The Quality of Carer–Patient Relationship Scale: Adaptation and Validation into Portuguese
Abstract
:1. Introduction
2. Materials and Methods
2.1. Phase 1: Cultural Adaptation of the QCPR
2.2. Phase 2: Validation of the European Portuguese Version of the QCPR
2.2.1. Sample
2.2.2. Measurement Scales
2.2.3. Procedures
2.2.4. Ethical Considerations
2.2.5. Data Analysis
3. Results
3.1. Phase 1: Cultural Adaptation of the QCPR
3.2. Phase 2: Validation of the European Portuguese Version of the QCPR (QCPR-P)
3.2.1. QCPR-P Comprehensibility
3.2.2. QCPR-P Score
3.2.3. QCPR-P Internal Consistency
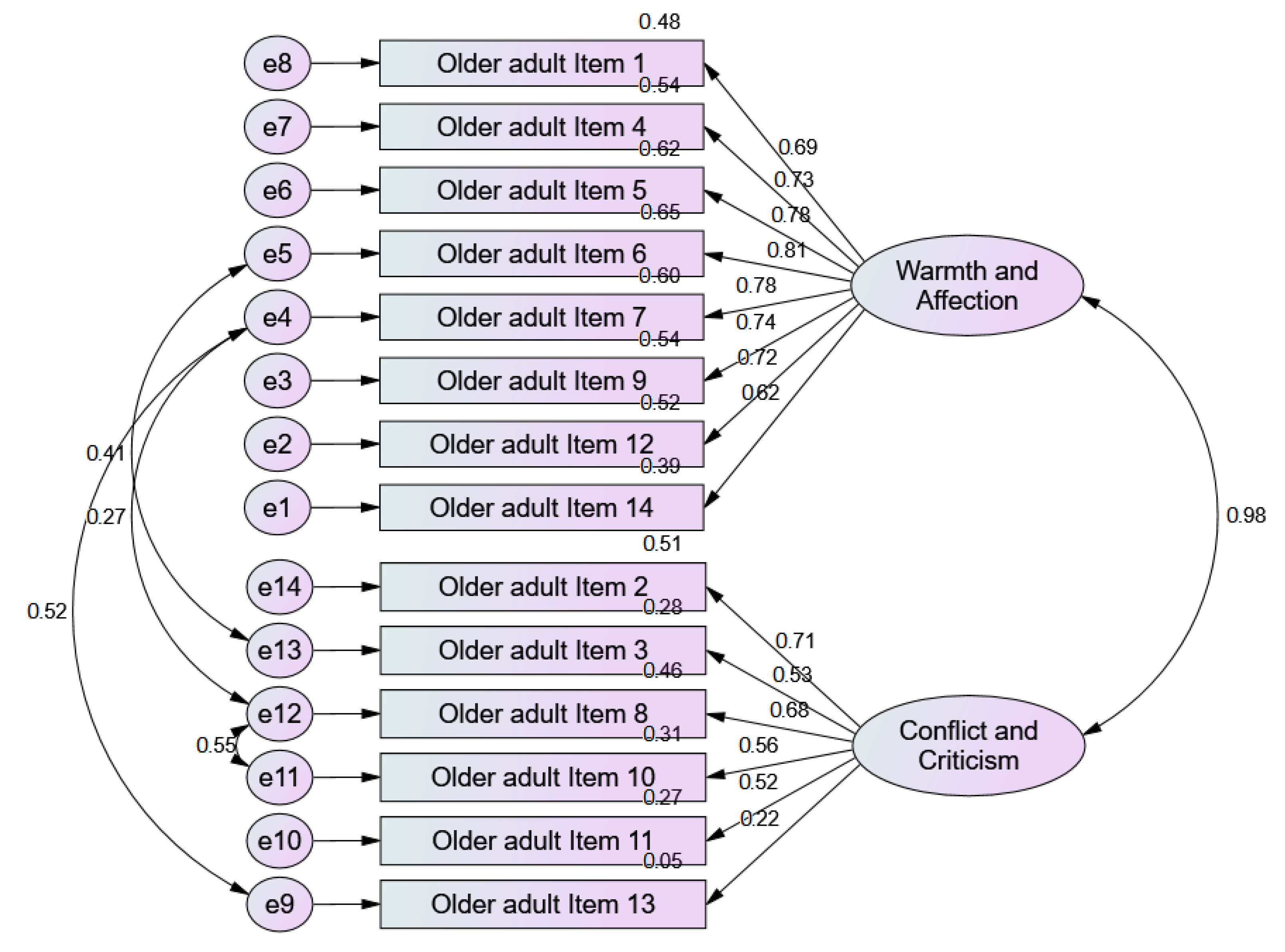
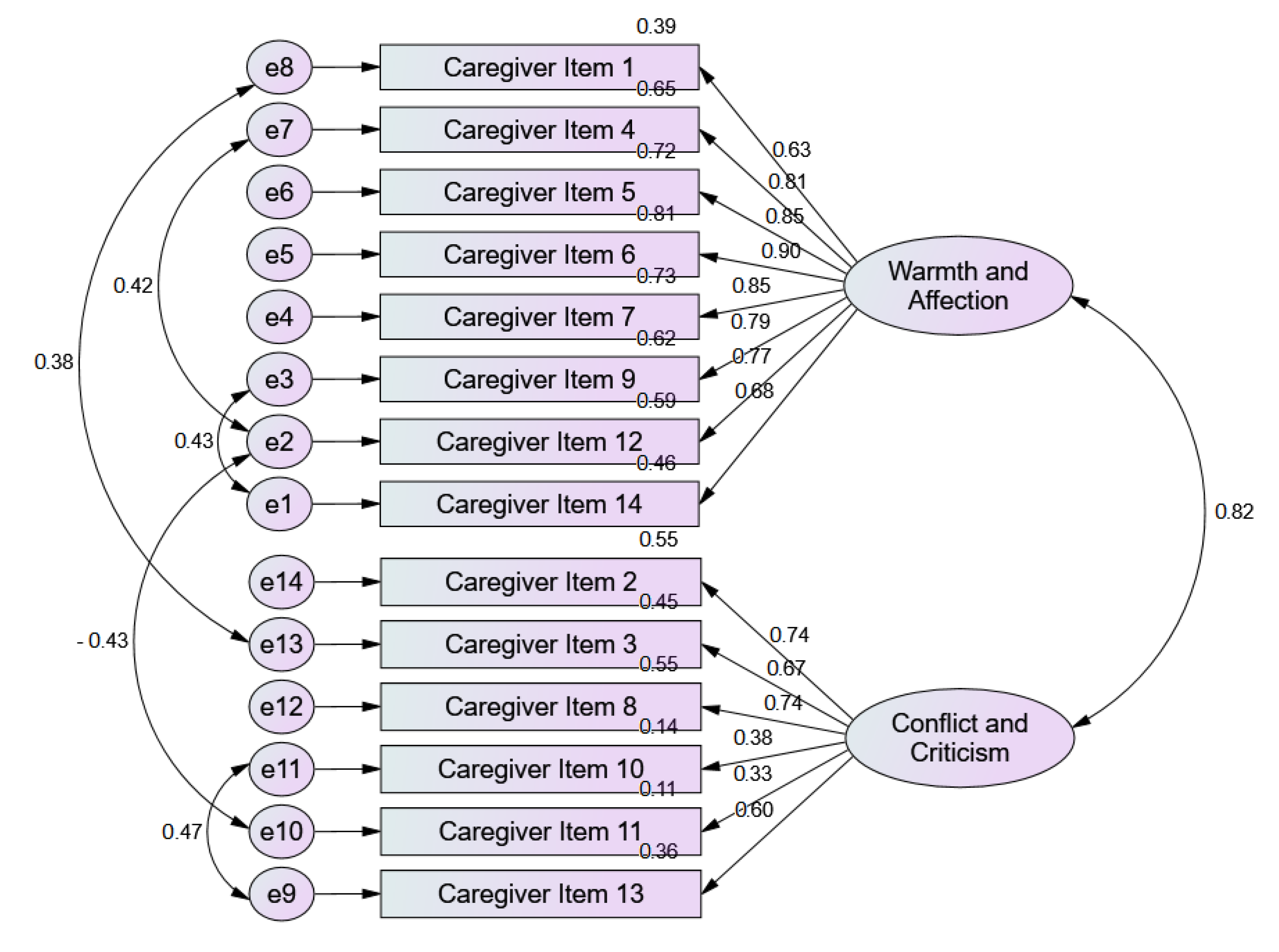
3.2.4. Overall Quality of Model Fit-QCPR-P
3.2.5. Composite Reliability
3.2.6. Construct Validity
3.2.7. Distribution of the QCPR-P Score in the Different Subgroups
3.2.8. Correlations between QCPR Score and Age
3.2.9. Correlations between the QCPR-P and Variables of Individual Functioning
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- European Commission. The 2018 Ageing Report: Economic & Budgetary Projections for the 28 EU Member States (2016 2070); Publications Office: Luxemburg, 2018. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Noel, M.A.; Kaluzynski, T.S.; Templeton, V.H. Quality Dementia Care. J. Appl. Gerontol. 2017, 36, 195–212. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, D.; Braun, A.; Dickinson, A.; Gage, H.; Hamilton, L.; Goodman, C.; Ashaye, K.; Iliffe, S.; Manthorpe, J. Managing behavioural and psychological symptoms in community dwelling older people with dementia: 1. A systematic review of the effectiveness of interventions. Dementia 2018, 18, 2925–2949. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Etters, L.; Goodall, D.; Harrison, B.E. Caregiver burden among dementia patient caregivers: A review of the literature. J. Am. Acad. Nurse Pr. 2008, 20, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Quinn, C.; Clare, L.; Woods, B. The impact of the quality of relationship on the experiences and wellbeing of caregivers of people with dementia: A systematic review. Aging Ment. Heal. 2009, 13, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Spruytte, N.; Audenhove, C.; Lammertyn, F.; Storms, G. The quality of the caregiving relationship in informal care for older adults with dementia and chronic psychiatric patients. Psychol. Psychother. Theory Res. Pr. 2002, 75, 295–311. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, B.; Spruytte, N.; Declercq, A. Zorgen Voor Een Kwetsbare, Thuiswonende Oudere: WarMte En Conflict in de Relatie Tussen Mantelzorgers En Ouderen. Tijdschr. Voor Welzijnsw. 2012, 36, 327. [Google Scholar]
- Nunes, D.P.; de Brito, T.R.P.; Duarte, Y.A.D.O.; Lebrão, M.L. Cuidadores de idosos e tensão excessiva associada ao cuidado: Evidências do Estudo SABE. Rev. Bras. Epidemiol. 2018, 21, e180020. [Google Scholar] [CrossRef] [Green Version]
- Vermeulen, B.; Declercq, A.; Spruytte, N. Met de Mantel Der Liefde? Over de Kwaliteit van de Relatie Tussen Kwetsbare Ouderen En Mantelzorgers. SWVG Feiten Cijfers 2011, 17, 1–7. [Google Scholar]
- Ribeiro, O.; Brandão, D.; Oliveira, A.F.; Martín, I.; Teixeira, L.; Paúl, C. The Modified Caregiver Strain Index: Portuguese version. J. Heal. Psychol. 2019. [Google Scholar] [CrossRef]
- Spruytte, N.; van Audenhove, C.; Lammertyn, F. Als Je Thuis Zorgt Voor Een Chronisch Ziek Familielid. Onderzoek over de Mantelzorg Voor Dementerende Ouderen En Voor Psychiatrische Patiënten; Garant: Leuven, Belgium, 2000. [Google Scholar]
- Spruytte, N.; van Audenhove, C.; Lammertyn, F. Predictors of institutionalization of cognitively-impaired elderly cared for by their relatives. Int. J. Geriatr. Psychiatry 2001, 16, 1119–1128. [Google Scholar] [CrossRef]
- Vermeulen, B.; Lauwers, H.; Spruytte, N.; van Audenhove, C. Experiences of family caregivers for persons with severe mental illness: An international exploration. Eur. Neuropsychopharmacol. 2015, 25, S374. [Google Scholar] [CrossRef]
- Orgeta, V.; Leung, P.; Yates, L.; Kang, S.; Hoare, Z.; Henderson, C.; Whitaker, C.; Burns, A.; Knapp, M.; Leroi, I.; et al. Individual cognitive stimulation therapy for dementia: A clinical effectiveness and cost-effectiveness pragmatic, multicentre, randomised controlled trial. Heal. Technol. Assess. 2015, 19, 1–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orrell, M.; Yates, L.; Leung, P.; Kang, S.; Hoare, Z.; Whitaker, C.; Burns, A.; Knapp, M.; Leroi, I.; Moniz-Cook, E.; et al. The impact of individual Cognitive Stimulation Therapy (iCST) on cognition, quality of life, caregiver health, and family relationships in dementia: A randomised controlled trial. PLoS Med. 2017, 14, e1002269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yates, L.A. The Development and Evaluation of Individual Cognitive Stimulation Therapy (ICST) for People with Dementia. Ph.D. Thesis, University College London (UCL), London, UK, 2016. [Google Scholar]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polit, D.; Beck, C. Nursing Research: Principles and Methods, 7th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2004. [Google Scholar]
- Brooke, P.; Bullock, R. Validation of a 6 Item Cognitive Impairment Test with a View to Primary Care Usage. Int J Geriatr Psychiatry 1999, 14, 936–940. [Google Scholar] [CrossRef]
- Logsdon, R.; Gibbons, L.E.; McCurry, S.; Teri, L. Quality of Life in Alzheimer’s Disease: Patient and Caregiver Reports. J. Ment. Health Aging 1999, 5, 21–32. [Google Scholar]
- Rosen, W.G.; Mohs, R.C.; Davis, K.L. A new rating scale for Alzheimer’s disease. Am. J. Psychiatry 1984, 141, 1356–1364. [Google Scholar] [CrossRef]
- Cummings, J.L.; Mega, M.; Gray, K.; Rosenberg-Thompson, S.; Carusi, D.A.; Gornbein, J. The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology 1994, 44, 2308. [Google Scholar] [CrossRef] [Green Version]
- Ware, J.; Kosinski, M.; Keller, S. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales, 2nd ed.; New England Medical Center: Boston, MA, USA, 1995. [Google Scholar]
- Marôco, J. Análise de Equações Estruturais—Fundamentos Teóricos, Software & Aplicações; PSE—Produtores e Serviço de Estatística, Lda.: Lisbon, Portugal, 2010. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Apóstolo, J.; Paiva, D.D.S.; Silva, R.; dos Santos, E.J.F.; Schultz, T. Adaptation and validation into Portuguese language of the six-item cognitive impairment test (6CIT). Aging Ment. Heal. 2017, 22, 1190–1195. [Google Scholar] [CrossRef]
- Braun, M.; Scholz, U.; Bailey, B.; Perren, S.; Hornung, R.; Martin, M. Dementia caregiving in spousal relationships: A dyadic perspective. Aging Ment. Heal. 2009, 13, 426–436. [Google Scholar] [CrossRef] [Green Version]
- Hanson, L.C.; Carey, T.S.; Caprio, A.J.; Lee, T.J.; Ersek, M.; Garrett, J.; Jackman, A.; Gilliam, R.; Wessell, K.; Mitchell, S.L. Improving Decision-Making for Feeding Options in Advanced Dementia: A Randomized, Controlled Trial. J. Am. Geriatr. Soc. 2011, 59, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
- Burgener, S.; Twigg, P. Relationships Among Caregiver Factors and Quality of Life in Care Recipients with Irreversible Dementia. Alzheimer Dis. Assoc. Disord. 2002, 16, 88–102. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.S.; Cheng, S.-T.; Wang, J. Unravelling positive aspects of caregiving in dementia: An integrative review of research literature. Int. J. Nurs. Stud. 2018, 79, 1–26. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic and Clinical Characteristics | Cared Person | Carer |
|---|---|---|
| Gender (male/female) | 15/38 | 11/42 |
| Age (Mean ± SD; range) | 79.20 ± 8.90; 60–97 | 58.13 ± 14.61; 20–81 |
| Education level, years (Mean ± SD; range) | 4.09 ± 2.44; 0–15 | 7.73 ± 4.10; 3–17 |
| Deterioration degree (%) | 56.6% mild NCD 43.4% moderate NCD | - - |
| Kinship degree with cared person (%) Son/Daughter Spouse Grandchild Paid Caregiver Daughter in law Neighbour | - - - - - - | 52.8% 26.4% 7.5% 7.5% 3.8% 1.9% |
| Cohabitation with cared person (%) | - | 64.2% |
| Scale’s Scores (Total and per Subscale) | QCPR (Cared Person’s Version) | QCPR (Carer’s Version) |
|---|---|---|
| Warmth subscale score (Mean ± SD; range) | 33.32 ± 3.82; 23–40 | 32.43 ± 5.70; 11–40 |
| Conflict/criticism subscale score (Mean ± SD; range) | 22.34 ± 3.79; 15–30 | 21.83 ± 4.55; 10–30 |
| Total QCPR score (Mean ± SD; range) | 55.66 ± 7.16; 39–70 | 54.26 ± 9.25; 21–70 |
| Typology of the relationship quality (%) | 5.7% poor quality 43.4% common quality 50.9% good quality | 7.5% poor quality 47.2% common quality 45.3% good quality |
| Item | Item Mean | Item Standard Deviation | Item-Total Correlation | Corrected Item-Total Correlation | Alpha If Item Deleted |
|---|---|---|---|---|---|
| Cared Person’s version | |||||
| 1 | 4.17 | 0.64 | 0.72 | 0.65 | 0.88 |
| 2 | 3.83 | 0.87 | 0.77 | 0.68 | 0.87 |
| 3 | 4.02 | 0.72 | 0.56 | 0.47 | 0.88 |
| 4 | 4.17 | 0.73 | 0.80 | 0.67 | 0.87 |
| 5 | 4. 13 | 0.56 | 0.70 | 0.70 | 0.88 |
| 6 | 4.19 | 0.59 | 0.72 | 0.77 | 0.87 |
| 7 | 4.04 | 0.83 | 0.77 | 0.78 | 0.87 |
| 8 | 3.81 | 1.06 | 0.75 | 0.69 | 0.87 |
| 9 | 4.19 | 0.59 | 0.72 | 0.68 | 0.88 |
| 10 | 3.42 | 1.12 | 0.64 | 0.55 | 0.88 |
| 11 | 3.92 | 1.05 | 0.63 | 0.48 | 0.88 |
| 12 | 4.17 | 0.47 | 0.70 | 0.69 | 0.88 |
| 13 | 3.53 | 1.15 | 0.36 | 0.20 | 0.90 |
| 14 | 4.26 | 0.49 | 0.60 | 0.54 | 0.88 |
| Carer’s version | |||||
| 1 | 3.75 | 0.92 | 0.64 | 0.65 | 0.90 |
| 2 | 3.49 | 1.03 | 0.70 | 0.67 | 0.90 |
| 3 | 4.04 | 0.96 | 0.71 | 0.64 | 0.90 |
| 4 | 3.94 | 0.99 | 0.69 | 0.71 | 0.90 |
| 5 | 3.85 | 0.95 | 0.69 | 0.71 | 0.90 |
| 6 | 4.26 | 0.79 | 0.70 | 0.81 | 0.90 |
| 7 | 4.00 | 0.98 | 0.74 | 0.77 | 0.90 |
| 8 | 3.66 | 1.14 | 0.73 | 0.67 | 0.90 |
| 9 | 4.15 | 0.84 | 0.70 | 0.78 | 0.90 |
| 10 | 3.06 | 1.15 | 0.41 | 0.37 | 0.92 |
| 11 | 4.49 | 0.82 | 0.54 | 0.34 | 0.91 |
| 12 | 4.13 | 0.81 | 0.63 | 0.62 | 0.91 |
| 13 | 3.26 | 1.40 | 0.70 | 0.56 | 0.91 |
| 14 | 4.32 | 0.67 | 0.71 | 0.64 | 0.91 |
| Descriptive Statistics | Cared Person | Carer | ||||
|---|---|---|---|---|---|---|
| 6-CIT | ADAS-Cog | INP | QoL-AD | SF-12 Physical | SF-12 Mental | |
| Mean (SD) | 13.68 (5.65) | 20.17 (7.53) | 11.31 (10.73) | 25.97 (5.67) | 55.62 (17.13) | 52.12 (16.66) |
| Range | 4–20 | 4–42 | 0–49 | 15.33–38.67 | 20.00–82.67 | 9.52–80.95 |
| Cared Person’s Version | Carer’s Version | |||||
|---|---|---|---|---|---|---|
| QCPR | 6-CIT | ADAS-Cog | INP | QoL-AD | SF-12 Physical | SF-12 Mental |
| Warmth subscale | −0.003 | 0.186 | −0.028 | 0.412 ** | 0.181 | 0.239 |
| Conflict/criticism subscale | 0.035 | 0.195 | −0.098 | 0.292 ** | 0.415 ** | 0.402 ** |
| Total | 0.018 | 0.195 | −0.073 | 0.356 ** | 0.318 * | 0.359 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, R.; Bobrowicz-Campos, E.; Santos-Costa, P.; Gil, I.; Neves, H.; Apóstolo, J. The Quality of Carer–Patient Relationship Scale: Adaptation and Validation into Portuguese. Int. J. Environ. Res. Public Health 2021, 18, 1264. https://doi.org/10.3390/ijerph18031264
Silva R, Bobrowicz-Campos E, Santos-Costa P, Gil I, Neves H, Apóstolo J. The Quality of Carer–Patient Relationship Scale: Adaptation and Validation into Portuguese. International Journal of Environmental Research and Public Health. 2021; 18(3):1264. https://doi.org/10.3390/ijerph18031264
Chicago/Turabian StyleSilva, Rosa, Elzbieta Bobrowicz-Campos, Paulo Santos-Costa, Isabel Gil, Hugo Neves, and João Apóstolo. 2021. "The Quality of Carer–Patient Relationship Scale: Adaptation and Validation into Portuguese" International Journal of Environmental Research and Public Health 18, no. 3: 1264. https://doi.org/10.3390/ijerph18031264
APA StyleSilva, R., Bobrowicz-Campos, E., Santos-Costa, P., Gil, I., Neves, H., & Apóstolo, J. (2021). The Quality of Carer–Patient Relationship Scale: Adaptation and Validation into Portuguese. International Journal of Environmental Research and Public Health, 18(3), 1264. https://doi.org/10.3390/ijerph18031264








