Distance from Healthcare Facilities Is Associated with Increased Morbidity of Acute Infection in Pediatric Patients in Matiari, Pakistan
Abstract
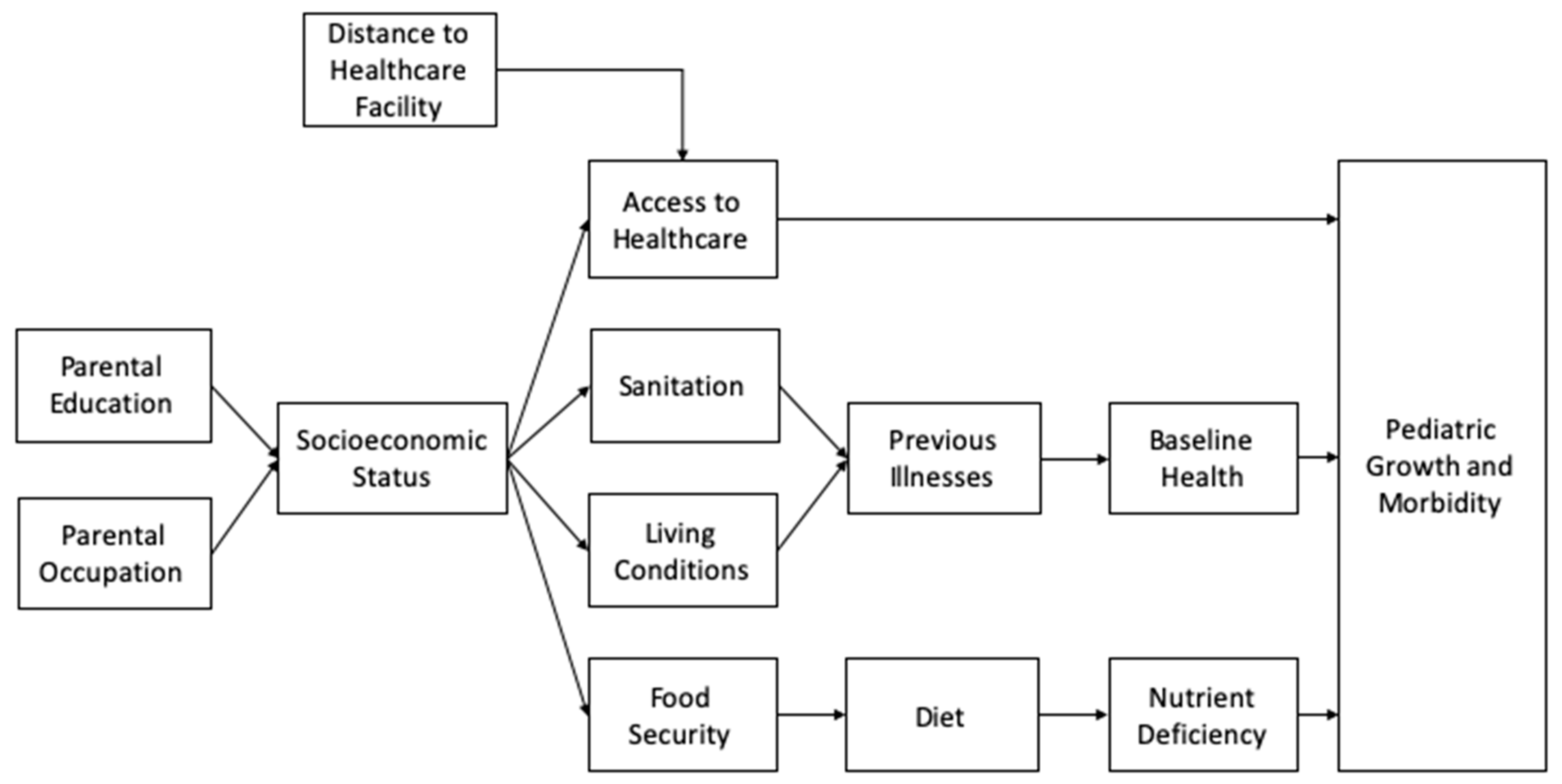
:1. Introduction
2. Materials and Methods
2.1. Study Participant Enrollment
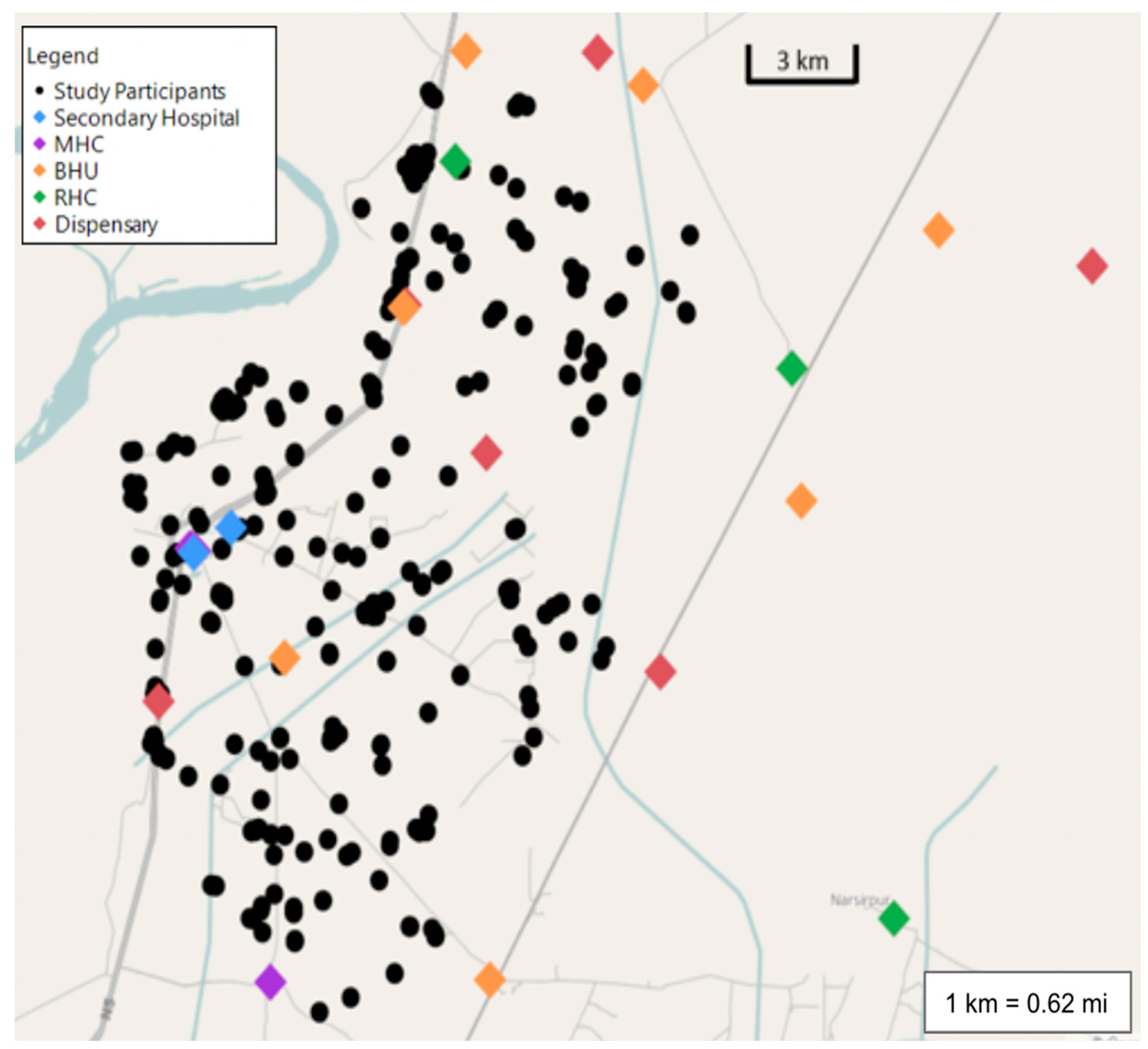
2.2. Geographical Data Collection of Healthcare Facilities and Participant Residence
2.3. Defining Clinical Outcomes: ARI Events, Diarrhea Events, and Growth Parameters
2.4. Calculation of Anthropometric Data and Correlation Analysis
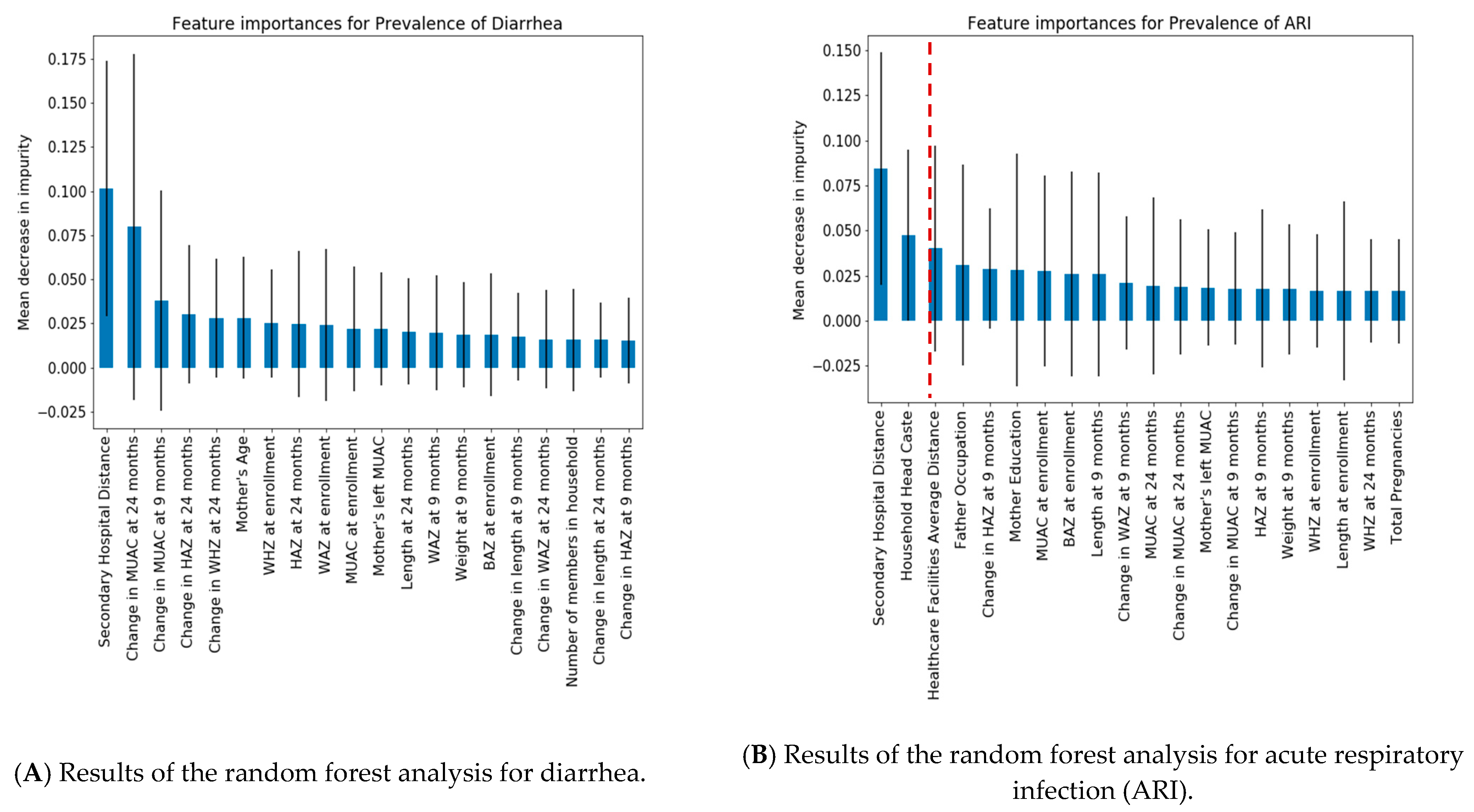
2.5. Random Forest Regression Modeling of Other Continuous Variables
3. Results
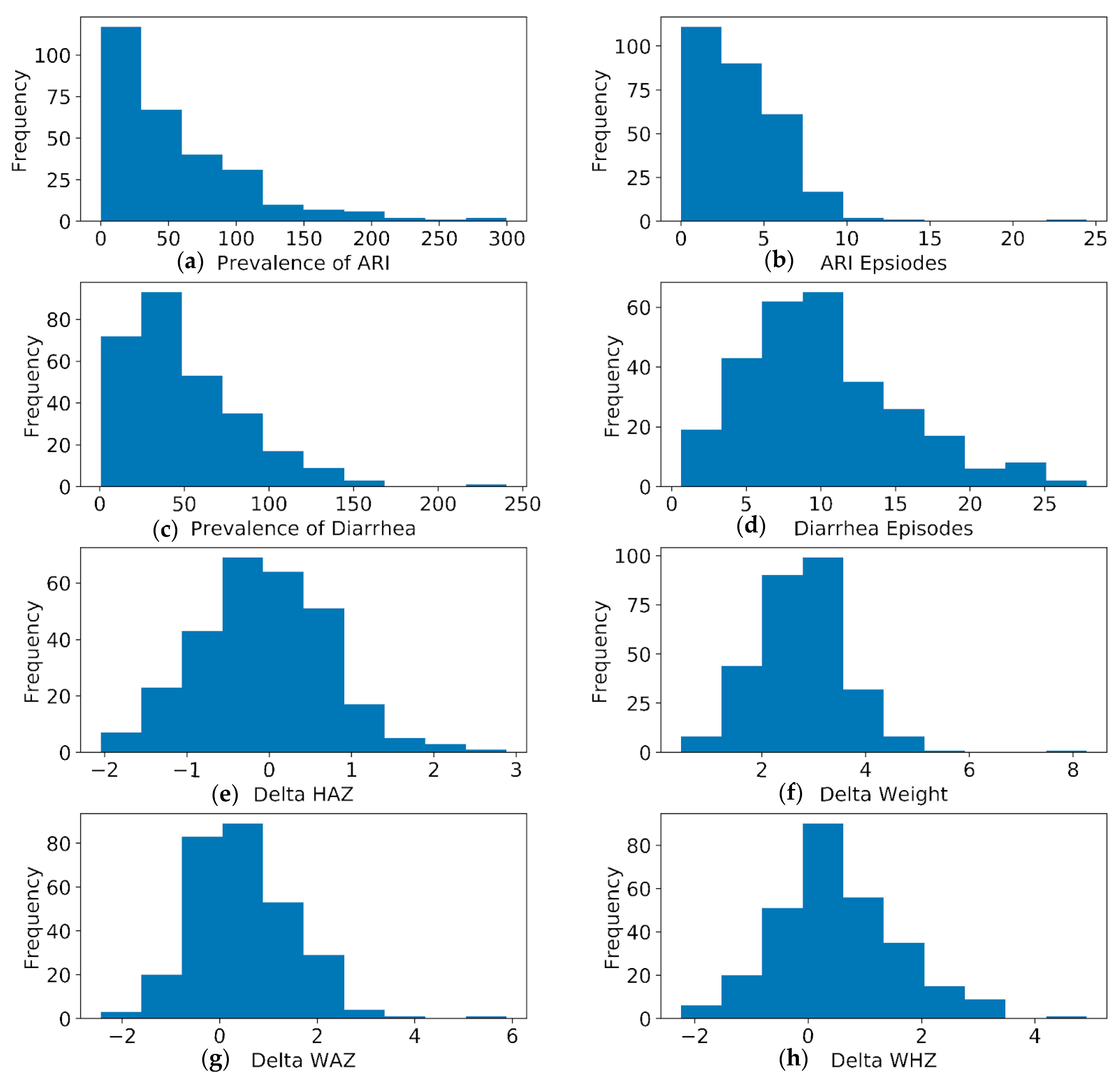
3.1. Descriptive Summary of Data Collection
3.2. Prevalence of ARI and Diarrhea Correlates with Study Participant Distance from Healthcare Facilities
3.3. Distance Has the Highest Variable Importance in ARI and Diarrhea Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hassan, A.; Mahmood, K.; Bukhsh, H.A. Healthcare System Of Pakistan. Int. J. Adv. Res. Publ. 2017, 1, 170–173. [Google Scholar]
- USAID. Pakistan Emergency Situational Analysis: District Matiari; USAID: Washington, DC, USA, 2014. [Google Scholar]
- Karra, M.; Fink, G.; Canning, D. Facility distance and child mortality: A multi-country study of health facility access, service utilization, and child health outcomes. Int. J. Epidemiol. 2017, 46, 817–826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McLaren, Z.M.; Ardington, C.; Leibbrandt, M. Distance decay and persistent health care disparities in South Africa. BMC Health Serv. Res. 2014, 14, 541. [Google Scholar] [CrossRef] [PubMed]
- Larson, P.S.; Mathanga, D.P.; Campbell, C.H.; Wilson, M.L. Distance to health services influences insecticide-treated net possession and use among six to 59 month-old children in Malawi. Malar. J. 2012, 11, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanford, J.I.; Kumar, S.; Luo, W.; MacEachren, A.M. It’s a long, long walk: Accessibility to hospitals, maternity and integrated health centers in Niger. Int. J. Health Geogr. 2012, 11, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, K.L.M.; Benova, L.; Campbell, O.M.R. A look back on how far to walk: Systematic review and meta-analysis of physical access to skilled care for childbirth in Sub-Saharan Africa. PLoS ONE 2017, 12, e0184432. [Google Scholar] [CrossRef] [Green Version]
- Shaw, N.T.; McGuire, S.K. Understanding the use of geographical information systems (GISs) in health informatics research: A review. BMJ Health Care Inform. 2017, 24, 228–233. [Google Scholar]
- Ali, M.; Rasool, S.; Park, J.K.; Saeed, S.; Ochiai, R.L.; Nizami, Q.; Acosta, C.J.; Bhutta, Z. Use of satellite imagery in constructing a household GIS database for health studies in Karachi, Pakistan. Int. J. Health Geogr. 2004, 3, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iqbal, N.T.; Syed, S.; Sadiq, K.; Khan, M.N.; Iqbal, J.; Ma, J.Z.; Umrani, F.; Ahmed, S.; Maier, E.A.; Denson, L.A.; et al. Study of Environmental Enteropathy and Malnutrition (SEEM) in Pakistan: Protocols for biopsy based biomarker discovery and validation. BMC Pediatr. 2019, 19, 247. [Google Scholar] [CrossRef]
- Anderson, N.B.; Armstead, C.A. Toward understanding the association of socioeconomic status and health: A new challenge for the biopsychosocial approach. Psychosom. Med. 1995, 57, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Poulain, T.; Vogel, M.; Kiess, W. Review on the role of socioeconomic status in child health and development. Curr. Opin. Pediatr. 2020, 32, 308–314. [Google Scholar] [CrossRef]
- Fox, E.W.; Ver Hoef, J.M.; Olsen, A.R. Comparing spatial regression to random forests for large environmental data sets. PLoS ONE 2020, 15, e0229509. [Google Scholar] [CrossRef] [Green Version]
- Hengl, T.; Heuvelink, G.B.; Kempen, B.; Leenaars, J.G.; Walsh, M.G.; Shepherd, K.D.; Sila, A.; MacMillan, R.A.; Mendes de Jesus, J.; Tamene, L.; et al. Mapping Soil Properties of Africa at 250 m Resolution: Random Forests Significantly Improve Current Predictions. PLoS ONE 2015, 10, e0125814. [Google Scholar] [CrossRef] [PubMed]
- Murphy, B.; Müller, S.; Yurchak, R. GeoStat-Framework/PyKrige v1.5.1; Zenodo: Geneva, Switzerland, 2020. [Google Scholar]
- Zaidi, S.A.; Sahibzada, S.A. Issues in Pakistan’s Health Sector [with Comments]. Pak. Dev. Rev. 1986, 25, 671–682. [Google Scholar] [CrossRef] [Green Version]
- Douthit, N.; Kiv, S.; Dwolatzky, T.; Biswas, S. Exposing some important barriers to health care access in the rural USA. Public Health 2015, 129, 611–620. [Google Scholar] [CrossRef] [PubMed]
- Puett, C.; Guerrero, S. Barriers to access for severe acute malnutrition treatment services in Pakistan and Ethiopia: A comparative qualitative analysis. Public Health Nutr. 2015, 18, 1873–1882. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adler, N.E.; Newman, K. Socioeconomic disparities in health: Pathways and policies. Health Aff. 2002, 21, 60–76. [Google Scholar] [CrossRef] [PubMed]
- Vukojevic, M.; Zovko, A.; Talic, I.; Tanovic, M.; Resic, B.; Vrdoljak, I.; Splavski, B. Parental Socioeconomic Status as a Predictor of Physical and Mental Health Outcomes in Children—Literature Review. Acta Clin. Croat. 2017, 56, 742–748. [Google Scholar] [CrossRef] [Green Version]
- Victora, C.G.; Wagstaff, A.; Schellenberg, J.A.; Gwatkin, D.; Claeson, M.; Habicht, J.P. Applying an equity lens to child health and mortality: More of the same is not enough. Lancet 2003, 362, 233–241. [Google Scholar] [CrossRef]
- Saleh, R. Secondary Level Health Facilities Assessment in Sindh 2011; World Health Organization: Islamabad, Pakistan, 2011. [Google Scholar]
- Olofin, I.; McDonald, C.M.; Ezzati, M.; Flaxman, S.; Black, R.E.; Fawzi, W.W.; Caulfield, L.E.; Danaei, G. Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: A pooled analysis of ten prospective studies. PLoS ONE 2013, 8, e64636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salam, R.A.; Qureshi, R.N.; Sheikh, S.; Khowaja, A.R.; Sawchuck, D.; Vidler, M.; von Dadelszen, P.; Zaidi, S.; Bhutta, Z. Potential for task-sharing to Lady Health Workers for identification and emergency management of pre-eclampsia at community level in Pakistan. Reprod. Health 2016, 13 (Suppl. 2), 107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | Mean (±SD) |
|---|---|
| Age at Enrollment (months, (mo)) | 4.2 (±1.0) |
| HAZ at Enrollment (mo) | −2.3 (±1.4) |
| WAZ at Enrollment (mo) | −3.6 (±1.4) |
| WHZ at Enrollment (mo) | −2.6 (±0.7) |
| Weight Difference from 0–6 to 24 months (kg) | 3.0 (±0.9) |
| Prevalence of ARI per year * | 54.2 (±53.3) |
| ARI Episodes ** | 5.0 (±3.6) |
| Prevalence of Diarrhea per year *** | 50.0 (±34.3) |
| Diarrhea Episodes **** | 14.8 (±17.7) |
| Distance from Healthcare Facility | 2.3 (±1.1) km 1.4 (±0.7) mi |
| Distance from Secondary Hospital | 6.5 (±3.5) km 4.0 (±2.2) mi |
| Distance from Maternal Health Center | 6.3 (±3.6) km 3.9 (±2.2) mi |
| Distance from Basic Health Unit | 3.6 (±1.4) km 2.2 (±0.9) mi |
| Distance from Rural Health Center | 9.0 (±4.8) km 5.6 (±3.0) mi |
| Distance from Dispensary | 4.0 (±1.8) km 2.5 (±1.1) mi |
| Variable | Secondary Hospital | Maternal Health Center | Basic Health Unit | Rural Health Center | Dispensary | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Correlation Coefficient | p-Value | Correlation Coefficient | p-Value | Correlation Coefficient | p-Value | Correlation Coefficient | p-Value | Correlation Coefficient | p-Value | |
| ARI Episodes | 0.057 | 0.334 | 0.067 | 0.258 | −0.081 | 0.176 | −0.154 | 0.009 | 0.022 | 0.711 |
| Prevalence of ARI | 0.154 | 0.009 | 0.185 | 0.002 | −0.126 | 0.034 | −0.212 | <0.001 | −0.044 | 0.466 |
| Diarrhea Episodes | 0.151 | 0.010 | 0.163 | 0.006 | −0.079 | 0.183 | −0.260 | <0.001 | −0.057 | 0.335 |
| Prevalence of Diarrhea | 0.228 | <0.001 | 0.223 | <0.001 | −0.044 | 0.459 | −0.212 | <0.001 | −0.005 | 0.940 |
| Delta Weight | −0.039 | 0.515 | −0.049 | 0.416 | −0.108 | 0.070 | 0.066 | 0.271 | −0.026 | 0.662 |
| Delta HAZ | 0.067 | 0.260 | −0.014 | 0.816 | −0.104 | 0.080 | 0.099 | 0.097 | −0.009 | 0.885 |
| Delta WAZ | 0.008 | 0.893 | −0.021 | 0.723 | −0.087 | 0.144 | 0.074 | 0.215 | −0.046 | 0.442 |
| Delta WHZ | −0.044 | 0.464 | −0.024 | 0.687 | −0.041 | 0.497 | 0.030 | 0.617 | −0.042 | 0.477 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corden, E.; Siddiqui, S.H.; Sharma, Y.; Raghib, M.F.; Adorno, W., III; Zulqarnain, F.; Ehsan, L.; Shrivastava, A.; Ahmed, S.; Umrani, F.; et al. Distance from Healthcare Facilities Is Associated with Increased Morbidity of Acute Infection in Pediatric Patients in Matiari, Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 11691. https://doi.org/10.3390/ijerph182111691
Corden E, Siddiqui SH, Sharma Y, Raghib MF, Adorno W III, Zulqarnain F, Ehsan L, Shrivastava A, Ahmed S, Umrani F, et al. Distance from Healthcare Facilities Is Associated with Increased Morbidity of Acute Infection in Pediatric Patients in Matiari, Pakistan. International Journal of Environmental Research and Public Health. 2021; 18(21):11691. https://doi.org/10.3390/ijerph182111691
Chicago/Turabian StyleCorden, Elise, Saman Hasan Siddiqui, Yash Sharma, Muhammad Faraz Raghib, William Adorno, III, Fatima Zulqarnain, Lubaina Ehsan, Aman Shrivastava, Sheraz Ahmed, Fayaz Umrani, and et al. 2021. "Distance from Healthcare Facilities Is Associated with Increased Morbidity of Acute Infection in Pediatric Patients in Matiari, Pakistan" International Journal of Environmental Research and Public Health 18, no. 21: 11691. https://doi.org/10.3390/ijerph182111691






