Exploring Doctors’ Emerging Commitment to Rural and General Practice Roles over Their Early Career
Abstract
:1. Introduction
2. Materials and Methods
2.1. Context of this Study
2.2. Comparison Groups—Specialty and Practice Location
2.3. Key Outcomes
2.4. Covariates
2.5. Analyses
3. Results
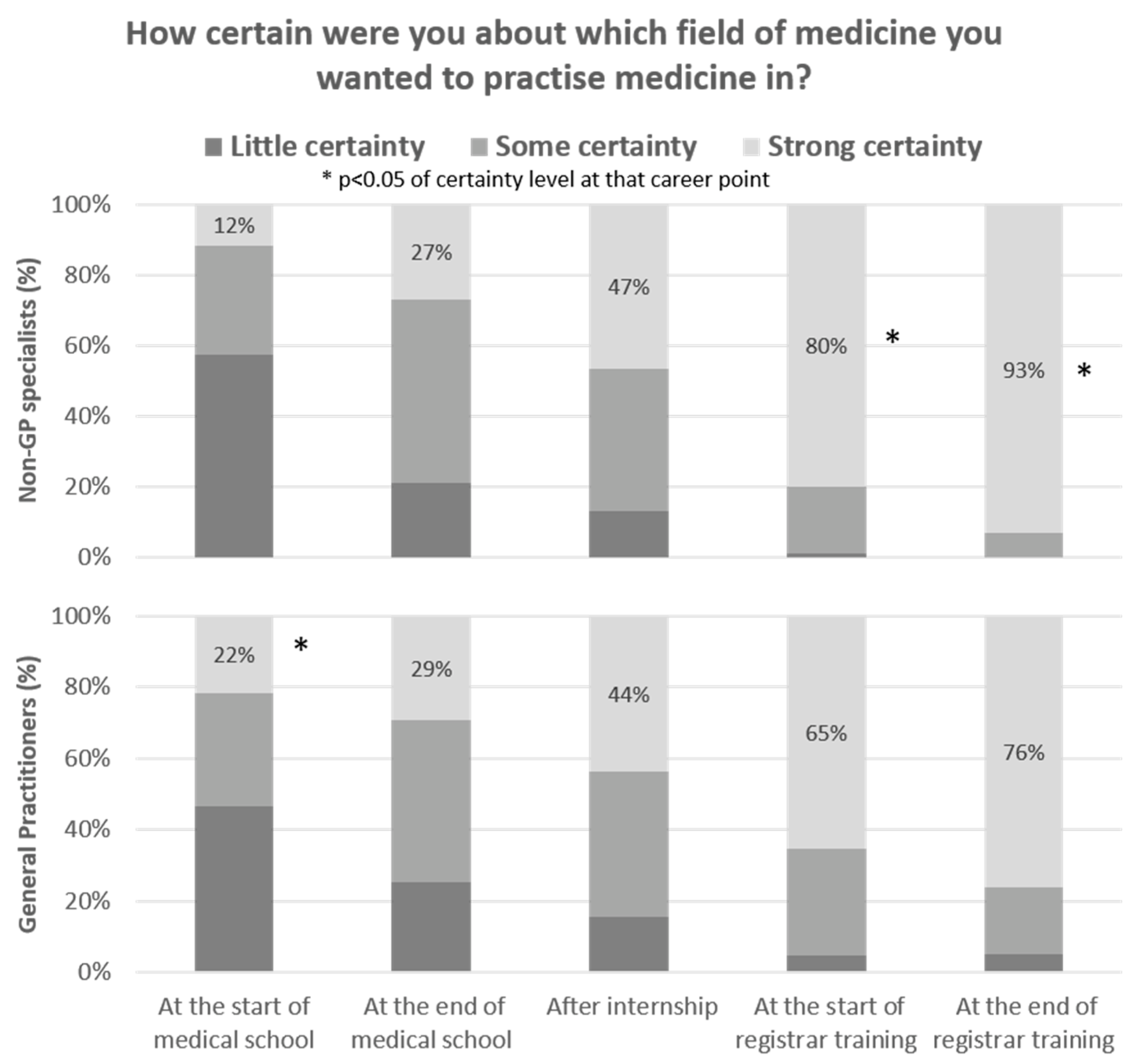
3.1. Certainty of Specialising as a GP or Non-GP Specialist
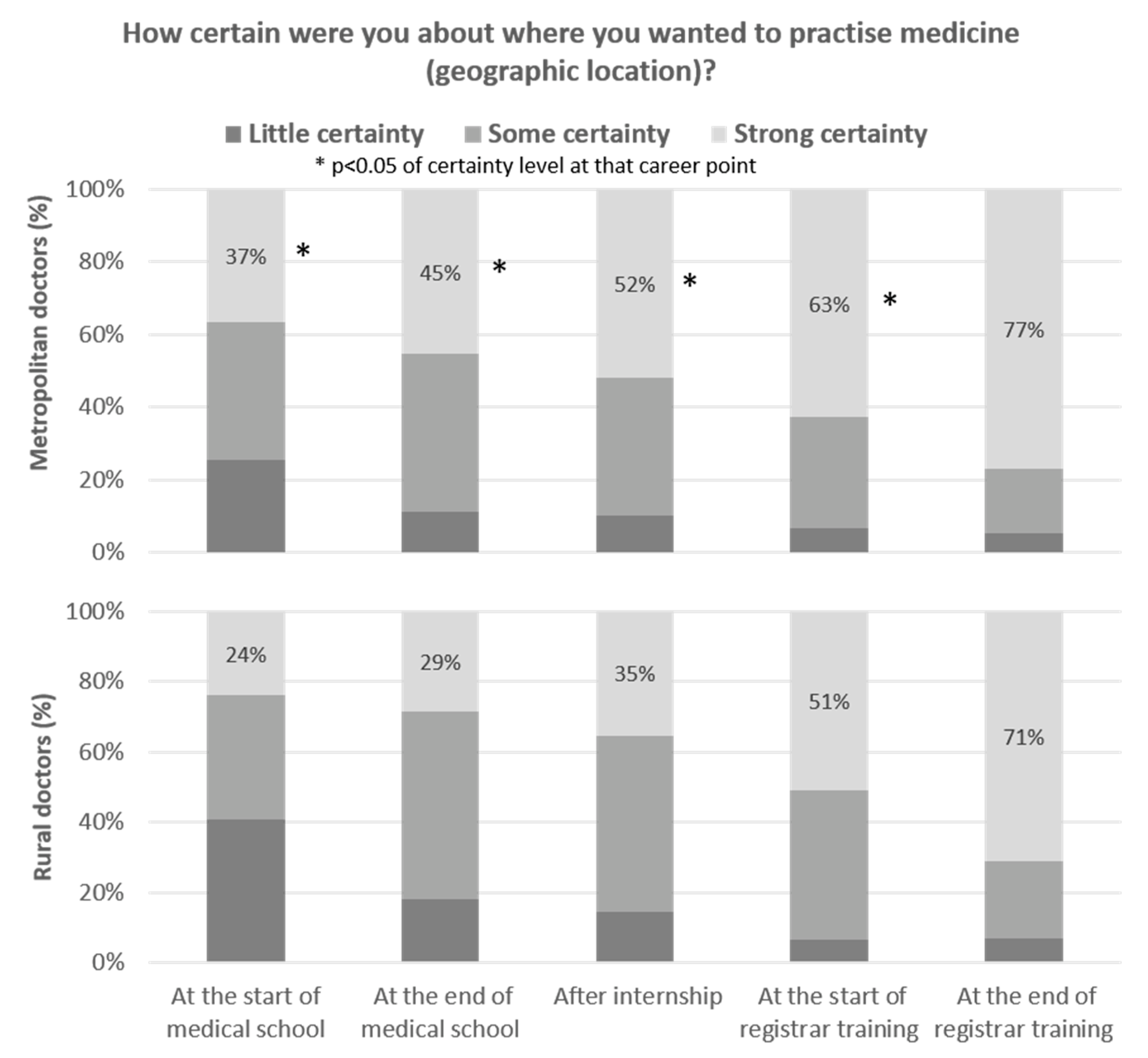
3.2. Certainty of Practising in Rural or Metropolitan Location
3.3. Other Influences on Certainty of Decision(s) of Specialty and Practice Location
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Verma, P.; Ford, J.A.; Stuart, A.; Howe, A.; Everington, S.; Steel, N. A systematic review of strategies to recruit and retain primary care doctors. BMC Health Serv. Res. 2016, 16, 126. [Google Scholar] [CrossRef] [Green Version]
- Dussault, G.; Franceschini, M.C. Not enough there, too many here: Understanding geographical imbalances in the distribution of the health workforce. Hum. Resour. Health 2006, 4, 12. [Google Scholar] [CrossRef] [PubMed]
- Starfield, B.; Shi, L.; Macinko, J. Contribution of Primary Care to Health Systems and Health. Milbank Q. 2005, 83, 457–502. [Google Scholar] [CrossRef]
- Prunuske, J. America Needs More Family Doctors: The 25x2030 Collaborative Aims to Get More Medical Students into Family Medicine. Am. Fam. Phys. 2020, 101, 82–83. [Google Scholar]
- Stigler, F.L.; Zipp, C.R.; Jeitler, K.; Semlitsch, T.; Siebenhofer, A. Comprehensive catalogue of international measures aimed at preventing general practitioner shortages. Fam. Pract. 2021, cmab045. [Google Scholar] [CrossRef] [PubMed]
- Alkot, M.M.; Gouda, M.A.; KhalafAllah, M.T.; Zahran, M.S.; Kallaf, M.M.; Zayed, A.M. Family Medicine in Egypt from Medical Students’ Perspective: A Nationwide Survey. Teach. Learn. Med. 2015, 27, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.L.; Wakerman, J.; Humphreys, J.S. Ensuring equity of access to primary health care in rural and remote Australia-what core services should be locally available? Int. J. Equity Health 2015, 14, 111. [Google Scholar] [CrossRef] [Green Version]
- Wilson, C.R.; Rourke, J.; Oandasan, I.F.; Bosco, C. Progress made on access to rural health care in Canada. Can. Fam. Phys. 2020, 66, 31–36. [Google Scholar]
- World Health Organization. Retention of the Health Workforce in Rural and Remote Areas: A Systematic Review; WHO: Geneva, Switzerland, 2020; Report No.: Human Resources for Health Observer Series No. 25. [Google Scholar]
- McGrail, M.R.; Wingrove, P.M.; Petterson, S.M.; Bazemore, A.W. Mobility of US Rural Primary Care Physicians During 2000–2014. Ann. Fam. Med. 2017, 15, 322–328. [Google Scholar] [CrossRef] [Green Version]
- Arshad, S.; McCombe, G.; Carberry, C.; Harrold, A.; Cullen, W. What factors influence medical students to enter a career in general practice? A scoping review. Ir. J. Med. Sci. 2020, 190, 657–665. [Google Scholar] [CrossRef]
- Scott, I.; Gowans, M.; Wright, B.; Brenneis, F.; Banner, S.; Boone, J. Determinants of choosing a career in family medicine. Can. Med. Assoc. J. 2010, 183, E1–E8. [Google Scholar] [CrossRef] [Green Version]
- Asghari, S.; Kirkland, M.; Blackmore, J.; Boyd, S.; Farrell, A.; Rourke, J.; Aubrey-Bassler, K.; Godwin, M.; Oandasan, I.; Walczak, A. A systematic review of reviews: Recruitment and retention of rural family physicians. Can. J. Rural. Med. 2020, 25, 20–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parlier, A.B.; Galvin, S.L.; Thach, S.; Kruidenier, D.; Fagan, E.B. The road to rural primary care: A narrative review of factors that help develop, recruit, and retain rural primary care physicians. Acad. Med. 2018, 93, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Weinhold, I.; Gurtner, S. Understanding shortages of sufficient health care in rural areas. Health Policy 2014, 118, 201–214. [Google Scholar] [CrossRef] [PubMed]
- Australian Government Department of Health. Health Workforce Data-Data Tool. 2019. Available online: https://hwd.health.gov.au/datatool.html (accessed on 19 March 2021).
- O’Sullivan, B.; McGrail, M.; Gurney, T.; Martin, P. A Realist Evaluation of Theory about Triggers for Doctors Choosing a Generalist or Specialist Medical Career. Int. J. Environ. Res. Public Health 2020, 17, 8566. [Google Scholar] [CrossRef]
- Querido, S.J.; Wigersma, L.; Cate, O.T. Traveling by winding roads or highways: Stability of medical students’ specialty preferences over time. Med. Teach. 2020, 42, 1298–1300. [Google Scholar] [CrossRef]
- Compton, M.T.; Frank, E.; Elon, L.; Carrera, J. Changes in U.S. medical students’ specialty interests over the course of medical school. J. Gen. Intern. Med. 2008, 23, 1095–1100. [Google Scholar] [CrossRef] [Green Version]
- Singh, A.; Alberti, H. Why UK medical students change career preferences: An interview study. Perspect. Med. Educ. 2020, 10, 41–49. [Google Scholar] [CrossRef]
- Cantone, R.E.; Deiorio, N.M.; Polston, A.; Schneider, B. Specialty choice stability: Are there implications for early entry into residency? PRiMER 2018, 2, 30. [Google Scholar] [CrossRef]
- Fischer, J.P.; Clinite, K.; Sullivan, E.; Jenkins, T.M.; Bourne, C.L.; Chou, C.; Diemer, G.; Dunne, D.; Hartung, P.J.; Paauw, D.; et al. Specialty and Lifestyle Preference Changes during Medical School. Med. Sci. Educ. 2019, 29, 995–1001. [Google Scholar] [CrossRef]
- Kaur, B.; Carberry, A.; Hogan, N.; Roberton, D.; Beilby, J. The medical schools outcomes database project: Australian medical student characteristics. BMC Med. Educ. 2014, 14, 18. [Google Scholar] [CrossRef] [Green Version]
- Bustraan, J.; Dijkhuizen, K.; Velthuis, S.; van der Post, R.; Driessen, E.; van Lith, J.M.M.; de Beaufort, A.J. Why do trainees leave hospital-based specialty training? A nationwide survey study investigating factors involved in attrition and subsequent career choices in the Netherlands. BMJ Open 2019, 9, e028631. [Google Scholar] [CrossRef]
- Hollis, A.C.; Streeter, J.; Van Hamel, C.; Milburn, L.; Alberti, H. The new cultural norm: Reasons why UK foundation doctors are choosing not to go straight into speciality training. BMC Med. Educ. 2020, 20, 282. [Google Scholar] [CrossRef]
- Dolea, C.; Stormont, L.; Braichet, J.-M. Evaluated strategies to increase attraction and retention of health workers in remote and rural areas. Bull. World Health Organ. 2010, 88, 379–385. [Google Scholar] [CrossRef]
- Farmer, J.; Kenny, A.; McKinstry, C.; Huysmans, R.D. A scoping review of the association between rural medical education and rural practice location. Hum. Resour. Health 2015, 13, 1–15. [Google Scholar] [CrossRef] [Green Version]
- McGrail, M.R.; Humphreys, J.S.; Joyce, C.M. Nature of association between rural background and practice location: A comparison of general practitioners and specialists. BMC Health Serv. Res. 2011, 11, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGirr, J.; Seal, A.; Barnard, A.; Cheek, C.; Garne, D.L.; Greenhill, J.; Kondalsamy-Chennakesavan, S.; Luscombe, G.; May, J.; McLeod, J.; et al. The Australian Rural Clinical School (RCS) program sup-ports rural medical workforce: Evidence from a cross-sectional study of 12 RCSs. Rural Remote Health 2019, 19, 4971. [Google Scholar]
- O’Sullivan, B.G.; McGrail, M.R. Effective dimensions of rural undergraduate training and the value of training policies for encouraging rural work. Med. Educ. 2020, 54, 364–374. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.; McGrail, M.; O’Sullivan, B.G.; Russell, D.J. Outcomes of a one-year longi-tudinal integrated medical clerkship in small rural Victorian communities. Rural Remote Health 2019, 19, 4987. [Google Scholar] [PubMed]
- Hirsh, D.A.; Ogur, B.; Thibault, G.E.; Cox, M. “Continuity” as an Organizing Principle for Clinical Education Reform. N. Engl. J. Med. 2007, 356, 858–866. [Google Scholar] [CrossRef] [Green Version]
- Jones, M.; Bushnell, J.A.; Humphreys, J. Are rural placements positively associated with rural intentions in medical graduates? Med. Educ. 2014, 48, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.; DeWitt, D.; Pallant, J.; Cunningham, C. Rural origin plus a rural clinical school placement is a significant predictor of medical students’ intentions to practice rurally: A multi-university study. Rural Remote. Health 2012, 12. [Google Scholar] [CrossRef]
- Playford, D.; Ngo, H.; Puddey, I. Intention mutability and translation of rural intention into actual rural medical practice. Med. Educ. 2021, 55, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Health Workforce Australia. Australia’s Future Health Workforce–Doctors; HWA: Adelaide, Australia, 2014. [Google Scholar]
- O’Sullivan, B.G.; McGrail, M.; Gurney, T. Selection, training and employment to encourage early-career doctors to pursue a rural postgraduate training pathway. Aust. J. Rural Health 2021, 29, 267–271. [Google Scholar] [CrossRef]
- Australian Government Department of Health. Health Workforce Classification: Modified Monash Model Canberra; Department of Health: Canberra, Australia, 2020. Available online: https://www.health.gov.au/health-workforce/health-workforce-classifications/modified-monash-model (accessed on 16 September 2021).
- Worley, P.; O’Sullivan, B.G.; Ellis, R. From locum-led outposts to locally led continuous rural training networks: The National Rural Generalist Pathway. Med. J. Aust. 2019, 211, 57–60. [Google Scholar] [CrossRef]
- Alberti, H.; Banner, K.; Collingwood, H.; Merritt, K. ‘Just a GP’: A mixed method study of undermining of general practice as a career choice in the UK. BMJ Open 2017, 7, e018520. [Google Scholar] [CrossRef] [Green Version]
- Playford, D.; May, J.A.; Ngo, H.; Puddey, I.B. Decline in new medical graduates registered as general practitioners. Med. J. Aust. 2020, 212, 421–422. [Google Scholar] [CrossRef] [Green Version]
- Vohra, A.; Ladyshewsky, R.; Trumble, S. Factors that affect general practice as a choice of medical speciality: Implications for policy development. Aust. Health Rev. 2019, 43, 230. [Google Scholar] [CrossRef]
- Cuesta-Briand, B.; Coleman, M.; Ledingham, R.; Moore, S.; Wright, H.; Oldham, D.; Playford, D. Extending a Conceptual Framework for Junior Doctors’ Career Decision Making and Rural Careers: Explorers versus Planners and Finding the ‘Right Fit’. Int. J. Environ. Res. Public Health 2020, 17, 1352. [Google Scholar] [CrossRef] [Green Version]
- Cano, G.; Bain-Donohue, S.; Moore, M. Why do some medical graduates lose their intention to practise rurally? Rural Remote Health 2021, 21, 5747. [Google Scholar] [CrossRef]
- Ostini, R.; McGrail, M.R.; Kondalsamy-Chennakesavan, S.; Hill, P.; O’Sullivan, B.; Selvey, L.A.; Eley, D.S.; Adegbija, O.; Boyle, F.M.; Dettrick, Z.; et al. Building a sustainable rural physician workforce. Med. J. Aust. 2021, 215, S5–S33. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, H.K.; Diamond, J.J.; Karkham, F.W.; Santana, A.J. The relationship between entering medical students’ backgrounds and career plans and their rural practice outcomes three decades later. Acad. Med. 2012, 87, 493–497. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, B.; McGrail, M.; Gurney, T.; Martin, P. Barriers to getting into postgraduate specialty training for junior Australian doctors: An interview-based study. PLoS ONE 2021, 16, e0258584. [Google Scholar] [CrossRef]
- McGrail, M.R.; Russell, D.J.; O’Sullivan, B.G. Family effects on the rurality of GP’s work location: A longitudinal panel study. Hum. Resour. Health 2017, 15, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Variable | Group | Participants | All UQ Graduates |
|---|---|---|---|
| PGY | 1–3 | 172 (22%) | 939 (21%) |
| 4–6 | 193 (25%) | 896 (20%) | |
| 7–9 | 166 (21%) | 884 (19%) | |
| 10–13 | 145 (19%) | 976 (21%) | |
| 14–17 | 99 (13%) | 845 (19%) | |
| Gender | Male | 378 (49%) | 2542 (56%) |
| Female | 397 (51%) | 1998 (44%) | |
| RCS participants | Yes | 236 (30%) | 1191(26%) |
| No | 539 (70%) | 3349 (74%) | |
| Age at medical school graduation | 28+ | 223 (29%) | 1242 (27%) |
| Under 28 | 552 (71%) | 3298 (73%) | |
| Working rurally (MMM 2–7) | Yes | 176 (24%) | 899 (20%) |
| No | 573 (76%) | 3558 (80%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGrail, M.; O’Sullivan, B.; Gurney, T.; Eley, D.; Kondalsamy-Chennakesavan, S. Exploring Doctors’ Emerging Commitment to Rural and General Practice Roles over Their Early Career. Int. J. Environ. Res. Public Health 2021, 18, 11835. https://doi.org/10.3390/ijerph182211835
McGrail M, O’Sullivan B, Gurney T, Eley D, Kondalsamy-Chennakesavan S. Exploring Doctors’ Emerging Commitment to Rural and General Practice Roles over Their Early Career. International Journal of Environmental Research and Public Health. 2021; 18(22):11835. https://doi.org/10.3390/ijerph182211835
Chicago/Turabian StyleMcGrail, Matthew, Belinda O’Sullivan, Tiana Gurney, Diann Eley, and Srinivas Kondalsamy-Chennakesavan. 2021. "Exploring Doctors’ Emerging Commitment to Rural and General Practice Roles over Their Early Career" International Journal of Environmental Research and Public Health 18, no. 22: 11835. https://doi.org/10.3390/ijerph182211835
APA StyleMcGrail, M., O’Sullivan, B., Gurney, T., Eley, D., & Kondalsamy-Chennakesavan, S. (2021). Exploring Doctors’ Emerging Commitment to Rural and General Practice Roles over Their Early Career. International Journal of Environmental Research and Public Health, 18(22), 11835. https://doi.org/10.3390/ijerph182211835








