Technology-Assisted Collaborative Care Program for People with Diabetes and/or High Blood Pressure Attending Primary Health Care: A Feasibility Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedures
2.4. Intervention
2.4.1. Computer-Assisted Psychosocial Intervention
2.4.2. Telephone Monitoring
2.4.3. Mobile Phone Application
2.5. Measures and Covariates
2.6. Data Analysis
2.7. Ethics Approval
3. Results
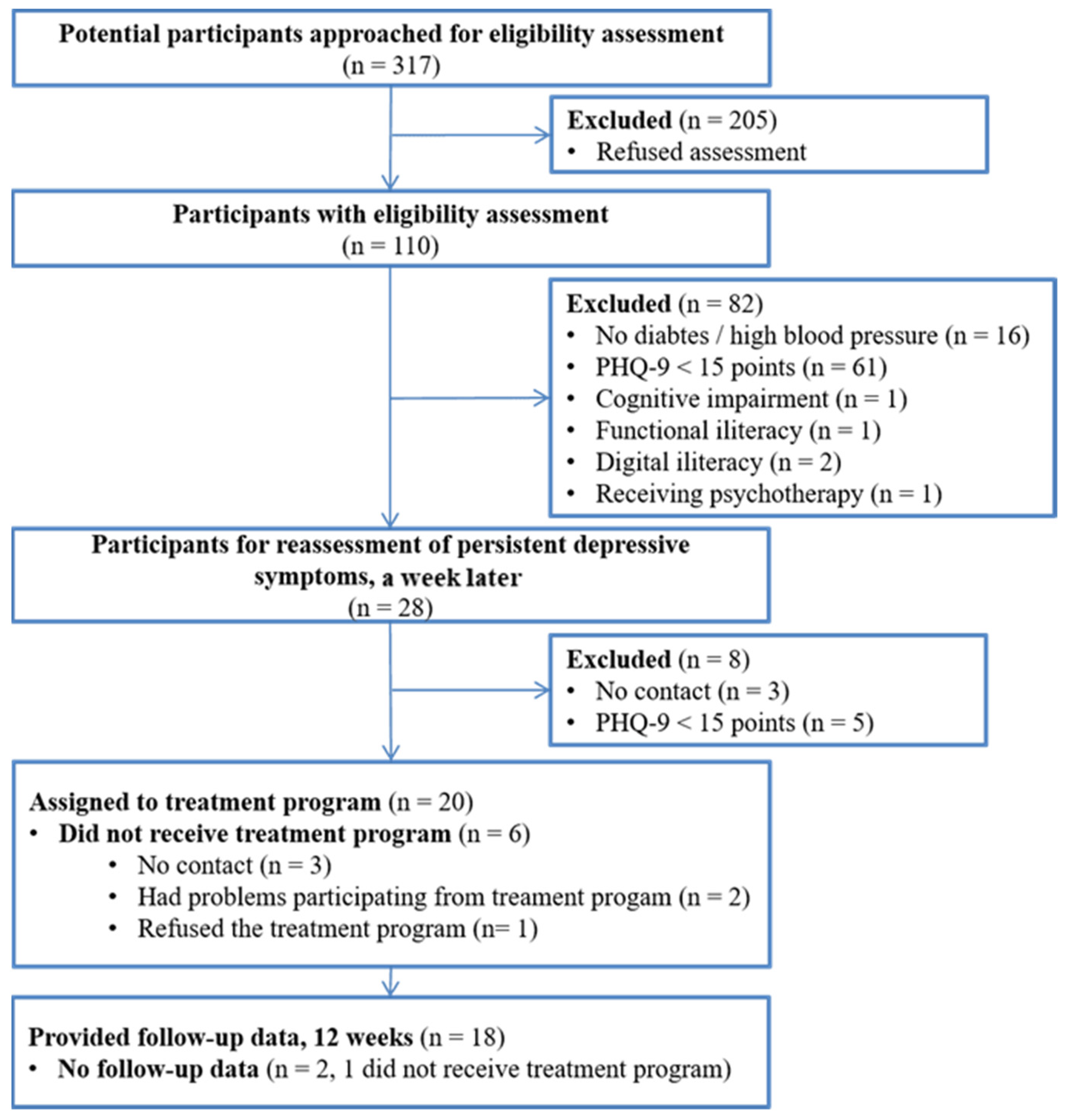
3.1. Recruitment
3.2. Characterization of the Sample
3.3. Use and Adherence to the Components of the Technology-Assisted Collaborative Care Program
3.4. Acceptability of the Computer-Assisted Psychosocial Intervention
3.5. Potential Efficacy of a Technology-Assisted Collaborative Care Program
3.5.1. Depression
3.5.2. Social Problem-Solving Skills
3.5.3. Health-Related Quality of Life
3.5.4. Use of Health-Care Services
3.5.5. Consumption and Adherence to Medications
3.6. Experiences of Patients with the Computer-Assisted Psychosocial Intervention
3.6.1. Satisfaction with the Intervention
3.6.2. Aspects Positively Valued
3.6.3. Aspects to Improve
3.6.4. Differences from the Usual Treatment
3.6.5. Extension
3.6.6. Graphic Aspects
3.6.7. Learning Achieved
4. Discussion
4.1. Principal Results
4.2. Comparison with Prior Work
4.3. Limitations
4.4. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1603–1658. [Google Scholar] [CrossRef] [Green Version]
- Prados-Torres, A.; Calderón-Larrañaga, A.; Hancco-Saavedra, J.; Poblador-Plou, B.; Akker, M.V.D. Multimorbidity patterns: A systematic review. J. Clin. Epidemiol. 2014, 67, 254–266. [Google Scholar] [CrossRef]
- Smith, D.J.; Court, H.; McLean, G.; Martin, D.; Martin, J.L.; Guthrie, B.; Gunn, J.; Mercer, S.W. Depression and multimorbidity: A cross-sectional study of 1,751,841 patients in primary care. J. Clin. Psychiatry 2014, 75, 1202–1208; quiz 8. [Google Scholar] [CrossRef]
- Deschênes, S.S.; Burns, R.; Schmitz, N. Associations between depression, chronic physical health conditions, and disability in a community sample: A focus on the persistence of depression. J. Affect. Disord. 2015, 179, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Moussavi, S.; Chatterji, S.; Verdes, E.; Tandon, A.; Patel, V.; Ustun, B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet 2007, 370, 851–858. [Google Scholar] [CrossRef]
- Grenard, J.L.; Munjas, B.A.; Adams, J.L.; Suttorp, M.; Maglione, M.; McGlynn, E.A.; Gellad, W.F. Depression and Medication Adherence in the Treatment of Chronic Diseases in the United States: A Meta-Analysis. J. Gen. Intern. Med. 2011, 26, 1175–1182. [Google Scholar] [CrossRef] [Green Version]
- Gathright, E.C.; Goldstein, C.M.; Josephson, R.A.; Hughes, J.W. Depression increases the risk of mortality in patients with heart failure: A meta-analysis. J. Psychosom. Res. 2017, 94, 82–89. [Google Scholar] [CrossRef] [Green Version]
- Jansen, L.; van Schijndel, M.; van Waarde, J.; van Busschbach, J. Health-economic outcomes in hospital patients with medi-cal-psychiatric comorbidity: A systematic review and meta-analysis. PLoS ONE. 2018, 13, e0194029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Dooren, F.E.; Nefs, G.; Schram, M.T.; Verhey, F.R.; Denollet, J.; Pouwer, F. Depression and risk of mortality in people with dia-betes mellitus: A systematic review and meta-analysis. PLoS ONE. 2013, 8, e57058. [Google Scholar]
- Huang, Y.; Wei, X.; Wu, T.; Chen, R.; Guo, A. Collaborative care for patients with depression and diabetes mellitus: A systematic review and meta-analysis. BMC Psychiatry 2013, 13, 260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panagioti, M.; Bower, P.; Kontopantelis, E.; Lovell, K.; Gilbody, S.; Waheed, W.; Dickens, C.; Archer, J.; Simon, G.; Ell, K. Association between Chronic Physical Con-ditions and the Effectiveness of Collaborative Care for Depression: An Individual Participant Data Meta-analysis. JAMA Psychiatry 2016, 73, 978–989. [Google Scholar] [CrossRef]
- Rossom, R.C.; Solberg, L.I.; Magnan, S.; Crain, A.L.; Beck, A.; Coleman, K.J.; Katzelnick, D.; Williams, M.D.; Neely, C.; Ohnsorg, K.; et al. Impact of a national collaborative care initiative for patients with depression and diabetes or cardiovascular disease. Gen. Hosp. Psychiatry 2017, 44, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Vanderlip, E.R.; Rundell, J.; Avery, M.; Alter, C.; Engel, C.; Fortney, J.; Lui, D.; Williams, M. Dissemination of Integrated Care within Adult Primary Care Settings: The Collaborative Care Model; Report Spring 2016; American Psychiatric Association (APA): Washington, DC, USA; Academy of Psychosomatic Medicine (APM): Bethesda, MD, USA, 2016. [Google Scholar]
- Overbeck, G.; Davidsen, A.S.; Kousgaard, M.B. Enablers and barriers to implementing collaborative care for anxiety and de-pression: A systematic qualitative review. Implement. Sci. 2016, 11, 165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitebird, R.R.; Solberg, L.I.; Jaeckels, N.A.; Pietruszewski, P.B.; Hadzic, S.; Unutzer, J.; Ohnsorg, K.A.; Rossom, R.C.; Beck, A.; Joslyn, K.; et al. Effective Implementation of collabora-tive care for depression: What is needed? Am. J. Manag. Care. 2014, 20, 699–707. [Google Scholar] [PubMed]
- Acharya, B.; Ekstrand, M.; Rimal, P.; Ali, M.; Swar, S.; Srinivasan, K.; Mohan, V.; Unützer, J.; Chwastiak, L.A. Collaborative Care for Mental Health in Low- and Middle-Income Countries: A WHO Health Systems Framework Assessment of Three Programs. Psychiatr. Serv. 2017, 68, 870–872. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kroenke, K.; Unutzer, J. Closing the False Divide: Sustainable Approaches to Integrating Mental Health Services into Primary Care. J. Gen. Intern. Med. 2017, 32, 404–410. [Google Scholar] [CrossRef] [Green Version]
- Jiang, Y.; Shorey, S.; Seah, B.; Chan, W.X.; Tam, W.W.S.; Wang, W. The effectiveness of psychological interventions on self-care, psychological and health outcomes in patients with chronic heart failure—A systematic review and meta-analysis. Int. J. Nurs. Stud. 2018, 78, 16–25. [Google Scholar] [CrossRef]
- Sudhir, P.M. Advances in psychological interventions for lifestyle disorders: Overview of interventions in cardiovascular disorder and type 2 diabetes mellitus. Curr. Opin. Psychiatry 2017, 30, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Bet, P.M.; Hugtenburg, J.G.; Penninx, B.W.; Balkom, A.; Nolen, W.A.; Hoogendijk, W.J. Treatment inadequacy in primary and spe-cialized care patients with depressive and/or anxiety disorders. Psychiatry Res. 2013, 210, 594–600. [Google Scholar] [CrossRef]
- Puyat, J.H.; Kazanjian, A.; Goldner, E.M.; Wong, H. How Often Do Individuals with Major Depression Receive Minimally Ade-quate Treatment? A Population-Based, Data Linkage Study. Can. J. Psychiatry 2016, 61, 394–404. [Google Scholar] [CrossRef]
- Wells, M.J.; Owen, J.J.; McCray, L.W.; Bishop, L.B.; Eells, T.D.; Brown, G.K.; Richards, D.; Thase, M.E.; Wright, J.H. Computer-Assisted Cognitive-Behavior Therapy for Depression in Primary Care. Prim. Care Companion CNS Disord. 2018, 20, 17r02196. [Google Scholar] [CrossRef] [PubMed]
- Alvarado, R.; Rojas, G.; Minoletti, A.; Alvarado, F.; Domínguez, C. Depression program in primary health care: The Chilean ex-perience. Int. J. Ment. Health 2012, 41, 38–47. [Google Scholar] [CrossRef]
- Araya, R.; Alvarado, R.; Minoletti, A. Chile: An ongoing mental health revolution. Lancet 2009, 374, 597–598. [Google Scholar] [CrossRef]
- Araya, R.; Rojas, G.; Fritsch, R.; Gaete, J.; Rojas, M.; Simon, G.; Peters, T. Treating depression in primary care in low-income women in Santiago, Chile: A randomised controlled trial. Lancet 2003, 361, 995–1000. [Google Scholar] [CrossRef]
- Minoletti, A.; Sepúlveda, R.; Horvitz-Lennon, M. Twenty years of mental health policies in Chile: Lessons and challenges. Int. J. Ment. Health 2012, 41, 21–37. [Google Scholar] [CrossRef] [Green Version]
- Ministerio de Salud de Chile. Estrategia Nacional de Salud Para el Cumplimiento de los Objetivos Sanitarios de la Década 2011–2020; Ministerio de Salud de Chile: Santiago, Chile, 2011. [Google Scholar]
- Dois, A.; Cazenave, A. Pesquisa de depresión mayor en hipertensos consultantes de la Atención Primaria. Revista Médica Chile 2009, 137, 475–480. [Google Scholar] [CrossRef] [Green Version]
- Martinez, P.; Rojas, G.; Fritsch, R.; Martinez, V.; Vohringer, P.A.; Castro, A. Comorbidity in people with depression seeking help at primary health care centers in Santiago, Chile. Rev. Med. Chile 2017, 145, 25–32. [Google Scholar]
- Menezes, P.; Quayle, J.; Garcia Claro, H.; da Silva, S.; Brandt, L.R.; Diez-Canseco, F.; Jaime Miranda, J.; Price, L.N.; Mohr, D.C.; Araya, R. Use of a Mobile Phone App to Treat De-pression Comorbid with Hypertension or Diabetes: A Pilot Study in Brazil and Peru. JMIR Ment. Health 2019, 6, e11698. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Baader, M.T.; Molina, F.J.L.; Venezian, B.S.; Rojas, C.C.; Farías, S.R.; Fierro-Freixenet, C.; Backenstrass, M.; Mundt, C. Validación y utilidad de la encuesta PHQ-9 (Patient Health Questionnaire) en el diagnóstico de depresión en pacientes usuarios de atención primaria en Chile. Rev. Chil. Neuro-Psiquiatr. 2012, 50, 10–22. [Google Scholar] [CrossRef]
- Maydeuolivares, A.; Fornells, A.R.; Gómez-Benito, J.; Dzurilla, T. Psychometric properties of the Spanish adaptation of the Social Problem-Solving Inventory-Revised (SPSI-R). Pers. Individ. Differ. 2000, 29, 699–708. [Google Scholar] [CrossRef] [Green Version]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [Green Version]
- Sekhon, M.; Cartwright, M.; Francis, J.J. Acceptability of health-care interventions: An overview of reviews and development of a theoretical framework. BMC Health Serv. Res. 2017, 17, 88. [Google Scholar] [CrossRef] [Green Version]
- StataCorp. Stata Statistical Software (Release 14); StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- Glaser, B.G.; Strauss, A.L. Discovery of Grounded Theory: Strategies for Qualitative Research; Routledge: Abingdon, UK, 2017. [Google Scholar]
- Löwe, B.; Kroenke, K.; Gräfe, K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J. Psychosom. Res. 2005, 58, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Dickens, C.; Cherrington, A.; Adeyemi, I.; Roughley, K.; Bower, P.; Garrett, C.; Bundy, C.; Coventry, P. Characteristics of psychological interventions that improve depression in people with coronary heart disease: A systematic review and meta-regression. Psychosom. Med. 2013, 75, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Petrak, F.; Baumeister, H.; Skinner, T.; Brown, A.; Holt, R. Depression and diabetes: Treatment and health-care delivery. Lancet Diabetes Endocrinol. 2015, 3, 472–485. [Google Scholar] [CrossRef]
- Rollman, B.L.; Herbeck, B.B.; Abebe, K.Z.; Spring, M.B.; Rotondi, A.J.; Rothenberger, S.D.; Karp, J.F. Effectiveness of Online Collabo-rative Care for Treating Mood and Anxiety Disorders in Primary Care: A Randomized Clinical Trial. JAMA Psychiatry 2018, 75, 56–64. [Google Scholar] [CrossRef]
- Bao, Y.; Druss, B.G.; Jung, H.-Y.; Chan, Y.-F.; Unützer, J. Unpacking Collaborative Care for Depression: Examining Two Essential Tasks for Implementation. Psychiatr. Serv. 2016, 67, 418–424. [Google Scholar] [CrossRef] [Green Version]
- Sharpe, M.; Walker, J.; Hansen, C.H.; Martin, P.; Symeonides, S.; Gourley, C.; Wall, L.; Weller, D.; Murray, G. Integrated collaborative care for comorbid major depression in patients with cancer (SMaRT Oncology-2): A multicentre randomised controlled effectiveness trial. Lancet 2014, 384, 1099–1108. [Google Scholar] [CrossRef]
- Strong, V.; Waters, R.; Hibberd, C.; Murray, G.; Wall, L.; Walker, J.; McHugh, G.; Walker, A.; Sharpe, M. Management of depression for people with cancer (SMaRT oncology 1): A randomised trial. Lancet 2008, 372, 40–48. [Google Scholar] [CrossRef] [Green Version]
- Walker, J.; Hansen, C.H.; Martin, P.; Symeonides, S.; Gourley, C.; Wall, L.; Weller, D.; Murray, G.; Sharpe, M. Integrated collaborative care for major depression comorbid with a poor prognosis cancer (SMaRT Oncology-3): A multicentre randomised controlled trial in patients with lung cancer. Lancet Oncol. 2014, 15, 1168–1176. [Google Scholar] [CrossRef]
- Brandt, L.R.; Hidalgo, L.; Diez-Canseco, F.; Araya, R.; Mohr, D.C.; Menezes, P.R.; Miranda, J.J. Addressing Depression Comorbid with Dia-betes or Hypertension in Resource-Poor Settings: A Qualitative Study about User Perception of a Nurse-Supported Smartphone App in Peru. JMIR Ment. Health 2019, 6, e11701. [Google Scholar] [CrossRef] [PubMed]
- Barnighausen, T.; Oldenburg, C.; Tugwell, P.; Bommer, C.; Ebert, C.; Barreto, M.; Djimeu, E.; Haber, N.; Waddington, H.; Rockers, P. Quasi-experimental study designs se-ries-paper 7: Assessing the assumptions. J. Clin. Epidemiol. 2017, 89, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C. How we design feasibility studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef] [Green Version]

| Session | Name | General Objective |
|---|---|---|
| 1 | What happens with my health? | Patients are introduced to the program and receive brief psychoeducation on depression. |
| 2 | What are diabetes and high blood pressure all about? | Patients received education on diabetes and/or high blood pressure care and their relationship with depression. |
| 3 | How to solve my problems? | Patients are introduced to problem-solving techniques. |
| 4 | Learning to solve my problems | Patients are motivated to use problem-solving techniques in their daily life. |
| 5 | What did I learn in this therapy? | Evaluate contents learned and reinforce those that are less incorporated. |
| Variable | n (%) |
|---|---|
| Previous diagnosis of depression | 13 (65.0) |
| History of treatments for depression1 | 13 (100.0) |
| Family history of mental health2 | |
| Depression | 12 (63.2) |
| Alcohol/drugs | 6 (33.3) |
| Anxiety | 5 (26.3) |
| Others (psychosis, bipolarity, suicide) | 7 (35.0) |
| Cigarrette consumption | 9 (45.0) |
| Medical comorbidities3 | |
| Arthrithis/osteoarthritis | 9 (47.4) |
| Heart disease | 3 (16.7) |
| Asthma/Emphysema, lung | 3 (15.8) |
| Thyroid problems | 7 (38.9) |
| Other medical comorbidities | 11 (55.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez, P.; Guajardo, V.; Gómez, V.E.; Brandt, S.; Szabo, W.; Soto-Brandt, G.; Farhang, M.; Baeza, P.; Campos, S.; Herrera, P.; et al. Technology-Assisted Collaborative Care Program for People with Diabetes and/or High Blood Pressure Attending Primary Health Care: A Feasibility Study. Int. J. Environ. Res. Public Health 2021, 18, 12000. https://doi.org/10.3390/ijerph182212000
Martínez P, Guajardo V, Gómez VE, Brandt S, Szabo W, Soto-Brandt G, Farhang M, Baeza P, Campos S, Herrera P, et al. Technology-Assisted Collaborative Care Program for People with Diabetes and/or High Blood Pressure Attending Primary Health Care: A Feasibility Study. International Journal of Environmental Research and Public Health. 2021; 18(22):12000. https://doi.org/10.3390/ijerph182212000
Chicago/Turabian StyleMartínez, Pablo, Viviana Guajardo, Víctor E. Gómez, Sebastián Brandt, Wilsa Szabo, Gonzalo Soto-Brandt, Maryam Farhang, Paulina Baeza, Solange Campos, Pablo Herrera, and et al. 2021. "Technology-Assisted Collaborative Care Program for People with Diabetes and/or High Blood Pressure Attending Primary Health Care: A Feasibility Study" International Journal of Environmental Research and Public Health 18, no. 22: 12000. https://doi.org/10.3390/ijerph182212000
APA StyleMartínez, P., Guajardo, V., Gómez, V. E., Brandt, S., Szabo, W., Soto-Brandt, G., Farhang, M., Baeza, P., Campos, S., Herrera, P., & Rojas, G. (2021). Technology-Assisted Collaborative Care Program for People with Diabetes and/or High Blood Pressure Attending Primary Health Care: A Feasibility Study. International Journal of Environmental Research and Public Health, 18(22), 12000. https://doi.org/10.3390/ijerph182212000






