Impact of Job Resources and Job Demands on Burnout among Physical Therapy Providers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Analysis
2.2. Measures
2.2.1. Demographic Data
2.2.2. Work Burnout Scale
2.2.3. Secondary Trauma Scale
2.2.4. Basic Psychological Needs at Work Scale
2.2.5. Physical Therapy Satisfaction Scale
3. Results
3.1. Sample Demographics
3.2. Preliminary Analyses
3.3. Impact of Covariates on Burnout
3.4. Impact of Job Demands on Burnout
3.5. Impact of Job Resources on Burnout
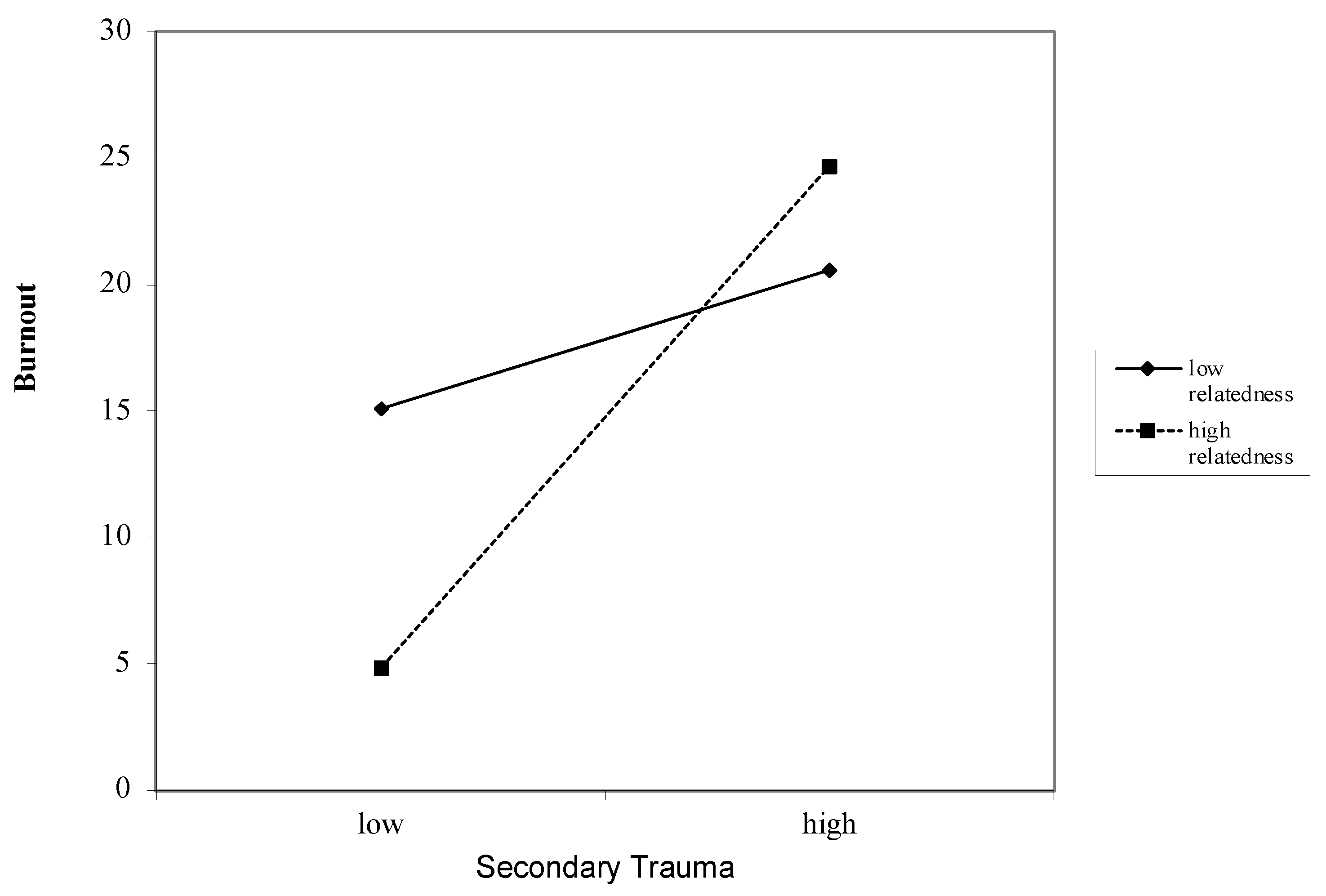
3.6. Interaction between Job Demands and Job Resources on Burnout
4. Discussion
4.1. Practice Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Han, S.; Shanafelt, T.D.; Sinsky, C.A.; Awad, K.M.; Dyrbye, L.N.; Fiscus, L.C.; Trockel, M.; Goh, J. Estimating the Attributable Cost of Physician Burnout in the United States. Ann. Intern. Med. 2019, 170, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef] [Green Version]
- Maslach, V.; Jackson, S.; Leiter, M. The Maslach Burnout Inventory Manual. In Evaluating Stress: A Book of Resources; Scarecrow Education: Lanham, MD, USA, 1997; Volume 3, pp. 191–218. [Google Scholar]
- Maslach, C. What have we learned about burnout and health? Psychol. Health 2001, 16, 607–611. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.E. Burnout in organizational settings. Appl. Soc. Psychol. Annu. 1984, 5, 133–153. [Google Scholar]
- Hall, L.H.; Johnson, J.; Watt, I.; Tsipa, A.; O’Connor, D.B. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS ONE 2016, 11, e0159015. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Clinic, M.; Shanafelt, T.D.; Sinsky, C.A.; Cipriano, P.F.; Bhatt, J.; Ommaya, A.; West, C.P.; Meyers, D.; American Medical Association; et al. Burnout Among Health Care Professionals: A Call to Explore and Address This Underrecognized Threat to Safe, High-Quality Care. NAM Perspect. 2017, 7. [Google Scholar] [CrossRef] [Green Version]
- Toker, S.; Melamed, S.; Berliner, S.; Zeltser, D.; Shapira, I. Burnout and Risk of Coronary Heart Disease. Psychosom. Med. 2012, 74, 840–847. [Google Scholar] [CrossRef] [PubMed]
- Dreison, K.C.; White, D.A.; Bauer, S.M.; Salyers, M.P.; McGuire, A.B. Integrating Self-Determination and Job demands-resources Theory in Predicting Mental Health Provider Burnout. Adm. Policy Ment. Health Ment. Health Serv. Res. 2016, 45, 121–130. [Google Scholar] [CrossRef] [Green Version]
- Bakker, A.; Demerouti, E. The Job Demands-Resources model: State of the art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef] [Green Version]
- Bakker, A.B.; Demerouti, E. Job demands-resources theory: Taking stock and looking forward. J. Occup. Health Psychol. 2017, 22, 273–285. [Google Scholar] [CrossRef]
- De Lange, A.H.; De Witte, H.; Notelaers, G. Should I stay or should I go? Examining longitudinal relations among job resources and work engagement for stayers versus movers. Work Stress 2008, 22, 201–223. [Google Scholar] [CrossRef]
- Broeck, A.V.D.; Vansteenkiste, M.; De Witte, H.; Lens, W. Explaining the relationships between job characteristics, burnout, and engagement: The role of basic psychological need satisfaction. Work Stress 2008, 22, 277–294. [Google Scholar] [CrossRef] [Green Version]
- Bakker, A.B.; Demerouti, E.; Taris, T.W.; Schaufeli, W.B.; Schreurs, P.J.G. A multigroup analysis of the job demands-resources model in four home care organizations. Int. J. Stress Manag. 2003, 10, 16–38. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M.; Vansteenkiste, M. Self-Determination Theory and the Explanatory Role of Psychological Needs in Human Well-Being; Oxford University Press: Oxford, UK, 2008; Available online: https://acuresearchbank.acu.edu.au/item/85z37/self-determination-theory-and-the-explanatory-role-of-psychological-needs-in-human-well-being (accessed on 18 May 2021).
- Deci, E.; Ryan, R.M. The What and Why of Goal Pursuits: Human Needs and the Self-Determination of Behavior. Psychol. Inq. 2000, 11, 227–268. [Google Scholar] [CrossRef]
- Broeck, A.V.D.; Vansteenkiste, M.; De Witte, H.; Soenens, B.; Lens, W. Capturing autonomy, competence, and relatedness at work: Construction and initial validation of the Work-related Basic Need Satisfaction scale. J. Occup. Organ. Psychol. 2010, 83, 981–1002. [Google Scholar] [CrossRef] [Green Version]
- Pardee, R.L. A Literature Review of Selected Theories Dealing With Job Satisfaction and Motivation. In Motivation Theories of Maslow, Herzberg, McGregor & McClelland. Available online: https://www.semanticscholar.org/paper/Motivation-Theories-of-Maslow%2C-Herzberg%2C-McGregor-%26-Pardee/9f7f6e5cc62946c153219e15674e786ee6aac01e (accessed on 18 August 2021).
- Deci, E.L.; Olafsen, A.H.; Ryan, R.M. Self-Determination Theory in Work Organizations: The State of a Science. Annu. Rev. Organ. Psychol. Organ. Behav. 2017, 4, 19–43. [Google Scholar] [CrossRef]
- Donohoe, E.; Nawawi, A.; Wilker, L.; Schindler, T.; Jette, D.U. Factors Associated With Burnout of Physical Therapists in Massachusetts Rehabilitation Hospitals. Phys. Ther. 1993, 73, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Leiter, M.P. Burnout. In Stress: Concepts, Cognition, Emotion, and Behavior; Elsevier: Amsterdam, The Netherlands, 2016; pp. 351–357. [Google Scholar] [CrossRef]
- Wolfe, G.A. Burnout of Therapists. Phys. Ther. 1981, 61, 1046–1050. [Google Scholar] [CrossRef]
- Balogun, J.; Titiloye, V.; Balogun, A.; Oyeyemi, A.; Katz, J. Prevalence and determinants of burnout among physical and occupational therapists. J. Allied Health 2002, 31, 131–139. [Google Scholar]
- Deckard, G.J.; Present, R.M. Impact of Role Stress on Physical Therapists’ Emotional and Physical Well-being. Phys. Ther. 1989, 69, 713–718. [Google Scholar] [CrossRef]
- Pines, A.; Maslach, C. Characteristics of Staff Burnout in Mental Health Settings. Psychiatr. Serv. 1978, 29, 233–237. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E.; Euwema, M.C. Job Resources Buffer the Impact of Job Demands on Burnout. J. Occup. Health Psychol. 2005, 10, 170–180. [Google Scholar] [CrossRef] [Green Version]
- Fernet, C.; Gagné, M.; Austin, S. When does quality of relationships with coworkers predict burnout over time? The moderating role of work motivation. J. Organ. Behav. 2010, 31, 1163–1180. [Google Scholar] [CrossRef]
- Fernet, C.; Austin, S.; Trépanier, S.-G.; Dussault, M. How do job characteristics contribute to burnout? Exploring the distinct mediating roles of perceived autonomy, competence, and relatedness. Eur. J. Work Organ. Psychol. 2013, 22, 123–137. [Google Scholar] [CrossRef]
- Campo, M.; Weiser, S.; Koenig, K.L.; Nordin, M. Work-Related Musculoskeletal Disorders in Physical Therapists: A Prospective Cohort Study With 1-Year Follow-up. Phys. Ther. 2008, 88, 608–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vieira, E.R.; Schneider, P.; Guidera, C.; Gadotti, I.C.; Brunt, D. Work-related musculoskeletal disorders among physical therapists: A systematic review. J. Back Musculoskelet. Rehabil. 2016, 29, 417–428. [Google Scholar] [CrossRef]
- Langballe, E.M.; Innstrand, S.T.; Hagtvet, K.A.; Falkum, E.; Aasland, O.G. The relationship between burnout and musculoskeletal pain in seven Norwegian occupational groups. Work 2009, 32, 179–188. [Google Scholar] [CrossRef]
- Campo, M.; Darragh, A.R. Impact of Work-Related Pain on Physical Therapists and Occupational Therapists. Phys. Ther. 2010, 90, 905–920. [Google Scholar] [CrossRef]
- Adams, R.E.; Boscarino, J.A.; Figley, C.R. Compassion fatigue and psychological distress among social workers: A validation study. Am. J. Orthopsychiatry 2006, 76, 103–108. [Google Scholar] [CrossRef] [Green Version]
- Newell, J.M.; MacNeil, G.A. Professional Burnout, Vicarious Trauma, Secondary Traumatic Stress, and Compassion Fatigue: A Review of Theoretical Terms, Risk Factors, and Preventive Methods for Clinicians and Researchers. In Best Practices in Mental Health; The Follmer Group: Chicago, IL, USA, 2010; Volume 6, pp. 57–68. [Google Scholar]
- Alkema, K.; Linton, J.M.; Davies, R. A Study of the Relationship Between Self-Care, Compassion Satisfaction, Compassion Fatigue, and Burnout Among Hospice Professionals. J. Soc. Work End-Of-Life Palliat. Care 2008, 4, 101–119. [Google Scholar] [CrossRef] [PubMed]
- Bride, B.E.; Radey, M.; Figley, C.R. Measuring Compassion Fatigue. Clin. Soc. Work J. 2007, 35, 155–163. [Google Scholar] [CrossRef]
- Campo, M.; Hyland, M.; Sueki, D.; Pappas, E. Wrist and hand pain in orthopaedic physical therapists: A mixed-methods study. Musculoskelet. Sci. Pr. 2019, 43, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Bowens, A.N.; Amamoo, M.A.; Blake, D.D.; Clark, B. Assessment of Professional Quality of Life in the Alabama Physical Therapy Workforce. Phys. Ther. 2021, 101. [Google Scholar] [CrossRef]
- Hulin, C.L.; Judge, T.A. Job attitudes. In Handbook of Psychology: Industrial and Organizational Psychology; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2003; Volume 13, pp. 255–276. [Google Scholar]
- Madson, T.J.; Hollman, J. Lumbar Traction for Managing Low Back Pain: A Survey of Physical Therapists in the United States. J. Orthop. Sports Phys. Ther. 2015, 45, 586–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheehan, K.B. E-mail Survey Response Rates: A Review. J. Comput. Commun. 2006, 6. [Google Scholar] [CrossRef]
- Green, S.B. How Many Subjects Does It Take to Do a Regression Analysis | EndNote Click. Available online: https://click.endnote.com/viewer?doi=10.1207%2Fs15327906mbr2603_7&token=WzgzNTkzLCIxMC4xMjA3L3MxNTMyNzkwNm1icjI2MDNfNyJd.Co5-1ZDetTCDJlZF395tdq2YW9A (accessed on 19 November 2021).
- Deci, E.L.; Ryan, R.M.; Gagné, M.; Leone, D.R.; Usunov, J.; Kornazheva, B.P. Need Satisfaction, Motivation, and Well-Being in the Work Organizations of a Former Eastern Bloc Country: A Cross-Cultural Study of Self-Determination. Pers. Soc. Psychol. Bull. 2001, 27, 930–942. [Google Scholar] [CrossRef] [Green Version]
- Ilardi, B.C.; Leone, D.; Kasser, T.; Ryan, R.M. Employee and Supervisor Ratings of Motivation: Main Effects and Discrepancies Associated with Job Satisfaction and Adjustment in a Factory Setting1. J. Appl. Soc. Psychol. 1993, 23, 1789–1805. [Google Scholar] [CrossRef]
- Kasser, T.; Davey, J.; Ryan, R.M. Motivation and employee-supervisor discrepancies in a psychiatric vocational rehabilitation setting. Rehabil. Psychol. 1992, 37, 175–188. [Google Scholar] [CrossRef]
- Schuster, N.D.; Nelson, D.L.; Quisling, C. Burnout Among Physical Therapists. Phys. Ther. 1984, 64, 299–303. [Google Scholar] [CrossRef]
- Bakker, A.B.; De Vries, J.D. Job demands-resources theory and self-regulation: New explanations and remedies for job burnout. Anxiety Stress. Coping 2020, 34, 1–21. [Google Scholar] [CrossRef]
- Peiro, J.M.; González-Romá, V.; Tordera, N.; Mañas, M.A. Does role stress predict burnout over time among health care professionals? Psychol. Health 2001, 16, 511–525. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Leiter, M.P.; Jackson, S.E. Making a significant difference with burnout interventions: Researcher and practitioner collaboration. J. Organ. Behav. 2011, 33, 296–300. [Google Scholar] [CrossRef]
- Lynch, A.M.; Kashikar-Zuck, S.; Goldschneider, K.R.; Jones, B.A. Psychosocial Risks for Disability in Children With Chronic Back Pain. J. Pain 2006, 7, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Baard, P.P.; Deci, E.L.; Ryan, R.M. Intrinsic Need Satisfaction: A Motivational Basis of Performance and Weil-Being in Two Work Settings1. J. Appl. Soc. Psychol. 2004, 34, 2045–2068. [Google Scholar] [CrossRef]
- Ducar, D.M.; Penberthy, J.K.; Schorling, J.B.; Leavell, V.A.; Calland, J.F. Mindfulness for healthcare providers fosters professional quality of life and mindful attention among emergency medical technicians. Explore 2020, 16, 61–68. [Google Scholar] [CrossRef]
- Harker, R.; Pidgeon, A.M.; Klaassen, F.; King, S. Exploring resilience and mindfulness as preventative factors for psychological distress burnout and secondary traumatic stress among human service professionals. Work 2016, 54, 631–637. [Google Scholar] [CrossRef]




| Physical demand | 1 | At the end of the workday, I experience physical pain. |
| 2 | I am concerned about the longevity of my career due to the physical strain my job puts on my body. | |
| 3 * | I enjoy the physicality of my work. | |
| 4 | The physical nature of my work restricts my ability to have physically active hobbies | |
| 5 * | My quality of life is not impacted by the physical nature of my job. | |
| Skillset | 1 | I am encouraged to explore my own areas of interest for treatment of my clients |
| 2 | I am able to apply my individual skillset to treat my clients | |
| 3 | I have the freedom to dictate my own continuing education development for techniques for treatment of my clients. | |
| 4 * | I feel restricted by the techniques I am allowed to use in my workplace | |
| 5 * | I do not feel adequately prepared to treat the clients who need my help. | |
| 6 | I have developed an expertise within Physical therapy that I am proud of. | |
| Impact | 1 | I feel like the education I provide to patients helps them better their overall health. |
| 2 | I am confident that my patients have lasting effects from my treatment. | |
| 3 * | I do not feel like my treatments provide long term relief to my clients. | |
| 4 | Most of my clients see improvements in their symptoms | |
| 5 | I make a positive difference in people’s lives | |
| 6 * | The amount of paperwork I am required to do impacts how effective I can be as a clinician. | |
| Respect | 1 | I am glad this is the profession I chose. |
| 2 | I am proud to tell people what I do for a living | |
| 3 | My job title is respected by others in the community. | |
| 4 * | I try to avoid talking to others about my work. | |
| 5 | I am treated as an equal by other healthcare professionals. | |
| 6 * | Physicians often talk down to me. | |
| 7 * | My professional opinion is often overruled by others. | |
| 8 | My clients appreciate the care I give them. |
| Characteristics | Frequency | Percent * |
|---|---|---|
| Gender | ||
| Female | 74 | 69.2 |
| Male | 33 | 30.8 |
| Age | ||
| 25–30 | 17 | 16.0 |
| 31–40 | 29 | 27.4 |
| 41–50 | 20 | 18.9 |
| 51–60 | 25 | 23.6 |
| 61–70 | 15 | 14.2 |
| Income | ||
| <USD 50,000 | 5 | 4.6 |
| USD 50,000–59,000 | 4 | 3.7 |
| USD 60,000–69,000 | 7 | 6.6 |
| USD 70,000–79,000 | 23 | 18.7 |
| USD 80,000–89,000 | 10 | 9.3 |
| USD 90,000–99,000 | 16 | 15.0 |
| USD 100,000–149,000 | 37 | 34.6 |
| >USD 150,000 | 5 | 4.6 |
| Total Debt | ||
| <USD 10,000 | 42 | 40.8 |
| USD 10,000–25,000 | 16 | 15.5 |
| USD 25,000–50,000 | 17 | 16.5 |
| USD 50,000–75,000 | 12 | 11.7 |
| USD 75,000–100,000 | 4 | 3.9 |
| >$100,000 | 12 | 11.7 |
| Setting | ||
| Private Practice | 44 | 41.1 |
| Hospital | 31 | 29.0 |
| Home Health | 3 | 2.8 |
| Other | 29 | 27.1 |
| Specialty | ||
| Orthopedics | 40 | 37.4 |
| Pediatrics | 7 | 6.5 |
| Spine/Neuro | 19 | 6.5 |
| Geriatrics | 7 | 17.8 |
| Other | 34 | 31.8 |
| Title | ||
| Junior PT | 5 | 4.7 |
| Senior PT/Head PT | 44 | 41.1 |
| Manager | 33 | 30.8 |
| Practice Owner | 7 | 16.8 |
| Other | 18 | 6.5 |
| Years Practiced as PT | ||
| <10 | 61 | 57.0 |
| 11–15 | 17 | 15.9 |
| 16–20 | 8 | 7.5 |
| 21–25 | 7 | 6.5 |
| 26–30 | 6 | 5.6 |
| 31+ | 8 | 7.4 |
| % of day spent in direct patient Care | ||
| 0–30% | 20 | 19.0 |
| 31–70% | 17 | 16.2 |
| 71–100% | 68 | 65.7 |
| Measure | M | SD | N | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 44.4 | 12.45 | 106 | ||||||||
| Debt | 10,000–25,000 | 1.18 | 103 | ||||||||
| Income | 80,000–89,000 | 2.04 | 107 | ||||||||
| Setting | 2.16 | 1.23 | 107 | ||||||||
| 1. Autonomy | 5.34 | 0.96 | 105 | (0.76) | |||||||
| 2. Competence | 6.05 | 0.78 | 106 | 0.49 ** | (0.67) | ||||||
| 3. Relatedness | 5.92 | 0.85 | 105 | 0.49 ** | 0.49 ** | (0.83) | |||||
| 4. Physical | 11.67 | 6.01 | 105 | −0.35 ** | −0.18 * | −0.20 * | (0.81) | ||||
| 5. Respect | 18.62 | 2.98 | 106 | 0.38 ** | 0.49 ** | −0.00 | 0.96 | (0.82) | |||
| 6. Impact | 25.03 | 2.62 | 104 | 0.45 ** | 0.63 ** | 0.27 ** | −0.05 | 0.32 ** | (0.79) | ||
| 7. Burnout | 18.90 | 8.72 | 104 | −0.51 ** | −0.51 * | −0.22 * | 0.50 ** | −0.36 ** | −0.36 ** | (0.85) | |
| 8.Secondary Trauma | 10.91 | 5.94 | 105 | −0.27 ** | −0.21 * | −0.16 | 0.39 ** | −0.12 | −0.10 | −0.62 | (0.81) |
| Moderators | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autonomy | Competence | Relatedness | Impact | Respect | ||||||||||||||||
| Variables | Step 1 | Step 2 | Step 3 | Step 4 | Step 1 | Step 2 | Step 3 | Step 4 | Step 1 | Step 2 | Step 3 | Step 4 | Step 1 | Step 2 | Step 3 | Step 4 | Step 1 | Step 2 | Step 3 | Step 4 |
| Age | −0.19 | −0.04 | 0.02 * | 0.05 | −0.19 | −0.04 | −0.02 | 0.02 | −0.19 | −0.04 | −0.07 | 0.09 | −0.19 | −0.04 | 0.02 | 0.04 | −0.19 | −0.04 | −0.02 | −0.01 |
| Total Debt | 0.24 * | 0.20 | 0.18 | 0.15* | 0.24 * | 0.17 | 0.14 | 0.14 | 0.24 * | 0.17 | 0.17 | 0.18 * | 0.24 * | 0.17 | 0.20 * | 0.21 * | 0.24 * | 0.17 | 0.12 | 0.10 |
| Setting | 0.14 | 0.03 | −0.09 | −0.13 | 0.14 | 0.03 | −0.04 | −0.04 | 0.14 | 0.03 | −0.03 | −0.12 | 0.14 | 0.03 | −0.00 | −0.03 | 0.14 | 0.03 | 0.04 | 0.06 |
| Secondary Trauma | 0.57 ** | 0.50 ** | 1.53 ** | 0.57 ** | 0.50 ** | 2.23 * | 0.57 ** | 0.54 ** | −2.13 ** | 0.57 ** | 0.55 ** | 1.24 | 0.57 ** | 0.55 ** | 1.84 ** | |||||
| Moderator | −0.40 ** | −0.03 | −0.40 ** | 0.02 | −0.16 | −0.93 ** | −0.31 ** | −0.19 | −0.26 ** | 0.10 | ||||||||||
| Secondary Trauma x Moderator | −1.01* | −1.70* | 2.74 ** | −0.70 | −1.31 * | |||||||||||||||
| F change | 5.04 * | 44.88 ** | 27.53 ** | 7.78 * | 5.09 * | 45.36 ** | 29.77 ** | 6.22 * | 5.04 * | 44.88 ** | 3.41 | 25.75 ** | 5.00 * | 44.40 ** | 17.38 ** | 0.42 | 5.09 * | 45.36 ** | 11.43 ** | 8.54 * |
| Moderators | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autonomy | Competence | Relatedness | Impact | Respect | ||||||||||||||||
| Variables | Step 1 | Step 2 | Step 3 | Step 4 | Step 1 | Step 2 | Step 3 | Step 4 | Step 1 | Step 2 | Step 3 | Step 4 | Step 1 | Step 2 | Step 3 | Step 4 | Step 1 | Step 2 | Step 3 | Step 4 |
| Age | −0.19 | −0.22 * | −0.14 | −0.13 | −0.19 | −0.22 * | −0.18 * | −0.17 * | −0.19 | −0.22 * | −0.24 * | −0.22 * | −0.19 | −0.22 * | −0.15 | −0.16 | −0.19 | −0.22 | −0.20 * | −0.20 * |
| Total Debt | 0.24 * | 0.22 * | 0.23 * | 0.22 * | 0.24 * | 0.22 * | 0.19 * | 0.19 * | 0.24 * | 0.22 * | 0.22 * | 0.22 * | −0.24 * | 0.22 * | 0.25 ** | 0.25 ** | 0.24 * | 0.22 * | 0.16 | 0.15 |
| Setting | 0.14 | 0.06 | −0.04 | −0.07 | 0.14 | 0.61 | −0.01 | −0.02 | 0.14 | 0.61 | −0.00 | −0.02 | 0.14 | 0.06 | 0.03 | −0.03 | 0.14 | 0.61 * | 0.07 | 0.07 |
| Physical Demands | 0.50 ** | −0.40 ** | 1.05 * | 0.50 ** | 0.44 ** | 0.96 | 0.50 ** | 0.48 ** | 1.03 | 0.50 ** | 0.50 ** | 0.42 | 0.50 ** | 0.50 ** | 1.40 * | |||||
| Moderator | −0.40 ** | −0.13 | −0.40 ** | −0.25 | −0.17 | 0.01 | −0.32 ** | −0.33 | −0.30 ** | −0.05 | ||||||||||
| Physical Demands x Moderator | −0.64 | −0.53 | −0.56 | −0.06 | −1.00 * | |||||||||||||||
| F change | 5.09 * | 37.00 ** | 17.70 ** | 2.51 | 5.09 * | 36.98 ** | 27.56 ** | 1.06 | 5.09 * | 36.98 ** | 3.60 | 1.01 | 5.04 ** | 36.60 ** | 17.10 ** | 0.01 | 5.09 ** | 36.98 ** | 13.43 ** | 3.94 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, R.M.; Bartholomew, J. Impact of Job Resources and Job Demands on Burnout among Physical Therapy Providers. Int. J. Environ. Res. Public Health 2021, 18, 12521. https://doi.org/10.3390/ijerph182312521
Patel RM, Bartholomew J. Impact of Job Resources and Job Demands on Burnout among Physical Therapy Providers. International Journal of Environmental Research and Public Health. 2021; 18(23):12521. https://doi.org/10.3390/ijerph182312521
Chicago/Turabian StylePatel, Rupal M., and John Bartholomew. 2021. "Impact of Job Resources and Job Demands on Burnout among Physical Therapy Providers" International Journal of Environmental Research and Public Health 18, no. 23: 12521. https://doi.org/10.3390/ijerph182312521
APA StylePatel, R. M., & Bartholomew, J. (2021). Impact of Job Resources and Job Demands on Burnout among Physical Therapy Providers. International Journal of Environmental Research and Public Health, 18(23), 12521. https://doi.org/10.3390/ijerph182312521






