Exposure Worry: The Psychological Impact of Perceived Ionizing Radiation Exposure in British Nuclear Test Veterans
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Data Collection
2.3. Analysis
3. Results
3.1. Worry, Responsibility, and Guilt
3.1.1. Worry
“I’m 81 and the other ones didn’t even saw that age, you know? We’re getting back to the beginning. It’s when you read about the one that kidneys or something, the kidneys were welded together when it was born and things like that, and the deformity in kids and things like that. I wouldn’t like the think that was my grandchildren, and I wouldn’t like to think- That’s what worries me. The carrying it on.” (Veteran M).
3.1.2. Responsibility and Guilt
“I do wonder about certain things in life. Um I mean my daughter had breast cancer, then she’s got tumours on the brain and then she died. Whether that was anything to do with it because I’ve read so many times that it’s not always the people who witnessed the test, it be the generation after that are affected. Also had a granddaughter with Katz disease, um that was a rare disease of the nervous system so you worry about these things whether it’s a contributing factor or not, but there’s nothing you can do about it obviously but you just can’t help wondering about it.” (Veteran Q).
“Deep down I’m very angry. Anger and guilt rather than frustration. Guilt. Because I know you say it isn’t my fault and yes I understand it isn’t my fault but I can’t convince myself it isn’t my fault. Can you understand that? It sounds totally illogical, but I can’t.” (Veteran F).
“No I mean, when my wife died we would’ve had another two years we’d have had our diamond wedding and it just goes through my mind “only if I hadn’t gone to Montebello would we have seen our 60 years?” (Veteran K).
3.2. Us vs. Them
“It brings back things like ‘us and them’. You hear about it and you see about it so, so commonly, um really on something like that which can have such disastrous effect on people you’d have thought everybody would be treated as a standard, by the same. But I didn’t know that at the time. It’s only something I’ve read in the last couple of years with these various articles I get but um you get bits of information keep coming out but it’s just uh bearing in mind what we had to go through or what could’ve happened that we’d all be treated the same.” (Veteran Q).
3.2.1. Power Dynamic
“My view of a nuclear test veteran is that we’re all members of the mushroom club, kept in the dark, shovelled shit from time to time. And that plaque up there tells you what else we are. Guinea pigs. Guinea pigs. That’s what we are. That’s my view of what nuclear test veterans are. A bunch of people who haven’t a clue what they are doing who were sent out there as guinea pigs to work on tests. They would never have sent us to the forward area where there’s nothing to pick up, to pick up bits, if that hadn’t been part of being guinea pigs and being part of the mushroom club.” (Veteran F).
“And if you say how do I identify with them, I identify as one of the 160 victims. Because we weren’t given a choice.” (Veteran A).
3.2.2. Recognition
“All I want. All I want-I’m not too worried about a medal. I mean it would be nice to have a medal because we’ve served our country probably as much as some of the people in the minor infringements that went on. But having said that, all I want is the British government to say, “yes we accept that” and the families around, perhaps give them a widow’s pension so that they look after the families that are suffering because of it. If we can prove that.” (Veteran F).
“No one has had the decency to say “yes, we did fail in that respect.” No one said that. And that really is the cause that I feel is really, really bad for a modern nation like this and our government still looked back on the old paperwork and says oh yeah, yeah, yeah. But they’re reading lies. They’re reading lies that the scientists have told them. Scientists know what’s going off. They’re the ones that pulled all the strings in Australia. Everything that happened in Australia, don’t know about Christmas Island, I wasn’t involved with that. But Maralinga was solely controlled by those people. And the Australian government was controlled to them. If they could lie to them then they certainly could lie to us. To this day no one has owned up.” (Veteran I)
3.3. Change across the Life Course
3.3.1. The Tests
“Like I said, one of the chaps must’ve said “oh yeah, yeah they do H bomb testing” which didn’t mean a lot really to an 18-year-old. It was just that we were going to a lovely, little island in the south pacific. Nice weather, and all that, you know.” (Veteran N).
“Well, how can I put it, I mean don’t forget I said to you earlier, we knew nothing about it. It’s when it all comes to the truth and ii told you I get little booklets and they put stories from the scientists who admitted- And all that carried on. That’s what angers you. When they tell you and you think “you’re a bloody guinea pig”. That’s what gets to you. But there’s nothing you can do about that now. You’ve just got to bite your tongue and that.” (Veteran M).
3.3.2. After the Tests
“Well we were very ignorant about it. Didn’t join the nuclear test veterans ‘til about 15 years after did I. so I hadn’t picked up on any things that were appearing in the BNTVA journal till about 15 years after. Then when I got it “well I haven’t got that, haven’t got that, haven’t got that. I’m alright, Jack”.” (Veteran C).
“At the time you think “nah it’s a pretty good posting, we have a great time, have a few drinks in the evening, really easy going. But when you actually get back and things start to occur that hindsight says 20/20 vision. It’s a wonderful thing, and when you get a bit of hindsight things start do come to affect you I think emotionally but I’m quite angry in a way. I’ve got more anger than anything else. Anger and guilt. Anger and guilty, those are the two things. I mean I’m ok mostly I think emotionally but I do get upset sometimes.” (Veteran F).
4. Discussion
4.1. Limitations
4.2. Future Work
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Darby, S.C.; Kendall, G.M.; Fell, T.P.; O’Hagan, J.A.; Muirhead, C.R.; Ennis, J.R.; Ball, A.M.; A Dennis, J.; Doll, R. A summary of mortality and incidence of cancer in men from the United Kingdom who participated in the United Kingdom’s atmospheric nuclear weapon tests and experimental programmes. BMJ 1988, 296, 332–338. [Google Scholar] [CrossRef] [Green Version]
- Kendall, G.M.; Muirhead, C.; Darby, S.C.; Doll, R.; Arnold, L.; Hagan, J.A.O. Epidemiological studies of UK test veterans: I. General description. J. Radiol. Prot. 2004, 24, 199–217. [Google Scholar] [CrossRef]
- Darby, S.C.; Kendall, G.M.; Fell, T.P.; Doll, R.; Goodill, A.A.; Conquest, A.J.; Jackson, D.A.; Haylock, R.G. Further follow up of mortality and incidence of cancer in men from the United Kingdom who participated in the United Kingdom’s atmospheric nuclear weapon tests and experimental programmes. BMJ 1993, 307, 1530–1535. [Google Scholar] [CrossRef] [Green Version]
- Muirhead, C.R.; Bingham, D.; Haylock, R.G.E.; O’Hagan, J.A.; Goodill, A.A.; Berridge, G.L.C.; English, M.A.; Hunter, N.; Kendall, G.M. Follow up of mortality and incidence of cancer 1952-98 in men from the UK who participated in the UK’s atmospheric nuclear weapon tests and experimental programmes. Occup. Environ. Med. 2003, 60, 165–172. [Google Scholar] [CrossRef] [Green Version]
- Muirhead, C.; Kendall, G.M.; Darby, S.C.; Doll, R.; Haylock, R.G.E.; Hagan, J.A.O.; Berridge, G.L.C.; A Phillipson, M.; Hunter, N. Epidemiological studies of UK test veterans: II. Mortality and cancer incidence. J. Radiol. Prot. 2004, 24, 219–241. [Google Scholar] [CrossRef]
- Danzer, A.; Danzer, N. The long-run consequences of Chernobyl: Evidence on subjective well-being, mental health and welfare. J. Public Econ. 2016, 135, 47–60. [Google Scholar] [CrossRef]
- Vyner, H. Invisible Trauma: The Psychosocial Effects of Invisible Environmental Contaminants; Lexington Books: Lexington, MA, USA, 1988. [Google Scholar]
- Abbott, P.; Wallace, C.; Beck, M. Chernobyl: Living with risk and uncertainty. Health Risk Soc. 2006, 8, 105–121. [Google Scholar] [CrossRef]
- Borkovec, T.D.; Ray, W.J.; Stoeber, J. Worry: A Cognitive Phenomenon Intimately Linked to Affective, Physiological, and Interpersonal Behavioral Processes. Cogn. Ther. Res. 1998, 22, 561–576. [Google Scholar] [CrossRef]
- Murphy, B.C.; Ellis, P.; Greenberg, S. Atomic veterans and their families: Responses to radiation exposure. Am. J. Orthopsychiatry 1990, 60, 418–427. [Google Scholar] [CrossRef]
- Brosschot, J.F.; Gerin, W.; Thayer, J.F. The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. J. Psychosom. Res. 2006, 60, 113–124. [Google Scholar] [CrossRef]
- Tallis, F.; Eysenck, M.W. Worry: Mechanisms and Modulating Influences. Behav. Cogn. Psychother. 1994, 22, 37–56. [Google Scholar] [CrossRef]
- Lifton, R.J. Psychological effects of the atomic bomb in Hiroshima: The theme of death. Daedalus 1963, 92, 462–497. [Google Scholar]
- Sawada, A.; Chaitin, J.; Bar-On, D. Surviving Hiroshima and Nagasaki—Experiences and Psychosocial Meanings. Psychiatry 2004, 67, 43–60. [Google Scholar] [CrossRef]
- Kamite, Y.; Igawa, H.; Kabir, R.S. A review of the long-term psychological effects of radiation exposure in the cases of the atomic bombings of Hiroshima and Nagasaki and the Chernobyl nuclear accident. Hiroshima Psychol. Res. 2017, 16, 49–68. [Google Scholar] [CrossRef]
- Schaeffer, M.A.; Baum, A. Adrenal Cortical Response to Stress at Three Mile Island. Psychosom. Med. 1984, 46, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Gatchel, R.J.; Schaeffer, M.A.; Baum, A. A Psychophysiological Field Study of Stress at Three Mile Island. Psychophysiology 1985, 22, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Davison, L.M.; Weiss, L.; O’Keeffe, M.; Baum, A. Acute stressors and chronic stress at Three Mile Island. J. Trauma. Stress 1991, 4, 481–493. [Google Scholar] [CrossRef]
- Ginzburg, H.M. The psychological consequences of the Chernobyl accident--findings from the International Atomic Energy Agency Study. Public Health Rep. 1993, 108, 184–192. [Google Scholar]
- Pastel, R.H. Radiophobia: Long-Term Psychological Consequences of Chernobyl. Mil. Med. 2002, 167, 134–136. [Google Scholar] [CrossRef] [Green Version]
- Bennett, B.; Repacholi, M.; Carr, Z. Health Effects of the Chernobyl Accident and Special Health Care Programmes; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Kamiya, K.; Ozasa, K.; Akiba, S.; Niwa, O.; Kodama, K.; Takamura, N.; Zaharieva, E.K.; Kimura, Y.; Wakeford, R. Long-term effects of radiation exposure on health. Lancet 2015, 386, 469–478. [Google Scholar] [CrossRef]
- Kunii, Y.; Suzuki, Y.; Shiga, T.; Yabe, H.; Yasumura, S.; Maeda, M.; Niwa, S.-I.; Otsuru, A.; Mashiko, H.; Abe, M.; et al. Severe Psychological Distress of Evacuees in Evacuation Zone Caused by the Fukushima Daiichi Nuclear Power Plant Accident: The Fukushima Health Management Survey. PLoS ONE 2016, 11, e0158821. [Google Scholar] [CrossRef]
- Thomas, G.; Symonds, P. Radiation Exposure and Health Effects—Is it Time to Reassess the Real Consequences? Clin. Oncol. 2016, 28, 231–236. [Google Scholar] [CrossRef] [Green Version]
- Maeda, M.; Oe, M. Mental Health Consequences and Social Issues After the Fukushima Disaster. Asia Pac. J. Public Health 2017, 29, 36S–46S. [Google Scholar] [CrossRef] [PubMed]
- Harada, N.; Shigemura, J.; Tanichi, M.; Kawaida, K.; Takahashi, S.; Yasukata, F. Mental health and psychological impacts from the 2011 Great East Japan Earthquake Disaster: A systematic literature review. Disaster Mil. Med. 2015, 1, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukasawa, M.; Kawakami, N.; Umeda, M.; Miyamoto, K.; Akiyama, T.; Horikoshi, N.; Yasumura, S.; Yabe, H.; Bromet, E.J. Environmental radiation level, radiation anxiety, and psychological distress of non-evacuee residents in Fukushima five years after the Great East Japan Earthquake: Multilevel analyses. SSM Popul. Health 2017, 3, 740–748. [Google Scholar] [CrossRef]
- Collins, D.L.; Bs, A.B.D.C. Chronic Stress from the Goiania137Cs Radiation Accident. Behav. Med. 1993, 18, 149–157. [Google Scholar] [CrossRef]
- Loganovsky, K.; Havenaar, J.M.; Tintle, N.L.; Guey, L.T.; Kotov, R.; Bromet, E.J. The mental health of clean-up workers 18 years after the Chernobyl accident. Psychol. Med. 2008, 38, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Foster, R.P. The long-term mental health effects of nuclear trauma in recent Russian immigrants in the United States. Am. J. Orthopsychiatry 2002, 72, 492–504. [Google Scholar] [CrossRef]
- Havenaar, J.M.; Rumyantzeva, G.M.; Brink, W.V.D.; Poelijoe, N.W.; Bout, J.V.D.; Van Engeland, H.; Koeter, M.W. Long-Term Mental Health Effects of the Chernobyl Disaster: An Epidemiologic Survey in Two Former Soviet Regions. Am. J. Psychiatry 1997, 154, 1605–1607. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; Tsutsumi, A.; Izutsu, T.; Kawamura, N.; Miyazaki, T.; Kikkawa, T. Persistent distress after psychological exposure to the Nagasaki atomic bomb explosion. Br. J. Psychiatry 2011, 199, 411–416. [Google Scholar] [CrossRef] [Green Version]
- Semenova, Y.; Pivina, L.; Manatova, A.; Bjørklund, G.; Glushkova, N.; Belikhina, T.; Dauletyarova, M.; Zhunussova, T. Mental distress in the rural Kazakhstani population exposed and non-exposed to radiation from the Semipalatinsk Nuclear Test Site. J. Environ. Radioact. 2019, 203, 39–47. [Google Scholar] [CrossRef]
- Vyner, H.M. The psychological effects of ionizing radiation. Cult. Med. Psychiatry 1983, 7, 241–261. [Google Scholar] [CrossRef]
- Miles, R.; Green, S.; Mynors, G.; Suppiah, J. British Nuclear Test Veterans Health Needs Audit; Ministry of Defence: London, UK, 2011.
- Alexis-Martin, B.; Waight, E.; Blell, M. Nuclear Families: A Social Study of British Nuclear Test Veteran Community Families; University of Southampton: Southampton, UK, 2019. [Google Scholar]
- Dockerty, J.; Jolly, J.; Kumar, A.; Larsen, T.; McBride, D.; McGill, S.; Turner, R.; Wall, S.; Williams, S.; Yi, A.; et al. The New Zealand nuclear veteran and families study, exploring the options to assess heritable health outcomes. N. Z. Med. J. 2020, 133, 70–78. [Google Scholar] [PubMed]
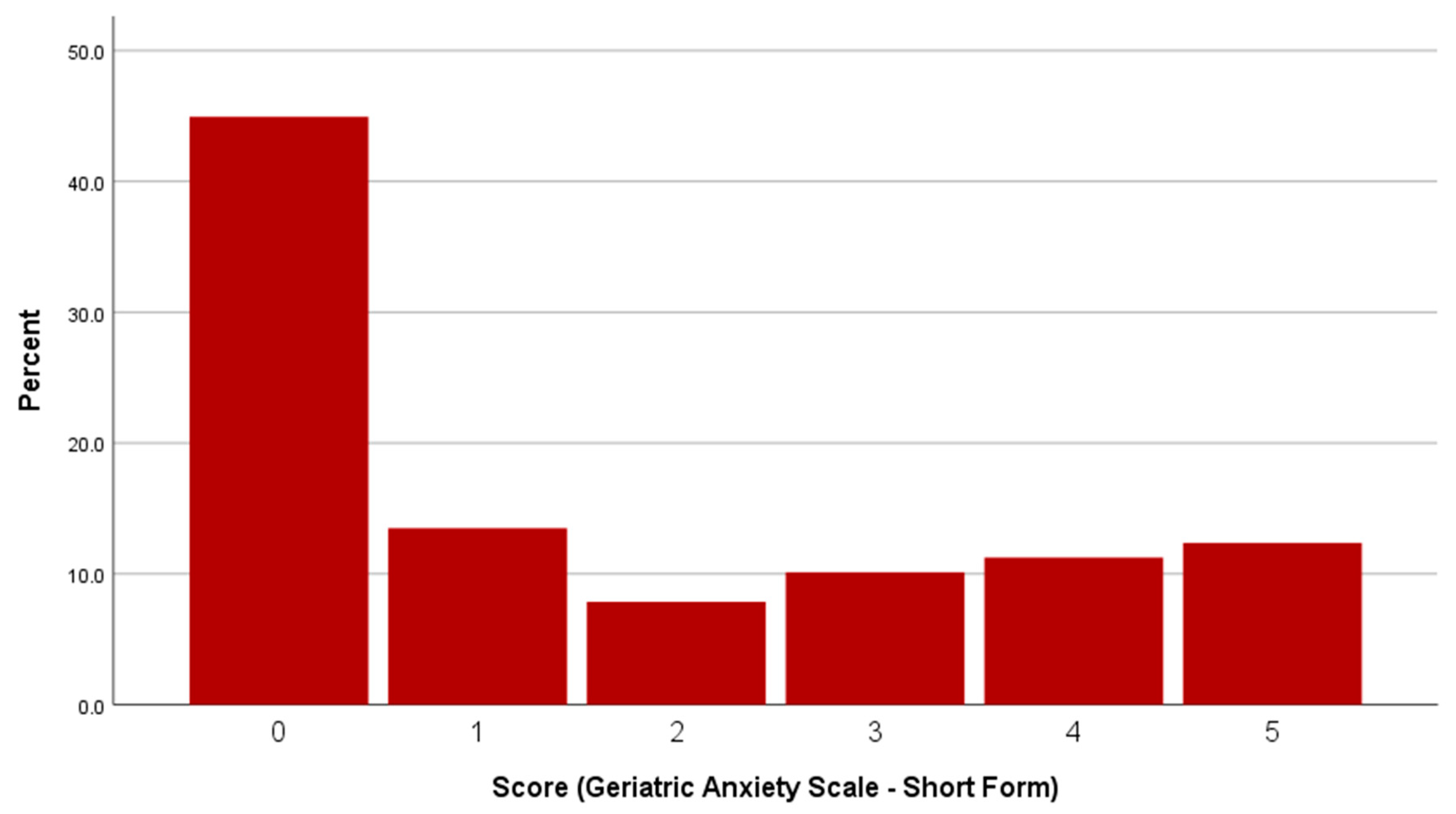
- Byrne, G.J.; Pachana, N.A. Development and validation of a short form of the Geriatric Anxiety Inventory—the GAI-SF. Int. Psychogeriatr. 2010, 23, 125–131. [Google Scholar] [CrossRef]
- Johnco, C.; Knight, A.; Tadic, D.; Wuthrich, V.M. Psychometric properties of the Geriatric Anxiety Inventory (GAI) and its short-form (GAI-SF) in a clinical and non-clinical sample of older adults. Int. Psychogeriatr. 2015, 27, 1089–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silver, J. Visual methods. In Introducing Qualitative Research in Psychology; Willig, C., Ed.; McGraw-Hill Education: New York City, NY, USA, 2013. [Google Scholar]
- Barton, K.C. Elicitation Techniques: Getting People to Talk About Ideas They Don’t Usually Talk About. Theory Res. Soc. Educ. 2015, 43, 179–205. [Google Scholar] [CrossRef]
- Harper, D. Talking about pictures: A case for photo elicitation. Vis. Stud. 2002, 17, 13–26. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Q. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Forlani, M.; Morri, M.; Murri, M.B.; Bernabei, V.; Moretti, F.; Attili, T.; Biondini, A.; De Ronchi, D.; Atti, A.R. Anxiety Symptoms in 74+ Community-Dwelling Elderly: Associations with Physical Morbidity, Depression and Alcohol Consumption. PLoS ONE 2014, 9, e89859. [Google Scholar] [CrossRef]
- Heissler, R.; Kopecek, M.; Pachana, N.A.; Frankova, V.; Georgi, H.S. Geriatric Anxiety Inventory (GAI) and its short form GAI-SF: Czech normative study. Cesk. Psychol. 2018, 62, 462–476. [Google Scholar]
- Kashimura, M.; Ishizu, K.; Fukumori, T.; Ishiwata, A.; Tateno, A.; Nomura, T.; Pachana, N.A. Psychometric properties of the Japanese version of the Geriatric Anxiety Inventory for community-dwelling older adults. Psychogeriatrics 2021, 21, 378–386. [Google Scholar] [CrossRef]
- Champagne, A.; Landreville, P.; Gosselin, P.; Carmichael, P.-H. Psychometric properties of the French Canadian version of the Geriatric Anxiety Inventory. Aging Ment. Health 2018, 22, 40–45. [Google Scholar] [CrossRef]
- Rhead, R.; MacManus, D.; Jones, M.; Greenberg, N.; Fear, N.T.; Goodwin, L. Mental health disorders and alcohol misuse among UK military veterans and the general population: A comparison study. Psychol. Med. 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Oster, C.; Morello, A.; Venning, A.; Redpath, P.; Lawn, S. The health and wellbeing needs of veterans: A rapid review. BMC Psychiatry 2017, 17, 414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milanak, M.E.; Gros, D.F.; Magruder, K.M.; Brawman-Mintzer, O.; Frueh, B.C. Prevalence and features of generalized anxiety disorder in Department of Veteran Affairs primary care settings. Psychiatry Res. 2013, 209, 173–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williamson, V.; Stevelink, S.A.; Greenberg, K.; Greenberg, N. Prevalence of Mental Health Disorders in Elderly U.S. Military Veterans: A Meta-Analysis and Systematic Review. Am. J. Geriatr. Psychiatry 2018, 26, 534–545. [Google Scholar] [CrossRef] [Green Version]
- DiNapoli, E.A.; Cully, J.A.; Wayde, E.; Sansgiry, S.; Yu, H.J.; Kunik, M.E. Age as a predictive factor of mental health service use among adults with depression and/or anxiety disorder receiving care through the Veterans Health Administration. Int. J. Geriatr. Psychiatry 2016, 31, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Basevitz, P.; Pushkar, D.; Chaikelson, J.; Conway, M.; Dalton, C. Age-Related Differences in Worry and Related Processes. Int. J. Aging Hum. Dev. 2008, 66, 283–305. [Google Scholar] [CrossRef]
- Gonçalves, D.C.; Byrne, G.J. Who worries most? Worry prevalence and patterns across the lifespan. Int. J. Geriatr. Psychiatry 2013, 28, 41–49. [Google Scholar] [CrossRef]
- Gould, C.E.; Edelstein, B.A. Worry, emotion control, and anxiety control in older and young adults. J. Anxiety Disord. 2010, 24, 759–766. [Google Scholar] [CrossRef]
- Suzuki, Y.; Yabe, H.; Yasumura, S.; Ohira, T.; Niwa, S.-I.; Ohtsuru, A.; Mashiko, H.; Maeda, M.; Abe, M. Psychological distress and the perception of radiation risks: The Fukushima health management survey. Bull. World Health Organ. 2015, 93, 598–605. [Google Scholar] [CrossRef]
- Watkins, E.; Moulds, M.; Mackintosh, B. Comparisons between rumination and worry in a non-clinical population. Behav. Res. Ther. 2005, 43, 1577–1585. [Google Scholar] [CrossRef]
- Beehler, G.; Baker, J.; Falkner, K.; Chegerova, T.; Pryshchepava, A.; Chegerov, V.; Zevon, M.; Bromet, E.; Havenaar, J.; Valdismarsdottir, H.; et al. A multilevel analysis of long-term psychological distress among Belarusians affected by the Chernobyl disaster. Public Health 2008, 122, 1239–1249. [Google Scholar] [CrossRef]
- Garcia, B. Social-psychological dilemmas and coping of atomic veterans. Am. J. Orthopsychiatry 1994, 64, 651–655. [Google Scholar] [CrossRef] [PubMed]
- Böhm, G.; Pfister, H.-R. Action tendencies and characteristics of environmental risks. Acta Psychol. 2000, 104, 317–337. [Google Scholar] [CrossRef]
- Böhm, G.; Pfister, H.-R. The perceiver’s social role and a risk’s causal structure as determinants of environmental risk evaluation. J. Risk Res. 2015, 20, 732–759. [Google Scholar] [CrossRef] [Green Version]
- Hallowell, N.; Arden-Jones, A.; Eeles, R.; Foster, C.; Lucassen, A.; Moynihan, C.; Watson, M. Guilt, blame and responsibility: Men’s understanding of their role in the transmission of BRCA1/2 mutations within their family. Sociol. Health Illn. 2006, 28, 969–988. [Google Scholar] [CrossRef]
- Strømsvik, N.; Råheim, M.; Gjengedal, E. Cancer worry among Norwegian male BRCA1/2 mutation carriers. Fam. Cancer 2011, 10, 597–603. [Google Scholar] [CrossRef] [Green Version]
- D’Agincourt-Canning, L. A gift or a yoke? Women’s and men’s responses to genetic risk information from BRCA1 and BRCA2 testing. Clin. Genet. 2006, 70, 462–472. [Google Scholar] [CrossRef] [PubMed]
- McAllister, L.A.; Callaghan, J.E.M.; Fellin, L. Masculinities and emotional expression in UK servicemen: ‘Big boys don’t cry’? J. Gend. Stud. 2018, 28, 257–270. [Google Scholar] [CrossRef] [Green Version]
- Jakupcak, M.; Blais, R.K.; Grossbard, J.; Garcia, H.; Okiishi, J. “Toughness” in association with mental health symptoms among Iraq and Afghanistan war veterans seeking Veterans Affairs health care. Psychol. Men Masc. 2014, 15, 100–104. [Google Scholar] [CrossRef] [Green Version]
- Masculinities, 2nd ed.; Polity: Cambridge, UK, 2005.
- Plys, E.; Smith, R.; Jacobs, M.L. Masculinity and Military Culture in VA Hospice and Palliative Care: A Narrative Review with Clinical Recommendations. J. Palliat. Care 2019, 35, 120–126. [Google Scholar] [CrossRef]
- Thoits, P.A. Mechanisms Linking Social Ties and Support to Physical and Mental Health. J. Health Soc. Behav. 2011, 52, 145–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamite, Y.; Kitani, T.; Ikeda, T.; Abe, K.; Kabir, R.S.; Morishima, Y. Survey and comparison of psychological factors between descendants and non-descendants of survivors of the atomic bomb: Generational differences in mental health indicators. J. Psychiatr. Res. 2021, 136, 398–401. [Google Scholar] [CrossRef] [PubMed]
- Kamite, Y. Prejudice and Health Anxiety about Radiation Exposure from Second-Generation Atomic Bomb Survivors: Results from a Qualitative Interview Study. Front. Psychol. 2017, 8, 1462. [Google Scholar] [CrossRef] [Green Version]
- Rasmussen, J.; Ewald, J.; Sterner, T. Gender and life-stage dependent reactions to the risk of radioactive contamination: A survey experiment in Sweden. PLoS ONE 2020, 15, e0232259. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collett, G.; Young, W.R.; Martin, W.; Anderson, R.M. Exposure Worry: The Psychological Impact of Perceived Ionizing Radiation Exposure in British Nuclear Test Veterans. Int. J. Environ. Res. Public Health 2021, 18, 12188. https://doi.org/10.3390/ijerph182212188
Collett G, Young WR, Martin W, Anderson RM. Exposure Worry: The Psychological Impact of Perceived Ionizing Radiation Exposure in British Nuclear Test Veterans. International Journal of Environmental Research and Public Health. 2021; 18(22):12188. https://doi.org/10.3390/ijerph182212188
Chicago/Turabian StyleCollett, George, William R. Young, Wendy Martin, and Rhona M. Anderson. 2021. "Exposure Worry: The Psychological Impact of Perceived Ionizing Radiation Exposure in British Nuclear Test Veterans" International Journal of Environmental Research and Public Health 18, no. 22: 12188. https://doi.org/10.3390/ijerph182212188





