An Integrated Management System for Noncommunicable Diseases Program Implementation in a Sub-Saharan Setting
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Participants
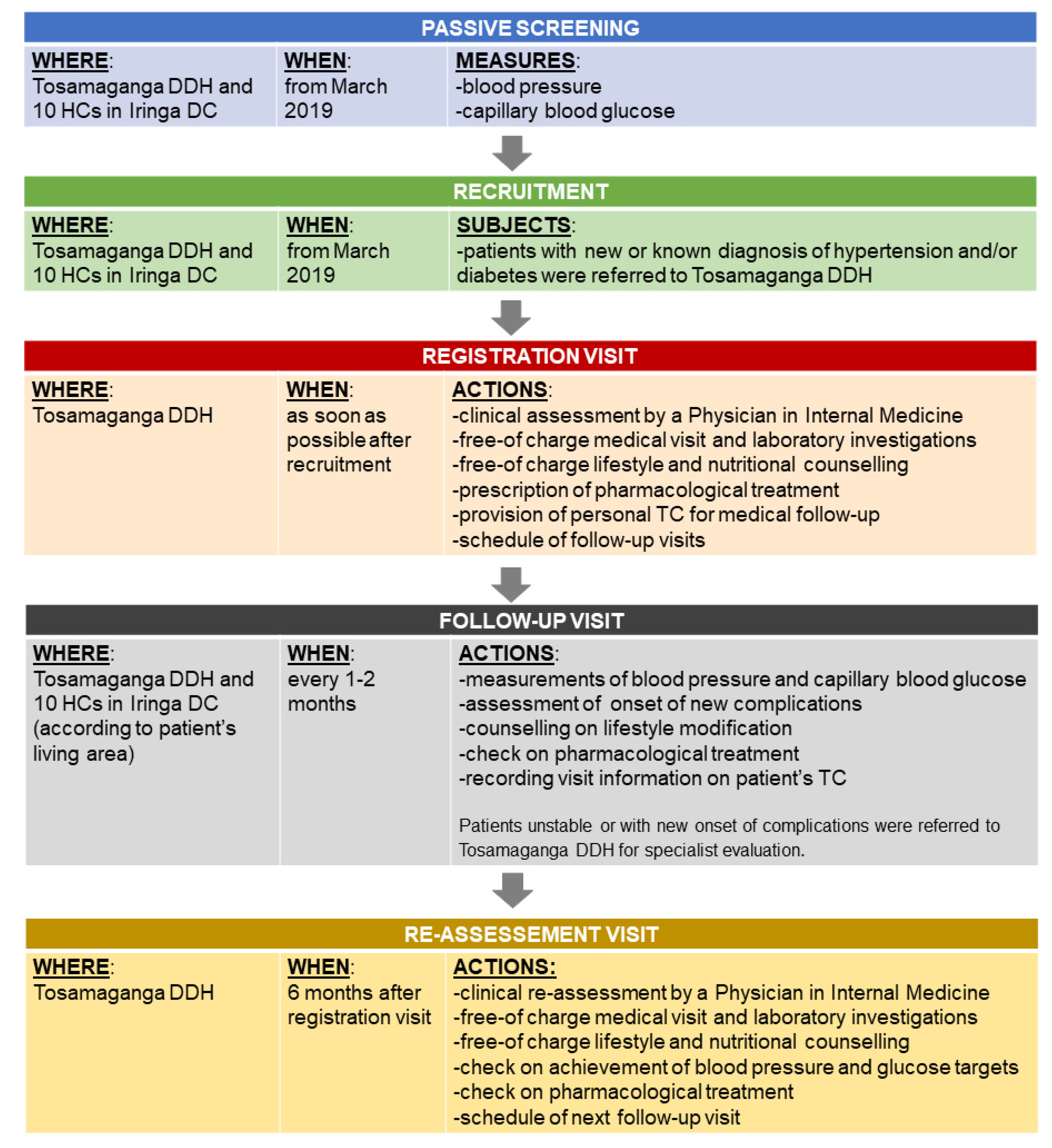
2.4. The Integrated Management System
2.5. Outcome Measures
2.6. Data Collection
2.7. Statistical Analysis
3. Results
3.1. Patients
3.2. Adherence to Follow-Up
3.3. Data Collection during Follow-Up Visits
4. Achievement of Treatment Target after Six Months of Follow-Up
Complications during Follow-Up
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Global Action Plan for the Prevention and Control of NCDs 2013-2020; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- WHO. Noncommunicable Diseases; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- The World Bank. Poverty; The World Bank: Washington, DC, USA, 2020. [Google Scholar]
- The 17 Sustainable Development Goals; The United Nations: New York, NY, USA, 2015; Available online: Sdgs.un.org/goals (accessed on 4 August 2021).
- Bukhman, G.; Mocumbi, A.O.; Horton, R. Reframing NCDs and injuries for the poorest billion: A Lancet Commission. Lancet 2015, 386, 1221–1222. [Google Scholar] [CrossRef]
- Bukhman, G.; Mocumbi, A.O.; Atun, R.; Becker, A.E.; Bhutta, Z.; Binagwaho, A. The Lancet NCDI Poverty Commission: Bridging a gap in universal health coverage for the poorest billion. Lancet 2020, 396, 991–1044. [Google Scholar] [CrossRef]
- The Tanzania NCDI Poverty Commission. Tanzania non-Communicable Diseases and Injuries Poverty Commission: Findings and Recommendations. August 2020. Available online: https://www.ncdipoverty.org/national-commission-reports (accessed on 4 August 2021).
- Institute for Health Metrics and Evaluation (IHME). Findings from the Global Burden of Disease Study 2017; IHME: Seattle, WA, USA, 2018. [Google Scholar]
- Tanzania Service Provision Assessment Survey 2014–2015; Ministry of Health and Social Welfare: Dar es Salaam, Tanzania, 2014.
- The DHS Program—Tanzania: Standard DHS. Available online: http://dhsprogram.com/what-we-do/survey2015-16 (accessed on 4 August 2021).
- Bintabara, D.; Mpondo, B.C.T. Preparedness of lower-level health facilities and the associated factors for the outpatient primary care of hypertension: Evidence from Tanzanian National survey. PLoS ONE 2018, 12, e0192942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peck, R.; Mghamba, J.; Vanobberghen, F.; Kavishe, B.; Rugarabamu, V.; Smeeth, L. Preparedness of Tanzania Health Facilities for outpatient primary care of hypertension and diabetes: A cross sectional survey. Lancet Glob. Health 2014, 2, 285–292. [Google Scholar] [CrossRef] [Green Version]
- WHO. Making Fair Choices on the Path to Universal Health Coverage; WHO: Geneva, Switzerland; Available online: http://www.who.int/choice/documents (accessed on 4 August 2021).
- Watkins, D.; Qi, J.; Horton, S. Costing Universal Health Coverage: The DCP3 Model | DCP3. Available online: http://dcp-3.org/resources/costs-and-affordability-essential-universalhealth-coverage-low-and-middle-income (accessed on 4 August 2021).
- Tanzania Health Sector Strategic Plan 2015-2020 (HSSP IV); Ministry of Health and Social Welfare: Dar es Salaam, Tanzania, 2015.
- Strategic and Action Plan for the Prevention and Control of Non Communicable Diseases in Tanzania 2016–2020; Ministry of Health, Community Development, Gender, Elderly and Children: Dar es Salaam, Tanzania, 2016.
- Tanzania STEPs Survey Report 2012; Ministry of Health and Social Welfare: Dar es Salaam, Tanzania, 2012.
- WHO. Noncommunicable Diseases (NCDs) Country Profile United Republic of Tanzania; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Edward, A.; Hoffmann, L.; Manase, F.; Matsushita, K.; Pariyo, G.W.; Brady, T.M. An exploratory study on the quality of patient screening and counseling for hypertension management in Tanzania. PLoS ONE 2020, 15, e0227439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet 2017, 389, 37–55. [Google Scholar] [CrossRef] [Green Version]
- Peck, R.N.; Green, E.; Mtabaji, J.; Majinge, C.; Smart, L.R.; Downs, J.A. Hypertension-related diseases as a common cause of hospital mortality in Tanzania: A 3-year prospective study. J. Hypertens. 2013, 31, 1806–1811. [Google Scholar] [CrossRef] [Green Version]
- Cleland, C.R.; Burton, M.J.; Hall, C.; Hall, A.; Courtright, P.; Makupa, W.U.; Philippin, H. Diabetic retinopathy in Tanzania: Prevalence and risk factors at entry into a regional screening programme. Trop. Med. Int. Health 2016, 21, 417–426. [Google Scholar] [CrossRef] [Green Version]
- Abbas, Z.G.; Lutale, J.K.; Bakker, K.; Baker, N.; Archibald, L.K. The “Step by Step” Diabetic Foot projectin Tanzania: A model for improving patient outcomes in less-developed countries. Int. Wound J. 2011, 8, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Doctors with Africa CUAMM. Available online: www.doctorswithafrica.org (accessed on 4 August 2021).
- Impementation of HIV/AIDS Care and Treatment Services in Tanzania; Ministry of Health, Community Development, Gender, Elderly and Children: Dar es Salaam, Tanzania, 2016.
- WHO. Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- WHO. HEARTS Technical Package for Cardiovascular Diseases Managment in Primary Health Care; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Global Health Workforce Alliance. Tanzania annex 5. Available online: https://www.who.int/workforcealliance/knowledge/resources/MLHWCountryCaseStudies_annex5_Tanzania.pdf (accessed on 4 August 2021).
- Standard Treatment Guidelines and National Essential Medicines List Tanzania Mainland; Ministry of Health, Community Development, Gender, Elderly and Children: Dar es Salaam, Tanzania, 2017.
- Cardiovascular Disease, Type 2 diabetes, Cancer and COPD in Adults, Case Management Desk Guide; Ministry of Health, Community Development, Gender, Elderly and Children: Dar es Salaam, Tanzania, 2013.
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 4 August 2021).
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- The World Bank Data. Life Expectancy at Birth, Total (Years), Tanzania. Available online: https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=TZ (accessed on 4 August 2021).
- Odunga, M. Tanzania: NHIF to Roll Out New Insurance Packages. 2019. Available online: Allafrica.com (accessed on 4 August 2021).
- WHO. Health Systems Financing: The Path to Universal Coverage; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Mtei, G.; Makawia, S.; Ally, M.; Kuwawenaruwa, A.; Meheus, F.; Borghi, J. Who pays and who benefits from health care? An assessment of equity in health care financing and benefit distribution in Tanzania. Health Policy Plan. 2012, 27 (Suppl. S1), i23–i34. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Variable | All Patients | Hypertensive Patients | Diabetic Patients | Hypertensive and Diabetic Patients |
|---|---|---|---|---|
| No. of subjects | 542 | 403 | 67 | 72 |
| Age, years a,b | 61 (53–69) | 62 (55–70) | 52 (44–60) | 61 (54–65) |
| Males:females | 134:408 | 92:311 | 21:46 | 21:51 |
| Personal insurance holders b | 190 (35.1) | 129 (32.1) | 27 (40.3) | 34 (47.2) |
| Referred from district health centers b | 312 (57.7) | 249 (61.9) | 37 (55.2) | 26 (36.1) |
| Job: | ||||
| Peasant | 312 (57.6) | 253 (62.8) | 29 (43.3) | 30 (41.7) |
| Employed | 70 (12.9) | 39 (9.7) | 15 (22.4) | 16 (22.2) |
| Unemployed c | 16 (3.0) | 7 (1.7) | 6 (9.0) | 3 (4.2) |
| Retired | 100 (18.4) | 77 (19.1) | 9 (13.4) | 14 (19.4) |
| Other/no response | 44 (8.1) | 27 (6.7) | 8 (11.9) | 9 (12.5) |
| Family history of hypertension b | 159 (29.4) | 125 (31.0) | 15 (22.7) | 19 (26.4) |
| Family history of diabetes | 67 (12.4) | 30 (7.4) | 17 (25.4) | 20 (27.8) |
| Regular daily alcohol consumption | 177 (32.7) | 144 (35.7) | 15 (22.4) | 18 (25.0) |
| Regular daily smoking habits | 26 (4.8) | 22 (5.4) | 2 (3.0) | 2 (2.8) |
| Sedentary lifestyle (>5 h spent seated daily) | 140 (25.8) | 100 (24.8) | 20 (29.9) | 20 (27.8) |
| Prior heart attack | 7 (1.3) | 7 (1.7) | 0 (0.0) | 0 (0.0) |
| Chronic heart failure | 59 (10.9) | 53 (13.1) | 0 (0.0) | 6 (8.3) |
| Prior stroke | 38 (7.0) | 28 (6.9) | 2 (3.0) | 8 (11.1) |
| Vision impairment | 25 (4.6) | 12 (3.0) | 7 (10.4) | 6 (8.3) |
| Diabetic foot | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miselli, M.A.; Cavallin, F.; Marwa, S.; Ndunguru, B.; Itambu, R.J.; Mutalemwa, K.; Rizzi, M.; Ciccarelli, G.; Conte, S.; Taddei, S.; et al. An Integrated Management System for Noncommunicable Diseases Program Implementation in a Sub-Saharan Setting. Int. J. Environ. Res. Public Health 2021, 18, 11619. https://doi.org/10.3390/ijerph182111619
Miselli MA, Cavallin F, Marwa S, Ndunguru B, Itambu RJ, Mutalemwa K, Rizzi M, Ciccarelli G, Conte S, Taddei S, et al. An Integrated Management System for Noncommunicable Diseases Program Implementation in a Sub-Saharan Setting. International Journal of Environmental Research and Public Health. 2021; 18(21):11619. https://doi.org/10.3390/ijerph182111619
Chicago/Turabian StyleMiselli, Maria Agata, Francesco Cavallin, Samwel Marwa, Bruno Ndunguru, Rehema John Itambu, Katunzi Mutalemwa, Monica Rizzi, Giulia Ciccarelli, Simone Conte, Stefano Taddei, and et al. 2021. "An Integrated Management System for Noncommunicable Diseases Program Implementation in a Sub-Saharan Setting" International Journal of Environmental Research and Public Health 18, no. 21: 11619. https://doi.org/10.3390/ijerph182111619







