Predictive Factors of Short-Term Related Musculoskeletal Pain in the Automotive Industry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Self-Reported Musculoskeletal Pain
2.4. Biomechanical Risk Factors
2.4.1. Posture
Posture—Percentage of Cycle Time
2.4.2. Force
2.5. Demographic Data
2.6. Statistical Analysis
3. Results
3.1. Sample Characteristics and Exposure
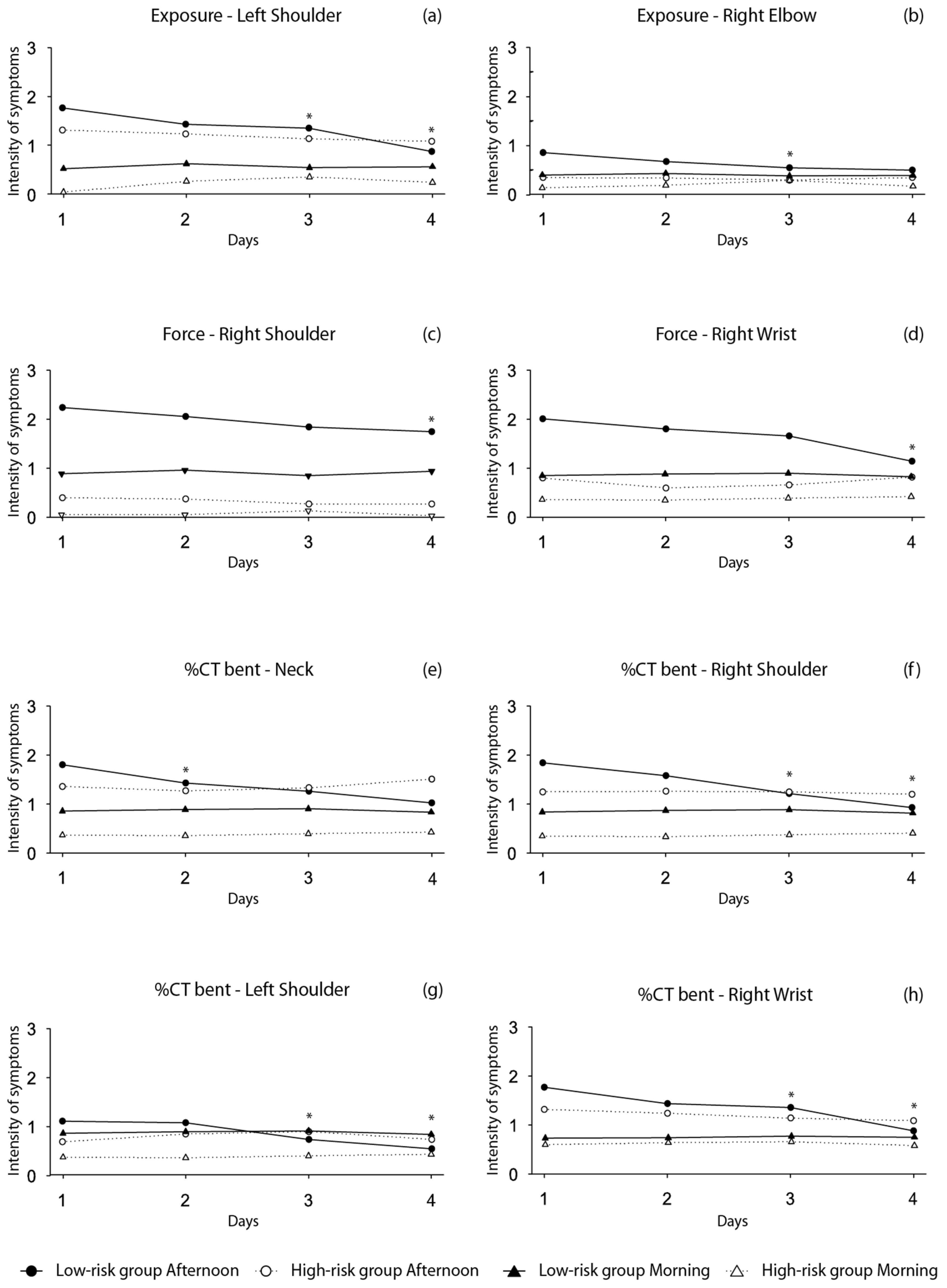
3.2. Musculoskeletal Symptoms Tendency according to Work Exposure
3.3. Predictive Models of Musculoskelatal Pain
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Kok, J.; Vroonhof, P.; Snijders, J.; Roullis, G.; Clarke, M.; Peereboom, K.; van Dorst, P.; Isusi, I. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics in the EU; European Agency for Safety and Health at Work: Bilbao, Spain, 2019; ISBN 9789294791450.
- Zare, M.; Malinge-Oudenot, A.; Höglund, R.; Biau, S.; Roquelaure, Y. Evaluation of ergonomic physical risk factors in a truck manufacturing plant:case study in SCANIA Production Angers. Ind. Health 2016, 54, 163. [Google Scholar] [CrossRef] [Green Version]
- Spallek, M.; Kuhn, W.; Uibel, S.; Van Mark, A.; Quarcoo, D. Work-related musculoskeletal disorders in the automotive industry due to repetitive work—Implications for rehabilitation. J. Occup. Med. Toxicol. 2010, 5, 6. [Google Scholar] [CrossRef] [Green Version]
- Ohlander, J.; Keskin, M.C.; Weiler, S.W.; Stork, J.; Radon, K. Snap-fit assembly and upper limb functional limitations in automotive production workers: A nested case-control study. Int. Arch. Occup. Environ. Health 2019, 92, 813–819. [Google Scholar] [CrossRef]
- Punnett, L. Ergonomic stressors and upper extremity disorders in vehicle manufacturing: Cross sectional exposure-response trends. Occup. Environ. Med. 1998, 55, 414–420. [Google Scholar] [CrossRef] [Green Version]
- Punnett, L.; Wegman, D.H. Work-related musculoskeletal disorders: The epidemiologic evidence and the debate. J. Electromyogr. Kinesiol. 2004, 14, 13–23. [Google Scholar] [CrossRef]
- Winkel, J.; Mathiassen, S.E. Assessment of physical work load in epidemiologic studies: Concepts, issues and operational considerations. Ergonomics 1994, 37, 979–988. [Google Scholar] [CrossRef] [PubMed]
- Visser, B.; Van Dieën, J.H. Pathophysiology of upper extremity muscle disorders. J. Electromyogr. Kinesiol. 2006, 16, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Nordander, C.; Hansson, G.Å.; Ohlsson, K.; Arvidsson, I.; Balogh, I.; Strömberg, U.; Rittner, R.; Skerfving, S. Exposure-response relationships for work-related neck and shoulder musculoskeletal disorders--Analyses of pooled uniform data sets. Appl. Ergon. 2016, 55, 70–84. [Google Scholar] [CrossRef] [PubMed]
- Bernard, B.P. Musculoskeletal Disorders and Workplace Factors. A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back; National Institute for Occupational Safety and Health (NIOSH): Cincinnati, OH, USA, 1997.
- Neupane, S.; Leino-Arjas, P.; Nygård, C.H.; Oakman, J.; Virtanen, P. Developmental pathways of multisite musculoskeletal pain: What is the influence of physical and psychosocial working conditions? Occup. Environ. Med. 2017, 74, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Coggon, D.; Ntani, G.; Palmer, K.T.; Felli, V.E.; Harari, R.; Barrero, L.H.; Felknor, S.A.; Gimeno, D.; Cattrell, A.; Serra, C.; et al. Disabling musculoskeletal pain in working populations: Is it the job, the person, or the culture? Pain 2013, 154, 856–863. [Google Scholar] [CrossRef] [Green Version]
- Da Costa, B.R.; Vieira, E.R. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. Am. J. Ind. Med. 2010, 53, 285–323. [Google Scholar] [CrossRef] [PubMed]
- Hallman, D.M.; Holtermann, A.; Dencker-Larsen, S.; Jørgensen, M.B.; Rasmussen, C.D.N. Are trajectories of neck-shoulder pain associated with sick leave and work ability in workers? A 1-year prospective study. BMJ Open 2019, 9, e022006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guerreiro, M.M.; Serranheira, F.; Cruz, E.B.; Sousa-Uva, A. Self-Reported Variables as Determinants of Upper Limb Musculoskeletal Symptoms in Assembly Line Workers. Saf. Health Work 2020, 11, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Thi Thu Tran, T.; Thi Thuy Phan, C.; Cong Pham, T.; Thuy Nguyen, Q. After-shift Musculoskeletal Disorder Symptoms in Female Workers and Work-related Factors: A Cross-sectional Study in a Seafood Processing Factory in Vietnam. AIMS Public Health 2016, 3, 733–749. [Google Scholar] [CrossRef] [PubMed]
- Van der Beek, A.J.; Frings-Dresen, M.H. Assessment of mechanical exposure in ergonomic epidemiology. Occup. Environ. Med. 1998, 55, 291–299. [Google Scholar] [CrossRef] [Green Version]
- Stigmar, K.G.E.; Petersson, I.F.; Jöud, A.; Grahn, B.E.M. Promoting work ability in a structured national rehabilitation program in patients with musculoskeletal disorders: Outcomes and predictors in a prospective cohort study. BMC Musculoskelet. Disord. 2013, 14, 57. [Google Scholar] [CrossRef] [Green Version]
- Charan, J.; Biswas, T. How to calculate sample size for different study designs in medical research? Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef] [Green Version]
- Jensen, M.P.; Karoly, P.; Braver, S. The measurement of clinical pain intensity: A comparison of six methods. Pain 1986, 27, 117–126. [Google Scholar] [CrossRef]
- Schaub, K.; Caragnano, G.; Britzke, B.; Bruder, R. The European Assembly Worksheet. Theor. Issues Ergon. Sci. 2013, 14, 616–639. [Google Scholar] [CrossRef]
- National Institute for Occupational Safety and Health. Ergonomic Guidelines for Manual Material Handling; National Institute for Occupational Safety and Health: Cincinnati, OH, USA, 2007.
- Ballinger, G.A. Using Generalized Estimating Equations for Longitudinal Data Analysis. Organ. Res. Methods 2004, 7, 127–150. [Google Scholar] [CrossRef]
- Lipsitz, S.R.; Fitzmaurice, G.M.; Orav, E.J.; Laird, N.M. Performance of Generalized Estimating Equations in Practical Situations. Biometrics 1994, 50, 270. [Google Scholar] [CrossRef] [PubMed]
- National Research Council; Institute of Medicine. Musculoskeletal Disorders and the Workplace: Low Back and Upper Extremities; The National Academies Press: Washington, DC, USA, 2001; ISBN 978-0-309-07284-7. [Google Scholar]
- Hoogendoorn, W.E.; Van Poppel, M.N.M.; Bongers, P.M.; Koes, B.W.; Bouter, L.M. Physical load during work and leisure time as risk factors for back pain. Scand. J. Work. Environ. Health 1999, 25, 387–403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Windt, D.; Thomas, E.; Pope, D.; Winter, A.; Macfarlane, G.; Bouter, L.; Silman, A.J. Occupational risk factors for shoulder pain: A systematic review. Occup. Environ. Med. 2000, 57, 433–442. [Google Scholar] [CrossRef] [Green Version]
- Heuvel, S.G.; Beek, A.J.; Blatter, B.M.; Bongers, P.M. Do work-related physical factors predict neck and upper limb symptoms in office workers? Int. Arch. Occup. Environ. Health 2006, 79, 585–592. [Google Scholar] [CrossRef] [Green Version]
- Christensen, J.O.; Knardahl, S. Work and neck pain: A prospective study of psychological, social, and mechanical risk factors. Pain 2010, 151, 162–173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silverstein, B.A.; Fine, L.J.; Armstrong, T.J. Hand wrist cumulative trauma disorders in industry. Br. J. Ind. Med. 1986, 43, 779–784. [Google Scholar] [CrossRef] [Green Version]
- Bláfoss, R.; Aagaard, P.; Andersen, L.L. Physical and psychosocial work environmental risk factors of low-back pain: Protocol for a 1 year prospective cohort study. BMC Musculoskelet. Disord. 2019, 20, 626. [Google Scholar] [CrossRef]
- Andersen, L.L.; Fallentin, N.; Ajslev, J.Z.N.; Jakobsen, M.D.; Sundstrup, E. Association between occupational lifting and day-to-day change in low-back pain intensity based on company records and text messages. Undefined 2017, 43, 68–74. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, C.A.; Manno, M.; Hogg-Johnson, S.; Haines, T.; Hurley, L.; McKenzie, D.; Beaton, D.E. Prognosis in Soft Tissue Disorders of the Shoulder: Predicting Both Change in Disability and Level of Disability after Treatment. Phys. Ther. 2006, 86, 1013–1032. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krebs, E.E.; Carey, T.S.; Weinberger, M. Accuracy of the Pain Numeric Rating Scale as a Screening Test in Primary Care. J. Gen. Intern. Med. 2007, 22, 1453–1461. [Google Scholar] [CrossRef] [Green Version]
- Sluiter, J.K.; Rest, K.M.; Frings-Dresen, M.H.W. Criteria document for evaluating the work-relatedness of upper-extremity musculoskeletal disorders. Scand. J. Work. Environ. Health 2001, 27, 1–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Podsakoff, P.M.; Mackenzie, S.B.; Lee, J.; Podsakoff, N.P. Common Method Biases in Behavioral Research: A Critical Review of the Literature and Recommended Remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef] [PubMed]

| Exposure | Posture | Force | %CT Shoulder | %CT Bent | Total Sample (n = 228) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Risk (n = 152) | High Risk (n = 76) | Low Risk (n = 152) | High Risk (n = 76) | Low Risk (n = 152) | High Risk (n = 76) | Low Risk (n = 152) | High Risk (n = 76) | Low Risk (n = 152) | High Risk (n = 76) | ||
| Age (years) | 30.3 ± 7.4 | 29.7 ± 6.5 | 30.4 ± 7.3 | 29.4 ± 6.7 | 30.1 ± 6.8 | 29.8 ± 7.6 | 29.7 ± 6.9 | 30.7 ± 7.4 | 30.2 ± 7.2 | 29.6 ± 6.9 | 30.0 ± 7.1 |
| Seniority (years) | 2.3 ± 4.5 | 1.2 ± 1.6 * | 2.9 ± 4.4 | 1.3 ± 2.2 * | 2.0 ± 3.9 | 1.8 ± 3.6 | 1.9 ± 3.9 | 2.0 ± 3.7 | 2.1 ± 4.0 | 1.6 ± 3.4 | 2.0 ± 3.8 |
| Gender (% female) | 39.1 | 40.8 | 39.5 | 39.5 | 38.4 | 42.1 | 44.1 | 30.3 | 36.8 | 44.7 | 39.5 |
| Pain at the Beginning of the Shift | |||||
|---|---|---|---|---|---|
| Exposure | Posture | Force | %CT Shoulder | %CT Bent | |
| Body Regions | High Risk * Low Risk β (95%CI) | High Risk * Low Risk β (95%CI) | High Risk * Low Risk β (95%CI) | High Risk * Low Risk β (95%CI) | High Risk * Low Risk β (95%CI) |
| Neck | 0.010 (−0.103–0.123) | 0.089 (−0.015–0.193) | −0.049 (−0.156–0.058) | −0.046 (−0.172–0.081) | 0.028 (−0.085–0.141) |
| Low Back | 0.020 (−0.112–0.152) | 0.124 (−0.001–0.249) | 0.007 (−0.106–0.120) † | −0.002 (−0.147–0.143) | 0.044 (−0.084–0.173) |
| Right Shoulder | 0.010 (−0.107–0.126) | 0.093 (−0.021–0.208) | 0.013 (−0.085–0.111) † | −0.047 (−0.178–0.084) | 0.014 (−0.107–0.136) |
| Left Shoulder | 0.055 (−0.010–0.119) † | 0.053 (0.002–0.104) *,† | −0.033 (−0.097–0.030) † | 0.035 (−0.035–0.104) | 0.054 (−0.021–0.129) |
| Right Elbow | 0.018 (−0.036–0.072) | 0.013 (−0.042–0.067) | 0.012 (−0.039–0.064) | 0.011 (−0.042–0.064) | −0.010 (−0.070–0.050) |
| Left elbow | 0.040 (−0.009–0.089) † | 0.026 (−0.014–0.067) † | 0.018 (−0.036–0.072) | 0.000 (−0.054–0.054) | −0.015 (−0.083–0.054) |
| Right wrist | 0.008 (−0.116–0.106) | 0.050 (−0.058–0.159) | 0.068 (−0.017–0.153) † | −0.029 (−0.149–0.091) | 0.035 (−0.075–0.144) |
| Left wrist | −0.012 (−0.091–0.068) | 0.064 (−0.019–0.147) | −0.009 (−0.087–0.070) | 0.006 (−0.081–0.093) | 0.017 (−0.068–0.102) |
| Right hand/fingers | 0.005 (−0.107–0.117) | 0.038 (−0.075–0.1519 | −0.027 (−0.130–0.076) | −0.050 (−0.177–0.076) | 0.003 (−0.112–0.118) |
| Left hand/fingers | 0.002 (−0.091–0.094) | 0.025 (−0.039–0.089) | −0.019 (−0.103–0.064) | −0.040 (−0.147–0.067) | 0.051 (−0.046–0.147) |
| Pain at the End of the Shift | |||||
| Exposure | Posture | Force | %CT Shoulder | %CT Bent | |
| Body Regions | High Risk * Low Risk β (95%CI) | High Risk * Low Risk β (95%CI) | High Risk * Low Risk β (95%CI) | High Risk * Low Risk β (95%CI) | High Risk * Low Risk β (95%CI) |
| Neck | 0.002 (−0.150–0.154) | 0.218 (0.067–0.368) * | −0.002 (−0.129–0.126) † | 0.015 (−0.131–0.162) | 0.113 (−0.041–0.267) |
| Low Back | 0.063 (−0.107–0.233) | 0.143 (−0.026–0.311) | 0.108 (−0.036–0.252) † | −0.008 (−0.180–0.164) | 0.054 (−0.111–0.220) |
| Right Shoulder | −0.027 (−0.169–0.115) † | 0.092 (−0.060–0.245) | 0.030 (−0.106–0.167) † | 0.030 (−0.127–0.188) | 0.080 (−0.066–0.227) |
| Left Shoulder | 0.140 (0.030–0.251) *,† | 0.221 (0.102–0.339) * | 0.004 (−0.108–0.117) † | 0.075 (−0.049–0.199) † | 0.136 (0.013–0.260) * |
| Right Elbow | 0.007 (−0.068–0.082) † | 0.055 (−0.042–0.152) | 0.015 (−0.057–0.088) † | −0.010 (−0.117–0.098) | 0.011 (−0.060–0.081) † |
| Left elbow | 0.031 (−0.040–0.102) † | 0.067 (−0.016–0.150) | 0.007 (−0.064–0.078) † | −0.008 (−0.092–0.077) | 0.016 (−0.071–0.102) |
| Right wrist | 0.005 (−0.131–0.141) | 0.020 (−0.114–0.153) | 0.107 (0.003–0.211) *,† | −0.050 (−0.191–0.090) | 0.084 (−0.049–0.218) |
| Left wrist | 0.056 (−0.071–0.183) | 0.103 (−0.029–0.235) | 0.081 (−0.041–0.203) | 0.039 (−0.107–0.186) | 0.065 (−0.060–0.191) |
| Right hand/fingers | −0.084 (−0.299–0.061) | −0.013 (−0.157–0.130) | −0.001 (−0.126–0.125) † | −0.046 (−0.199–0.107) | −0.094 (−0.239–0.052) |
| Left hand/finger | −0.062 (−0.175–0.050) | 0.051 (−0.070–0.172) | 0.047 (−0.057–0.150) † | −0.014 (−0.142–0.114) | 0.063 (−0.055–0.180) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assunção, A.; Moniz-Pereira, V.; Fujão, C.; Bernardes, S.; Veloso, A.P.; Carnide, F. Predictive Factors of Short-Term Related Musculoskeletal Pain in the Automotive Industry. Int. J. Environ. Res. Public Health 2021, 18, 13062. https://doi.org/10.3390/ijerph182413062
Assunção A, Moniz-Pereira V, Fujão C, Bernardes S, Veloso AP, Carnide F. Predictive Factors of Short-Term Related Musculoskeletal Pain in the Automotive Industry. International Journal of Environmental Research and Public Health. 2021; 18(24):13062. https://doi.org/10.3390/ijerph182413062
Chicago/Turabian StyleAssunção, Ana, Vera Moniz-Pereira, Carlos Fujão, Sarah Bernardes, António P. Veloso, and Filomena Carnide. 2021. "Predictive Factors of Short-Term Related Musculoskeletal Pain in the Automotive Industry" International Journal of Environmental Research and Public Health 18, no. 24: 13062. https://doi.org/10.3390/ijerph182413062
APA StyleAssunção, A., Moniz-Pereira, V., Fujão, C., Bernardes, S., Veloso, A. P., & Carnide, F. (2021). Predictive Factors of Short-Term Related Musculoskeletal Pain in the Automotive Industry. International Journal of Environmental Research and Public Health, 18(24), 13062. https://doi.org/10.3390/ijerph182413062







