Impact of COVID-19 Lockdown, during the Two Waves, on Drug Use and Emergency Department Access in People with Epilepsy: An Interrupted Time-Series Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Data Source and Ethical Approval
2.2. Study Population and Outcome
2.3. Statistical Analysis
3. Results
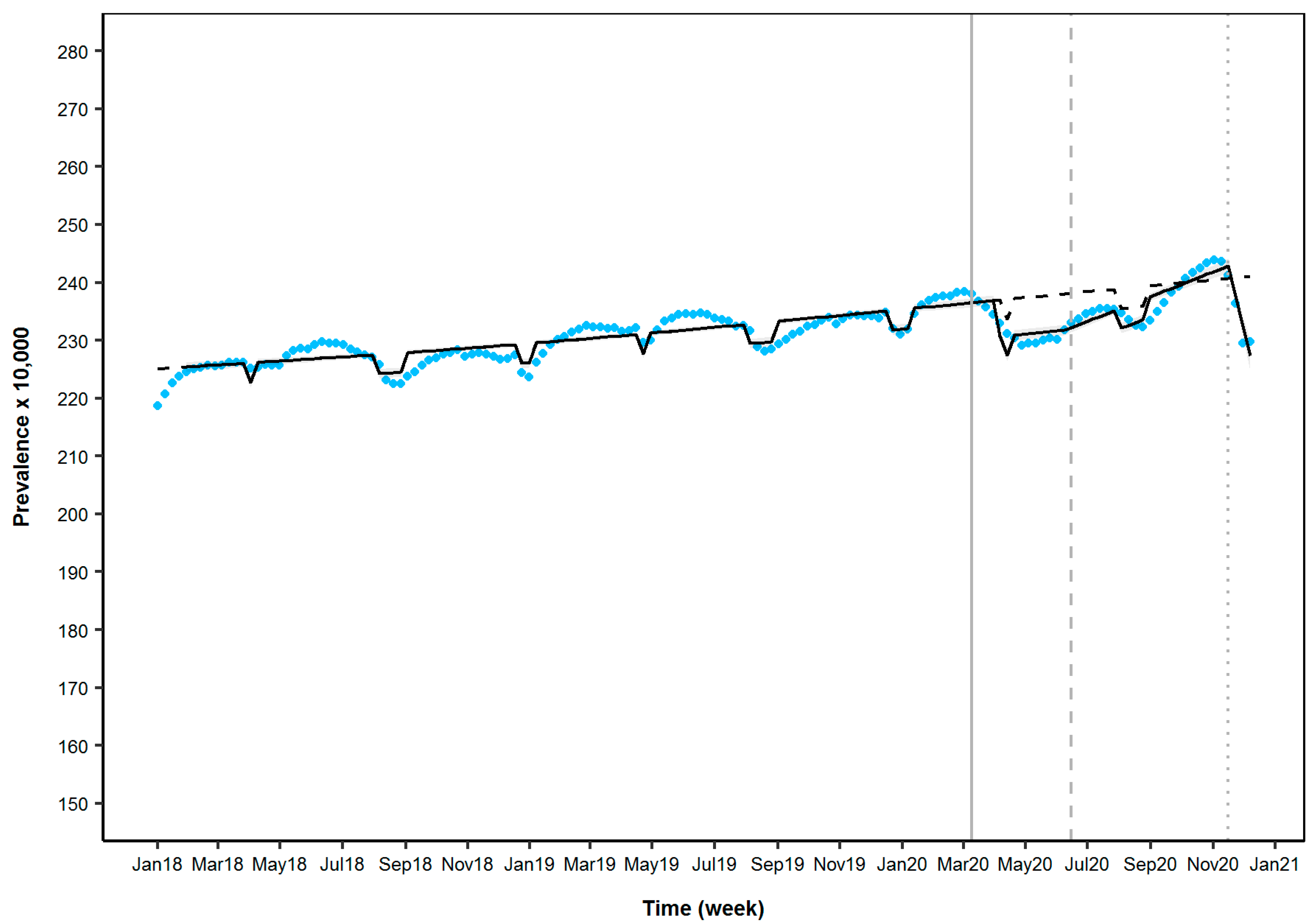
3.1. Prevalence of AEs Use
3.2. Incidence of AEs Use
3.3. Emergency Department Access
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Prevalence of AE Drug Use | ||||
|---|---|---|---|---|
| Significant Parameter 1 | Estimated β | Prevalence Ratio | 95%CI | p-Value |
| First Lockdown (4th week) 2 | −0.027 | 0.974 | 0.967–0.980 | <0.001 |
| Post-First Lockdown (1st week) 3 | 0.002 | 1.002 | 1.001–1.002 | <0.001 |
| Second Lockdown (1st week) 3 | −0.024 | 0.976 | 0.972–0.980 | <0.001 |
References
- Helmy, Y.A.; Fawzy, M.; Elaswad, A.; Sobieh, A.; Kenney, S.P.; Shehata, A.A. The COVID-19 Pandemic: A Comprehensive Review of Taxonomy, Genetics, Epidemiology, Diagnosis, Treatment, and Control. J. Clin. Med. 2020, 9, 1225. [Google Scholar] [CrossRef]
- Hasan, M.N.; Haider, N.; Stigler, F.L.; Khan, R.A.; McCoy, D.; Zumla, A.; Kock, R.A.; Uddin, J. The Global Case-Fatality Rate of COVID-19 Has Been Declining Since May 2020. Am. J. Trop. Med. Hyg. 2021, 104, 2176–2184. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Chen, Z.; Rychkova, M.; Dunne, J.; Lee, J.; Kalilani, L.; Lawn, N.; Kwan, P. Treatment initiation decisions in newly diagnosed epilepsy—A longitudinal cohort study. Epilepsia 2020, 61, 445–454. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2021. Available online: https://covid19.who.int/ (accessed on 31 January 2021).
- Official Gazette of the Italian Republic. DPCM 22 marzo 2020. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19, applicabili sull’intero territorio nazionale. n. 76 del 22 marzo 2020. 2020. Available online: http://www.governo.it/it/articolo/coronavirus-firmato-il-dpcm-22-marzo-2020/14363 (accessed on 3 January 2021).
- Cheli, M.; Dinoto, A.; Olivo, S.; Marinella, T.; Stokelj, D.; Cominotto, F.; Francesco, B.; Paolo, M. SARS-CoV-2 pandemic and epilepsy: The impact on emergency department attendances for seizures. Seizure 2020, 82, 23–26. [Google Scholar] [CrossRef]
- Beghi, E. The Epidemiology of Epilepsy. Neuroepidemiology 2020, 54, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.-L.; Hsu, M.-T.; Chen, S.-S. The impact of SARS on epilepsy: The experience of drug withdrawal in epileptic patients. Seizure 2005, 14, 557–561. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kobayashi, S.; Endo, W.; Inui, T.; Wakusawa, K.; Tanaka, S.; Onuma, A.; Haginoya, K. The lack of antiepileptic drugs and worsening of seizures among physically handicapped patients with epilepsy during the Great East Japan Earthquake. Brain Dev. 2016, 38, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Shibahara, I.; Osawa, S.-I.; Kon, H.; Morita, T.; Nakasato, N.; Tominaga, T.; Narita, N. Increase in the number of patients with seizures following the Great East-Japan Earthquake. Epilepsia 2013, 54, e49–e52. [Google Scholar] [CrossRef] [PubMed]
- Assenza, G.; Lanzone, J.; Brigo, F.; Coppola, A.; Di Gennaro, G.; Di Lazzaro, V.; Ricci, L.; Romigi, A.; Tombini, M.; Mecarelli, O. Epilepsy Care in the Time of COVID-19 Pandemic in Italy: Risk Factors for Seizure Worsening. Front. Neurol. 2020, 11, 737. [Google Scholar] [CrossRef]
- Sanchez-Larsen, A.; Gonzalez-Villar, E.; Díaz-Maroto, I.; Layos-Romero, A.; Martínez-Martín, Á.; Alcahut-Rodriguez, C.; Grande-Martin, A.; Sopelana-Garay, D. Influence of the COVID-19 outbreak in people with epilepsy: Analysis of a Spanish population (EPICOVID registry). Epilepsy Behav. 2020, 112, 107396. [Google Scholar] [CrossRef]
- Davico, C.; Marcotulli, D.; Lux, C.; Terrinoni, A.; Ferrara, M.; di Santo, F.; Ricci, F.; Vittorini, R.; Calderoni, D.; Amianto, F.; et al. Where have the children with epilepsy gone? An observational study of seizure-related accesses to emergency department at the time of COVID-19. Seizure 2020, 83, 38–40. [Google Scholar] [CrossRef]
- Cabona, C.; Deleo, F.; Marinelli, L.; Audenino, D.; Arnaldi, D.; Rossi, F.; Di Giacomo, R.; Buffoni, C.; Rosa, G.J.; Didato, G.; et al. Epilepsy course during COVID-19 pandemic in three Italian epilepsy centers. Epilepsy Behav. 2020, 112, 107375. [Google Scholar] [CrossRef]
- Giometto, S.; Baglietto, L.; Conte, M.; Vannacci, A.; Tuccori, M.; Mugelli, A.; Gini, R.; Lucenteforte, E. Use of antiseizure medications and safety of branded versus generic formulations: A comparative study on Tuscan administrative databases. Epilepsy Behav. 2021, 117, 107876. [Google Scholar] [CrossRef]
- Trifirò, G.; Gini, R.; Barone-Adesi, F.; Beghi, E.; Cantarutti, A.; Capuano, A.; Carnovale, C.; Clavenna, A.; Dellagiovanna, M.; Ferrajoo, C.; et al. The Role of European Healthcare Databases for Post-Marketing Drug Effective-ness, Safety and Value Evaluation: Where Does Italy Stand? Drug Saf. 2019, 42, 347–363. [Google Scholar] [CrossRef]
- Merlo, J.; Wessling, A.; Melander, A. Comparison of dose standard units for drug utilisation studies. Eur. J. Clin. Pharmacol. 1996, 50, 27–30. [Google Scholar] [CrossRef]
- Pazzagli, L.; Brandt, L.; Linder, M.; Myers, D.; Mavros, P.; Andersen, M.; Bahmanyar, S. Methods for constructing treatment episodes and impact on exposure-outcome associations. Eur. J. Clin. Pharmacol. 2019, 76, 267–275. [Google Scholar] [CrossRef] [Green Version]
- Italian Office of National Statistics—Istituto Nazionale di Statistica (ISTAT). Available online: https://www.istat.it/ (accessed on 6 June 2021).
- Kontopantelis, E.; Doran, T.; Springate, D.A.; Buchan, I.; Reeves, D. Regression based quasi-experimental approach when randomisation is not an option: Interrupted time series analysis. BMJ 2015, 350, h2750. [Google Scholar] [CrossRef] [Green Version]
- Penfold, R.B.; Zhang, F. Use of Interrupted Time Series Analysis in Evaluating Health Care Quality Improvements. Acad. Pediatr. 2013, 13, S38–S44. [Google Scholar] [CrossRef] [PubMed]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Derrick, T.R.; Thomas, J.M. Time Series Analysis: The Cross-Correlation Function. Kinesiology Publications 2004 at Iowa State University Digital Repository. Available online: https://lib.dr.iastate.edu/kin_pubs/46 (accessed on 6 May 2021).
- Antonazzo, I.C.; Fornari, C.; Paoletti, O.; Bartolini, C.; Conti, S.; Cortesi, P.A.; Mantovani, L.G.; Gini, R.; Mazzaglia, G. COVID-19 Outbreak Impact on Anticoagulants Utilization: An Interrupted Time-Series Analysis Using Health Care Administrative Databases. Thromb. Haemost. 2021, 121, 1115–1118. [Google Scholar] [CrossRef] [PubMed]
- Meyer, A.-C.L.; Dua, T.; Boscardin, W.J.; Escarce, J.J.; Saxena, S.; Birbeck, G.L.; Boscardin, J. Critical determinants of the epilepsy treatment gap: A cross-national analysis in resource-limited settings. Epilepsia 2012, 53, 2178–2185. [Google Scholar] [CrossRef] [Green Version]
- Sharma, R.; Agarwal, M.; Gupta, M.; Somendra, S.; Saxena, S.K. Clinical Characteristics and Differential Clinical Diagnosis of Novel Coronavirus Disease 2019 (COVID-19). Med. Virol. Pathog. Dis. Control 2020, 2019, 55–70. [Google Scholar] [CrossRef]
- Cross, J.H.; Kwon, C.-S.; Asadi-Pooya, A.A.; Balagura, G.; Gómez-Iglesias, P.; Guekht, A.; Hall, J.; Ikeda, A.; Kishk, N.A.; Murphy, P.; et al. Epilepsy care during the COVID-19 pandemic. Epilepsia 2021, 62, 2322–2332. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, K.; Hamano, S.; Horiguchi, A.; Nonoyama, H.; Hirata, Y.; Matsuura, R.; Koichihara, R.; Oka, A.; Hirano, D. Telemedicine in epilepsy management during the coronavirus disease 2019 pandemic. Pediatr. Int. 2021. [Google Scholar] [CrossRef]
- Kanner, A.M. Can Neurochemical Changes of Mood Disorders Explain the Increase Risk of Epilepsy or its Worse Seizure Control? Neurochem. Res. 2017, 42, 2071–2076. [Google Scholar] [CrossRef]
- Kovac, S.; Walker, M. Neuropeptides in epilepsy. Neuropeptides 2013, 47, 467–475. [Google Scholar] [CrossRef]
- Tolmacheva, E.A.; Oitzl, M.S.; van Luijtelaar, G. Stress, glucocorticoids and absences in a genetic epilepsy model. Horm. Behav. 2012, 61, 706–710. [Google Scholar] [CrossRef] [PubMed]
- Cano-López, I.; Gonzalez-Bono, E. Cortisol levels and seizures in adults with epilepsy: A systematic review. Neurosci. Biobehav. Rev. 2019, 103, 216–229. [Google Scholar] [CrossRef]
- Joëls, M. Stress, the hippocampus, and epilepsy. Epilepsia 2009, 50, 586–597. [Google Scholar] [CrossRef] [PubMed]
- Castro, O.W.; Santos, V.R.; Pun, R.Y.K.; McKlveen, J.M.; Batie, M.; Holland, K.D.; Gardner, M.; Garcia-Cairasco, N.; Herman, J.P.; Danzer, S.C. Impact of corticosterone treatment on spontaneous seizure frequency and epileptiform activity in mice with chronic epilepsy. PLoS ONE 2012, 7, e46044. [Google Scholar]
- Djamshidian, A.; Lees, A.J. Can stress trigger Parkinson’s disease? J. Neurol. Neurosurg Psychiatry 2014, 85, 878–881. [Google Scholar] [CrossRef]
- Jones, N.C.; Lee, H.E.; Yang, M.; Rees, S.M.; Morris, M.J.; O’Brien, T.J.; Salzberg, M.R. Repeatedly stressed rats have enhanced vulnerability to amygdala kindling epilepto-genesis. Psychoneuroendocrinology 2013, 38, 263–270. [Google Scholar] [CrossRef]
- Koe, A.S.; Salzberg, M.R.; Morris, M.J.; O’Brien, T.J.; Jones, N.C. Early life maternal separation stress augmentation of limbic ep-ileptogenesis: The role of corticosterone and HPA axis programming. Psychoneuroendocrinology 2014, 42, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Baldin, E.; Hauser, W.A.; Pack, A.; Hesdorffer, D.C. Stress is associated with an increased risk of recurrent seizures in adults. Epilepsia 2017, 58, 1037–1046. [Google Scholar] [CrossRef] [Green Version]
- Huang, S.; Wu, C.; Jia, Y.; Li, G.; Zhu, Z.; Lu, K.; Yang, Y.; Wang, F.; Zhu, S. COVID-19 outbreak: The impact of stress on seizures in patients with epilepsy. Epilepsia 2020, 61, 1884–1893. [Google Scholar] [CrossRef] [PubMed]
- Haut, S.R.; Vouyiouklis, M.; Shinnar, S. Stress and epilepsy: A patient perception survey. Epilepsy Behav. 2003, 4, 511–514. [Google Scholar] [CrossRef]
- Asadi-Pooya, A.A. Seizures associated with coronavirus infections. Seizure 2020, 79, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Asadi-Pooya, A.A.; Simani, L.; Shahisavandi, M.; Barzegar, Z. COVID-19, de novo seizures, and epilepsy: A systematic review. Neurol. Sci. 2021, 42, 415–431. [Google Scholar] [CrossRef]
- Glauser, T.; Shinnar, S.; Gloss, D.; Alldredge, B.; Arya, R.; Bainbridge, J.; Bare, M.; Bleck, T.; Dodson, W.E.; Garrity, L.; et al. Evidence-Based Guideline: Treatment of Convulsive Status Epilepticus in Children and Adults: Report of the Guideline Committee of the American Epilepsy Society. Epilepsy Curr. 2016, 16, 48–61. [Google Scholar] [CrossRef] [Green Version]
- Ochoa, J.G.; Kilgo, W.A. The Role of Benzodiazepines in the Treatment of Epilepsy. Curr. Treat. Options Neurol. 2016, 18, 18. [Google Scholar] [CrossRef]
- Kanner, A.M. Management of psychiatric and neurological comorbidities in epilepsy. Nat. Rev. Neurol. 2016, 12, 106–116. [Google Scholar] [CrossRef] [PubMed]
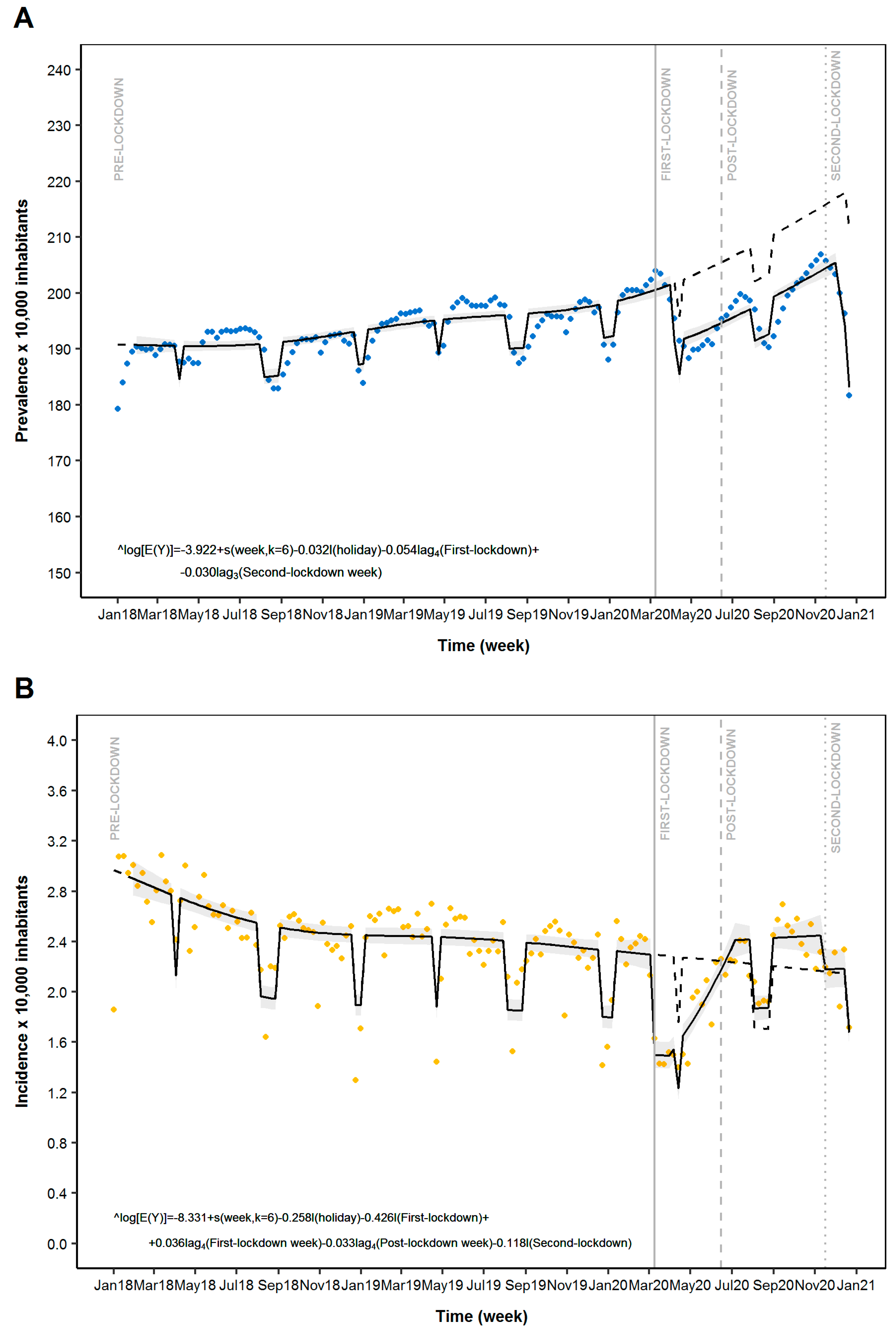

| Prevalence of ASM Use | ||||
|---|---|---|---|---|
| Model Parameter 1 | β | Prevalence Ratio | 95%CI | p-Value |
| First Lockdown (4th week) 3 | −0.054 | 0.947 | 0.935–0.960 | <0.001 |
| Second Lockdown (3rd week) 4 | −0.030 | 0.970 | 0.962–0.978 | <0.001 |
| Incidence of ASM Use | ||||
| Model parameter1 | β | Incidence Ratio | 95%CI | p-value |
| First Lockdown (1st week) 3 | −0.426 | 0.653 | 0.593–0.719 | <0.001 |
| First Lockdown (4th week) 4 | 0.036 | 1.037 | 1.027–1.046 | <0.001 |
| Post-Lockdown (4th week) 4 | −0.033 | 0.967 | 0.956–0.979 | <0.001 |
| Second Lockdown (1st week) 3 | −0.118 | 0.889 | 0.799–0.990 | 0.032 |
| Emergency Department access | ||||
| Model parameter 2 | β | Events Ratio | 95%CI | p-value |
| First Lockdown (1st week) 3 | −0.323 | 0.724 | 0.638–0.822 | <0.001 |
| Post-First Lockdown (1st week) 4 | 0.267 | 1.306 | 1.150–1.484 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antonazzo, I.C.; Fornari, C.; Maumus-Robert, S.; Cei, E.; Paoletti, O.; Conti, S.; Cortesi, P.A.; Mantovani, L.G.; Gini, R.; Mazzaglia, G. Impact of COVID-19 Lockdown, during the Two Waves, on Drug Use and Emergency Department Access in People with Epilepsy: An Interrupted Time-Series Analysis. Int. J. Environ. Res. Public Health 2021, 18, 13253. https://doi.org/10.3390/ijerph182413253
Antonazzo IC, Fornari C, Maumus-Robert S, Cei E, Paoletti O, Conti S, Cortesi PA, Mantovani LG, Gini R, Mazzaglia G. Impact of COVID-19 Lockdown, during the Two Waves, on Drug Use and Emergency Department Access in People with Epilepsy: An Interrupted Time-Series Analysis. International Journal of Environmental Research and Public Health. 2021; 18(24):13253. https://doi.org/10.3390/ijerph182413253
Chicago/Turabian StyleAntonazzo, Ippazio Cosimo, Carla Fornari, Sandy Maumus-Robert, Eleonora Cei, Olga Paoletti, Sara Conti, Paolo Angelo Cortesi, Lorenzo Giovanni Mantovani, Rosa Gini, and Giampiero Mazzaglia. 2021. "Impact of COVID-19 Lockdown, during the Two Waves, on Drug Use and Emergency Department Access in People with Epilepsy: An Interrupted Time-Series Analysis" International Journal of Environmental Research and Public Health 18, no. 24: 13253. https://doi.org/10.3390/ijerph182413253









