro Ferrara, and Vincenza Gianfredi. 2021. "Dietary Fiber Intake and Risk of Pancreatic Cancer: Systematic Review and Meta-Analysis of Observational Studies" International Journal of Environmental Research and Public Health 18, no. 21: 11556. https://doi.org/10.3390/ijerph182111556
APA StyleNucci, D., Santangelo, O. E., Provenzano, S., Fatigoni, C., Nardi, M., Ferrara, P., & Gianfredi, V. (2021). Dietary Fiber Intake and Risk of Pancreatic Cancer: Systematic Review and Meta-Analysis of Observational Studies. International Journal of Environmental Research and Public Health, 18(21), 11556. https://doi.org/10.3390/ijerph182111556








