The Impact of Information Sources on COVID-19-Related Knowledge, Attitudes, and Practices (KAP) among University Students: A Nationwide Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Instrument
2.4. Data Collection
2.5. Outcome Measures
2.6. Ethical Considerations
2.7. Statistical Analysis
3. Results
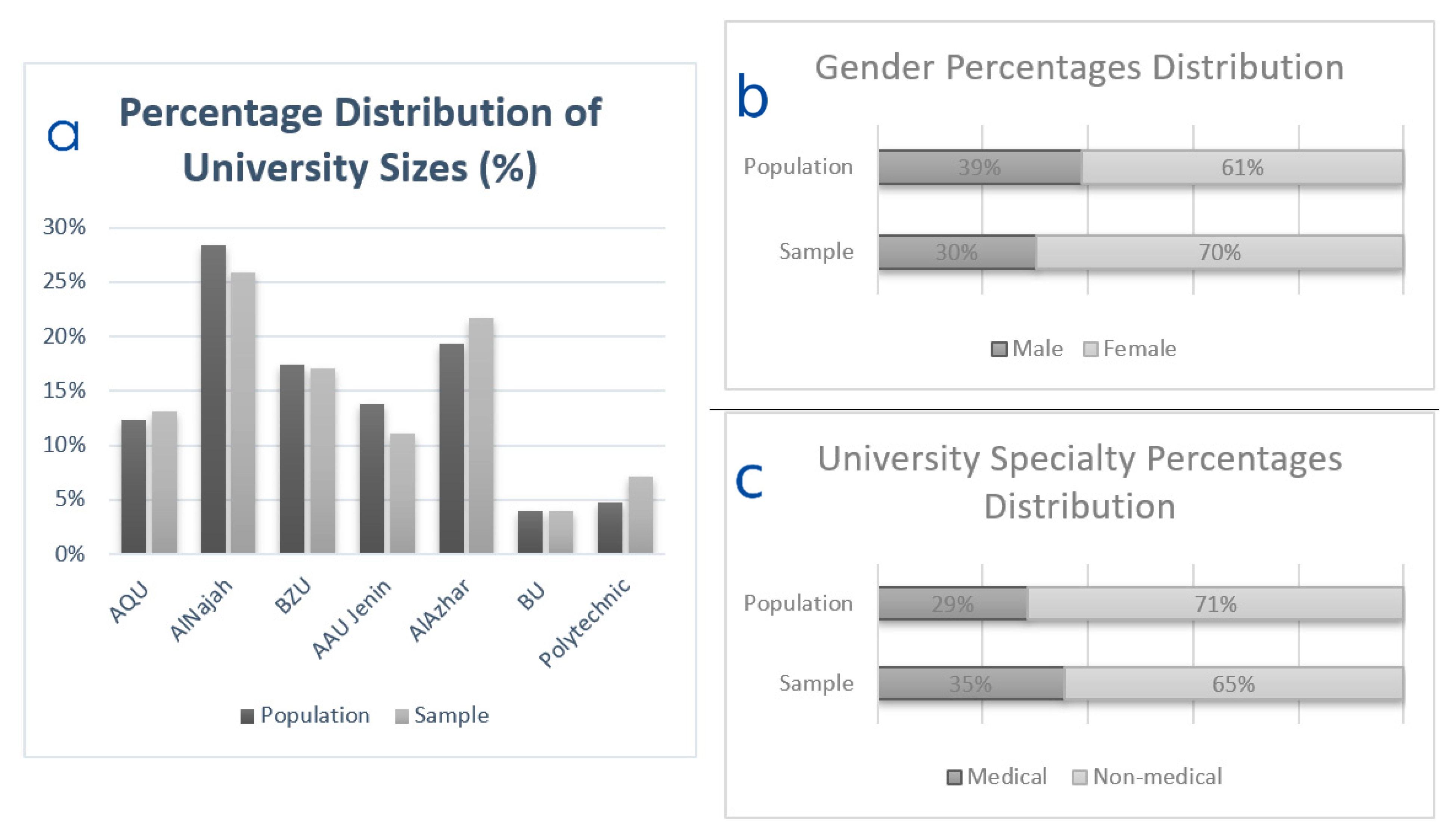
3.1. Demographic Characteristics
3.2. Information Sources
3.3. COVID-19-Related Knowledge
3.4. COVID-19-Related Attitudes
3.5. COVID-19-Related Practices
3.6. Impact of Information Sources on COVID-19-Related KAP
3.7. Information Seeking Strategies and COVID-19 Knowledge
3.8. Information Seeking Strategies and Attitudes towards COVID-19
3.9. Information Seeking Strategies and COVID-19-Related Practices
4. Discussion
4.1. Strengths
4.2. Limitations
4.3. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). COVID-19 Timeline. Available online: https://www.who.int/news/item/27-04-2020-who-timeline---covid-19 (accessed on 19 September 2021).
- World Health Organization (WHO). Novel Coronavirus—China. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON233 (accessed on 19 September 2021).
- World Health Organization (WHO). Naming the Coronavirus Disease (COVID-19) and the Virus That Causes It. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (accessed on 19 September 2021).
- Cascella, M.; Rajnik, M.; Aleem, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment of Coronavirus (COVID-19); StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Zhou, M.; Zhang, X.; Qu, J. Coronavirus disease 2019 (COVID-19): A clinical update. Front. Med. 2020, 14, 126–135. [Google Scholar] [CrossRef] [Green Version]
- Jin, X.; Lian, J.S.; Hu, J.H.; Gao, J.; Zheng, L.; Zhang, Y.M.; Hao, S.R.; Jia, H.Y.; Cai, H.; Zhang, X.L.; et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut 2020, 69, 1002–1009. [Google Scholar] [CrossRef] [Green Version]
- National Institute of Neurological Disorders and Stroke. Coronavirus and the Nervous System. Available online: https://www.ninds.nih.gov/Current-Research/Coronavirus-and-NINDS/nervous-system (accessed on 21 September 2021).
- Ahmed, M.U.; Hanif, M.; Ali, M.J.; Haider, M.A.; Kherani, D.; Memon, G.M.; Karim, A.H.; Sattar, A. Neurological Manifestations of COVID-19 (SARS-CoV-2): A Review. Front. Neurol. 2020, 11, 518. [Google Scholar] [CrossRef]
- Sheraton, M.; Deo, N.; Kashyap, R.; Surani, S. A Review of Neurological Complications of COVID-19. Cureus 2020, 12, e8192. [Google Scholar] [CrossRef]
- Chen, X.; Laurent, S.; Onur, O.A.; Kleineberg, N.N.; Fink, G.R.; Schweitzer, F.; Warnke, C. A systematic review of neurological symptoms and complications of COVID-19. J. Neurol. 2020, 268, 392–402. [Google Scholar] [CrossRef]
- dos Santos, J.A.; Normando, A.G.C.; da Silva, R.L.C.; Acevedo, A.C.; Canto, G.D.L.; Sugaya, N.; Santos-Silva, A.R.; Guerra, E.N.S. Oral Manifestations in Patients with COVID-19: A 6-Month Update. J. Dent. Res. 2021, 100, 1321–1329. [Google Scholar] [CrossRef]
- Rokkas, T. Gastrointestinal involvement in COVID-19: A systematic review and meta-analysis. Ann. Gastroenterol. 2020, 33, 355. [Google Scholar] [CrossRef] [PubMed]
- Tariq, R.; Saha, S.; Furqan, F.; Hassett, L.; Pardi, D.; Khanna, S. Prevalence and Mortality of COVID-19 Patients with Gastrointestinal Symptoms: A Systematic Review and Meta-analysis. Mayo Clin. Proc. 2020, 95, 1632–1648. [Google Scholar] [CrossRef] [PubMed]
- Seirafianpour, F.; Sodagar, S.; Pour Mohammad, A.; Panahi, P.; Mozafarpoor, S.; Almasi, S.; Goodarzi, A. Cutaneous manifestations and considerations in COVID-19 pandemic: A systematic review. Dermatol. Ther. 2020, 33, e13986. [Google Scholar] [CrossRef] [PubMed]
- Wollina, U.; Karadağ, A.S.; Rowland-Payne, C.; Chiriac, A.; Lotti, T. Cutaneous signs in COVID-19 patients: A review. Dermatol. Ther. 2020, 33, e13549. [Google Scholar] [CrossRef]
- Riad, A.; Kassem, I.; Issa, J.; Badrah, M.; Klugar, M. Angular cheilitis of COVID-19 patients: A case-series and literature review. Oral Dis. 2020. [Google Scholar] [CrossRef]
- Hocková, B.; Riad, A.; Valky, J.; Šulajová, Z.; Stebel, A.; Slávik, R.; Bečková, Z.; Pokorná, A.; Klugarová, J.; Klugar, M. Oral Complications of ICU Patients with COVID-19: Case-Series and Review of Two Hundred Ten Cases. J. Clin. Med. 2021, 10, 581. [Google Scholar] [CrossRef]
- Riad, A.; Kassem, I.; Hockova, B.; Badrah, M.; Klugar, M. Tongue ulcers associated with SARS-CoV-2 infection: A case series. Oral Dis. 2020. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. Available online: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations (accessed on 19 September 2021).
- Majumder, J.; Minko, T. Recent Developments on Therapeutic and Diagnostic Approaches for COVID-19. AAPS J. 2021, 23, 14. [Google Scholar] [CrossRef] [PubMed]
- Mahase, E. COVID-19: Molnupiravir reduces risk of hospital admission or death by 50% in patients at risk, MSD reports. BMJ 2021, 375, n2422. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Issues Its First Emergency Use Validation for a COVID-19 Vaccine and Emphasizes Need for Equitable Global Access. Available online: https://www.who.int/news/item/31-12-2020-who-issues-its-first-emergency-use-validation-for-a-covid-19-vaccine-and-emphasizes-need-for-equitable-global-access (accessed on 19 September 2021).
- World Health Organization (WHO). WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—13 March 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 1 May 2020).
- Bloomberg More than 5.92 Billion Shots Given: COVID-19 Vaccine Tracker. Available online: https://www.bloomberg.com/graphics/covid-vaccine-tracker-global-distribution/ (accessed on 19 September 2021).
- Riad, A.; Pokorná, A.; Klugarová, J.; Antalová, N.; Kantorová, L.; Koščík, M.; Klugar, M. Side Effects of mRNA-Based COVID-19 Vaccines among Young Adults (18–30 Years Old): An Independent Post-Marketing Study. Pharmaceuticals 2021, 14, 1049. [Google Scholar] [CrossRef]
- Klugar, M.; Riad, A.; Mekhemar, M.; Conrad, J.; Buchbender, M.; Howaldt, H.-P.; Attia, S. Side Effects of mRNA-Based and Viral Vector-Based COVID-19 Vaccines among German Healthcare Workers. Biology 2021, 10, 752. [Google Scholar] [CrossRef]
- Riad, A.; Hocková, B.; Kantorová, L.; Slávik, R.; Spurná, L.; Stebel, A.; Havriľak, M.; Klugar, M. Side Effects of mRNA-Based COVID-19 Vaccine: Nationwide Phase IV Study among Healthcare Workers in Slovakia. Pharmaceuticals 2021, 14, 873. [Google Scholar] [CrossRef] [PubMed]
- Dziedzic, A.; Riad, A.; Attia, S.; Klugar, M.; Tanasiewicz, M. Self-Reported Adverse Events of COVID-19 Vaccines in Polish Healthcare Workers and Medical Students. Cross-Sectional Study and Pooled Analysis of CoVaST Project Results in Central Europe. J. Clin. Med. 2021, 10, 5338. [Google Scholar] [CrossRef]
- Riad, A.; Sağıroğlu, D.; Üstün, B.; Pokorná, A.; Klugarová, J.; Attia, S.; Klugar, M. Prevalence and Risk Factors of CoronaVac Side Effects: An Independent Cross-Sectional Study among Healthcare Workers in Turkey. J. Clin. Med. 2021, 10, 2629. [Google Scholar] [CrossRef] [PubMed]
- Riad, A.; Pokorná, A.; Mekhemar, M.; Conrad, J.; Klugarová, J.; Koščík, M.; Klugar, M.; Attia, S. Safety of ChAdOx1 nCoV-19 Vaccine: Independent Evidence from Two EU States. Vaccines 2021, 9, 673. [Google Scholar] [CrossRef]
- The British Broadcasting Corporation (BBC). Coronavirus: The World in Lockdown in Maps and Charts. Available online: https://www.bbc.com/news/world-52103747 (accessed on 19 September 2021).
- Kenyon, C. Flattening-the-curve associated with reduced COVID-19 case fatality rates—An ecological analysis of 65 countries. J. Infect. 2020, 81, e98–e99. [Google Scholar] [CrossRef] [PubMed]
- Thunstrom, L.; Newbold, S.; Finnoff, D.; Ashworth, M.; Shogren, J.F. The Benefits and Costs of Using Social Distancing to Flatten the Curve for COVID-19. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Greenstone, M.; Nigam, V. Does Social Distancing Matter? SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Alawia, R.; Riad, A.; Kateeb, E. Risk perception and readiness of dental students to treat patients amid COVID-19: Implication for dental education. Oral Dis. 2020. [Google Scholar] [CrossRef]
- Alawia, R.; Riad, A.; Kateeb, E. Knowledge and attitudes among dental students about COVID-19 and its precautionary measures: A cross-sectional study. J. Oral Med. Oral Surg. 2021, 27, 17. [Google Scholar] [CrossRef]
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 2020, 15, e0236337. [Google Scholar] [CrossRef] [PubMed]
- Fawaz, M.; Samaha, A. E-learning: Depression, anxiety, and stress symptomatology among Lebanese university students during COVID-19 quarantine. Nurs. Forum 2021, 56, 52–57. [Google Scholar] [CrossRef]
- Juvinyà-Canal, D.; Suñer-Soler, R.; Porquet, A.B.; Vernay, M.; Blanchard, H.; Bertran-Noguer, C. Health Literacy among Health and Social Care University Students. Int. J. Environ. Res. Public Health 2020, 17, 2273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vozikis, A.; Drivas, K.; Milioris, K. Health literacy among university students in Greece: Determinants and association with self-perceived health, health behaviours and health risks. Arch. Public Health 2014, 72, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kateeb, E.; Danadneh, M.; Pokorná, A.; Klugarová, J.; Abdulqader, H.; Klugar, M.; Riad, A. Predictors of Willingness to Receive COVID-19 Vaccine: Cross-Sectional Study of Palestinian Dental Students. Vaccines 2021, 9, 954. [Google Scholar] [CrossRef]
- Riad, A.; Abdulqader, H.; Morgado, M.; Domnori, S.; Koščík, M.; Mendes, J.J.; Klugar, M.; Kateeb, E. Global Prevalence and Drivers of Dental Students’ COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 566. [Google Scholar] [CrossRef]
- Attia, S.; Howaldt, H.-P. Impact of COVID-19 on the Dental Community: Part I before Vaccine (BV). J. Clin. Med. 2021, 10, 288. [Google Scholar] [CrossRef]
- Ammar, N.; Aly, N.M.; Folayan, M.O.; Khader, Y.; Virtanen, J.I.; Al-Batayneh, O.B.; Mohebbi, S.Z.; Attia, S.; Howaldt, H.-P.; Boettger, S.; et al. Behavior change due to COVID-19 among dental academics—The theory of planned behavior: Stresses, worries, training, and pandemic severity. PLoS ONE 2020, 15, e0239961. [Google Scholar] [CrossRef] [PubMed]
- Ammar, N.; Aly, N.M.; Folayan, M.O.; Khader, Y.; Mohebbi, S.Z.; Attia, S.; Howaldt, H.-P.; Boettger, S.; Virtanen, J.; Madi, M.; et al. Perceived Preparedness of Dental Academic Institutions to Cope with the COVID-19 Pandemic: A Multi-Country Survey. Int. J. Environ. Res. Public Health 2021, 18, 1445. [Google Scholar] [CrossRef]
- Ammar, N.; Aly, N.M.; Folayan, M.O.; Mohebbi, S.Z.; Attia, S.; Howaldt, H.-P.; Boettger, S.; Khader, Y.; Maharani, D.A.; Rahardjo, A.; et al. Knowledge of dental academics about the COVID-19 pandemic: A multi-country online survey. BMC Med. Educ. 2020, 20, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Mekhemar, M.; Attia, S.; Dörfer, C.; Conrad, J. Dental Students in Germany throughout the COVID-19 Pandemic: A Psychological Assessment and Cross-Sectional Survey. Biology 2021, 10, 611. [Google Scholar] [CrossRef] [PubMed]
- Brennen, J.; Simon, F.; Howard, P.; Nielsen, R. Types, Sources, and Claims of COVID-19 Misinformation. Ph.D. Thesis, University of Oxford, Oxford, UK, 2020. [Google Scholar]
- United Nations Office for the Coordination of Humanitarian Affairs—Occupied Palestinian Territory; United Nations Office for the Coordination of Humanitarian Affairs. COVID-19 Emergency Situation Report 6 (21–28 April 2020). Available online: https://www.ochaopt.org/content/covid-19-emergency-situation-report-6 (accessed on 19 September 2021).
- Nazzal, S. Coronavirus Disease (COVID-19) in Palestine. Available online: https://corona.ps/ (accessed on 19 September 2021).
- Kouzy, R.; Abi Jaoude, J.; Kraitem, A.; El Alam, M.B.; Karam, B.; Adib, E.; Zarka, J.; Traboulsi, C.; Akl, E.W.; Baddour, K.; et al. Coronavirus Goes Viral: Quantifying the COVID-19 Misinformation Epidemic on Twitter. Cureus 2020, 12, e7255. [Google Scholar] [CrossRef] [Green Version]
- Van Bavel, J.J.V.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef]
- Qazi, A.; Qazi, J.; Naseer, K.; Zeeshan, M.; Hardaker, G.; Maitama, J.Z.; Haruna, K. Analyzing situational awareness through public opinion to predict adoption of social distancing amid pandemic COVID-19. J. Med. Virol. 2020, 92, 849–855. [Google Scholar] [CrossRef]
- Setbon, M.; Raude, J. Factors in vaccination intention against the pandemic influenza A/H1N1. Eur. J. Public Health 2010, 20, 490–494. [Google Scholar] [CrossRef] [Green Version]
- Rubin, G.J.; Amlôt, R.; Page, L.; Wessely, S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: Cross sectional telephone survey. BMJ 2009, 339, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, S.T. Managing News Overload (MNO): The COVID-19 Infodemic. Information 2020, 11, 375. [Google Scholar] [CrossRef]
- Bastani, P.; Hakimzadeh, S.M.; Bahrami, M.A. Designing a conceptual framework for misinformation on social media: A qualitative study on COVID-19. BMC Res. Notes 2021, 14, 408. [Google Scholar] [CrossRef] [PubMed]
- Bok, S.; Martin, D.E.; Acosta, E.; Lee, M.; Shum, J. Validation of the COVID-19 Transmission Misinformation Scale and Conditional Indirect Negative Effects on Wearing a Mask in Public. Int. J. Environ. Res. Public Health 2021, 18, 11319. [Google Scholar] [CrossRef]
- Leitner, S.; Gula, B.; Jannach, D.; Krieg-Holz, U.; Wall, F. Understanding the dynamics emerging from infodemics: A call to action for interdisciplinary research. SN Bus. Econ. 2021, 1, 23. [Google Scholar] [CrossRef]
- Bin Naeem, S.; Bhatti, R.; Khan, A. An exploration of how fake news is taking over social media and putting public health at risk. Health Inf. Libr. J. 2021, 38, 143–149. [Google Scholar] [CrossRef]
- Creative Research Systems (CRS). Sample Size Calculator. Available online: https://www.surveysystem.com/sscalc.htm (accessed on 19 September 2021).
- University of Miami. What Does the Public Know about COVID-19? Available online: https://news.miami.edu/stories/2020/04/what-does-the-public-know-about-covid-19.html (accessed on 19 September 2021).
- U.S. Food & Drug Administration (FDA). COVID-19 Frequently Asked Questions. Available online: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-frequently-asked-questions (accessed on 19 September 2021).
- Daniel, C. DeSimone COVID-19 (Coronavirus) Drugs: Are There Any That Work? Available online: https://www.mayoclinic.org/diseases-conditions/coronavirus/expert-answers/coronavirus-drugs/faq-20485627 (accessed on 19 September 2021).
- World Health Organization (WHO). Advice for the Public. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 19 September 2021).
- Bernardi, R.A. Validating Research Results when Cronbach’s Alpha is Below. 70: A Methodological Procedure. Educ. Psychol. Meas. 2016, 54, 766–775. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistics notes: Cronbach’s alpha. BMJ 1997, 314, 572. [Google Scholar] [CrossRef] [Green Version]
- Zhong, B.L.; Luo, W.; Li, H.M.; Zhang, Q.Q.; Liu, X.G.; Li, W.T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef]
- World Medical Association (WMA). World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA J. Am. Med. Assoc. 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. UroToday Int. J. 2007, 335, 806–808. [Google Scholar] [CrossRef] [Green Version]
- SPSS Inc. IBM SPSS Statistics 28. Available online: https://www.ibm.com/support/pages/ibm-spss-statistics-28-documentation (accessed on 14 March 2021).
- Olaimat, A.N.; Aolymat, I.; Shahbaz, H.M.; Holley, R.A. Knowledge and Information Sources About COVID-19 among University Students in Jordan: A Cross-Sectional Study. Front. Public Health 2020, 8, 254. [Google Scholar] [CrossRef] [PubMed]
- Alzoubi, H.; Alnawaiseh, N.; Al-Mnayyis, A.; Abu-Lubad, M.; Aqel, A.; Al-Shagahin, H. COVID-19—Knowledge, attitude and practice among medical and non-medical university students in Jordan. J. Pure Appl. Microbiol. 2020, 14, 17–24. [Google Scholar] [CrossRef] [Green Version]
- Abdelhafiz, A.S.; Mohammed, Z.; Ibrahim, M.E.; Ziady, H.H.; Alorabi, M.; Ayyad, M.; Sultan, E.A. Knowledge, Perceptions, and Attitude of Egyptians Towards the Novel Coronavirus Disease (COVID-19). J. Community Health 2020, 45, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Mixed Migration Centre; Snapshot, M.A. 4Mi Knowledge of COVID-19, Information Sources and Reported Needs among Afghan Returnees. Available online: https://mixedmigration.org/wp-content/uploads/2020/07/120_covid_snapshot_Asia.pdf (accessed on 19 September 2021).
- Wilson, R.E.; Gosling, S.D.; Graham, L.T. A Review of Facebook Research in the Social Sciences. Perspect. Psychol. Sci. 2012, 7, 203–220. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). Coronavirus Disease (COVID-19): Masks. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-masks (accessed on 19 September 2021).
- Cascella, M.; Rajnik, M.; Cuomo, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment Coronavirus; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Alemi, Q.; Stempel, C.; Siddiq, H.; Kim, E. Refugees and COVID-19: Achieving a comprehensive public health response. Bull. World Health Organ. 2020, 98, 510. [Google Scholar] [CrossRef]
- Vonen, H.D.; Olsen, M.L.; Eriksen, S.S.; Jervelund, S.S.; Eikemo, T.A. Refugee camps and COVID-19: Can we prevent a humanitarian crisis? Scand. J. Public Health 2021, 49, 27–28. [Google Scholar] [CrossRef]
- Xiong, P.; Ming, W.; Zhang, C.; Bai, J.; Luo, C.; Cao, W.; Zhang, F.; Tao, Q. Factors Influencing Mental Health Among Chinese Medical and Non-medical Students in the Early Stage of the COVID-19 Pandemic. Front. Public Health 2021, 9, 417. [Google Scholar] [CrossRef]




| Category | Source |
|---|---|
| Official Sources | World Health Organization (WHO) |
| Palestinian Ministry of Health (MoH) | |
| Scientific Sources | Scholarly Articles |
| Healthcare Workers | |
| Community Sources | Friends and Family Members |
| Lecturers | |
| Social Media | |
| Media Sources | Television (TV) |
| Newspapers including news websites |
| Variable | Outcome | Frequency | Percentage |
|---|---|---|---|
| Age | 18–20 years | 462 | 48.6% |
| 21–23 years | 443 | 46.6% | |
| 24–26 years | 39 | 4.1% | |
| >26 years | 7 | 0.7% | |
| Gender | Female | 664 | 69.8% |
| Male | 287 | 30.2% | |
| Social Status | Single | 919 | 96.6% |
| Married | 27 | 2.8% | |
| Divorced | 4 | 0.4% | |
| Widow/er | 1 | 0.1% | |
| Study Field | Healthcare | 337 | 35.4% |
| Non-healthcare | 614 | 64.6% | |
| Study Year | 1st Year | 158 | 16.6% |
| 2nd Year | 201 | 21.1% | |
| 3rd Year | 222 | 23.3% | |
| 4th Year | 236 | 24.8% | |
| 5th Year | 85 | 8.9% | |
| Other | 49 | 5.2% | |
| Residence | City | 549 | 57.7% |
| Village | 337 | 35.4% | |
| Camp | 65 | 6.8% | |
| Monthly Household Income | <1000 ILS | 71 | 7.5% |
| 1000–1999 ILS | 111 | 11.7% | |
| 2000–2999 ILS | 160 | 16.8% | |
| 3000–3999 ILS | 177 | 18.6% | |
| 4000–4999 ILS | 108 | 11.4% | |
| 5000–5999 ILS | 132 | 13.9% | |
| ≥5999 ILS | 192 | 20.2% |
| Item | Outcome | Frequency | Percentage |
|---|---|---|---|
| The main clinical symptoms of COVID-19 are fever, tiredness, sore throat, and dry cough. | Yes | 923 | 97.1% |
| No | 14 | 1.5% | |
| I don’t know | 14 | 1.5% | |
| Some people become infected with SARS-CoV-2 but don’t develop any symptoms and don’t feel sick. | Yes | 862 | 90.6% |
| No | 45 | 4.7% | |
| I don’t know | 44 | 4.6% | |
| It is not necessary for children and young adults to take measures to prevent the infection by SARS-CoV-2. | Yes | 34 | 3.6% |
| No | 35 | 3.7% | |
| I don’t know | 882 | 92.7% | |
| SARS-CoV-2 can be transmitted through mosquito bites. | Yes | 55 | 5.8% |
| No | 305 | 32.1% | |
| I don’t know | 591 | 62.1% | |
| SARS-CoV-2 cannot be transmitted in areas with hot and humid climates. | Yes | 121 | 12.7% |
| No | 250 | 26.3% | |
| I don’t know | 580 | 61% | |
| Persons with COVID-19 are only infectious when they are showing symptoms. | Yes | 91 | 9.6% |
| No | 77 | 8.1% | |
| I don’t know | 783 | 82.3% | |
| SARS-CoV-2 can transmit from through small droplets which are secreted when an infected person coughs or exhales. | Yes | 896 | 94.2% |
| No | 35 | 3.7% | |
| I don’t know | 20 | 2.1% | |
| One of the best ways to protect yourself is to wash your hands frequently with soap or clean them with an alcohol-based hand rub. | Yes | 910 | 95.7% |
| No | 18 | 1.9% | |
| I don’t know | 23 | 2.4% | |
| Physical distancing and treatment of people who are infected with SARS-CoV-2 are effective ways to reduce the spread of the virus. | Yes | 917 | 96.4% |
| No | 14 | 1.5% | |
| I don’t know | 20 | 2.1% | |
| Older persons and persons with pre-existing medical conditions seem to develop serious illness more often than others. | Yes | 885 | 93.1% |
| No | 46 | 4.8% | |
| I don’t know | 20 | 2.1% |
| Item | Outcome | Frequency | Percentage |
|---|---|---|---|
| Are you concerned about the impact that this outbreak will have on your community? | Yes | 778 | 81.8% |
| No | 145 | 15.2% | |
| Not Sure | 28 | 2.9% | |
| Do you think that COVID-19 had been contained and will soon be over? | Yes | 325 | 34.2% |
| No | 447 | 47% | |
| Not Sure | 179 | 18.8% | |
| Do you think the Palestinian Public Health Service was well prepared for the COVID-19 pandemic? | Yes | 290 | 30.5% |
| No | 480 | 50.5% | |
| Not Sure | 181 | 19% |
| Item | Outcome | Frequency | Percentage |
|---|---|---|---|
| Which of the following describes your current behavior? | I am continuing to socialize in public spaces (code = 0) | 28 | 2.9% |
| I do not know (code = 1) | 16 | 1.7% | |
| I am continuing to socialize in public spaces but less often (code = 2) | 92 | 9.7% | |
| I am not going to public spaces, but I am socializing with my friends or family in my or their homes (code = 3) | 229 | 24.1% | |
| I am not going to public spaces, and I am socializing with my friends and family less often (code = 4) | 375 | 39.4% | |
| I am not going to public spaces, and I am not socializing with friends or family (code = 5) | 211 | 22.2% | |
| In the past week, have you gone to any crowded places? | Yes | 202 | 21.2% |
| No | 723 | 76% | |
| I prefer not to answer | 26 | 2.7% | |
| In the past week, have you worn a mask when leaving home? | Yes | 317 | 33.3% |
| No | 572 | 60.1% | |
| Not Sure | 62 | 6.5% |
| Information Sources Groups | Frequency | Percentage | Knowledge Score | Did You Wear a Mask upon Leaving Your House Last Week? | |||
|---|---|---|---|---|---|---|---|
| µ | SD | Yes (%) | No (%) | Not Sure (%) | |||
| C | 154 | 16.2% | 8.5 | 1.6 | 23% | 73% | 5% |
| O | 124 | 13% | 8.6 | 1.3 | 31% | 61% | 7% |
| Sc | 17 | 1.8% | 8.6 | 1.4 | 35% | 59% | 6% |
| T | 14 | 1.5% | 8.6 | 2.8 | 43% | 50% | 7% |
| O + C | 147 | 15.5% | 8.8 | 1.6 | 24% | 67% | 8% |
| O + Sc | 80 | 8.4% | 9.1 | 1.3 | 50% | 44% | 6% |
| C + T | 20 | 2.1% | 7.8 | 2.7 | 30% | 70% | 0% |
| O + T | 16 | 1.7% | 8.4 | 1.5 | 50% | 50% | 0% |
| Sc + C | 14 | 1.5% | 8.5 | 1.1 | 29% | 71% | 0% |
| Sc + T | 1 | 0.1% | 8.0 | - | 0% | 100% | 0% |
| O + Sc + C | 142 | 14.9% | 8.8 | 1.3 | 39% | 51% | 10% |
| O + C + T | 107 | 11.3% | 8.5 | 1.5 | 29% | 66% | 5% |
| O + Sc + T | 12 | 1.3% | 8.5 | 1.9 | 58% | 42% | 0% |
| Sc + C + T | 7 | 0.7% | 8.9 | 1.5 | 43% | 57% | 0% |
| O + Sc + C + T | 94 | 9.9% | 8.8 | 1.4 | 44% | 49% | 7% |
| Other | 2 | 0.2% | 7.5 | 2.1 | 0% | 50% | 50% |
| Variable | Outcome | Do You Think That COVID-19 Has Been Contained and Will Soon Be Over? | ||
|---|---|---|---|---|
| Yes (%) | No (%) | Not Sure (%) | ||
| Trusted Source | Scholarly Articles | 33% | 47% | 20% |
| WHO | 31% | 50% | 18% | |
| MoH | 43% | 39% | 18% | |
| Television | 60% | 40% | 0% | |
| Family, Friends or Lecturers | 60% | 40% | 0% | |
| Social Media | 45% | 30% | 25% | |
| Healthcare Workers | 33% | 44% | 23% | |
| Newspapers | 100% | 0% | 0% | |
| Other | 33% | 50% | 17% | |
| Fact-checking Method | Official Sources | 28% | 52% | 20% |
| Healthcare Workers | 44% | 42% | 14% | |
| Social Media | 45% | 39% | 16% | |
| Searching Web | 39% | 47% | 14% | |
| Family or Friends | 44% | 28% | 28% | |
| Not Sure | 42% | 36% | 23% | |
| Other | 36% | 45% | 18% | |
| Media Format | Video | 36% | 44% | 20% |
| Video and Text | 67% | 33% | 0% | |
| Text | 34% | 48% | 18% | |
| Photo | 23% | 56% | 21% | |
| Voice | 50% | 33% | 17% | |
| Charts | 19% | 59% | 22% | |
| Other | 0% | 100% | 0% | |
| Video, Text, Photos or Charts | 50% | 50% | 0% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baker, I.; Marzouqa, N.; Yaghi, B.N.; Adawi, S.O.; Yousef, S.; Sabooh, T.N.; Salhab, N.M.; Khrishi, H.M.; Qabaja, Y.; Riad, A.; et al. The Impact of Information Sources on COVID-19-Related Knowledge, Attitudes, and Practices (KAP) among University Students: A Nationwide Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 12462. https://doi.org/10.3390/ijerph182312462
Baker I, Marzouqa N, Yaghi BN, Adawi SO, Yousef S, Sabooh TN, Salhab NM, Khrishi HM, Qabaja Y, Riad A, et al. The Impact of Information Sources on COVID-19-Related Knowledge, Attitudes, and Practices (KAP) among University Students: A Nationwide Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(23):12462. https://doi.org/10.3390/ijerph182312462
Chicago/Turabian StyleBaker, Israa, Nizar Marzouqa, Bashar Nafe’ Yaghi, Samer Osama Adawi, Shahd Yousef, Tayseer Nedal Sabooh, Nataly Mazen Salhab, Hiba Mahmoud Khrishi, Yahya Qabaja, Abanoub Riad, and et al. 2021. "The Impact of Information Sources on COVID-19-Related Knowledge, Attitudes, and Practices (KAP) among University Students: A Nationwide Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 23: 12462. https://doi.org/10.3390/ijerph182312462
APA StyleBaker, I., Marzouqa, N., Yaghi, B. N., Adawi, S. O., Yousef, S., Sabooh, T. N., Salhab, N. M., Khrishi, H. M., Qabaja, Y., Riad, A., Kateeb, E., & Attia, S. (2021). The Impact of Information Sources on COVID-19-Related Knowledge, Attitudes, and Practices (KAP) among University Students: A Nationwide Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(23), 12462. https://doi.org/10.3390/ijerph182312462










