Health Literacy in the Canton of Zurich: First Results of a Representative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Questionnaire
2.2.1. Health-Literacy-Index and Specific Indices
- 0 to 25 points = inadequate health literacy,
- >25 to 33 points = problematic health literacy,
- >33 to 42 points = sufficient health literacy,
- >42 to 50 points = excellent health literacy.
2.2.2. Sociodemographic Characteristics
2.3. Statistical Analyses
3. Results
3.1. Characteristics of the Study Population
3.2. Health Literacy of the Population of Zurich
3.3. Sociodemographic Characteristics and Health Literacy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Item | On a Scale from Very Easy to Very Difficult, how Easy Would You Say It Is… | Very Easy | Rather Easy | Rather Difficult | Very Difficult | No Answer |
|---|---|---|---|---|---|---|
| 1 | to find information about symptoms of illnesses that concern you? | 2 | 15 | 58 | 25 | 0 |
| 2 | to find information on treatments of illnesses that concern you? | 4 | 19 | 56 | 20 | 1 |
| 3 | to find out what to do in case of a medical emergency? | 2 | 13 | 47 | 37 | 1 |
| 4 | to find out where to get professional help when you are ill? (e.g., doctor, pharmacist, psychologist) | 1 | 13 | 55 | 31 | 0 |
| 5 | to understand what your doctor says to you? | 4 | 12 | 54 | 30 | 0 |
| 6 | to understand the leaflets that come with your medicine? | 6 | 16 | 50 | 26 | 2 |
| 7 | to understand what to do in a medical emergency? | 1 | 10 | 54 | 33 | 2 |
| 8 | to understand your doctor’s or pharmacist’s instruction on how to take a prescribed medicine? | 0 | 5 | 54 | 41 | 0 |
| 9 | to judge how information from your doctor applies to you? | 2 | 19 | 56 | 22 | 1 |
| 10 | to judge the advantages and disadvantages of different treatment options? | 15 | 35 | 37 | 11 | 2 |
| 11 | to judge when you may need to get a second opinion from another doctor? | 9 | 29 | 43 | 14 | 5 |
| 12 | to judge if the information about illness in the media is reliable? (e.g., TV, Internet or other media) | 17 | 27 | 43 | 9 | 4 |
| 13 | to use information the doctor gives you to make decisions about your illness? | 4 | 13 | 60 | 21 | 2 |
| 14 | to follow the instructions on medication? | 2 | 5 | 51 | 42 | 0 |
| 15 | to call an ambulance in an emergency? | 0 | 2 | 32 | 65 | 1 |
| 16 | to follow instructions from your doctor or pharmacist? | 1 | 4 | 54 | 41 | 0 |
| 17 | to find information about how to manage unhealthy behavior such as smoking, low physical activity and drinking too much? | 1 | 11 | 53 | 32 | 3 |
| 18 | to find information on how to manage mental health problems like stress or depression? | 6 | 29 | 41 | 18 | 6 |
| 19 | to find information about vaccinations and health screenings that you should have? (e.g., colorectal cancer screening, blood sugar test) | 3 | 18 | 54 | 23 | 2 |
| 20 | to find information on how to prevent or manage conditions like being overweight, high blood pressure or high cholesterol? | 1 | 12 | 60 | 27 | 0 |
| 21 | to understand health warnings about behavior such as smoking, low physical activity and drinking too much? | 1 | 11 | 52 | 36 | 0 |
| 22 | to understand why you need vaccinations? | 3 | 11 | 54 | 30 | 2 |
| 23 | to understand why you need health screenings? (e.g., colorectal cancer screening, blood sugar test) | 1 | 6 | 50 | 43 | 0 |
| 24 | to judge how reliable health warnings are, such as smoking, low physical activity and drinking too much? | 2 | 16 | 48 | 33 | 1 |
| 25 | to judge when you need to go to a doctor for a check-up? | 6 | 22 | 49 | 23 | 0 |
| 26 | to judge which vaccinations you may need? | 13 | 29 | 43 | 14 | 1 |
| 27 | to judge which health screenings you may have? (e.g., colorectal cancer screening, blood sugar test) | 17 | 29 | 34 | 19 | 1 |
| 28 | to judge if the information on health risks in the media is reliable? (e.g., TV, Internet or other media) | 20 | 25 | 44 | 9 | 2 |
| 29 | to decide if you should have a flu vaccination? | 5 | 19 | 46 | 28 | 2 |
| 30 | to decide how you can protect yourself from illness based on advice from family and friends? | 6 | 16 | 59 | 16 | 3 |
| 31 | to decide how you can protect yourself from illness based on information in the media? (e.g., Newspapers, TV or Internet) | 10 | 28 | 47 | 10 | 5 |
| 32 | to find information on healthy activities such as exercise, healthy food and nutrition? | 1 | 3 | 57 | 39 | 0 |
| 33 | to find out about activities that are good for your mental well-being? | 4 | 18 | 49 | 26 | 3 |
| 34 | to find information on how your neighborhood could be more health-friendly? | 6 | 30 | 45 | 18 | 1 |
| 35 | to find out about political changes that may affect health? | 22 | 39 | 29 | 7 | 3 |
| 36 | to find out about efforts to promote your health at work, at school or in the community? | 6 | 21 | 42 | 20 | 11 |
| 37 | to understand advice on health from family members or friends? | 4 | 11 | 60 | 23 | 2 |
| 38 | to understand information on food packaging? | 9 | 21 | 51 | 18 | 1 |
| 39 | to understand information in the media on how to get healthier? | 8 | 17 | 54 | 19 | 2 |
| 40 | to understand information on how to keep your mind healthy? | 4 | 23 | 53 | 19 | 1 |
| 41 | to judge where your life affects your health and wellbeing? | 4 | 35 | 45 | 15 | 1 |
| 42 | to judge how your housing conditions help you to stay healthy? | 3 | 22 | 56 | 18 | 1 |
| 43 | to judge which everyday behavior is related to your health? | 2 | 25 | 48 | 25 | 0 |
| 44 | to make decisions to improve your health? | 4 | 18 | 52 | 26 | 0 |
| 45 | to join a sports club or exercise class if you want to? | 2 | 10 | 47 | 40 | 1 |
| 46 | to influence your living conditions that affect your health and wellbeing? | 5 | 29 | 49 | 17 | 0 |
| 47 | to take part in activities that improve health and wellbeing? | 4 | 21 | 52 | 19 | 4 |
Appendix B
| Domains of HL | Excellent | Sufficient | Problematic | Inadequate |
|---|---|---|---|---|
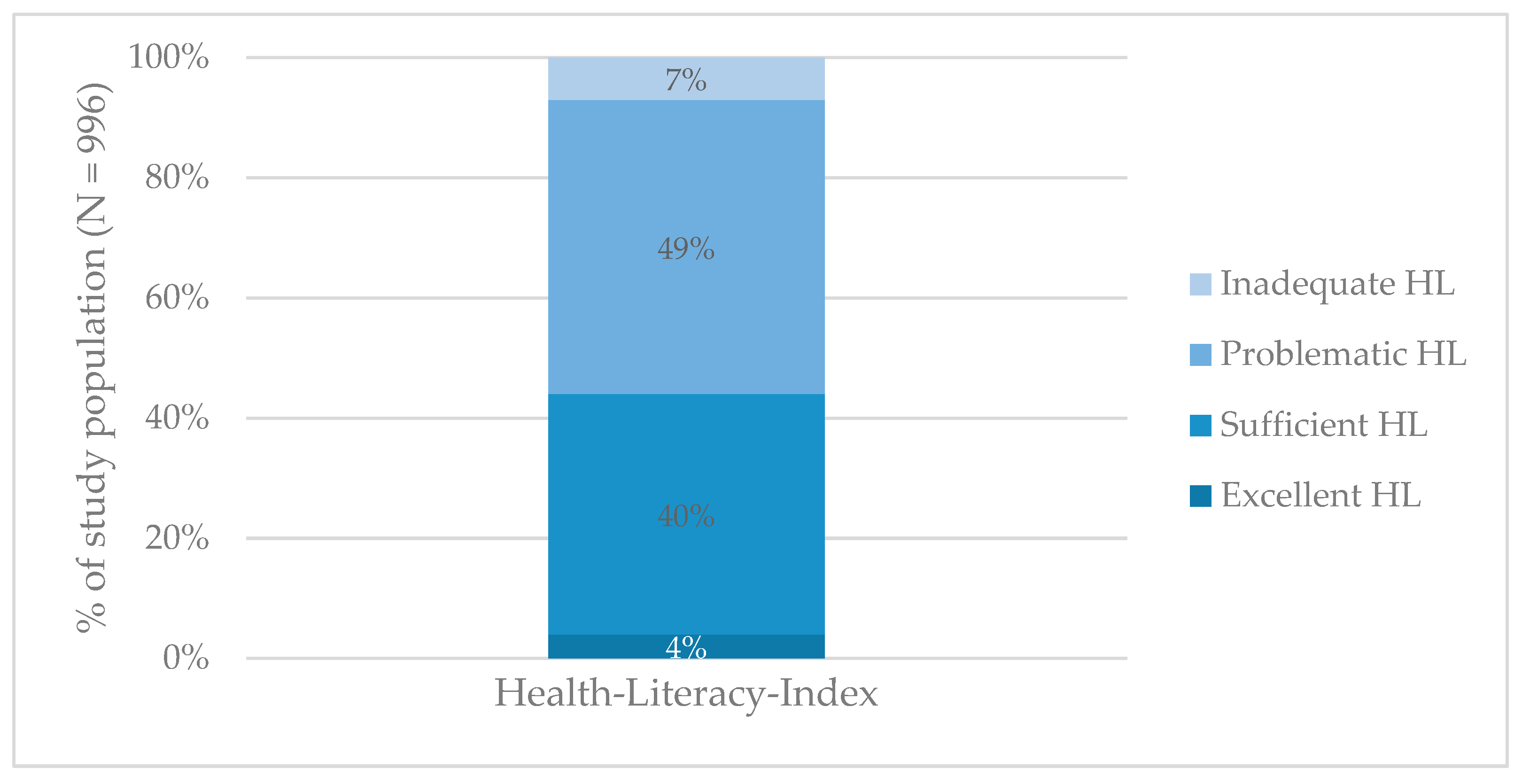
| health literacy | 4% | 40% | 49% | 7% |
| health promotion | 3% | 35% | 49% | 13% |
| disease prevention | 6% | 39% | 44% | 11% |
| healthcare | 7% | 56% | 30% | 7% |
References
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H.; (HLS-EU) Consortium Health Literacy Project European. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sørensen, K.; Pleasant, A. Understanding the Conceptual Importance of the Differences Among Health Literacy Definitions. Stud. Health Technol. Inform. 2017, 240, 3–14. [Google Scholar] [PubMed]
- De Gani, S.M.; Rebecca, J.; Bieri, U.; Kocher, J.P. Health Literacy Survey Schweiz 2019–2021; Schlussbericht im Auftrag des Bundesamt für Gesundheit; Careum Stiftung: Zürich, Switzerland, 2021. [Google Scholar]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaeffer, D.; Berens, E.M.; Gille, S.; Griese, L.; Klinger, J.; de Sombre, S.; Vogt, D.; Hurrelmann, K. Gesundheitskompetenz Der Bevölkerung in Deutschland Vor und Während Der Corona Pandemie: Ergebnisse Des HLS-GER 2; Universität Bielefeld, Interdisziplinäres Zentrum für Gesundheitskompetenzforschung: Bielefeld, Germany, 2021. [Google Scholar]
- HLS-EU Consortium. Comparative Report on Health Literacy in Eight EU Member States: The European Health Literacy Survey HLS-EU: (Second Extended and Revised Version, Date 22 July 2014). 2012. Available online: https://cdn1.sph.harvard.edu/wp-content/uploads/sites/135/2015/09/neu_rev_hls-eu_report_2015_05_13_lit.pdf (accessed on 29 November 2021).
- Bieri, U.; Kocher, J.P.; Gauch, C.; Tschöppe, S.; Venetz, A.; Hagemann, M.; Schwab, J.L.; Schüpbach, S.; Frind, A. Bevölkerungsbefragung “Erhebung Gesundheits-Kompetenz 2015”: Schlussbericht; Studie im Auftrag Des Bundesamt für Gesundheit BAG, Abteilung Gesundheitsstrategien. 2016. Available online: https://www.bag.admin.ch/dam/bag/de/dokumente/nat-gesundheitspolitik/gesundheitskompetenz/erhebung-gesundheitskompetenz-schweiz.pdf.download.pdf/erhebung-gesundheitskompetenz-chweiz.pdf (accessed on 29 November 2021).
- Schneider, M.; Jaks, R.; Nowak-Flück, D.; Nicca, D.; de Gani, S.M. Mental Health Literacy in Zurich: A First Measurement Attempt Using the General HLS-EU-Q47. Front. Public Health 2021, 9, 723900. [Google Scholar] [CrossRef] [PubMed]
- Vogt, D.; Gehrig, S.M. Bedeutung und Stärkung von Gesundheitskompetenz/Health Literacy in Der Prävention und Gesundheitsförderung. In Prävention und Gesundheitsförderung; Tiemann, M., Mohokum, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 1–11. [Google Scholar]
- Sørensen, K.; Broucke, S.V.D.; Pelikan, J.M.; Fullam, J.; Doyle, G.; Slonska, Z.; Kondilis, B.; Stoffels, V.; Osborne, R.H.; Brand, H. Measuring health literacy in populations: Illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health 2013, 13, 948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bundesamt für Statistik (BfS). Ständige und Nichtständige Wohnbevölkerung Nach Institutionellen Gliederungen, Staatsangehörigkeit (Kategorie), Geschlecht und Alter: Bundesamt für Statistik. 2020. Available online: https://www.pxweb.bfs.admin.ch/pxweb/de/px-x-0102010000_101/-/px-x-0102010000_101.px/ (accessed on 25 October 2021).
- Bundesamt für Statistik (BfS). Ständige Wohnbevölkerung Ab 15 Jahren Nach Höchster Abgeschlossener Ausbildung und Kanton: Bundesamt für Statistik. 2018. Available online: https://www.bfs.admin.ch/bfs/de/home/statistiken/kataloge-datenbanken/tabellen.assetdetail.4242914.html (accessed on 25 October 2021).
- Hurrelmann, K.; Klinger, J.; Schaeffer, D. Gesundheitskompetenz Der Bevölkerung in Deutschland: Vergleich Der Erhebungen 2014 und 2020; Universität Bielefeld, Interdisziplinäres Zentrum für Gesundheitskompetenzforschung: Bielefeld, Germany, 2020. [Google Scholar]
- Nutbeam, D.; Lloyd, J.E. Understanding and Responding to Health Literacy as a Social Determinant of Health. Annu. Rev. Public Health 2021, 42, 159–173. [Google Scholar] [CrossRef] [PubMed]
- Schillinger, D. The Intersections Between Social Determinants of Health, Health Literacy, and Health Disparities. Stud. Health Technol. Inform. 2020, 269, 22–41. [Google Scholar] [PubMed]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S.; Commission on Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Kickbusch, I.; Pelikan, J.M.; Apfel, F.; Agis, D.T. Health Literacy: The Solid Facts; World Health Organization: Geneva, Switzerland, 2013; ISBN 978-92-890-00154. Available online: https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf (accessed on 29 November 2021).
- Ganahl, K.; Röthlin, F.; Pelikan, J.M. Die Gesundheitskompetenz Der Österreichischen Bevölkerung: Nach Bundesländern und im Internationalen Vergleich; Fonds Gesundes Österreich; MSD Be Well; Executive Agency for Health and Consumers; Ludwig Boltzmann Gesellschaft GmbH: Vienna, Austria, 2013. [Google Scholar]
- Griebler, R.; Straßmayr, C.; Mikšová, D.; Link, T.; Nowak, P. Gesundheitskompetenz in Österreich: Ergebnisse Der Österreichischen Gesundheitskompetenzerhebung HLS19-AT. Wien: Bundesministerium für Soziales, Gesundheit, Pflege und Konsumentenschutz. 2021. Available online: https://jasmin.goeg.at/1833/ (accessed on 29 November 2021).
- Palumbo, R.; Annarumma, C.; Adinolfi, P.; Musella, M.; Piscopo, G. The Italian Health Literacy Project: Insights from the Assessment of Health Literacy Skills in Italy. Health Policy 2016, 120, 1087–1094. [Google Scholar] [CrossRef]
- Pelikan, J.M.; Röthlin, F.; Ganahl, K. Die Gesundheitskompetenz Der Österreichischen Bevölkerung—Nach Bundesländern und im Internationalen Vergleich. Abschlussbericht der Österreichischen Gesundheitskompetenz (Health Literacy) Bundesländer-Studie; Abschlussbericht der Österreichichen Gesundheitskompetenz (Health Literacy) Bundesländerstudie. 2013. Available online: https://fgoe.org/sites/fgoe.org/files/project-attachments/Gesundheitskompetenz_Bundesl%C3%A4nder_%C3%96ffentlich.pdf (accessed on 29 November 2021).
- Buja, A.; Rabensteiner, A.; Sperotto, M.; Grotto, G.; Bertoncello, C.; Cocchio, S.; Baldovin, T.; Contu, P.; Lorini, C.; Baldo, V. Health Literacy and Physical Activity: A Systematic Review. J. Phys. Act. Health 2020, 17, 1259–1274. [Google Scholar] [CrossRef]
- Dewalt, D.A.; Berkman, N.D.; Sheridan, S.; Lohr, K.N.; Pignone, M.P. Literacy and health outcomes: A systematic review of the literature. J. Gen. Intern. Med. 2004, 19, 1228–1239. [Google Scholar] [CrossRef]
- Kickbusch, I. Health literacy: An essential skill for the twenty-first century. Health Educ. 2008, 108, 101–104. [Google Scholar] [CrossRef]
- Nutbeam, D. Discussion Paper on Promoting, Measuring and Implementing Health Literacy: Implications for Policy and Practice in Non-Communicable Disease Prevention and Control; WHO GCM/NCD Working Group: Geneva, Switzerland, 2017; pp. 1–29. [Google Scholar]
- Geboers, B.; Reijneveld, S.A.; Koot, J.A.R.; de Winter, A.F. Moving towards a Comprehensive Approach for Health Literacy Interventions: The Development of a Health Literacy Intervention Model. Int. J. Envron. Res. Public Health 2018, 15, 1268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Total (n = 1000) % (n) | |
|---|---|
| Gender | |
| Female | 51% (507) |
| Male | 49% (493) |
| Age | |
| 18–39 | 37% (374) |
| 40–64 | 42% (420) |
| 65+ | 21% (206) |
| Education | |
| Low | 7% (72) |
| Medium | 74% (739) |
| High | 19% (189) |
| Migration background | |
| Yes | 40% (398) |
| No | 60% (602) |
| Type of settlement | |
| Rural | 5% (50) |
| Small/mid-sized city | 16% (160) |
| Big city | 79% (790) |
| Self-perceived social status | |
| Until lower intermediate | 37% (374) |
| Intermediate | 35% (349) |
| From upper intermediate | 27% (270) |
| Financial deprivation | |
| Very low | 16% (163) |
| Low | 17% (166) |
| Middle | 19% (192) |
| High | 8% (76) |
| Very high | 38% (369) |
| Excellent | Sufficient | Problematic | Inadequate | |
|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | |
| Gender (n = 996) | ||||
| Male (n = 490) | 2% (11) | 44% (210) | 45% (241) | 8% (28) |
| Female (n = 506) | 6% (17) | 36% (196) | 53% (269) | 5% (24) |
| Age (n = 996) | ||||
| 18–39 (n = 373) | 2% (6) | 47% (173) | 47% (183) | 5% (11) |
| 40–64 (n = 419) | 6% (17) | 43% (188) | 49% (209) | 1% (5) |
| 65+ (n = 204) | 3% (5) | 21% (45) | 55% (118) | 22% (36) |
| Education (n = 996) | ||||
| Low (n = 71) | 2% (1) | 26% (19) | 55% (39) | 17% (12) |
| Medium (n = 736) | 2% (13) | 40% (293) | 54% (396) | 5% (34) |
| High (n = 189) | 8% (14) | 49% (94) | 40% (75) | 3% (6) |
| Migration background (n = 996) | ||||
| Yes (n = 397) | 4% (11) | 36% (155) | 51% (206) | 9% (25) |
| No (n = 599) | 4% (17) | 43% (251) | 48% (304) | 5% (27) |
| Type of settlement (n = 996) | ||||
| Rural (n = 50) | 0% (0) | 26% (13) | 70% (36) | 4% (1) |
| Small/mid-sized city (n = 160) | 6% (7) | 35% (59) | 51% (84) | 8% (10) |
| Big city (n = 786) | 4% (21) | 42% (334) | 48% (390) | 7% (41) |
| Self-perceived social status (n = 989) | ||||
| Until lower intermediate (n = 371) | 2% (7) | 29% (115) | 55% (215) | 13% (34) |
| Intermediate (n = 348) | 1% (5) | 47% (155) | 48% (175) | 4% (13) |
| From upper intermediate (n = 270) | 7% (16) | 46% (134) | 44% (115) | 3% (5) |
| Financial deprivation (n = 962) | ||||
| Very low (n = 161) | 12% (18) | 51% (87) | 36% (54) | 2% (2) |
| Low (n = 166) | 6% (5) | 65% (115) | 26% (41) | 3% (5) |
| Middle (n = 192) | 2% (3) | 40% (77) | 55% (107) | 3% (5) |
| High (n = 76) | 1% (2) | 30% (26) | 59% (44) | 10% (4) |
| Very high (n = 367) | 0% (0) | 24% (92) | 63% (240) | 13% (35) |
| Health-Literacy-Index and… | ρ |
|---|---|
| Gender | −0.023 |
| Age | −0.209 * |
| Education | 0.260 * |
| Financial deprivation | −0.408 * |
| Self-perceived social status | 0.288 * |
| Migration background | −0.077 * |
| Health-Literacy-Index and… | β |
|---|---|
| Gender | 0.056 |
| Age | −0.119 ** |
| Education | 0.128 ** |
| Financial deprivation | −0.290 ** |
| Self-perceived social status | 0.078 * |
| Migration background | −0.26 |
| Adjusted R2 | 0.203 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guggiari, E.; Jaks, R.; Berger, F.M.P.; Nicca, D.; De Gani, S.M. Health Literacy in the Canton of Zurich: First Results of a Representative Study. Int. J. Environ. Res. Public Health 2021, 18, 12755. https://doi.org/10.3390/ijerph182312755
Guggiari E, Jaks R, Berger FMP, Nicca D, De Gani SM. Health Literacy in the Canton of Zurich: First Results of a Representative Study. International Journal of Environmental Research and Public Health. 2021; 18(23):12755. https://doi.org/10.3390/ijerph182312755
Chicago/Turabian StyleGuggiari, Elena, Rebecca Jaks, Fabian Marc Pascal Berger, Dunja Nicca, and Saskia Maria De Gani. 2021. "Health Literacy in the Canton of Zurich: First Results of a Representative Study" International Journal of Environmental Research and Public Health 18, no. 23: 12755. https://doi.org/10.3390/ijerph182312755






