The Unmet Medical Demand among China’s Urban Residents
Abstract
:1. Introduction
2. Literature Review
3. Methodology
3.1. Model Specification
3.2. Econometric Specification
4. Data
5. Results and Discussion
5.1. Econometric Results
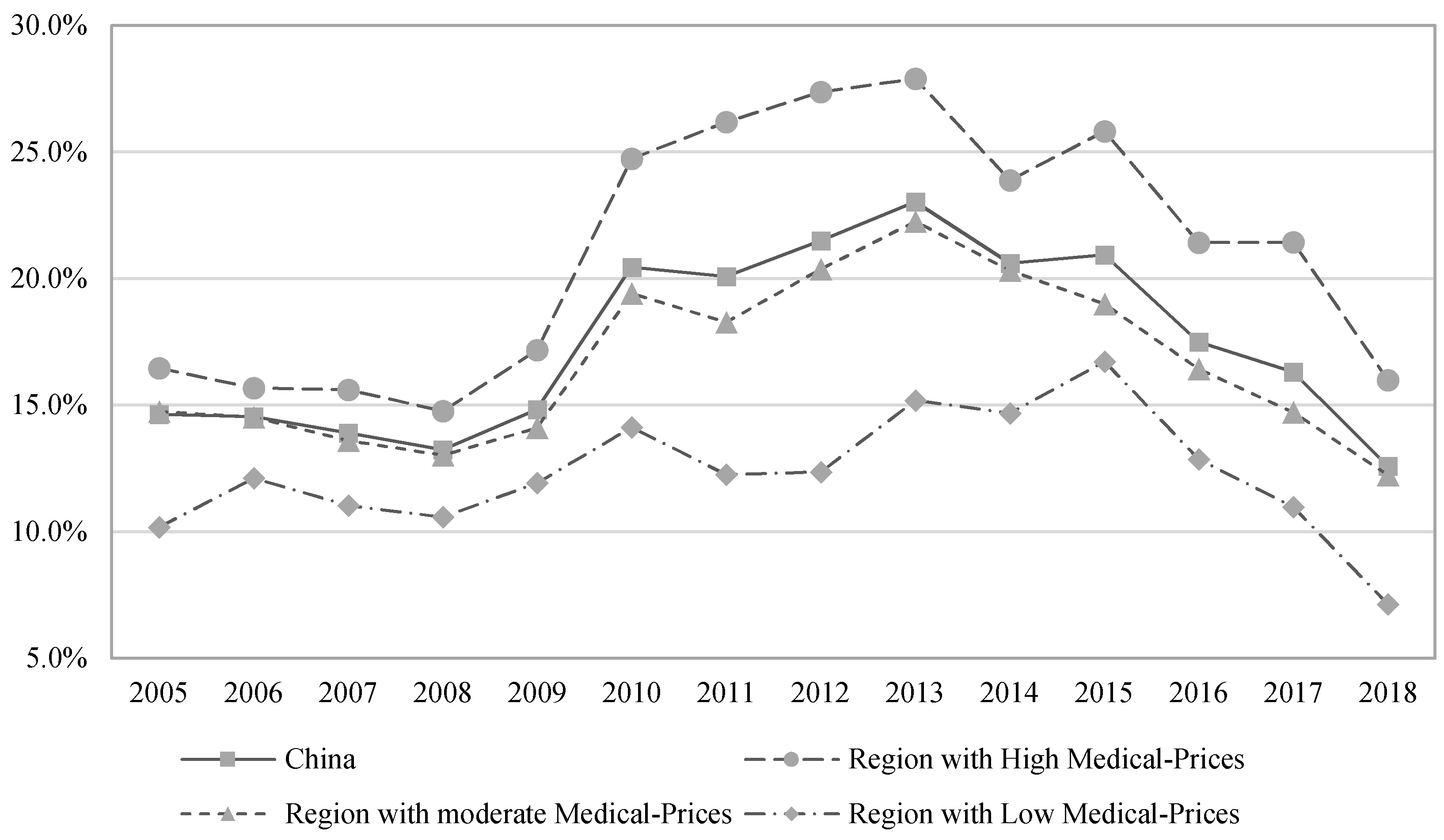
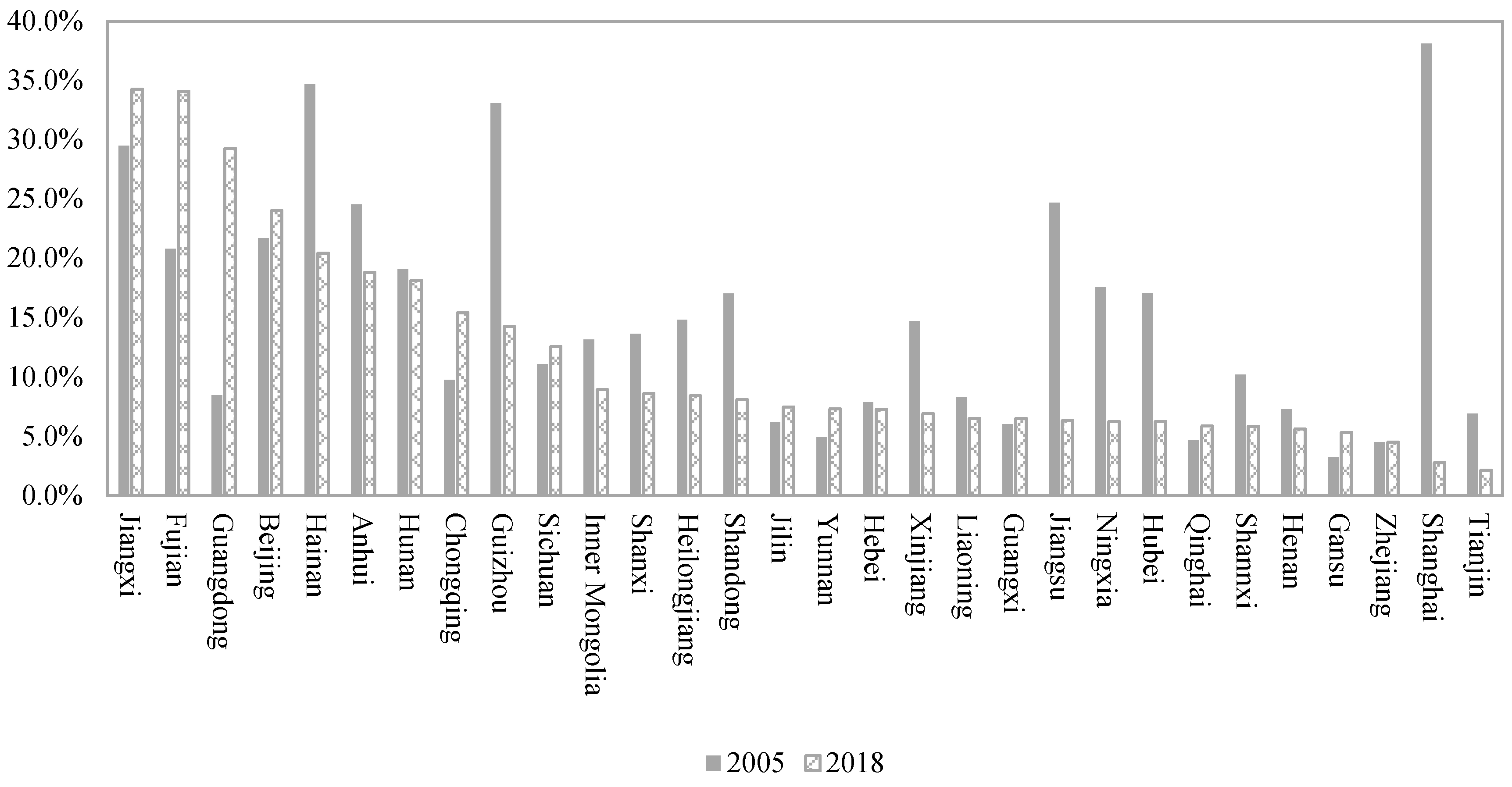
5.2. Unmet Medical Demand
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morris, S.; Sutton, M.; Gravelle, H. Inequity and inequality in the use of health care in England: An empirical investigation. Soc. Sci. Med. 2005, 60, 1251–1266. [Google Scholar] [CrossRef] [PubMed]
- Arrow, K.J. Uncertainty and the Welfare Economics of Medical Care. Am. Econ. Rev. 1963, 53, 941–973. [Google Scholar]
- Salm, M.; Wübker, A. Sources of regional variation in healthcare utilization in Germany. J. Health Econ. 2019, 69, 102271. [Google Scholar] [CrossRef] [PubMed]
- Tracking Universal Health Coverage: 2017 Global Monitoring Report. Available online: https://documents1.worldbank.org/curated/en/640121513095868125/pdf/122029-WP-REVISED-PUBLIC.pdf (accessed on 13 December 2017).
- Wagstaff, A. Poverty and health sector inequalities. Bull. World Health Organ. 2002, 80, 97–105. [Google Scholar]
- Statistical Bulletin on China’s Health Development 2019. Available online: http://www.nhc.gov.cn/guihuaxxs/s10748/202006/ebfe31f24cc145b198dd730603ec4442.shtml (accessed on 6 June 2020).
- Statistical Information Center of National Health Commission PRC. The Sixth Survey of National Health Services of China; People’s Medical Publishing House: Beijing, China, 2021; pp. 42–59.
- Reeves, A.; McKee, M.; Stuckler, D. The attack on universal health coverage in Europe: Recession, austerity and unmet needs. Eur. J. Public Health 2015, 25, 364–365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Connolly, S.; Wren, M.-A. Unmet healthcare needs in Ireland: Analysis using the EU-SILC survey. Health Policy 2017, 121, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.S.; Jung, B.; Kim, D.; Ha, I.H. Factors underlying unmet medical needs: A cross-sectional study. Int. J. Environ. Res. Public Health 2019, 16, 2391. [Google Scholar] [CrossRef] [Green Version]
- Njagi, P.; Arsenijevic, J.; Groot, W. Cost–related unmet need for healthcare services in Kenya. BMC Health Serv. Res. 2020, 20, 322. [Google Scholar] [CrossRef]
- Jung, B.; Ha, I.-H. Determining the reasons for unmet healthcare needs in South Korea: A secondary data analysis. Health Qual. Life Outcomes 2021, 19, 99. [Google Scholar] [CrossRef]
- Sanmartin, C.; Houle, C.; Tremblay, S.; Berthelot, J.-M. Changes in unmet health care needs. Health Rep. 2002, 13, 15–21. [Google Scholar] [PubMed]
- Pappa, E.; Kontodimopoulos, N.; Papadopoulos, A.; Tountas, Y.; Niakas, D. Investigating Unmet Health Needs in Primary Health Care Services in a Representative Sample of the Greek Population. Int. J. Environ. Res. Public Health 2013, 10, 2017–2027. [Google Scholar] [CrossRef] [Green Version]
- Grossman, M. On the Concept of Health Capital and the Demand for Health. J. Politics Econ. 1972, 80, 223–255. [Google Scholar] [CrossRef] [Green Version]
- Mocan, H.; Tekin, E.; Zax, J.S. The Demand for Medical Care in Urban China. World Dev. 2004, 32, 289–304. [Google Scholar] [CrossRef] [Green Version]
- Chaupain-Guillot, S.; Guillot, O. Health system characteristics and unmet care needs in Europe: An analysis based on EU-SILC data. Eur. J. Health Econ. 2015, 16, 781–796. [Google Scholar] [CrossRef]
- Fiorillo, D. Reasons for unmet needs for health care: The role of social capital and social support in some western EU countries. Int. J. Health Econ. Manag. 2020, 20, 79–98. [Google Scholar] [CrossRef] [Green Version]
- Narayan, P.K.; Narayan, S. Does environmental quality influence health expenditures? Empirical evidence from a panel of selected OECD countries. Ecol. Econ. 2008, 65, 367–374. [Google Scholar] [CrossRef]
- Liljas, B. The demand for health with uncertainty and insurance. J. Health Econ. 1998, 17, 153–170. [Google Scholar] [CrossRef]
- Ariizumi, H. Effect of public long-term care insurance on consumption, medical care demand, and welfare. J. Health Econ. 2008, 27, 1423–1435. [Google Scholar] [CrossRef]
- Fors, S.; Thorslund, M. Enduring inequality: Educational disparities in health among the oldest old in Sweden 1992–2011. Int. J. Public Health 2015, 60, 91–98. [Google Scholar] [CrossRef]
- Ross, C.E.; Wu, C.L. Education, age, and the cumulative advantage in health. J. Health Soc. Behav. 1996, 37, 104–120. [Google Scholar] [CrossRef]
- Blundell, R.; Windmeijer, F. Identifying demand for health resources using waiting times information. Health Econ. 2000, 9, 465–474. [Google Scholar] [CrossRef]
- Zhou, Z.; Su, Y.; Gao, J.; Xu, L.; Zhang, Y. New estimates of elasticity of demand for healthcare in rural China. Health Policy 2011, 103, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Mielck, A.; Kiess, R.; Knesebeck, O.V.D.; Stirbu, I.; E Kunst, A. Association between forgone care and household income among the elderly in five Western European countries–analyses based on survey data from the SHARE-study. BMC Health Serv. Res. 2009, 9, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jang, H.-Y.; Ko, Y.; Han, S.-Y. The Effects of Social Networks of the Older Adults with Limited Instrumental Activities of Daily Living on Unmet Medical Needs. Int. J. Environ. Res. Public Health 2021, 18, 27. [Google Scholar]
- Erbsland, M.; Ried, W.; Ulrich, V. Health, health care, and the environment. Econometric evidence from German micro data. Health Econ. 1995, 4, 169–182. [Google Scholar] [CrossRef] [Green Version]
- Hadley, J. Sicker and poorer--the consequences of being uninsured: A review of the research on the relationship between health insurance, medical care use, health, work, and income. Med. Care Res Rev. 2003, 60, 3S–75S. [Google Scholar] [CrossRef]
- Aigner, D.; Lovell, C.; Schmidt, P. Formulation and estimation of stochastic frontier production function models. J. Econ. 1977, 6, 21–37. [Google Scholar] [CrossRef]
- Battese, G.E.; Coelli, T.J. A model for technical inefficiency effects in a stochastic frontier production function for panel data. Empir. Econ. 1995, 20, 325–332. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, P.; Sickles, R.C. Production frontiers and panel data. J. Bus. Econ. Stat. 1984, 2, 367–374. [Google Scholar]
- Cornwell, C.; Schmidt, P.; Sickles, R.C. Production frontiers with cross-sectional and time-series variation in efficiency levels. J. Econom. 1990, 46, 185–200. [Google Scholar] [CrossRef]
- Greene, W. Reconsidering heterogeneity in panel data estimators of the stochastic frontier model. J. Econ. 2005, 126, 269–303. [Google Scholar] [CrossRef]
- Farsi, M.; Filippini, M.; Kuenzle, M. Unobserved heterogeneity in stochastic cost frontier models: An application to Swiss nursing homes. Appl. Econ. 2005, 37, 2127–2141. [Google Scholar] [CrossRef]
- Mundlak, Y. On the Pooling of Time Series and Cross Section Data. Econom. J. Econom. Soc. 1978, 46, 69–85. [Google Scholar] [CrossRef]
- Huang, C.J.; Liu, J.-T. Estimation of a non-neutral stochastic frontier production function. J. Prod. Anal. 1994, 5, 171–180. [Google Scholar] [CrossRef]
- Wang, H.J.; Schmidt, P. One-step and two-step estimation of the effects of exogenous variables on technical efficiency levels. J. Product. Anal. 2002, 18, 129–144. [Google Scholar] [CrossRef]
- National Bureau of Statistics PRC. China Urban life and Price Yearbook (2006–2019); China Statistics Press: Beijing, China, 2020; pp. 72–84.
- National Bureau of Statistics PRC. Yearbook of China Insurance (2006–2019); China Statistics Press: Beijing, China, 2020; pp. 81–88.
- National Bureau of Statistics PRC. China Statistical Yearbook (2006–2019); China Statistics Press: Beijing, China, 2020; pp. 216–218.
- National Bureau of Statistics PRC. China Health Statistical Yearbook (2006–2019); China Statistics Press: Beijing, China, 2020; pp. 78–79.
- National Bureau of Statistics PRC. China Population and Employment Yearbook (2006–2019); China Statistics Press: Beijing, China, 2020; pp. 10–11.
- Mehrara, M.; Musai, M.; Amiri, H. The relationship between health expenditure and GDP in OECD countries using PSTR. Eur. J. Econ. Financ. Adm. Sci. 2010, 24, 50–58. [Google Scholar]
- Yang, S.; Wang, D.; Li, W.; Wang, C.; Yang, X.; Lo, K. Decoupling of Elderly Healthcare Demand and Expenditure in China. Healthcare 2021, 9, 1346. [Google Scholar] [CrossRef]
- Newhouse, J.P.; Phelps, C.E. New estimates of price and income elasticities of medical care services. In The Role of Health Insurance in the Health Services Sector; Rosett, R.N., Ed.; NBER: New York, NY, USA, 1976; pp. 261–320. [Google Scholar]
- Baltagi, B.H. An alternative derivation of Mundlak’s fixed effects results using system estimation. Economet. Theor. 2006, 22, 1191–1194. [Google Scholar] [CrossRef]
- Conti, G.; Heckman, J.; Urzua, S. The Education-Health Gradient. Am. Econ. Rev. 2010, 100, 234–238. [Google Scholar] [CrossRef] [Green Version]
| Study | Concept | Method | Explaining Variables |
|---|---|---|---|
| Grossman (1972) [15] | Demand for health | Conceptual Framework | Medical care, age, time inputs, goods input, oc human capital |
| Blundell and Wind-meijer (2000) [24] | Demand for health services at the ward level in the UK | Semi-parametric selection model | Average waiting time routine surgery in days, standardized estimated costs 1991–1992 acute care, NHS (National Health Service of the United Kingdom) hospital accessibility, general practitioner accessibility, the proportion of the 75 years and older not in nursing and residential homes, private hospital accessibility, standardized mortality ratio ages 0–74, standardized illness ratio ages 0–74, for residents in households only, the proportion of persons with head in manual class, proportion of those of pensionable age living alone, the proportion of dependents in single households, proportion of the economically active that is unemployed, and proportion of residents in households with no car |
| Mocan et al. (2004) [16] | Demand for medical care covered urban households | Two-part model and a discrete factor model | Price of medical care, price of food, the opportunity cost of time, age, environmental, and the variables that influence the productivity of health investment |
| Ariizumi (2008) [21] | Medical care demand | Conceptual Framework | Public long-term care insurance, age, health status, medical investment, level of consumption, and presence of a chronic illness |
| Zhou et al. (2011) [25] | Demand for healthcare across individuals from rural China | The probit regression model, zero-truncated negative binomial equation | Outpatient price, inpatient price, income, gender, age, and marriage |
| Pappa et al. (2013) [14] | Unmet health needs across 1000 consenting subjects | Multiple binary logistic regression analysis | Sex, age, marital status, children, education, occupation, urbanity, physician, consultations, and chronic diseases |
| Chaupain-Guillot and Guillot (2015) [17] | Unmet care needs across 400,000 individuals aged 16 and over | Multilevel logistic equation | Sex, age, self-perceived health, citizenship, education level, family situation, household income, housing tenure status, the existence of debts, and whether the household has a car or not |
| Connolly and Wren (2017) [9] | Unmet healthcare needs across 4922 households in Ireland | Multivariate logistic regression | Sex, age group, marital status, education, principal economic status, income, eligibility category, health status, and chronic illness |
| Yoon et al. (2019) [10] | Unmet medical needs across adults over 19 years old from Korea | Multiple logistic regression | Sex, age, education, marital status, economic activity, income, medical insurance type, private insurance, non-covered treatment, chronic disease, disability, regular exercise, pain, self-rated health status, and depression |
| Fiorillo (2020) [18] | Unmet needs for health care across 260,000 respondents from 14 Member States of the EU | Expanded probit model | Social capital, social support, and individual characteristics (gender, marital status, age, household size, country of birth, education, economic features, health status, and size of municipality) |
| Njagi et al. (2020) [11] | Unmet need for healthcare services across 33,675 households n from Kenya | Multilevel regression model | Gender, age, education level, employment status, type of service, self-rated health, chronic illness, insurance status, household size, residence, and wealth index |
| Jang et al. (2021) [27] | Unmet medical needs across 2281 older adults with limited IADL from Koreans | Logistic regression analysis | Age, gender, educational level, household income, number of chronic diseases, living arrangement, contact with friend and neighbor, social activity, emotional support, instrumental support, physical support, and financial support |
| Jung and Ha (2021) [12] | Unmet healthcare needs across 26,598 participants aged 19 years and older from Korea | Multiple logistic regression models | Age, marital status, family member, education level, region, employment, income, occupation, medical insurance type, private insurance, smoking history, alcohol consumption, body mass index, exercise, self-rated health status, stress level, pain, and depression |
| Mean | Maximum | Minimum | Coefficient of Variance | |
|---|---|---|---|---|
| Medical Demand | 1.775 | 2.464 | 1.003 | 0.144 |
| Income | 9.730 | 10.826 | 8.986 | 0.040 |
| Medical Price | 4.966 | 5.999 | 3.993 | 0.060 |
| Health Condition | 2.790 | 4.760 | 0.095 | 0.263 |
| Medical Resources | 1.819 | 3.311 | 0.920 | 0.225 |
| Education | 2.166 | 2.530 | 1.853 | 0.052 |
| Aging | 2.190 | 2.728 | 1.449 | 0.106 |
| Health Insurance | 7.434 | 8.775 | 6.263 | 0.061 |
| Public Health Care | 5.875 | 7.428 | 3.655 | 0.138 |
| OLS | RE | FRE | MRE | |||
|---|---|---|---|---|---|---|
| Main Equation | Auxiliary Equation | Main Equation | Auxiliary Equation | |||
| Income | 0.359 *** | 0.785 *** | 0.341 *** | 0.306 *** | −3.040 | |
| (0.065) | (0.063) | (0.060) | (0.059) | (2.154) | ||
| Medical Price | −0.519 *** | −0.601 *** | −0.495 *** | −0.447 *** | ||
| (0.060) | (0.085) | (0.055) | (0.065) | |||
| Health Condition | 0.018 | 0.064 *** | 0.022 | 0.008 | 0.058 | |
| (0.023) | (0.020) | (0.022) | (0.022) | (0.761) | ||
| Medical Resources | 0.276 *** | 0.008 | 0.300 *** | 0.292 *** | −0.959 | |
| (0.033) | (0.037) | (0.033) | (0.032) | (0.905) | ||
| Constant | 0.308 | −3.069 *** | 0.534 | −4.310 *** | 0.685 | 26.726 |
| (0.536) | (0.441) | (0.498) | (0.278) | (0.479) | (22.479) | |
| uit | 0.285 *** | 0.276 *** | ||||
| (0.025) | (0.021) | |||||
| Lambda | 2.494 *** | 2.490 *** | ||||
| (0.039) | (0.040) | |||||
| Prediction Squared | −0.071 | −0.250 | −0.271 | |||
| (0.344) | (0.320) | (0.355) | ||||
| MRE (1) | MRE (2) | MRE (3) | MRE (4) | |||||
|---|---|---|---|---|---|---|---|---|
| Main Equation | Auxiliary Equation | Main Equation | Auxiliary Equation | Main Equation | Auxiliary Equation | Main Equation | Auxiliary Equation | |
| Medical Demand | ||||||||
| Income | 0.297 *** | −5.358 *** | 0.422 *** | −1.727 ** | 0.339 *** | −1.529 * | 0.247 *** | −4.400 ** |
| (0.054) | (1.939) | (0.063) | (0.762) | (0.073) | (0.781) | (0.055) | (2.003) | |
| Medical Price | −0.264 *** | −0.494 *** | −0.393 *** | −0.178 ** | ||||
| (0.074) | (0.077) | (0.084) | (0.073) | |||||
| Health Conditions | 0.035 * | −0.389 | 0.056 ** | −0.772 ** | 0.049 ** | −0.686 ** | 0.030 * | 0.071 |
| (0.021) | (0.634) | (0.022) | (0.332) | (0.022) | (0.327) | (0.020) | (0.627) | |
| Medical Resources | 0.267 *** | −0.989 | 0.250 *** | 0.902 * | 0.235 *** | 0.959 * | 0.256 *** | −0.174 |
| (0.030) | (0.791) | (0.032) | (0.495) | (0.032) | (0.498) | (0.034) | (0.683) | |
| Constant | −0.190 | 50.491 ** | −0.402 | 13.809 * | −0.047 | 11.517 | −0.098 | 38.413 * |
| (0.510) | (19.988) | (0.565) | (7.862) | (0.574) | (8.122) | (0.484) | (20.720) | |
| The Unmet Medical Demand | ||||||||
| Medical Price | 3.498 *** | 6.718 ** | 8.550 *** | 5.800 *** | ||||
| (0.728) | (2.835) | (2.646) | (1.029) | |||||
| Education | −6.047 *** | −15.967 *** | −14.840 *** | −6.797 *** | ||||
| (1.366) | (4.958) | (3.989) | (1.486) | |||||
| Aging | −4.181 *** | −3.888 *** | −1.303 *** | |||||
| (1.359) | (1.231) | (0.401) | ||||||
| Medical Insurance | −1.847 ** | −2.095 *** | ||||||
| (0.817) | (0.490) | |||||||
| Public Medical Care | 0.496 * | |||||||
| (0.274) | ||||||||
| Constant | −7.073 *** | 5.565 | 7.163 | −1.600 | ||||
| (2.251) | (7.158) | (5.586) | (2.607) | |||||
| Lambda | 2.285 *** | 2.408 *** | 2.500 *** | 2.114 *** | ||||
| (0.040) | (0.040) | (0.039) | (0.041) | |||||
| Prediction Squared | −0.212 | −0.009 | −0.156 | −0.269 | ||||
| (0.427) | (0.345) | (0.446) | (0.503) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheng, P.; Yang, T.; Zhang, T. The Unmet Medical Demand among China’s Urban Residents. Int. J. Environ. Res. Public Health 2021, 18, 11708. https://doi.org/10.3390/ijerph182111708
Sheng P, Yang T, Zhang T. The Unmet Medical Demand among China’s Urban Residents. International Journal of Environmental Research and Public Health. 2021; 18(21):11708. https://doi.org/10.3390/ijerph182111708
Chicago/Turabian StyleSheng, Pengfei, Tingting Yang, and Tengfei Zhang. 2021. "The Unmet Medical Demand among China’s Urban Residents" International Journal of Environmental Research and Public Health 18, no. 21: 11708. https://doi.org/10.3390/ijerph182111708
APA StyleSheng, P., Yang, T., & Zhang, T. (2021). The Unmet Medical Demand among China’s Urban Residents. International Journal of Environmental Research and Public Health, 18(21), 11708. https://doi.org/10.3390/ijerph182111708





