Considerations in Planning Physical Activity for Older Adults in Hot Climates: A Narrative Review
Abstract
1. Introduction
2. Methods
Search Strategy
3. Definitions
3.1. Older Adults
3.2. What Is “Healthy Ageing”?
3.3. Definitions of Physical Activity
3.4. Types of Exercise
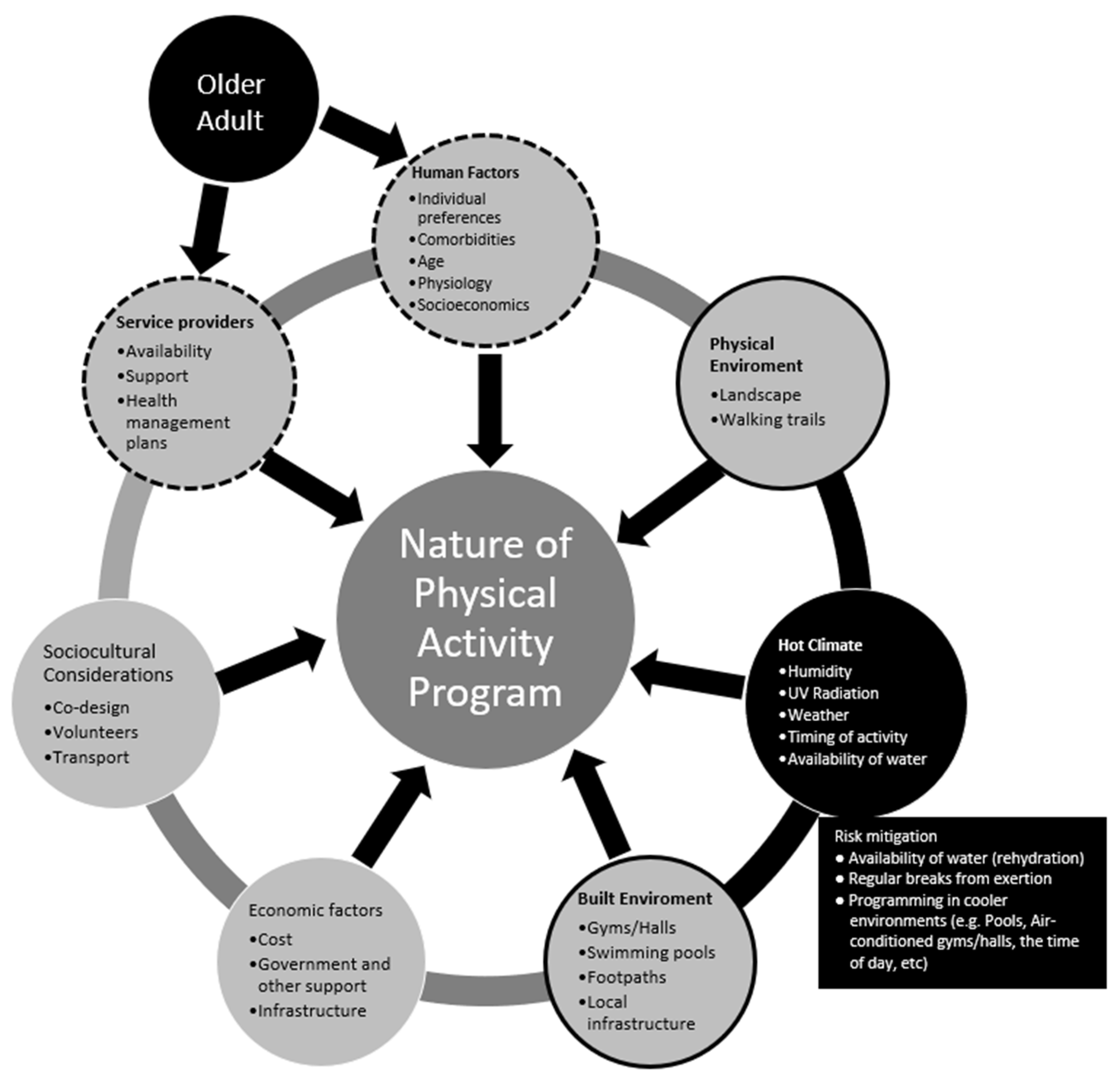
4. Factors Affecting Physical Activity in Older Adults
4.1. Physiological Changes, Thermoregulation, and Comorbidities in Older Adults
4.2. Barriers and Enablers
4.3. Environmental Factors
4.3.1. Physical Environment
4.3.2. Timing of Exercise to Accommodate Climatic Factors
4.4. Special Population Groups
4.5. Risk Management
5. Recommendations: What Does This Mean in Practice?
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Warburton, D.; Nicol, C.; Bredin, S. Health benefits of physical activity: The evidence. CMAJ 2006, 176, 801–809. [Google Scholar] [CrossRef]
- Taylor, A.; Cable, N.; Faulkner, G.; Hillsdon, M.; Narici, M.; Van Der Bij, A. Physical activity and older adults: A review of health benefits and the effectiveness of interventions. J. Sports Sci. 2004, 22, 703–725. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendations from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1094–1105. [Google Scholar] [CrossRef]
- Lopez, A.; Adair, T. Slower increase in life expectancy in Australia than in other high income countries: The contributions of age and cause of death. Med. J. Aust. 2019, 210, 403–409. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. 3101.0—Australian Demographic Statistics. June 2019. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/0/1CD2B1952AFC5E7ACA257298000F2E76?OpenDocument (accessed on 15 May 2020).
- Australian Bureau of Statistics. Physical Activity (Section). Available online: https://www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0.55.001 (accessed on 13 May 2020).
- Mason, A. Demographic transition and demographic dividends in developed and developing countries. In Proceedings of the United Nations Expert Group Meeting on Social and Economic Implications of Changing Population Age Structures, Mexico City, Mexico, 31 August–2 September 2005; p. 5. [Google Scholar]
- World Health Organisation. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 15 May 2020).
- World Health Organisation. Global Recommendations on Physical Activity for Health; World Health Organisation: Geneva, Switzerland, 2010. [Google Scholar]
- Sims, J.; Hill, K.; Hunt, S.; Haralambous, B.; Brown, A.; Engel, L.; Huang, N.; Kerse, N.; Ory, M. National Physical Activity Recommendations for Older Australians: Discussion Document; National Ageing Research Institute: Canberra, Australia, 2006.
- Australian Government—Department of Veterans Affairs & Department of Health and Ageing. Choose Health: Be Active—A Physical Activity Guide for Older Australians; Australian Government—Department of Veterans Affairs & Department of Health and Ageing: Canberra, Australia, 2005.
- World Health Organisation. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organisation: Geneva, Switzerland, 2020. [Google Scholar]
- Australian Institute of Health and Welfare. Insufficient Physical Activity. Cat. No. PHE 248; Australian Institute of Health and Welfare: Canberra, Australia, 2020. [Google Scholar]
- Zubala, A.; MacGillivray, S.; Frost, H.; Kroll, T.; Skelton, D.A.; Gavine, A.; Gray, N.M.; Toma, M.; Morris, J. Promotion of physical activity interventions for community dwelling older adults: A systematic review of reviews. PLoS ONE 2017, 12, 1–36. [Google Scholar] [CrossRef]
- Brotherhood, J.R. Heat stress and strain in exercise and sport. J. Sci. Med. Sport 2008, 11, 6–19. [Google Scholar] [CrossRef]
- Matthews, T.K.; Wilby, R.L.; Murphy, C. Communicating the deadly consequences of global warming for human heat stress. Proc. Natl. Acad. Sci. USA 2017, 114, 3861–3866. [Google Scholar] [CrossRef]
- Ferrari, R. Writing narrative style literature reviews. Med. Writ. 2015, 24, 230–235. [Google Scholar] [CrossRef]
- Uddin, M.; Arafat, S. Barriers to and Facilitators of Physical Activity Program Use Among Older Adults. Int. J. Percept. Public Health 2016, 1, 14–24. [Google Scholar]
- Greenhalgh, T.; Thorne, S.; Malterud, K. Time to challenge the spurious hierarchy of systematic over narrative reviews? Eur. J. Clin. Invest. 2018, 48, e12931. [Google Scholar] [CrossRef]
- Gusenbauer, M.; Haddaway, N.R. Which academic search systems are suitable for systematic reviews or meta-analyses? Evaluating retrieval qualities of Google Scholar, PubMed, and 26 other resources. Res. Synth. Methods 2020, 11, 181–217. [Google Scholar] [CrossRef] [PubMed]
- Australian Government: Australian Law Reform Commission. Who are older Australians? Available online: https://www.alrc.gov.au/publication/elder-abuse-a-national-legal-response-alrc-report-131/2-concepts-and-context-2/who-are-older-australians/ (accessed on 15 May 2020).
- Australian Government. National Aboriginal and Torres Strait Islander Flexible Aged Care Program; Program Manual; Department of Health, Australian Government: Canberra, Australia, 2019.
- Australian Government—Department of Health and Ageing. Living Longer. Living Better. Aged Care Reform Package (Technical Document); Australian Government—Department of Health and Ageing: Canberra, Australia, 2012.
- World Health Organisation. Decade of Healthy Ageing 2020–2030; World Health Organisation: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organisation. What is Healthy Ageing? Available online: https://www.who.int/ageing/healthy-ageing/en/ (accessed on 15 May 2020).
- Martin, P.; Kelly, N.; Kahana, B.; Kahana, E.; Willcox, B.J.; Willcox, D.C.; Poon, L.W. Defining successful aging: A tangible or elusive concept? Gerontologist 2015, 55, 14–25. [Google Scholar] [CrossRef]
- World Health Organisation. Physical Activity. Available online: https://www.who.int/dietphysicalactivity/pa/en/ (accessed on 18 May 2020).
- National Institute on Ageing. Four Types of Exercise Can Improve Your Health and Physical Ability. Available online: https://www.nia.nih.gov/health/four-types-exercise-can-improve-your-health-and-physical-ability (accessed on 18 May 2020).
- Jones, G.R.; Stathokostas, L.; Young, B.W.; Wister, A.V.; Chau, S.; Clark, P.; Duggan, M.; Mitchell, D.; Nordland, P. Development of a physical literacy model for older adults—A consensus process by the collaborative working group on physical literacy for older Canadians. BMC Geriatr. 2018, 18, 13. [Google Scholar] [CrossRef]
- Navaratnarajah, A.; Jackson, S.H. The physiology of ageing. Medicine 2013, 41, 5–8. [Google Scholar] [CrossRef]
- de Labra, C.; Guimaraes-Pinheiro, C.; Maseda, A.; Lorenzo, T.; Millán-Calenti, J.C. Effects of physical exercise interventions in frail older adults: A systematic review of randomized controlled trials. BMC Geriatr. 2015, 15, 154. [Google Scholar] [CrossRef]
- Balmain, B.N.; Sabapathy, S.; Louis, M.; Morris, N.R. Aging and Thermoregulatory Control: The Clinical Implications of Exercising under Heat Stress in Older Individuals. Biomed. Res. Int. 2018, 2018, 8306154. [Google Scholar] [CrossRef]
- Gagnon, D.; Jay, O.; Kenny, G.P. The evaporative requirement for heat balance determines whole-body sweat rate during exercise under conditions permitting full evaporation. J. Physiol. 2013, 591, 2925–2935. [Google Scholar]
- Kenny, G.P.; Yardley, J.; Brown, C.; Sigal, R.J.; Jay, O. Heat stress in older individuals and patients with common chronic diseases. CMAJ 2010, 182, 1053–1060. [Google Scholar] [CrossRef]
- Shibasaki, M.; Okazaki, K.; Inoue, Y. Aging and thermoregulation. J. Phys. Fit. Sports Med. 2013, 2, 37–47. [Google Scholar] [CrossRef]
- Kenney, W.L.; Hodgson, J.L. Heat tolerance, thermoregulation and ageing. Sports Med. 1987, 4, 446–456. [Google Scholar] [CrossRef]
- Charkoudian, N. Skin blood flow in adult human thermoregulation: How it works, when it does not, and why. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2003; pp. 603–612. [Google Scholar]
- González-Alonso, J.; Crandall, C.G.; Johnson, J.M. The cardiovascular challenge of exercising in the heat. J. Physiol. 2008, 586, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.M.; Pierzga, J.M.; Kenney, W.L. Aerobic training and cutaneous vasodilation in young and older men. J. Appl. Physiol. 1999, 86, 1676–1686. [Google Scholar] [CrossRef] [PubMed]
- Tew, G.A.; Klonizakis, M.; Saxton, J.M. Effects of ageing and fitness on skin-microvessel vasodilator function in humans. Eur. J. Appl. Physiol. 2010, 109, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, C.G.; Kenney, W.L. Effects of age and acclimation on responses to passive heat exposure. J. Appl. Physiol. 1993, 75, 2162–2167. [Google Scholar] [CrossRef]
- Aoyagi, Y.; McLellan, T.M.; Shephard, R.J. Interactions of Physical Training and Heat Acclimation. Sports Med. 1997, 23, 173–210. [Google Scholar] [CrossRef]
- Roser, M.; Ortiz-Ospina, E.; Ritchie, H. Life Expectancy. Our World in Data. 2013. Available online: https://ourworldindata.org/life-expectancy (accessed on 18 January 2021).
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef]
- Hussain, M.A.; Katzenellenbogen, J.M.; Sanfilippo, F.M.; Murray, K.; Thompson, S.C. Complexity in disease management: A linked data analysis of multimorbidity in Aboriginal and non-Aboriginal patients hospitalised with atherothrombotic disease in Western Australia. PLoS ONE 2018, 13, e0201496. [Google Scholar] [CrossRef]
- Courneya, K.S.; Mackey, J.R.; Jones, L.W. Coping with cancer: Can exercise help? Phys. Sports Med. 2000, 28, 49–73. [Google Scholar]
- Courneya, K.S.; Vallance, J.K.; McNeely, M.L.; Karvinen, K.H.; Peddle, C.J.; Mackey, J.R. Exercise issues in older cancer survivors. Crit. Rev. Oncol. Hematol. 2004, 51, 249–261. [Google Scholar] [CrossRef]
- Fransen, M.; McConnell, S.; Bell, M. Therapeutic exercise for people with osteoarthritis of the hip or knee. A systematic review. J. Rheumatol. 2002, 29, 1737–1745. [Google Scholar]
- Newton, R.U.; Galvao, D.A. Exercise in prevention and management of cancer. Curr. Treat. Options Oncol. 2008, 9, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Yohannes, A.M.; Caton, S. Management of depression in older people with osteoarthritis: A systematic review. Aging Ment. Health 2010, 14, 637–651. [Google Scholar] [CrossRef]
- Rivera-Torres, S.; Fahey, T.D.; Rivers, M.A. Adherence to Exercise Programs in Older Adults: Informative Report. Gerontol. Geriatr. Med. 2019, 5, 1–10. [Google Scholar] [CrossRef]
- Picorelli, A.M.; Pereira, L.S.; Pereira, D.S.; Felicio, D.; Sherrington, C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: A systematic review. J. Physiother 2014, 60, 151–156. [Google Scholar] [CrossRef]
- Lewis, M.V.; Szabo, R.A.; Weiner, K.R.; McCall, L.; Piterman, L. Cultural barriers to exercise amongst the ethnic elderly. Internet J. Health Promot. 1997, 4, 1–7. [Google Scholar]
- Resnick, B.; Spellbring, A.M. Understanding what motivates older adults to exercise. J. Gerontol. Nurs. 2000, 26, 34–42. [Google Scholar] [CrossRef]
- Jancey, J.M.; Clarke, A.; Howat, P.; Maycock, B.; Lee, A.H. Perceptions of physical activity by older adults: A qualitative study. Health Educ. J. 2009, 68, 196–206. [Google Scholar] [CrossRef]
- Bennett, J.A.; Winters-Stone, K. Motivating older adults to exercise: What works? Age Ageing 2011, 40, 148–149. [Google Scholar] [CrossRef]
- Schutzer, K.A.; Graves, B.S. Barriers and motivations to exercise in older adults. Prev. Med. 2004, 39, 1056–1061. [Google Scholar] [CrossRef]
- Bethancourt, H.J.; Rosenberg, D.E.; Beatty, T.; Arterburn, D.E. Barriers to and facilitators of physical activity program use among older adults. Clin. Med. Res. 2014, 12, 10–20. [Google Scholar] [CrossRef]
- Boehm, J.; Franklin, R.C.; Newitt, R.; McFarlane, K.; Grant, T.; Kurkowski, B. Barriers and motivators to exercise for older adults: A focus on those living in rural and remote areas of Australia. Aust. J. Rural Health 2013, 21, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Burton, E.; Farrier, K.; Lewin, G.; Pettigrew, S.; Hill, A.M.; Airey, P.; Bainbridge, L.; Hill, K.D. Motivators and Barriers for Older People Participating in Resistance Training: A Systematic Review. J. Aging Phys. Act. 2017, 25, 311–324. [Google Scholar] [CrossRef]
- Biedenweg, K.; Meischke, H.; Bohl, A.; Hammerback, K.; Williams, B.; Poe, P.; Phelan, E.A. Understanding older adults’ motivators and barriers to participating in organized programs supporting exercise behaviors. J. Prim. Prev. 2014, 35, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Barnett, D.W.; Barnett, A.; Nathan, A.; Van Cauwenberg, J.; Cerin, E. Built environmental correlates of older adults’ total physical activity and walking: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.R.; Tong, A.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Pinto, R.Z.; Ferreira, M.L. Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br. J. Sports Med. 2015, 49, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, R.E.; Saelens, B.E.; Sauvage-Mar, C. Understanding Physical Activity through Interactions Between the Built Environment and Social Cognition: A Systematic Review. Sports Med. 2018, 48, 1893–1912. [Google Scholar] [CrossRef]
- Van Cauwenberg, J.; Nathan, A.; Barnett, A.; Barnett, D.W.; Cerin, E. The Council on Environment Physical Activity—Older Adults Working Group. Relationships Between Neighbourhood Physical Environmental Attributes and Older Adults’ Leisure-Time Physical Activity: A Systematic Review and Meta-Analysis. Sports Med. 2018, 48, 1635–1660. [Google Scholar] [CrossRef] [PubMed]
- Spiteri, K.; Broom, D.; Bekhet, A.H.; de Caro, J.X.; Laventure, B.; Grafton, K. Barriers and Motivators of Physical Activity Participation in Middle-Aged and Older Adults—A Systematic Review. J. Aging Phys. Act. 2019, 27, 929–944. [Google Scholar] [CrossRef]
- Haselwandter, E.M.; Corcoran, M.P.; Folta, S.C.; Hyatt, R.; Fenton, M.; Nelson, M.E. The Built Environment, Physical Activity, and Aging in the United States: A State of the Science Review. J. Aging Phys. Act. 2015, 23, 323–329. [Google Scholar] [CrossRef]
- Van Dyck, D.; Cerin, E.; Conway, T.L.; De Bourdeaudhuij, I.; Owen, N.; Kerr, J.; Cardon, G.; Frank, L.D.; Saelens, B.E.; Sallis, J.F. Perceived neighborhood environmental attributes associated with adults’ leisure-time physical activity: Findings from Belgium, Australia and the USA. Health Place 2013, 19, 59–68. [Google Scholar] [CrossRef]
- Dorwart, C.E. Views From the Path: Evaluating Physical Activity Use Patterns and Design Preferences of Older Adults on the Bolin Creek Greenway Trail. J. Aging Phys. Act. 2015, 23, 513–523. [Google Scholar] [CrossRef] [PubMed]
- Levinger, P.; Sales, M.; Polman, R.; Haines, T.; Dow, B.; Biddle, S.J.H.; Duque, G.; Hill, K.D. Outdoor physical activity for older people-the senior exercise park: Current research, challenges and future directions. Health Promot. J. Aust. 2018, 29, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Nykiforuk, C.I.J.; Rawson, D.; McGetrick, J.A.; Belon, A.P. Canadian policy perspectives on promoting physical activity across age-friendly communities: Lessons for advocacy and action. Ageing Soc. 2019, 39, 307–339. [Google Scholar] [CrossRef]
- Cleland, V.; Hughes, C.; Thornton, L.; Squibb, K.; Venn, A.; Ball, K. Environmental barriers and enablers to physical activity participation among rural adults: A qualitative study. Health Promot. J. Aust. 2015, 26, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Hue, O. The Challenge of Performing Aerobic Exercise in Tropical Environments: Applied Knowledge and Perspectives. Int. J. Sports Physiol. Perform. 2011, 6, 443–454. [Google Scholar] [CrossRef]
- Caldwell, K.; Fernandez, R.; Traynor, V.; Perrin, C. Effects of spending time outdoors in daylight on the psychosocial well-being of older people and their family carers: A systematic review. Jbi Evid. Synth. 2014, 12, 277–320. [Google Scholar] [CrossRef][Green Version]
- Dahlberg, E.E.; Hamilton, S.J.; Hamid, F.; Thompson, S.C. Indigenous Australians Perceptions’ of Physical Activity: A Qualitative Systematic Review. Int. J. Envrion. Res. Public Health 2018, 15, 1492. [Google Scholar] [CrossRef]
- Dimer, L.; Dowling, T.; Jones, J.; Cheetham, C.; Thomas, T.; Smith, J.; McManus, A.; Maiorana, A.J. Build it and they will come: Outcomes from a successful cardiac rehabilitation program at an Aboriginal Medical Service. Aust. Health Rev. 2013, 37, 79–82. [Google Scholar] [CrossRef]
- Mendham, A.E.; Duffield, R.; Marino, F.; Coutts, A.J. A 12-week sports-based exercise programme for inactive Indigenous Australian men improved clinical risk factors associated with type 2 diabetes mellitus. J. Sci. Med. Sport 2015, 18, 438–443. [Google Scholar] [CrossRef]
- Passmore, E.; Shepherd, B.; Milat, A.; Maher, L.; Hennessey, K.; Havrlant, R.; Maxwell, M.; Hodge, W.; Christian, F.; Richards, J.; et al. The impact of a community-led program promoting weight loss and healthy living in Aboriginal communities: The New South Wales Knockout Health Challenge. BMC Public Health 2017, 17, 951–959. [Google Scholar] [CrossRef]
- Rowley, K.G.; Daniel, M.; Skinner, K.; Skinner, M.; White, G.A.; Dea, K. Effectiveness of a community-directed ‘healthy lifestyle’ program in a remote Australian Aboriginal community. Aust. N. Z. J. Public Health 2000, 24, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Buys, N. Effectiveness of a participative community singing program to improve health behaviors and increase physical activity in Australian Aboriginal and Torres Strait Islander people. Int. J. Disabil. Hum. Dev. 2013, 12, 297–304. [Google Scholar] [CrossRef]
- Davey, M.; Moore, W.; Walters, J. Tasmanian Aborigines step up to health: Evaluation of a cardiopulmonary rehabilitation and secondary prevention program. BMC Health Serv. Res. 2014, 14, 349. [Google Scholar] [CrossRef] [PubMed]
- Lukaszyk, C.; Coombes, J.; Sherrington, C.; Tiedemann, A.; Keay, L.; Mackean, T. The Ironbark program: Implementation and impact of a community-based fall prevention pilot program for older Aboriginal and Torres Strait Islander people. Health Promot. J. Aust. 2018, 29, 189–198. [Google Scholar] [CrossRef]
- Stickney, B.; Vilshanskaya, O. Engaging older people with English as a second language and frail older people in physical activity. Health Promot. J. Aust. 2005, 16, 116–123. [Google Scholar] [CrossRef]
- Pasick, R.J.; D’onofrio, C.N.; Otero-Sabogal, R. Similarities and differences across cultures: Questions to inform a third generation for health promotion research. Health Educ. Q. 1996, 23, 142–161. [Google Scholar] [CrossRef]
- Batt, M.E.; Tanji, J.; Börjesson, M. Exercise at 65 and Beyond. Sports Med. 2013, 43, 525–530. [Google Scholar] [CrossRef]
- Elward, K.; Larson, E.B. Benefits of exercise for older adults: A review of existing evidence and current recommendations for the general population. Clin. Geriatr. Med. 1992, 8, 35–50. [Google Scholar] [CrossRef]
- Gill, T.M.; DiPietro, L.; Krumholz, H.M. Role of exercise stress testing and safety monitoring for older persons starting an exercise program. JAMA 2000, 284, 342–349. [Google Scholar] [CrossRef]
- Morey, N.C.; Sullivan, R.J. Medical assessment for health advocacy and practical strategies for exercise initiation. Am. J. Prev. Med. 2003, 25, 204–208. [Google Scholar] [CrossRef]
- Skelton, D.A.; Dinan, S.M. Exercise for falls management: Rationale for an exercise programme to reduce postural instability. Physiother. Theory Pr. 1999, 15, 105–120. [Google Scholar] [CrossRef]
- Gardner, M.M.; Robertson, M.C.; Campbell, A.J. Exercise in preventing falls and fall related injuries in older people: A review of randomised controlled trials. Br J Sports Med 2000, 34, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Day, L.; Fildes, B.; Gordon, I. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002, 325, 128–134. [Google Scholar] [CrossRef]
- Kannus, P.; Parkkari, J.; Niemi, S.; Pasanen, M.; Palvanen, M.; Jarvinen, M.; Vuori, I. Prevention of hip fracture in elderly people with use of a hip protector. N. Engl. J. Med. 2000, 343, 1506–1513. [Google Scholar] [CrossRef] [PubMed]
- Siscovick, D.S.; Ekelund, L.G.; Johnson, J.L.; Truong, Y.; Adler, A. Sensitivity of exercise electrocardiography for acute cardiac events during moderate and strenuous physical activity. The Lipid Research Clinics Coronary Primary Prevention Trial. Arch. Intern. Med. 1991, 151, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Siscovick, D.S.; Weiss, N.S.; Fletcher, R.H.; Lasky, T. The incidence of primary cardiac arrest during vigorous exercise. N. Engl. J. Med. 1984, 311, 874–877. [Google Scholar] [CrossRef]
- Zaleski, A.L.; Taylor, B.A.; Panza, G.A.; Wu, Y.; Pescatello, L.S.; Thompson, P.D. Coming of Age: Considerations in the Prescription of Exercise for Older Adults. Methodist Debakey Cardiovasc. J. 2016, 12, 98–104. [Google Scholar] [CrossRef]
- Carron, A.V.; Hausenblas, H.A.; Mack, D. Social influence and exercise: A meta-analysis. J. Sport Exerc. Psychol. 1996, 18, 1–6. [Google Scholar] [CrossRef]
- Schehl, B.; Leukel, J. Associations between individual factors, environmental factors, and outdoor independence in older adults. Eur. J. Ageing 2020, 17, 291–298. [Google Scholar] [CrossRef]
- Gray, P.M.; Murphy, M.H.; Gallagher, A.M.; Simpson, E.E.A. Motives and Barriers to Physical Activity Among Older Adults of Different Socioeconomic Status. J. Aging Phys. Act. 2016, 24, 419–429. [Google Scholar] [CrossRef]
- Dergance, J.M.; Calmbach, W.L.; Dhanda, R.; Miles, T.P.; Hazuda, H.P.; Mouton, C.P. Barriers to and benefits of leisure time physical activity in the elderly: Differences across cultures. J. Am. Geriatr. Soc. 2003, 51, 863–868. [Google Scholar] [CrossRef] [PubMed]
- Kolt, G.S.; Paterson, J.E.; Cheung, V.Y. Barriers to physical activity participation in older Tongan adults living in New Zealand. Australas. J. Ageing 2006, 25, 119–125. [Google Scholar] [CrossRef]
| Type | Minimum Recommended Duration | Examples |
|---|---|---|
| Endurance Activities that increase heart and breathing rate. They target the heart, lungs and circulatory system. |
|
|
| Strength Activities that help strengthen muscle and bone to maintain daily functions and balance and reduce falls risk. |
|
|
| Flexibility Activities that help to increase mobility and maintain ease of movement. |
|
|
| Balance Activities that improve balance and stability and help prevent falls. |
|
|
| Factors Associated with Physical Inactivity [51] | Physical Literacy Factor [29] (Intrapersonal, Interpersonal, Organisational, Community, Policy) | Ease of Modifiability (Modifiable/Not Modifiable) |
|---|---|---|
| Demographic factors | ||
| Older age | Intrapersonal | Not modifiable |
| Female Sex | Intrapersonal | Not modifiable |
| Non-white race/ethnicity | Community | Not modifiable |
| Low socioeconomic status | Community | Modifiable * |
| Health-related clinical factors | ||
| Chronic illness | Intrapersonal | Modifiable * |
| Poor general health and physical function | Intrapersonal | Modifiable * |
| Overweight/obesity | Intrapersonal | Modifiable * |
| Cognitive and psychological factors | ||
| Greater perceived barriers to physical activity | Intrapersonal | Modifiable |
| Lack of enjoyment of physical activity | Intrapersonal | Modifiable |
| Low expectations of benefits from physical activity | Intrapersonal | Modifiable |
| Poor psychological health | Intrapersonal | Modifiable * |
| Low self-efficacy for physical activity | Intrapersonal | Modifiable * |
| Low self-motivation for physical activity | Intrapersonal | Modifiable * |
| Lack of readiness to change physical activity behaviours | Intrapersonal | Modifiable |
| Poor fitness level | Intrapersonal | Modifiable |
| Behavioural factors | ||
| Prior physical activity | Intrapersonal | Modifiable |
| Smoking | Intrapersonal | Modifiable |
| Type A Behaviour (assoc’d with poorer adherence but greater overall physical activity levels) | Intrapersonal | Modifiable * |
| Social factors | ||
| Lack of cohesion in exercise group | Interpersonal | Modifiable |
| Lack of physician influence/advice for physical activity | Interpersonal | Modifiable |
| Lack of social support for physical activity | Community | Modifiable |
| Program-related factors | ||
| High physical activity intensity | Organisational | Modifiable |
| Long physical activity duration | Organisational | Modifiable |
| Environmental factors | ||
| Lack of access to facilities/parks/trails | Community/Policy | Modifiable * |
| Lack of neighbourhood safety | Community/Policy | Modifiable * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
See, L.; Rasiah, R.L.; Laing, R.; Thompson, S.C. Considerations in Planning Physical Activity for Older Adults in Hot Climates: A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 1331. https://doi.org/10.3390/ijerph18031331
See L, Rasiah RL, Laing R, Thompson SC. Considerations in Planning Physical Activity for Older Adults in Hot Climates: A Narrative Review. International Journal of Environmental Research and Public Health. 2021; 18(3):1331. https://doi.org/10.3390/ijerph18031331
Chicago/Turabian StyleSee, Lydia, Rohan L. Rasiah, Rachael Laing, and Sandra C. Thompson. 2021. "Considerations in Planning Physical Activity for Older Adults in Hot Climates: A Narrative Review" International Journal of Environmental Research and Public Health 18, no. 3: 1331. https://doi.org/10.3390/ijerph18031331
APA StyleSee, L., Rasiah, R. L., Laing, R., & Thompson, S. C. (2021). Considerations in Planning Physical Activity for Older Adults in Hot Climates: A Narrative Review. International Journal of Environmental Research and Public Health, 18(3), 1331. https://doi.org/10.3390/ijerph18031331







