Enhancing Self-Esteem and Body Image of Breast Cancer Women through Interventions: A Systematic Review
Abstract
1. Introduction
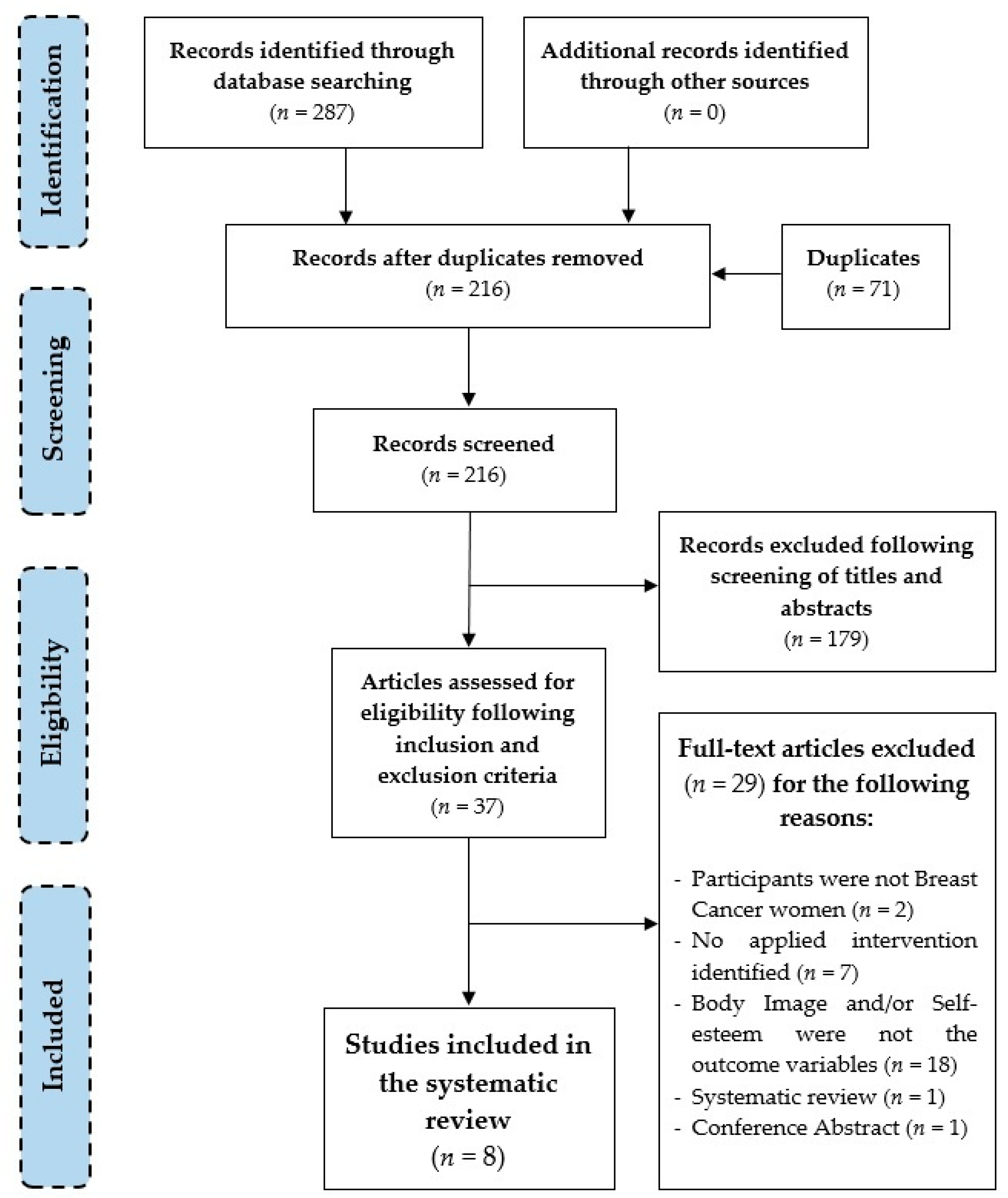
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Eligibility Criteria
2.3. Data Collection Process
2.4. Analysis
3. Results
3.1. Findings
3.2. Study Characteristics
3.2.1. Design of the Studies
3.2.2. Participants and Regrouping
3.2.3. Interventions and Professionals Who Implement These
3.2.4. Changes in BI and Self-Esteem after the Interventions
3.2.5. Methodology and Measurements
3.2.6. Characteristics of the Participants
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO (World Health Organization). Breast Cancer: Prevention and Control. Breast Cancer Burden. Available online: https://www.who.int/cancer/detection/breastcancer/en/index1.html (accessed on 8 October 2020).
- Boing, L.; do Bem Fretta, T.; de Carvalho Souza Vieira, M.; Pereira, G.S.; Moratelli, J.; Sperandio, F.F.; Bergmann, A.; Baptista, F.; Dias, M.; de Azevedo Guimarães, A.C. Pilates and dance to patients with breast cancer undergoing treatment: Study protocol for a randomized clinical trial–MoveMama study. Trials 2020, 21, 35. [Google Scholar] [CrossRef]
- Guil, R.; González-Ruiz, P.; Merchán-Clavellino, A.; Morales-Sánchez, L.; Zayas, A.; Gómez-Molinero, R. Breast Cancer and Resilience: The Controversial Role of Perceived Emotional Intelligence. Front. Psychol. 2020, 11, 3604. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Nardin, S.; Mora, E.; Varughese, F.M.; D’Avanzo, F.; Vachanaram, A.R.; Rossi, V.; Saggia, C.; Rubinelli, S.; Gennari, A. Breast cancer survivorship, quality of life, and late toxicities. Front. Oncol. 2020, 10, 864. [Google Scholar] [CrossRef]
- Coleman, R.E.; Marshall, H.; Cameron, D.; Dodwell, D.; Burkinshaw, R.; Keane, M.; Gil, M.; Houston, S.J.; Grieve, R.J.; Ritchie, D. Breast-cancer adjuvant therapy with zoledronic acid. N. Engl. J. Med. 2011, 365, 1396–1405. [Google Scholar] [CrossRef] [PubMed]
- González, C.M.; Calva, E.A.; Zambrano, L.M.B.; Medina, S.M.; López, J.R.P. Ansiedad y calidad de vida en mujeres con cáncer de mama: Una revisión teórica. Psicol. Y Salud 2018, 28, 155–165. [Google Scholar] [CrossRef]
- Martino, M.L.; Lemmo, D.; Gargiulo, A.; Barberio, D.; Abate, V.; Avino, F.; Tortoriello, R. Underfifty women and breast cancer: Narrative markers of meaning-making in traumatic experience. Front. Psychol. 2019, 10, 618. [Google Scholar] [CrossRef] [PubMed]
- Dibbell-Hope, S. The use of dance/movement therapy in psychological adaptation to breast cancer. Arts Psychother. 2000, 27, 51–68. [Google Scholar] [CrossRef]
- Fetaini, M.; Hawari, A.; Kaki, F.; Ujaimi, R.; Tashkandi, H.; AbuSanad, A. Impact of breast cancer treatments on body image and quality of life in survivors. IJMDCs 2020, 4, 635–644. [Google Scholar] [CrossRef]
- Andrzejczak, E.; Markocka-Mączka, K.; Lewandowski, A. Partner relationships after mastectomy in women not offered breast reconstruction. Psychooncology 2013, 22, 1653–1657. [Google Scholar] [CrossRef]
- Beaver, K.; Williamson, S.; Briggs, J. Exploring patient experiences of neo-adjuvant chemotherapy for breast cancer. Eur. J. Oncol. Nurs. 2016, 20, 77–86. [Google Scholar] [CrossRef]
- Farthmann, J.; Hanjalic-Beck, A.; Veit, J.; Rautenberg, B.; Stickeler, E.; Erbes, T.; Hasenburg, A. The impact of chemotherapy for breast cancer on sexual function and health-related quality of life. Support. Care Cancer 2016, 24, 2603–2609. [Google Scholar] [CrossRef]
- Ljungman, L.; Ahlgren, J.; Petersson, L.M.; Flynn, K.E.; Weinfurt, K.; Gorman, J.R.; Lampic, C. Sexual dysfunction and reproductive concerns in young women with breast cancer: Type, prevalence, and predictors of problems. Psychooncology 2018, 27, 2770–2777. [Google Scholar] [CrossRef] [PubMed]
- Pintado Cucarella, M.S.P. Bienestar Emocional, Imagen Corporal, Autoestima y Sexualidad en Mujeres con Cáncer de Mama. Ph.D. Thesis, Universitat de València, Departamento de Personalidad, Evaluación y Tratamientos Psicológicos, Valencia, Spain, 2013. [Google Scholar]
- Valverde, M.; Nieto, R.; Gutiérrez, L.A. Imagen corporal y autoestima en mujeres mastectomizadas. Psicooncología 2014, 11, 45–57. [Google Scholar]
- Bratovcic, V.; Mikic, B.; Kostovski, Z.; Teskeredzic, A.; Tanovic, I. Relations between Different Dimensions of Self-Perception, Self-Esteem and Body Mass Index of Female Students. Int. J. Morphol. 2015, 33, 1338–1342. [Google Scholar] [CrossRef]
- Gillen, M.M. Associations between positive body image and indicators of men’s and women’s mental and physical health. Body Image 2015, 13, 67–74. [Google Scholar] [CrossRef]
- Sebastián, J.; Manos, D.; Bueno, M.J.; Mateos, N. Body image and self-esteem in women with breast cancer participating in a psychosocial intervention program. Clin. Health 2008, 18, 137–161. [Google Scholar]
- Abrahams, H.J.G.; Gielissen, M.F.M.; Verhagen, C.; Knoop, H. The relationship of fatigue in breast cancer survivors with quality of life and factors to address in psychological interventions: A systematic review. Clin. Psychol. Rev. 2018, 63, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Carreira, H.; Williams, R.; Dempsey, H. Quality of life and mental health in breast cancer survivors compared with non-cancer controls: A study of patient-reported outcomes in the United Kingdom. J. Cancer Surviv. 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Pintado, S. Self-concept and emotional well-being in patients with breast cancer. Rev. Iberoam. Psicol. Salud 2017, 8, 76–84. [Google Scholar] [CrossRef]
- Taylor, S.E. (Ed.) Manejo de enfermedades crónicas. In Psicología de la Salud, 6th ed.; McGraw Hill Interamericana: México, México, 2007; pp. 286–312. [Google Scholar]
- Cash, T.F. Body-image attitudes: Evaluation, investment, and affect. Percept. Mot. Skills 1994, 78, 1168–1170. [Google Scholar] [CrossRef]
- Cash, T. Encyclopedia of Body Image and Human Appearance; Elsevier: London, UK, 2012. [Google Scholar]
- Cash, T.F.; Pruzinsky, T.E. Body Images: Development, Deviance, and Change; Guilford Press: New York, NY, USA, 1990. [Google Scholar]
- Mock, V. Body image in women treated for breast cancer. Nurs. Res. 1993, 42, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Brandão, T.; Schulz, M.S.; Matos, P.M. Psychological adjustment after breast cancer: A systematic review of longitudinal studies. Psychooncology 2017, 26, 917–926. [Google Scholar] [CrossRef]
- Davis, C.; Tami, P.; Ramsay, D.; Melanson, L.; MacLean, L.; Nersesian, S.; Ramjeesingh, R. Body image in older breast cancer survivors: A systematic review. Psychooncology 2020, 29, 823–832. [Google Scholar] [CrossRef]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton University Press: Princeton, NJ, USA, 1965. [Google Scholar]
- Koçan, S.; Gürsoy, A. Body image of women with breast cancer after mastectomy: A qualitative research. J. Breast Health 2016, 12, 145–150. [Google Scholar] [CrossRef]
- Porroche-Escudero, A.; Coll-Planas, G.; Riba, C. Cicatrices (in)visibles. Perspectivas feministas sobre el cáncer de mama. In Influencia de la Salud Laboral y El Medio Ambiente en el Cáncer de Mama; Valls-Llobet, C., Ed.; Vic: Eumo Editorial: Bellaterra, Spain, 2017; pp. 85–94. [Google Scholar]
- Porroche-Escudero, A.; Arrieta, B. Deseo sexual, vivencias corporales y reivindicaciones médicas en materia de cáncer de mama. In Cicatrices (in)Visibles. Perspectivas Feministas Sobre el Cáncer de Mama; Porroche-Escudero, A., Coll-Planas, G., Riba, C., Eds.; Vic: Eumo Editorial: Bellaterra, Spain, 2017; pp. 131–140. [Google Scholar]
- Carver, C.S.; Pozo-Kaderman, C.; Price, A.A.; Noriega, V.; Harris, S.D.; Derhagopian, R.P.; Robinson, D.S.; Moffatt, F.L. Concern about aspects of body image and adjustment to early stage breast cancer. Psychosom. Med. 1998, 60, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Carminatti, M.; Boing, L.; Leite, B.; Sperandio, F.; Korpalski, T.; Fretta, T.; Guimarães, A. Effects of belly dancing on body image and self-esteem in women with breast cancer—Pilot study. Rev. Bras. Med. Esporte. 2019, 25, 464–468. [Google Scholar] [CrossRef]
- Coll-Planas, G.; Visa, M. The wounded blogger: Analysis of narratives by women with breast cancer. Sociol. Health Illn. 2016, 38, 884–898. [Google Scholar] [CrossRef][Green Version]
- Menon, A.S.; O’Mahony, M. Women’s body image following mastectomy: Snap shots of their daily lives. Appl. Nurs. Res. 2019, 47, 4–9. [Google Scholar] [CrossRef]
- Villarreal-Garza, C.; Martinez-Cannon, B.A.; Platas, A.; Mohar, A.; Partridge, A.H.; Gil-Moran, A.; Lopez-Aguirre, Y.E. Fertility concerns among breast cancer patients in Mexico. Breast 2017, 33, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Sebastián, J.; Bueno, M.J.; Mateos, N. Apoyo Emocional y Calidad de Vida en Mujeres Con Cáncer de Mama; Ministerio de Trabajo y Asuntos Sociales, Instituto de la Mujer: Madrid, India, 2002. [Google Scholar]
- Fobair, P.; Stewart, S.L.; Chang, S.; D’Onofrio, C.; Banks, P.J.; Bloom, J.R. Body image and sexual problems in young women with breast cancer. Psychooncology 2006, 15, 579–594. [Google Scholar] [CrossRef]
- Kovačević, P.; Miljković, S.; Višnjić, A.; Kozarski, J.; Janković, R. Quality of Life Indicators in Patients Operated on for Breast Cancer in Relation to the Type of Surgery—A Retrospective Cohort Study of Women in Serbia. Medicina 2020, 56, 402. [Google Scholar] [CrossRef]
- Prates, A.C.L.; Freitas-Junior, R.; Prates, M.F.O.; Veloso, M.D.F.; Barros, N.D.M. Influence of body image in women undergoing treatment for breast cancer. Rev. Bras. Ginecol. Obstet. 2017, 39, 175–183. [Google Scholar] [CrossRef]
- Bardot, J.; Magalon, G.; Mazzola, R.F. History of breast cancer reconstruction treatment. Ann. Chir. Plast. Esthet. 2018, 63, 363–369. [Google Scholar] [CrossRef]
- Teo, I.; Reece, G.P.; Christie, I.C.; Guindani, M.; Markey, M.K.; Heinberg, L.J.; Crosby, M.A.; Fingeret, M.C. Body image and quality of life of breast cancer patients: Influence of timing and stage of breast reconstruction. Psychooncology 2016, 25, 1106–1112. [Google Scholar] [CrossRef]
- Lagendijk, M.; van Egdom, L.S.E.; van Veen, F.E.E.; Vos, E.L.; Mureau, M.A.M.; van Leeuwen, N.; Hazelzet, J.A.; Lingsma, H.F.; Koppert, L.B. Patient-reported outcome measures may add value in breast cancer surgery. Ann. Surg. Oncol. 2018, 25, 3563–3571. [Google Scholar] [CrossRef] [PubMed]
- Amaral, A.C.S.; Medeiros, A.D.S.F.; Araújo, A.C.D.M.R.; Ana, A.A.D.S.; Hudson, T.A.; Ferreira, M.E.C. Apreciação corporal e aspectos associados entre adolescentes e mulheres jovens. J. Bras. Psiquiatr. 2019, 68, 16–22. [Google Scholar] [CrossRef]
- Olchowska-Kotala, A. Body esteem and self-esteem in middle-aged women. J. Women Aging 2018, 30, 417–427. [Google Scholar] [CrossRef] [PubMed]
- Pop, C. Self-Esteem and Body Image Perception in a Sample of University Students. Eur. J. Educ. Res. 2016, 64, 31–44. [Google Scholar] [CrossRef]
- Annunziata, M.A.; Giovannini, L.; Muzzatti, B. Assessing the body image: Relevance, application and instruments for oncological settings. Support. Care Cancer 2012, 20, 901–907. [Google Scholar] [CrossRef]
- Vicente Pardo, J.M.; López-Guillén García, A. Problemas y factores psicológicos en el retorno al trabajo tras incapacidad temporal prolongada por cáncer de mama. Med. Segur. Trab. 2017, 63, 245–259. [Google Scholar]
- Edelman, S.; Bell, D.R.; Kidman, A.D. A group cognitive behaviour therapy programme with metastatic breast cancer patients. Psychooncology 1999, 8, 295–305. [Google Scholar] [CrossRef]
- Cocker, K.I.; Bell, D.R.; Kidman, A.D. Cognitive behaviour therapy with advanced breast cancer patients: A brief report of a pilot study. Psychooncology 1994, 3, 233–237. [Google Scholar] [CrossRef]
- Christensen, D.N. Postmastectomy couple counseling: An outcome study of a structured treatment protocol. J. Sex. Marital. Ther. 1983, 9, 266–275. [Google Scholar] [CrossRef]
- Vos, P.J.; Visser, A.P.; Garssen, B.; Duivenvoorden, H.J.; de Haes, H.C. Effects of delayed psychosocial interventions versus early psychosocial interventions for women with early stage breast cancer. Patient Educ. Couns. 2006, 60, 212–219. [Google Scholar] [CrossRef]
- Brandão, T.; Mena, P. Eficácia das intervençoes psicológicas em grupo dirigidas a mulheres com cancro da mama: Uma revisão sistemática. Rev. Port. Saúde Pública 2015, 33, 98–106. [Google Scholar] [CrossRef]
- Kissane, D.W.; Bloch, S.; Miach, P.; Smith, G.C.; Seddon, A.; Keks, N. Cognitive-existential group therapy for patients with primary breast cancer—techniques and themes. Psychooncology 1997, 6, 25–33. [Google Scholar] [CrossRef]
- Vinogradov, S.; Yalom, I.D. Guía Breve de Psicoterapia de Grupo; Paidós Ibérica: Barcelona, Spain, 1996; pp. 2–44. [Google Scholar]
- Gottlieb, B.H. Marshalling Social Support: Format, Processes and Effects; Sage: Newbury Park, CA, USA, 1988. [Google Scholar]
- Esplen, M.J.; Warner, E.; Boquiren, V.; Wong, J.; Toner, B. Restoring body image after cancer (ReBIC): A group therapy intervention. Psychooncology 2020, 29, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Esplen, M.J.; Wong, J.; Warner, E.; Toner, B. Restoring body image after cancer (ReBIC): Results of a randomized controlled trial. J. Clin. Oncol. 2018, 36, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Trachtenberg, L.; Wong, J.; Rennie, H.; McLeod, D.; Leung, Y.; Warner, E.; Esplen, M.J. Feasibility and acceptability of i-Restoring Body Image after Cancer (i-ReBIC): A pilot trial for female cancer survivors. Psychooncology 2020, 29, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Goldov, N. The Effect of Medical Dance/Movement Therapy on Body Image Wellness in Women with Breast Cancer. Ph.D. Thesis, Argosy University, Seattle, WA, USA, 2011. [Google Scholar]
- Volders, J.H.; Haloua, M.H.; Krekel, N.M.A.; Negenborn, V.L.; Kolk, R.H.E.; Cardozo, A.L.; van Amerongen, A.T. Intraoperative ultrasound guidance in breast-conserving surgery shows superiority in oncological outcome, long-term cosmetic and patient-reported outcomes: Final outcomes of a randomized controlled trial (COBALT). Eur. J. Surg Oncol. 2017, 43, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Quintard, B.; Lakdja, F. Assessing the effect of beauty treatments on psychological distress, body image, and coping: A longitudinal study of patients undergoing surgical procedures for breast cancer. Psycho Oncol. 2008, 17, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Bellver-Pérez, A.; Peris-Juan, C.; Santaballa-Beltrán, A. Effectiveness of therapy group in women with localized breast cancer. Int. J. Clin. Health Psychol. 2019, 19, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Daneshvar, M.; Vakilian, K.; Zadeh-Emran, A.H.; Zadeh, R.H. The Effect of ACT on Self-Esteem and Self-efficacy of Women with Breast Cancer in Iran. Curr. Wom. Health Rev. 2020, 16, 74–80. [Google Scholar] [CrossRef]
- Landry, S.; Chasles, G.; Pointreau, Y.; Bourgeois, H.; Boyas, S. Influence of an adapted physical activity program on self-esteem and quality of life of breast cancer patients after mastectomy. Oncology 2018, 95, 188–191. [Google Scholar] [CrossRef]
- Mishra, S.I.; Scherer, R.W.; Geigle, P.M.; Berlanstein, D.R.; Topaloglu, O.; Gotay, C.C.; Snyder, C. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst. Rev. 2012, 8, CD007566. [Google Scholar] [CrossRef]
- Gokal, K.; Munir, F.; Wallis, D.; Ahmed, S.; Boiangiu, I.; Kancherla, K. Can physical activity help to maintain cognitive functioning and psychosocial well-being among breast cancer patients treated with chemotherapy? A randomised controlled trial: Study protocol. BMC Public Health 2015, 15, 414. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Franco, C.; Amutio, A.; Mañas, I.; Sánchez-Sánchez, L.C.; Mateos-Pérez, E. Improving psychosocial functioning in mastectomized women through a mindfulness-based program: Flow meditation. Int. J. Stress Manag. 2019, 27, 74–81. [Google Scholar] [CrossRef]
- Osypiuk, K.; Ligibel, J.; Giobbie-Hurder, A.; Vergara-Diaz, G.; Bonato, P.; Quinn, R.; Ng, W.; Wayne, P.M. Qigong Mind-Body Exercise as a Biopsychosocial Therapy for Persistent Post-Surgical Pain in Breast Cancer: A Pilot Study. Integr. Cancer Ther. 2020, 19, 1–12. [Google Scholar] [CrossRef]
- Elias, A.C.A.; Ricci, M.D.; Rodriguez, L.H.D.; Pinto, S.D.; Giglio, J.S.; Baracat, E.C. The biopsychosocial spiritual model applied to the treatment of women with breast cancer, through RIME intervention (relaxation, mental images, spirituality). Complement. Ther. Clin. Pract. 2015, 21, 1–6. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Helgeson, V.S.; Cohen, S.; Schulz, R.; Yasko, J. Education and peer discussion group interventions and adjustment to breast cancer. Arch. Gen. Psychiatry 1999, 56, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Lewis-Smith, H.; Diedrichs, P.C.; Harcourt, D. A pilot study of a body image intervention for breast cancer survivors. Body Image 2018, 27, 21–31. [Google Scholar] [CrossRef]
- Narváez, A.; Rubiños, C.; Cortés-Funes, F.; Gómez, R.; García, A. Evaluation of effectiveness of a group cognitive-behavioral therapy on body image, self-esteem, sexuality and distress in breast cancer patients. Psicooncologia 2008, 5, 93–102. [Google Scholar]
- Park, H.Y.; Kim, J.H.; Choi, S.; Kang, E.; Oh, S.; Kim, J.Y.; Kim, S.W. Psychological effects of a cosmetic education programme in patients with breast cancer. Eur. J. Cancer Care 2015, 24, 493–502. [Google Scholar] [CrossRef] [PubMed]
- Richard, A.; Harbeck, N.; Wuerstlein, R.; Wilhelm, F.H. Recover your smile: Effects of a beauty care intervention on depressive symptoms, quality of life, and self-esteem in patients with early breast cancer. Psychooncology 2019, 28, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, M. Rosenberg self-esteem scale (RSE). Acceptance and commitment therapy. Meas. Package 1965, 61, 18. [Google Scholar]
- Hopwood, P.; Fletcher, I.; Lee, A.; Al Ghazal, S. A body image scale for use with cancer patients. Eur. J. Cancer 2001, 37, 189–197. [Google Scholar] [CrossRef]
- Curbow, B.; Somerfield, M. Use of the Rosenberg Self-Esteem Scale with Adult Cancer Patients. J. Psychosoc. Oncol. 1991, 9, 113–131. [Google Scholar] [CrossRef]
- Vonz Collani, G.; Herzberg, P.Y. Eine revidierte Fassung der deutschsprachigen Skala zum Selbstwertgefühl von Rosenberg [A Revised Version of the German Adaptation of Rosenberg’s Self-Esteem Scale]. ZDDP 2003, 24, 3–7. [Google Scholar]
- Robins, R.W.; Hendin, H.M.; Trzesniewski, K.H. Measuring global self-esteem: Construct validation of a single-item measure and the Rosenberg Self-Esteem Scale. Pers. Soc. Psychol. Bull. 2001, 27, 151–161. [Google Scholar] [CrossRef]
- Berscheid, E.; Walster, E.; Bohrnstedt, G. Body Image: A Psychology Today questionnaire. Psychol. Today 1972, 6, 57–64. [Google Scholar]
- Cash, T.F. User’s Manual for the Multidimensional Body-Self Relations Questionnaire; Norfolk, V.A., Ed.; Old Dominion University: Norfolk, VA, USA, 2000. [Google Scholar]
- Fairburn, C.G.; Beglin, S.J. Assessment of eating disorders: Interview or self-report questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar]
- Rosen, J.C.; Srebnik, D.; Saltzberg, E.; Wendt, S. Development of a body image avoidance questionnaire. Psychol. Assess 1991, 31, 32–37. [Google Scholar] [CrossRef]
- Avalos, L.; Tylka, T.L.; Wood-Barcalow, N. The body appreciation scale: Development and psychometric evaluation. Body Image 2005, 2, 285–297. [Google Scholar] [CrossRef]
- McLean, S.A.; Paxton, S.J.; Wertheim, E.H. Factors associated with body dissatisfaction and disordered eating in women in midlife. Int. J. Eat. Disord. 2010, 43, 527–536. [Google Scholar] [CrossRef]
- Conçalves, C.O.; Tavares, M.C.G.; Campana, A.N.N.B.; Cabello, C. Validation of the instrument “Body image after breast cancer” in Brazil. Motriz. Rev. Educ. Fis. 2014, 20, 8–15. [Google Scholar]
- Tucker, L.A. Internal structure, factor satisfaction, and reliability of the Body Cathexis Scale. Percept. Mot. Skills 1981, 53, 891–896. [Google Scholar] [CrossRef]
- Schag, C.A.C.; Heinrich, R.L. CARES Cancer Rehabilitation Evaluation System; Cares Consultants: Santa Monica, CA, USA, 1988. [Google Scholar]
- Boing, L.; Baptista, F.; Pereira, G.S.; Sperandio, F.F.; Moratelli, J.; Cardoso, A.A.; de Azevedo Guimarães, A.C. Benefits of belly dance on quality of life, fatigue, and depressive symptoms in women with breast cancer–A pilot study of a non-randomised clinical trial. J. Bodyw. Mov. Ther. 2018, 22, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Villarini, M.; Acito, M.; Gianfredi, V.; Berrino, F.; Gargano, G.; Somaini, M.; Nucci, D.; Moretti, M.; Villarini, A. Validation of self-reported anthropometric measures and body mass index in a subcohort of the dianaweb population study. Clin. Breast Cancer 2019, 19, e511–e518. [Google Scholar] [CrossRef] [PubMed]
- Burton, N.W.; Pakenham, K.I.; Brown, W.J. Feasibility and effectiveness of psychosocial resilience training: A pilot study of the Ready program. Psychol. Health Med. 2010, 15, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Velasco, S. Sexos, Género y Salud. Teoría y Métodos Para La Práctica Y Programas De Salud; Minerva Ediciones: Madrid, Spain, 2009. [Google Scholar]
- Valls-Lobet, C. The science of difference the invisibility of women in health sciences. Mètode 2017, 7, 121–125. [Google Scholar]
- Ehrenreich, B. Welcome to Cancerland. Harper’s Mag. 2001, 303, 43–53. [Google Scholar]
- Watts, R.J.; Griffith, D.M.; Abdul-Adil, J. Sociopolitical development as an antidote for oppression—Theory and action. Am. J. Community Psychol. 1999, 27, 255–271. [Google Scholar] [CrossRef]
- Greco, C. Reconstrucción mamaria: ¿las múltiples formas de reconstruir la feminidad? Un análisis de las estrategias de construcción de la feminidad después de la mastectomía. In Cicatrices (in)Visibles. Perspectivas Feministas Sobre el Cáncer de Mama; Porroche-Escudero, G., Coll-Planas, G., Ribas, C., Eds.; Ediciones Bellatera: Barcelona, Spain, 2017; pp. 109–118. [Google Scholar]
- Downing, N.E.; Roush, K.L. From passive acceptance to active commitment: A model of feminist identity development for women. Couns. Psychol. 1985, 13, 695–709. [Google Scholar] [CrossRef]
- Bradt, J.; Shim, M.; Goodill, S.W. Dance/Movement therapy for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, S. Mujeres feministas en lucha contra el cáncer de mama: Lo personal y lo político. Anu. Psicol. 2008, 39, 23–29. [Google Scholar]
- Flay, B.R.; Biglan, A.; Boruch, R.F.; Castro, F.G.; Gottfredson, D.; Kellam, S.; Mościcki, E.K.; Schinke, S.; Valentine, J.C.; Ji, P. Standards of evidence: Criteria for efficacy, effectiveness and dissemination. Prev. Sci. 2005, 6, 151–175. [Google Scholar] [CrossRef] [PubMed]
- Helgeson, V.S.; Snyder, P.; Seltman, H. Psychological and Physical Adjustment to Breast Cancer Over 4 Years: Identifying Distinct Trajectories of Change. Health Psychol. 2004, 23, 3–15. [Google Scholar] [CrossRef]
- Hopwood, P. The assessment of body image in cancer patients. Eur. J. Cancer 1993, 2, 276–281. [Google Scholar] [CrossRef]
- Yurek, D.; Farrar, W.; Andersen, B.L. Breast cancer surgery: Comparing surgical groups and determining individual differences in postoperative sexuality and body change stress. J. Consult. Clin. Psychol. 2000, 68, 697. [Google Scholar] [CrossRef]
- Wilkinson, S. Women with breast cancer talking causes: Comparing content, biographical and discursive analyses. Fem. Psychol. 2000, 10, 431–460. [Google Scholar] [CrossRef]
- Brems, S.; Griffiths, M. Health women’s way: Learning to listen. In The Health of Women: A Global Perspective; Koblinsky, M., Timyan, J., Gay, J., Eds.; Westview Press: Boulder, CO, USA, 1993; pp. 255–273. [Google Scholar]
- Bloom, J.R.; Stewart, S.L.; Chang, S.; Banks, P.J. Then and now: Quality of life of young breast cancer survivors. Psychooncology 2004, 13, 147–160. [Google Scholar] [CrossRef]
- Moyer, A.; Salovey, P. Psychosocial sequelae of breast cancer and its treatment. Ann. Behav. Med. 1996, 18, 110–125. [Google Scholar] [CrossRef] [PubMed]
- Avis, N.; Crawford, S.; Manuel, J. Psychosocial problems among younger women with breast cancer. Psychooncology 2004, 13, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Vos, P.J.; Garssen, B.; Visser, A.P.; Duivenvoorden, H.J.; De Haes, H. Psychosocial intervention for women with primary, non-metastatic breast cancer: A comparison between participants and nonparticipants. Psychother. Psychosom. 2004, 73, 276–285. [Google Scholar] [CrossRef] [PubMed]
| Database | Search Strategies |
|---|---|
| Web of Science (WOS) | Topic: ((“Breast Cancer” OR “Breast Cancer Women”) AND “Self-esteem” AND “Body image” AND (“Therapy” OR “Intervention”)) Refined by: Languages: (ENGLISH OR SPANISH) Results: 68 records |
| Scopus | TITLE-ABS-KEY ((“Breast Cancer” OR “Breast Cancer Women”) AND “Self-esteem” AND “Body image” AND (“Therapy” OR “Intervention”)) AND (LIMIT-TO (LANGUAGE, “English”) OR LIMIT-TO (LANGUAGE, “Spanish”)) Results: 47 records |
| PubMed | (“Breast Cancer” OR “Breast Cancer Women”) AND “Self-esteem” AND “Body image” AND (“Therapy” OR “Intervention”)) Filters: English, Spanish Results: 30 records |
| PsycINFO | ((“Breast Cancer” OR “Breast Cancer Women”) AND “Self-esteem” AND “Body image” AND (“Therapy” OR “Intervention”)) AND la.exact(“ENG” OR “SPA”) Results: 25 records |
| PsycArticles | ((“Breast Cancer” OR “Breast Cancer Women”) AND “Self-esteem” AND “Body image” AND (“Therapy” OR “Intervention”)) AND la.exact(“ENG” OR “SPA”) Results: 117 records |
| P | I | C | O | S | |
|---|---|---|---|---|---|
| I | Women with BC (early diagnosed, in treatment or long-term patient, survivors) | Psychological, physical, spiritual, beauty care, arts and dance interventions or therapies | CG or comparison between pre-post after intervention in the IG | Improving self-esteem and BI | Experimental and quasi-experimental design with pre-post measures |
| E | Participants with other type of cancers, or other illnessess | Surgery interventions and systemic BC therapies | No results of comparisons | Other outcomes/Self-esteem or BI separately with other outcomes | Observational, comparative, and validation scale studies/Systematic reviews/Meta-analyses/Clinical guides/Study protocols |
| Study | Design | Scope | Participants | Measures | Details of Implemented Interventions | Results |
|---|---|---|---|---|---|---|
| Study 1. Carminatti et al., (2019) [35] | NRCT Pretest and posttest design | Influence of belly dancing on BI and self-esteem. | 19 women diagnosed with BC (m.a. = 54.55) 11 in IG (m.a.: not mentioned) 8 in CG (m.a.: not mentioned) | Body image: BIBCQ (Body Image After Breast Cancer Questionnaire). Self-esteem: RSE (Rosenberg Self-Esteem Scale). | Type: Belly dance intervention Classification: Physical activity therapy. Extent: 24 sessions in 12 weeks (2 sessions p/w). Duration: 1 h/session. Assess other outcome variables: no Contents: (1) Warm-up initial stretching; (2) Main part; (3) Relaxation. Who implements interventions: not mentioned | Significant differences were observed between pre- and post- intervention in BI, but not in self-esteem. Improvement of femininity and confidence were reported by spontaneous reports during the classes. |
| Study 2. Dibbel-Hope (2000) [9] | RCT Pretest and posttest design | Influence of AMTG in the levels of psychological adaptation; their sustainability over time. | 33 women diagnosed with BC (mean age = 54.7) geographically separated according to where they lived into Northern (1) or Southern (2) areas. They were randomly assigned: 10–12 women in IG1 (m.a.: not mentioned) 10–12 women in IG2 (m.a.: not mentioned) CG1: not mentioned CG2: not mentioned | Quantitative: Body-image and Self-esteem: BWB (Borscht-Walter-Bohrnstedt Body-Image Scale). Qualitative: Interviews and Written program evaluation. | Type: Dance/Movement Therapy Classification: Physical activity therapy. Extent: 6 sessions in 6 weeks (1 session p/w). Duration: 3 h/session. Assess other outcome variables: yes. Contents: (1) Circle to check-in their life that week; (2) movement group; (3) discussion group and closing ritual. Who implements interventions: Therapists from the dance/movement therapy community who teach Authentic Movement locally, nationally and internationally. | Quantitative results: There were no observed significant improvements in BI and Self-esteem. CG1 reported greater dissatisfaction with BI than did the CG2 (sociodemographic differences) IG2 showed higher levels of BI (satisfaction with the body) than CG2 (effects pre-post intervention). Age and past experience with dance and sports predict satisfaction with BI and self-esteem. No relationship between type of medical treatment and BI. Qualitative results: After AMTG, participants showed strongly self-perceived improvement in BI and self-esteem (increase in awareness, acceptance and appreciation of the body and the self). |
| Study 3. Helgeson et al., (1999) [74] | RCT Pretest, posttest and follow-up | Effects of education-based and peer discussion-based group intervention in women with BC | 312 BC women (m.a.: 48.25) randomly assigned: 79 women in Education Groups 74 women in Peer-Discussion Groups 82 women in Combination Groups 77 women in CG | Self-esteem: RSE (Rosenberg Self-Esteem Scale). Body Image: 14-item body-image scale based on the Cancer Rehabilitation Evaluation Systems (CARES). | Type: Education and peer-discussion group interventions Classification: Group therapy. Extent: 8 sessions in 8 weeks (1 session p/w). Duration: Education (45min./session); Peer discussion (60min./session); Combination (135min./session); CG did not assist to intervention groups. Assess other outcome variables: yes. Contents of sessions: Education (adverse effects of chemotherapy, nutrition, exercise, body image, relationships/sexuality, between others; Peer Discussion (promotion of feelings of acceptance and encouragement to expression of feelings and confrontation of problems; Combination (the combined intervention was a sequential combination, beginning with education and ending with peer discussion contents). Who implements interventions: an oncology nurse and an oncology social worker. | Before group interventions, patients of Education Groups showed higher self-esteem and better BI. There was no evidence of benefits from Peer discussion group interventions. |
| Study 4. Lewis-Smith et al., (2018) [75] | Quasi-experimental pretest-posttest and follow-up design | Effects of a CBT based intervention in BC survivors. | 22 women (m.a.: 51.55 years) who had completed active treatment for BC. 9 in IG1 12 in IG2 | Quantitative: Body dissatisfaction (cancer-specific): Hopwood Scale. Body dissatisfaction (general): MBSRQ Weight and Shape Concern: EDE-Q Body image avoidance: BIAQ Body appreciation: Body Appreciation Scale. Acceptance of aging-related appearance changes: PARCA. Body-related self-care-attitude: Body-Related Self-Care Scale. Appearance investment: Self-Objectification Questionnaire. Internalization of appearance ideals: SATAQ-3. Appearance comparisons: PACS- Body image-related avoidance of intimacy: RFH and CAR Intimacy Scale. Self-esteem: The Single-Item Self-Esteem Scale. Qualitative: Focus groups and interviews | Type: Cognitive-Behavioral Therapy based-intervention. Adapted BI intervention ‘Accepting your Body after Cancer’. Classification: Group therapy. Extent: 7 sessions in 7 weeks (1 session p/w). Duration: 2 h/session. Assess other outcome variables: yes Contents: Session 1 (body image), Session 2 (CBT, anxiety, body image and self-esteem); Session 3 (stopping negative body-related self-talk, balanced thoughts, self-care activity schedule, body function and movement; Session 4 (sociocultural pressures for women in midlife, internalization of the youthful-thin ideal, body comparisons, body nurture); Session 5 (exploration of relationships and intimacy; managing people’s reaction; cognitive restructuring process; physical activity and movement); Session 6 (Core beliefs, Modifying mistaken beliefs), Mindful eating, relaxation exercise); Session 7 (positive body affirmations, reducing the chances of a setback, dealing with a setback, future plans). Who applies interventions: Clinical psychologist and peer BC nurse specialists. Type: focus groups Number of groups: 6 Participants: 3–5 women each Duration: 3 h. including short breaks. Contents: opinions in relation to each session’s content. Who implements interventions: Clinical psychologist and peer BC nurse specialists. | Quantitative results: Significant improvements were identified at post-test and sustained, or emerged at 1-month follow-up, iin the majority of the BI measures and self-esteem. There were no significant improvements in body-related self-care attitude at either post-test or follow-up. Qualitative results: Most participants felt the intervention was beneficial and had improved their BI. |
| Study 5. Narváez et al., (2008) [76] | RCT Pretest and posttest design | Effectiveness of a CBT in BC Survivors. | 38 women (m.a.: 50.2 years) who have been diagnosed with BC and have been operated on for a mastectomy in the last three years. 19 in IG (m.a.: not mentioned) 19 in a CG (m.a.: not mentioned) | Body image: Hopwood scale. Self-esteem: RSE (Rosenberg Self-Esteem Scale). | Type: Cognitive-Behavioral Therapy Classification: Group Therapy. Extent: 9 sessions in 9 weeks (1 session p/w). Duration: 1.5 h/session. Assess other outcome variables: yes. Contents: mood status (2 sessions), BI and self-esteem (4 sessions), sexuality (2 sessions) and closing with the tests (1 session). Who implements interventions: not mentioned. | After the treatment, there were observed statistically significant beneficial differences between IG and CG in self-esteem. However, while there were observed improvements in BI, they were not statistically significant. |
| Study 6. Park et al., (2015) [77] | Prospective NRCT Pretest, posttest and follow-up | Effects of a cosmetic program on patients who had undergone a mastectomy for BC. | 31 women in IG (m.a.: 43.97 years) 29 women in CG (m.a.: 45.41 years) | Body image: BCS (Body Cathexis Scale). Self-esteem: RSE (Rosenberg Self-Esteem Scale). | Type: Cosmetic education program ‘Make up your life’ Classification: Cosmetic and beauty treatments Extent: 1-day session. Duration: 2 h. Assess other outcome variables: yes. Contents: useful skills, including skin care, facial massage, applying make-up, hair care for depilation, and dressing strategies to preserve physical appearance). Each woman received a free make-up kit and practiced each of the techniques. After applying their make-up, the patients and professionals discussed and shared experiences related to changes in their appearance through the program. Finally, participants took pictures of their made-over appearance. Who implements interventions: two professional beauty specialists. | There were observed positive changes in BI and self-esteem, but were not significant. |
| Study 7. Richard et al., (2019) [78] | RCT Pretest, posttest and follow-up | Effects of a beauty care intervention in patients with early BC. | 20 women with BC in IG (m.a.: 39.6 years) 19 women with BC in CG (m.a.: 37.4 years) | Body image: BIS (Body Image Scale). Self-esteem: RSE (Rosenberg Self-Esteem Scale). | Type: Beauty care intervention. Classification: Cosmetic and beauty treatments Extent: 1-day session. Duration: 4 h. Assess other outcome variables: yes. Contents: makeup workshop, a photo shooting, and of receiving professionally edited portrait and upper-body photos Who implements interventions: professional beauty specialists. | The intervention had a positive effect on the women’s BI, and self-esteem. No differences between CG and IG were found at the pretest. At posttest 1 and 2, patients of IG reported higher self-esteem than at pretest, as well as than CG. This change was maintained in the follow-up measures. From pretest to posttests (1 and 2) both groups reported increases in BI, irrespective of intervention. These changes decreased as the follow-up tests were passed. |
| Study 8. Sebastián et al., (2008) [19] | NRCT Pretest, posttest and follow-up | Effectiveness of an intervention program psychosocial | 188 women (m.a.: 48 years) 107 women in IG 81 women in CG | Body image: Hopwood scale. Self-esteem: RSE (Rosenberg Self-Esteem Scale). | Type: Psychosocial intervention program. Classification: Group therapy. Extent: 14 sessions in 14 weeks (1session p/w). Duration: 2 h/session. Assess other outcome variables: no. Contents: are divided in five blocks: (1) Preparation for Chemotherapy (1 session); (2) Education for Health (5 sessions); (3) Body image (5 partial sessions); stress management and personal coping skills (5 partial sessions) and communication skills and setting of goals (3 partial sessions). Who implements interventions: two female psychologists. | Women who participated in the program, at 6-month follow up, showed more positive BI and higher self-esteem than women who did not participate. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morales-Sánchez, L.; Luque-Ribelles, V.; Gil-Olarte, P.; Ruiz-González, P.; Guil, R. Enhancing Self-Esteem and Body Image of Breast Cancer Women through Interventions: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 1640. https://doi.org/10.3390/ijerph18041640
Morales-Sánchez L, Luque-Ribelles V, Gil-Olarte P, Ruiz-González P, Guil R. Enhancing Self-Esteem and Body Image of Breast Cancer Women through Interventions: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(4):1640. https://doi.org/10.3390/ijerph18041640
Chicago/Turabian StyleMorales-Sánchez, Lucía, Violeta Luque-Ribelles, Paloma Gil-Olarte, Paula Ruiz-González, and Rocío Guil. 2021. "Enhancing Self-Esteem and Body Image of Breast Cancer Women through Interventions: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 4: 1640. https://doi.org/10.3390/ijerph18041640
APA StyleMorales-Sánchez, L., Luque-Ribelles, V., Gil-Olarte, P., Ruiz-González, P., & Guil, R. (2021). Enhancing Self-Esteem and Body Image of Breast Cancer Women through Interventions: A Systematic Review. International Journal of Environmental Research and Public Health, 18(4), 1640. https://doi.org/10.3390/ijerph18041640









