Seroprevalence of Anti-SARS-CoV-2 Antibodies among Municipal Staff in the Municipality of Prishtina
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Details
2.2. Patient and Public Involvement
2.3. Sample Selection
2.4. Variables
2.5. Outcome Measures
2.6. Statistical Analysis
3. Results
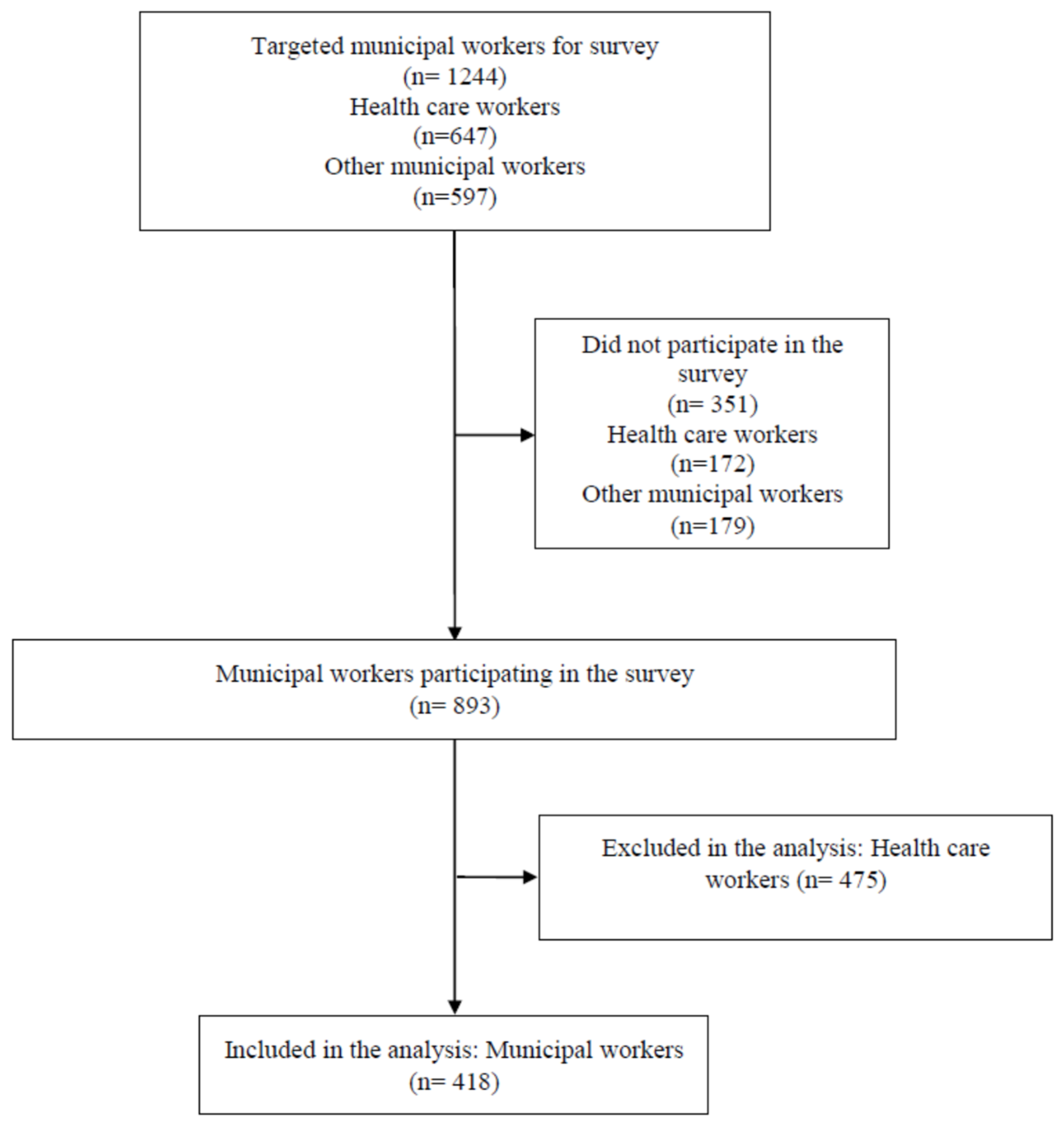
3.1. Study Sample
3.2. Seroprevalence of Anti-SARS-CoV-2 Antibodies
3.3. Effect of Different Factors on Seroprevalence Odds
4. Discussion
4.1. Study Strengths and Limitations
4.2. Context
4.3. Policy Implications
4.4. Research Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bojaj, G.; Agahi, R.; Hoxha, I. Treatment of the First COVID-19 Case in Kosovo and Management of the Pandemic. Sci. Prog. Res. 2021, 1, 58–62. [Google Scholar] [CrossRef]
- WHO. COVID-19 Weekly Epidemiological Update. 25 May 2021. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19 (accessed on 28 November 2021).
- Gallopeni, F.; Bajraktari, I.; Selmani, E.; Tahirbegolli, I.A.; Sahiti, G.; Muastafa, A.; Bojaj, G.; Muharremi, V.B.; Tahirbegolli, B. Anxiety and depressive symptoms among healthcare professionals during the Covid-19 pandemic in Kosovo: A cross sectional study. J. Psychosom. Res. 2020, 137, 110212. [Google Scholar] [CrossRef]
- Kauzya, J.-M.; Niland, E. The Role of Public Service and Public Servants during the COVID-19 Pandemic 2020; Report No.: Policy Brief No. 79; Department of Economic and Social Affairs Economic Analysis, The United Nations: New York, NY, USA, 2020. [Google Scholar]
- Schuster, C.; Weitzman, L.; Mikkelsen, K.S.; Meyer-Sahling, J.; Bersch, K.; Fukuyama, F.; Paskov, P.; Rogger, D.; Mistree, D.; Kay, K. Responding to COVID-19 through Surveys of Public Servants. Public Adm. Rev. 2020, 80, 792–796. [Google Scholar] [CrossRef]
- Contreras, G.S.; Mora, M.R.; Gómez, P.J.; Pablo, B.d.M.; Pablo, C.; del Monte, B. Analysis of Data on Socio-Demographic and Clinical Factors of the COVID-19 Coronavirus Epidemic in Spain on Cases of Recovered and Death Cases. Mod. Appl. Sci. 2020, 14. [Google Scholar] [CrossRef]
- Roederer, T.; Mollo, B.; Vincent, C.; Nikolay, B.; E Llosa, A.; Nesbitt, R.; Vanhomwegen, J.; Rose, T.; Goyard, S.; Anna, F.; et al. Seroprevalence and risk factors of exposure to COVID-19 in homeless people in Paris, France: A cross-sectional study. Lancet Public Health 2021, 6, e202–e209. [Google Scholar] [CrossRef]
- Baral, S.; Chandler, R.; Prieto, R.G.; Gupta, S.; Mishra, S.; Kulldorff, M. Leveraging epidemiological principles to evaluate Sweden’s COVID-19 response. Ann. Epidemiol. 2021, 54, 21–26. [Google Scholar] [CrossRef]
- Inbaraj, L.R.; George, C.E.; Chandrasingh, S. Seroprevalence of COVID-19 infection in a rural district of South India: A population-based seroepidemiological study. PLoS ONE 2021, 16, e0249247. [Google Scholar] [CrossRef]
- Bruckner, T.A.; Parker, D.M.; Bartell, S.M.; Vieira, V.M.; Khan, S.; Noymer, A.; Drum, E.; Albala, B.; Zahn, M.; Boden-Albala, B. Estimated seroprevalence of SARS-CoV-2 antibodies among adults in Orange County, California. Sci. Rep. 2021, 11, 3081. [Google Scholar] [CrossRef] [PubMed]
- Sabino, E.C.; Buss, L.F.; Carvalho, M.P.S.; Prete, C.A., Jr.; Crispim, M.A.E.; Fraiji, N.A.; Pereira, R.H.M.; Parag, K.V.; da Silva Peixoto, P.; Kraemer, M.U.G.; et al. Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence. Lancet 2021, 397, 452–455. [Google Scholar] [CrossRef]
- Alharbi, N.K.; Alghnam, S.; Algaissi, A.; Albalawi, H.; Alenazi, M.W.; Albargawi, A.M.; Alharbi, A.G.; Alhazmi, A.; Al Qarni, A.; Alfarhan, A.; et al. Nationwide Seroprevalence of SARS-CoV-2 in Saudi Arabia. J. Infect. Public Health 2021, 14, 832–838. [Google Scholar] [CrossRef]
- Poustchi, H.; Darvishian, M.; Mohammadi, Z.; Shayanrad, A.; Delavari, A.; Bahadorimonfared, A.; Eslami, S.; Javanmard, S.H.; Shakiba, E.; Somi, M.H.; et al. SARS-CoV-2 antibody seroprevalence in the general population and high-risk occupational groups across 18 cities in Iran: A population-based cross-sectional study. Lancet Infect. Dis. 2021, 21, 473–481. [Google Scholar] [CrossRef]
- Rostami, A.; Sepidarkish, M.; Leeflang, M.M.; Riahi, S.M.; Shiadeh, M.N.; Esfandyari, S.; Mokdad, A.H.; Hotez, P.J.; Gasser, R.B. SARS-CoV-2 seroprevalence worldwide: A systematic review and meta-analysis. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2021, 27, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, H.; Seyama, K.; Ito, K.; Ai, T.; Nojiri, S.; Hori, S.; Wakita, M.; Saito, K.; Shida, Y.; Nagura, R.; et al. SARS-CoV-2 seroprevalence in healthcare workers at a frontline hospital in Tokyo. Sci. Rep. 2021, 11, 8380. [Google Scholar] [CrossRef]
- Montenegro, P.; Brotons, C.; Serrano, J.; Fernández, D.; Garcia-Ramos, C.; Ichazo, B.; Lemaire, J.; Moral, I.; Wienese, R.P.; Pitarch, M.; et al. Community seroprevalence of COVID-19 in probable and possible cases at primary health care centres in Spain. Fam. Pract. 2021, 38, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Alkurt, G.; Murt, A.; Aydin, Z.; Tatli, O.; Agaoglu, N.B.; Irvem, A.; Aydin, M.; Karaali, R.; Gunes, M.; Yesilyurt, B.; et al. Seroprevalence of coronavirus disease 2019 (COVID-19) among health care workers from three pandemic hospitals of Turkey. PLoS ONE 2021, 16, e0247865. [Google Scholar] [CrossRef]
- Suda, G.; Ogawa, K.; Kimura, M.; Maehara, O.; Kitagataya, T.; Ohara, M.; Tokuchi, Y.; Kubo, A.; Yamada, R.; Shigesawa, T.; et al. Time-dependent changes in the seroprevalence of COVID-19 in asymptomatic liver disease outpatients in an area in Japan undergoing a second wave of COVID-19. Hepatol. Res. 2020, 50, 1196–1200. [Google Scholar] [CrossRef]
- Murhekar, M.V.; Bhatnagar, T.; Selvaraju, S.; Rade, K.; Saravanakumar, V.; Thangaraj, J.W.V.; Kumar, M.S.; Shah, N.; Sabarinathan, R.; Turuk, A.; et al. Prevalence of SARS-CoV-2 infection in India: Findings from the national serosurvey, May–June 2020. Indian J. Med. Res. 2020, 152, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Mutambudzi, M.; Niedzwiedz, C.; Macdonald, E.B.; Leyland, A.; Mair, F.; Anderson, J.; Celis-Morales, C.; Cleland, J.; Forbes, J.; Gill, J.; et al. Occupation and risk of severe COVID-19: Prospective cohort study of 120 075 UK Biobank participants. Occup. Environ. Med. 2021, 78, 307. [Google Scholar] [CrossRef]
- Pathela, P.; Crawley, A.; Weiss, D.; Maldin, B.; Cornell, J.; Purdin, J.; Schumacher, P.K.; Marovich, S.; Li, J.; Daskalakis, D.; et al. Seroprevalence of SARS-CoV-2 following the largest initial epidemic wave in the United States: Findings from New York City, May 13–July 21, 2020. J. Infect. Dis. 2021, 224, 196–206. [Google Scholar] [CrossRef]
- Tuells, J.; Egoavil, C.M.; Pardo, M.A.P.; Montagud, A.C.; Montagud, E.; Caballero, P.; Zapater, P.; Puig-Barberá, J.; Hurtado-Sanchez, J.A. Seroprevalence study and cross-sectional survey on COVID-19 for a plan to reopen the University of Alicante (Spain). Int. J. Environ. Res. Public Health 2021, 18, 1908. [Google Scholar] [CrossRef]
- Singh, P.P.; Srivastava, A.K.; Upadhyay, S.K.; Singh, A.; Upadhyay, S.; Kumar, P.; Rai, V.; Shrivastava, P.; Chaubey, G. The association of ABO blood group with the asymptomatic COVID-19 cases in India. medRxiv 2021, arXiv:2021.04.01.21254681. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strobe Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Li, W.; Zhang, B.; Lu, J.; Liu, S.; Chang, Z.; Peng, C.; Liu, X.; Zhang, P.; Ling, Y.; Tao, K.; et al. Characteristics of Household Transmission of COVID-19. Clin. Infect. Dis. 2020, 71, 1943–1946. [Google Scholar] [CrossRef] [PubMed]
- Lan, F.-Y.; Suharlim, C.; Kales, S.N.; Yang, J. Association between SARS-CoV-2 infection, exposure risk and mental health among a cohort of essential retail workers in the USA. Occup. Environ. Med. 2021, 78, 237–243. [Google Scholar] [CrossRef]
- Shastri, M.D.; Shukla, S.D.; Chong, W.C.; Kc, R.; Dua, K.; Patel, R.P.; Peterson, G.M.; O’Toole, R.F. Smoking and COVID-19: What we know so far. Respir. Med. 2021, 176, 106237. [Google Scholar] [CrossRef] [PubMed]
- Van Zyl-Smit, R.N.; Richards, G.; Leone, F.T. Tobacco smoking and COVID-19 infection. Lancet Respir. Med. 2020, 8, 664–665. [Google Scholar] [CrossRef]
- Deeks, J.J.; Dinnes, J.; Takwoingi, Y.; Davenport, C.; Spijker, R.; Taylor-Phillips, S.; Adriano, A.; Beese, S.; Dretzke, J.; di Ruffano, L.F.; et al. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst. Rev. 2020, 2020, CD013652. [Google Scholar]
- Moodley, S.V.; Zungu, M.; Malotle, M.; Voyi, K.; Claassen, N.; Ramodike, J.; Thunzi, N.; Mlangeni, N. A health worker knowledge, attitudes and practices survey of SARS-CoV-2 infection prevention and control in South Africa. BMC Infect. Dis. 2021, 21, 138. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, A.; Kandil, S.; El-Sayed, M.H.; Girgis, S.; Hafez, H.; Yosef, M.; Saber, S.; Ezzelarab, H.; Ramadan, M.; Afifi, I.; et al. Universal COVID-19 screening of 4040 health care workers in a resource-limited setting: An Egyptian pilot model in a university with 12 public hospitals and medical centers. Int. J. Epidemiol. 2021, 50, 50–61. [Google Scholar] [CrossRef]
- Mukwege, D.; Byabene, A.K.; Akonkwa, E.M.; Dahma, H.; Dauby, N.; Buhendwa, J.-P.C.; Le Coadou, A.; Montesinos, I.; Bruyneel, M.; Cadière, G.-B.; et al. High SARS-CoV-2 Seroprevalence in Healthcare Workers in Bukavu, Eastern Democratic Republic of Congo. Am. J. Trop. Med. Hyg. 2021, 104, 1526–1530. [Google Scholar] [CrossRef] [PubMed]
- Dang, A.K.; Le, X.T.T.; Le, H.T.; Tran, B.X.; Do, T.T.T.; Phan, H.T.B.; Nguyen, T.T.; Pham, Q.T.; Ta, N.T.K.; Nguyen, Q.T.; et al. Evidence of COVID-19 Impacts on Occupations During the First Vietnamese National Lockdown. Ann. Glob. Health. 2020, 86, 112. [Google Scholar] [CrossRef]
- Baptista, M.C.; Burton, W.N.; Pawlecki, B.; Pransky, G. A Physician’s Guide for Workers’ Return to Work During COVID-19 Pandemic. J. Occup. Environ. Med. 2021, 63, 199–220. [Google Scholar] [CrossRef]
- Fellows of the Collegium Ramazzini. 24th Collegium Ramazzini Statement: Prevention of Work-Related Infection in the COVID-19 Pandemic. Ann. Glob. Health 2020, 86, 79. [Google Scholar] [CrossRef] [PubMed]
- Iavicoli, S.; Boccuni, F.; Buresti, G.; Gagliardi, D.; Persechino, B.; Valenti, A.; Rondinone, B.M. Risk assessment at work and prevention strategies on COVID-19 in Italy. PLoS ONE 2021, 16, e0248874. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J.; Chu, D.K.; Akl, E.A.; El-harakeh, A.; Bognanni, A.; et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Fan, Z.; Mou, Y.; Cheng, R.; Zhao, Y.; Zhang, F. Investigation of Knowledge, Attitude and Practice of Personal Protection Among Different Types of Workers Returning to Work Under COVID-19 Epidemic. Front. Public Health 2021, 9, 679699. [Google Scholar] [CrossRef]
- Sharma, N.; Sharma, P.; Basu, S.; Saxena, S.; Chawla, R.; Dushyant, K.; Mundeja, N.; Marak, Z.S.; Singh, S.; Singh, G.K.; et al. The seroprevalence and trends of SARS-CoV-2 in Delhi, India: A repeated population-based seroepidemiological study. medRxiv 2020, arXiv:2020.12.13.20248123. [Google Scholar] [CrossRef]
- Prats-Uribe, A.; Paredes, R.; Prieto-Alhambra, D. Ethnicity, comorbidity, socioeconomic status, and their associations with COVID-19 infection in England: A cohort analysis of UK Biobank data. medRxiv 2020. [Google Scholar] [CrossRef]
- Møller, M. The Dilemma between Self-Protection and Service Provision under Danish COVID-19 Guidelines: A Comparison of Public Servants’ Experiences in the Pandemic Frontline. J. Comp. Policy Anal. Res. Pract. 2021, 23, 95–108. [Google Scholar] [CrossRef]
- Franch-Pardo, I.; Napoletano, B.M.; Rosete-Verges, F. Spatial analysis and GIS in the study of COVID-19. Rev. Sci. Total. Environ. 2020, 739, 140033. [Google Scholar] [CrossRef]
- Ahasan, R.; Hossain, M. Leveraging GIS and spatial analysis for informed decision-making in COVID-19 pandemic. Health Policy Technol. 2021, 10, 7–9. [Google Scholar] [CrossRef] [PubMed]
| Events/Total; % | |
|---|---|
| IgM- or IgG-positive | 88/418; 21.05% |
| IgM-positive | 40/418; 9.57% |
| IgG-positive | 81/418; 19.38% |
| Variable a | Positive | Negative | Crude Odds Ratio (95% CI) | p Value | Adjusted Odds Ratio (95% CI) | p Value |
|---|---|---|---|---|---|---|
| Events/Total; % | Events/Total; % | |||||
| Blood Group | ||||||
| O | 26/88; 29.5% | 106/330; 32.1% | Reference | Reference | ||
| A | 27/88; 30.7% | 80/330; 24.2% | 1.38 (0.75–2.54) | 0.307 | 1.35 (0.70–2.61) | 0.375 |
| B | 11/88; 12.5% | 26/330; 7.9% | 1.72 (0.76–3.94) | 0.195 | 1.72 (0.70–4.24) | 0.240 |
| AB | 3/88; 3.4% | 18/330; 5.5% | 0.68 (0.19–2.48) | 0.559 | 0.57 (0.15–2.23) | 0.420 |
| Do not know/refuse | 21/88; 23.9% | 100/330; 30.3% | 0.86 (0.45–1.62) | 0.633 | 1.05 (0.53–2.06) | 0.896 |
| With existing conditions | 8/88; 9.1% | 55/330; 16.7% | 0.50 (0.23–1.09) | 0.082 | 0.59 (0.26–1.35) | 0.211 |
| Smoking | 17/88; 19.3% | 119/330; 36.1% | 0.42 (0.24–0.75) | 0.003 | 0.52 (0.28–0.97) | 0.040 |
| Has infected family members | 37/88; 42.0% | 82/330; 24.8% | 2.19 (1.34–3.59) | 0.002 | 2.00 (1.17–3.41) | 0.011 |
| Settlement size | 178.6077 * | 220.1931 ** | 1.00 (1.00–1.00) | 0.023 | 1.00 (1.00–1.00) | 0.028 |
| Hand Hygiene is Regularly Practiced | ||||||
| False | 1/88; 1.1% | 5/330; 1.5% | Reference | Reference | ||
| True | 85/88; 96.6% | 324/330; 98.2% | 1.31 (0.15–11.38) | 0.806 | 0.68 (0.04–11.54) | 0.791 |
| Do not know/refuse | 2/88; 2.3% | 1/330; 0.3% | 9.99 (0.40–250.42) | 0.161 | 0.10 (0.00–19.27) | 0.394 |
| Family Member that Respect Maximally Protective Measures | ||||||
| False | 1/88; (1.1) | 5/330; (1.5) | Reference | Reference | ||
| True | 84/88; 95.5% | 323/330; 97.9% | 1.30 (0.15–11.28) | 0.812 | 1.06 (0.05–21.55) | 0.969 |
| Do not know/refuse | 3/88; 3.4% | 2/330; 0.6% | 7.50 (0.46–122.70) | 0.158 | 13.61 (0.16–1146.77) | 0.248 |
| Keeping Distance of 2 m in the Office | ||||||
| False | 9/88; 10.2% | 48/330; 14.5% | Reference | Reference | ||
| True | 64/88; 72.7% | 247/330; 74.8% | 1.38 (0.64–2.96) | 0.406 | 1.36 (0.51–3.65) | 0.540 |
| Do not know/refuse | 15/88; 17.0% | 35/330; 10.6% | 2.29 (0.90–5.82) | 0.083 | 0.59 (0.93–3.80) | 0.581 |
| Keeping Distance of 2 m in Other Workplace Spaces | ||||||
| False | 9/88; 10.2% | 41/330; 12.4% | Reference | Reference | ||
| True | 63/88; 71.6% | 262/330; 79.4% | 1.09 (0.51–2.37) | 0.817 | 1.00 (0.35–2.87) | 0.998 |
| Do not know/refuse | 16/88; 18.2% | 27/33;0 8.2% | 2.70 (1.04–6.98) | 0.041 | 3.23 (0.50–21.00) | 0.220 |
| Leave from Work of Workers Positive with COVID-19 Practiced | ||||||
| False | 3/88; 3.4% | 7/330; 2.1% | Reference | Reference | ||
| True | 75/88; 85.2% | 307/330; 93.0% | 0.57 (0.14–2.26) | 0.423 | 0.51 (0.10–2.52) | 0.407 |
| Do not know/refuse | 10/88; 11.4% | 16/330; 4.8% | 1.46 (0.30–6.98) | 0.637 | 0.65 (0.98–4.36) | 0.661 |
| Presence in Crowded Workplace Locations | ||||||
| False | 32/88; 36.4% | 166/330; 50.3% | Reference | Reference | ||
| True | 27/88; 30.7% | 98/330; 29.7% | 1.43 (0.81–2.53) | 0.219 | 1.33 (0.72–2.47) | 0.362 |
| Do not know/refuse | 29/88; 33.0% | 66/330; 20.0% | 2.28 (1.28–4.06) | 0.005 | 1.76 (0.90–3.41) | 0.096 |
| Careful Office | ||||||
| False | 3/88; 3.4% | 21/330; 6.4% | Reference | Reference | ||
| True | 81/88; 92.0% | 303/330; 91.8% | 1.87 (0.54–6.43) | 0.320 | 2.88 (0.59–14.02) | 0.19 |
| Do not know/refuse | 4/88; 4.5% | 6/330; 1.8% | 4.67 (0.81–26.87) | 0.085 | 3.45 (0.34–35.01) | 0.294 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gashi, B.; Osmani, V.; Halili, R.; Hoxha, T.; Kamberi, A.; Hoti, N.; Agahi, R.; Basha, V.; Berisha, V.; Hoxha, I. Seroprevalence of Anti-SARS-CoV-2 Antibodies among Municipal Staff in the Municipality of Prishtina. Int. J. Environ. Res. Public Health 2021, 18, 12545. https://doi.org/10.3390/ijerph182312545
Gashi B, Osmani V, Halili R, Hoxha T, Kamberi A, Hoti N, Agahi R, Basha V, Berisha V, Hoxha I. Seroprevalence of Anti-SARS-CoV-2 Antibodies among Municipal Staff in the Municipality of Prishtina. International Journal of Environmental Research and Public Health. 2021; 18(23):12545. https://doi.org/10.3390/ijerph182312545
Chicago/Turabian StyleGashi, Bujar, Vesa Osmani, Rrezart Halili, Teuta Hoxha, Agron Kamberi, Nexhmedin Hoti, Riaz Agahi, Vlora Basha, Visar Berisha, and Ilir Hoxha. 2021. "Seroprevalence of Anti-SARS-CoV-2 Antibodies among Municipal Staff in the Municipality of Prishtina" International Journal of Environmental Research and Public Health 18, no. 23: 12545. https://doi.org/10.3390/ijerph182312545
APA StyleGashi, B., Osmani, V., Halili, R., Hoxha, T., Kamberi, A., Hoti, N., Agahi, R., Basha, V., Berisha, V., & Hoxha, I. (2021). Seroprevalence of Anti-SARS-CoV-2 Antibodies among Municipal Staff in the Municipality of Prishtina. International Journal of Environmental Research and Public Health, 18(23), 12545. https://doi.org/10.3390/ijerph182312545








