Comparison of Learning Transfer Using Simulation Problem-Based Learning and Demonstration: An Application of Papanicolaou Smear Nursing Education
Abstract
1. Introduction
1.1. Aims
1.2. Research Hypotheses
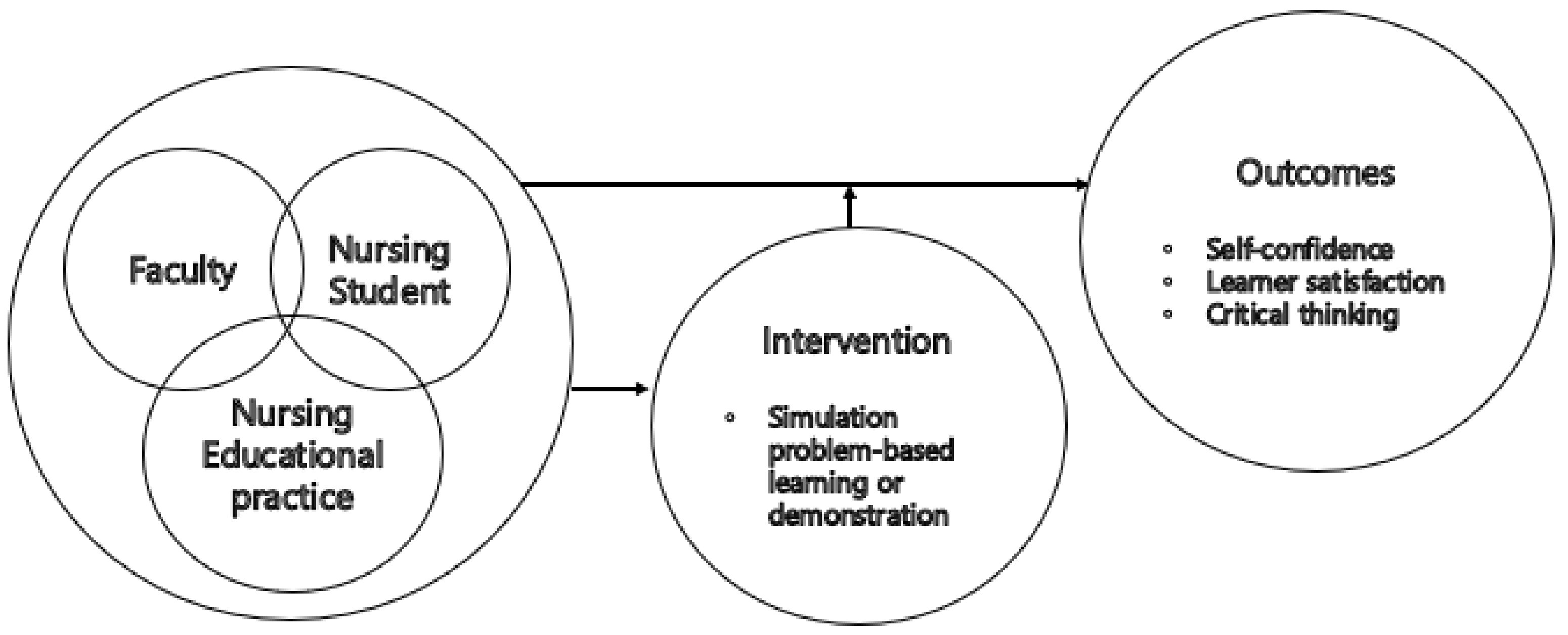
2. Materials and Methods
2.1. Research Design
2.2. Subjects and Setting
2.3. Research Procedures
2.3.1. Preliminary Assessment
2.3.2. Interventions: Simulation Problem-Based Learning (S-PBL) vs. Demonstration
2.3.3. Outcome Assessment
2.4. Data Collection
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
3.1. Homogeneity Test
3.2. Correlation between Variables
3.3. Effects of Intervention
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baharum, N.N.; Ariffin, F.; Isa, M.R.; Tin, S.T. Health literacy, knowledge on cervical cancer and pap smear and its influence on pre-marital Malay Muslim women attitude towards pap smear. Asian Pac. J. Cancer Prevent. 2020, 21, 2021. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Health Insurance Review & Assessment Service. Open Access Big Data Platform Service. Available online: http://opendata.hira.or.kr/op/opc/olapMfrnIntrsIlnsInfo.do (accessed on 31 December 2020).
- Kang, M.; Ha, S.Y.; Cho, H.Y.; Chung, D.H.; Kim, N.R.; An, J.; Lee, S.; Seok, J.Y.; Jeong, J. Comparison of Papanicolaou smear and human papillomavirus (HPV) test as cervical screening tools: Can we rely on HPV test alone as a screening method? An 11-year retrospective experience at a single institution. J. Pathol. Transl. Med. 2020, 54, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Jayapalan, S.; Bindu, R.S. Papanicolaou smear: A diagnostic aid in sexually transmitted infections. Indian J. Sex. Transm. Dis. AIDS 2020, 41, 143. [Google Scholar] [CrossRef]
- Cannon-Diehl, M.R. Simulation in healthcare and nursing: State of the science. Crit. Care Nurs. Q. 2009, 32, 128–136. [Google Scholar] [CrossRef]
- Suh, E. Development of a conceptual framework for nursing simulation education utilizing human patient simulators and standardized patients. J. Korean Acad. Soc. Nurs. Educ. 2012, 18, 206–219. [Google Scholar] [CrossRef]
- Lasater, K. High-fidelity simulation and the development of clinical judgment: Students’ experiences. J. Nurs. Educ. 2007, 46, 269–276. [Google Scholar] [CrossRef]
- Bambini, D.; Washburn, J.; Perkins, R. Outcomes of clinical simulation for novice nursing students: Communication, confidence, clinical judgment. Nurs. Educ. Perspect. 2009, 30, 79–82. [Google Scholar]
- Ryoo, E.N.; Ha, E.H.; Cho, J.Y. Comparison of learning effects using high-fidelity and multi-mode simulation: An application of emergency care for a patient with cardiac arrest. J. Korean Acad. Nurs. 2013, 43, 185–193. [Google Scholar] [CrossRef]
- Kim, M.N.; Cho Chung, H.I.; Kim, Y.A. A meta-analysis of the effect of simulation-based education for delivery nursing in Korea. J. Korean Soc. Matern. Child. Health 2016, 20, 297–309. [Google Scholar]
- Kim, M.; Ha, J. Simulation-based education program on postpartum hemorrhage for nursing students. Korean J. Women Health Nurs. 2020, 26, 19–27. [Google Scholar] [CrossRef]
- Jeffries, P.R. A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nurs. Educ. Perspect. 2005, 26, 96–103. [Google Scholar]
- Hong, S.; Park, B.; Lee, H.; Lee, J.H. Analysis and evaluation of the national league for nursing/Jeffries Simulation Theory. J. Korean Soc. Simul. Nurs. 2019, 7, 27–44. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Chung, C.W.; Kim, H.S.; Park, Y.S. Effects of high-fidelity simulation-based education on maternity nursing. Perspect. Nurs. Sci. 2011, 8, 86–96. [Google Scholar]
- Yun, S.Y.; Choi, J.Y. A comparative study on learning outcomes according to the integration sequences of S-PBL in nursing students: Randomized crossover design. J. Korean Acad. Nurs. 2019, 49, 92–103. [Google Scholar] [CrossRef]
- Benner, P. From Novice to Expert: Excellence and Power in Clinical Nursing Practice; Addison-Wesley Publishing Co., Nursing Division: Menlo Park, CA, USA, 1984. [Google Scholar]
- Solli, H.; Haukedal, T.A.; Husebø, S.E.; Reierson, I.Å. The art of balancing: The facilitator’s role in briefing in simulation-based learning from the perspective of nursing students–a qualitative study. BMC Nurs. 2020, 19, 99. [Google Scholar] [CrossRef] [PubMed]
- Von Baeyer, C.L. Children’s self-reports of pain intensity: Scale selection, limitations and interpretation. Pain Res. Manag. 2006, 11, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Vivekananda-Schmidt, P.; Lewis, M.; Hassell, A.B.; Coady, D.; Walker, D.; Kay, L.; Rahman, A. Validation of MSAT: An instrument to measure medical students’ self-assessed confidence in musculoskeletal examination skills. Med. Educ. 2007, 41, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Yoo, M.S. Development of standardized patient managed instruction for a fundamentals of nursing course. Ph.D. Thesis, Yonsei University, Seoul, Korea, 2000. [Google Scholar]
- Yoon, J. Development of an instrument for the measurement of critical thinking disposition. Ph.D. Thesis, Graduate School of Catholic University, Seoul, Korea, 2004. [Google Scholar]
- Son, H.K.; Kim, D.H. Effect of SEGUE-based communication education on nursing simulation practice: A quasi-experimental design. Contemp. Nurse 2019, 55, 330–340. [Google Scholar] [CrossRef]
- Bucknall, T.K.; Forbes, H.; Phillips, N.M.; Hewitt, N.A.; Cooper, S.; Bogossian, F.; First2Act Investigators. An analysis of nursing students’ decision-making in teams during simulations of acute patient deterioration. J. Adv. Nurs. 2016, 72, 2482–2494. [Google Scholar] [CrossRef]
- Zapko, K.A.; Ferranto, M.L.G.; Blasiman, R.; Shelestak, D. Evaluating best educational practices, student satisfaction, and self-confidence in simulation: A descriptive study. Nurse Educ. Today 2018, 60, 28–34. [Google Scholar] [CrossRef]
- Hogg, G.; Miller, D. The effects of an enhanced simulation programme on medical students’ confidence responding to clinical deterioration. Nurse Educ. Today 2016, 16, 161. [Google Scholar] [CrossRef] [PubMed]
- Ha, E.H.; Lim, E.J. Peer-led written debriefing versus instructor-led oral debriefing: Using multimode simulation. Clin. Simul. Nurs. 2018, 18, 38–46. [Google Scholar] [CrossRef]
- Brannan, J.D.; White, A.; Bezanson, J.L. Simulator effects on cognitive skills and confidence levels. J. Nurs. Educ. 2008, 47, 495–500. [Google Scholar] [CrossRef]
- Massoth, C.; Röder, H.; Ohlenburg, H.; Hessler, M.; Zarbock, A.; Pöpping, D.M.; Wenk, M. High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Med. Educ. 2019, 19, 29. [Google Scholar] [CrossRef] [PubMed]
- Cooper, S.; Cant, R.P.; Bogossian, F.; Bucknall, T.; Hopmans, R. Doing the right thing at the right time: Assessing responses to patient deterioration in electronic simulation scenarios using Course-of-Action analysis. Comput. Inform. Nurs. CIN 2015, 33, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Cooper, S.J.; Hopmans, R.; Cant, R.P.; Bogossian, F.; Giannis, A.; King, R. Deteriorating patients: Global reach and impact of an e-simulation program. Clin. Simul. Nurs. 2017, 13, 562–572. [Google Scholar] [CrossRef]
- Shin, H.; Kim, M.J. Evaluation of an integrated simulation courseware in a pediatric nursing practicum. J. Nurs. Educ. 2014, 53, 589–594. [Google Scholar] [CrossRef]
- Park, S.A.; Kim, H.Y. Development and effects of a labor nursing education program using a high-fidelity simulator for nursing students in Korea. Korean J. Women Health Nurs. 2020, 26, 240–249. [Google Scholar] [CrossRef]
- Bosse, H.M.; Schultz, J.H.; Nickel, M.; Lutz, T.; Möltner, A.; Jünger, J.; Huwendiek, S.; Nikendei, C. The effect of using standardized patients or peer role play on ratings of undergraduate communication training: A randomized controlled trial. Patient Educ. Couns. 2012, 87, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, J. The impact of simulation prebriefing on perceptions of overall effectiveness, learning, and self-confidence in nursing students. Nurs. Educ. Perspect. 2017, 38, 119–125. [Google Scholar] [CrossRef]
- Miles, D.A. Simulation learning and transfer in undergraduate nursing education: A grounded theory study. J. Nurs. Educ. 2018, 57, 347–353. [Google Scholar] [CrossRef]


| Category | Item |
|---|---|
| Nursing scenario | A patient (F/20 years old) visited an obstetrics and gynecology outpatient clinic with her mother for cervical cancer screening. Provide Pap smear nursing to the patient who is worried about her first gynecological examination. |
| Attitude | 1. Wash hands with water and soap |
| 2. Introduce yourself to the patient | |
| 3. Check who is the subject of examination between the patient and guardian | |
| 4. Ask the patient’s name with an open-ended question to confirm the patient and verify the patient (name, registration number) by comparing hospitalization ID bracelet with the patient list (or prescription form) | |
| 5. Provide an explanation before every treatment | |
| 6. Listen to the patient and answer the questions accurately and clearly | |
| Assessment | 7. Assess information related to Pap smear (e.g., regular check-ups, sexual experience, health history, obstetric history, etc.) |
| 8. Assess whether it is possible to test for cervical cancer today (e.g., vaginal insertion, vaginal washing, sexual interaction, menstruation, etc.) | |
| 9. Assess patient’s anxiety | |
| Skill | Perform treatment based on the assessed information |
| 10. Provide information on Pap smear examination (e.g., undressing and changing into skirt for examination, lithotomy position, etc.) | |
| 11. Protect the privacy of the patient (e.g., covering the examination area with a screen or sheet, etc.) | |
| 12. Provide emotional support to the patient | |
| 13. Perform aseptic techniques | |
| 14. Perform Pap smear test | |
| 15. Explain to the patient about the current situation and how the results of the test will be delivered | |
| Communication | 16. When necessary, communicate effectively with multi-disciplinary team members (nurse or doctor) (e.g., Situation-Background-Assessment-Recommendation) |
| 17. Update records (e.g., Overall condition of the patient, nursing performance, etc.) |
| Characteristics | Categories/Range | Mean (SD 3)/Frequency (%) | t/p | |
|---|---|---|---|---|
| Exp. 1 (n = 52) | Cont. 2 (n = 53) | |||
| age (years) | 22.54 (2.84) | 22.08 (1.99) | 0.97 (0.335) | |
| gender | female | 41 (78.8) | 44 (83.0) | 0.54 (0.590) |
| male | 11 (21.2) | 9 (17.0) | ||
| motivationfor major choice | employment | 12 (23.1) | 18 (34.0) | 1.72 (0.088) |
| other’s recommendation | 8 (15.4) | 12 (22.6) | ||
| one’s own will | 32 (61.5) | 23 (43.4) | ||
| satisfaction with major | very satisfied | 8 (15.4) | 9 (17.0) | 0.83 (0.409) |
| satisfied | 29 (55.8) | 31 (58.5) | ||
| moderate | 13 (25.0) | 13 (24.5) | ||
| unsatisfied | 1 (1.9) | 0 (0.0) | ||
| very unsatisfied | 1 (1.9) | 0 (0.0) | ||
| clinical practice satisfaction | very satisfied | 4 (7.7) | 7 (13.2) | 1.93 (0.057) |
| satisfied | 23 (44.2) | 28 (52.8) | ||
| moderate | 18 (34.6) | 16 (30.2) | ||
| unsatisfied | 7 (13.5) | 2 (3.8) | ||
| very unsatisfied | 0 (0.0) | 0 (0.0) | ||
| academic achievement | very high | 2 (3.8) | 7 (13.2) | 0.94 (0.348) |
| high | 12 (23.1) | 14 (26.4) | ||
| moderate | 32 (61.5) | 21 (39.6) | ||
| Low | 3 (5.8) | 10 (18.9) | ||
| very low | 3 (5.8) | 1 (1.9) | ||
| Academic stress | very high | 11 (21.2) | 6 (11.3) | 1.57 (0.119) |
| high | 25 (48.1) | 25 (47.2) | ||
| moderate | 11 (21.2) | 14 (26.4) | ||
| Low | 5 (9.6) | 7 (13.2) | ||
| very low | 0 (0.0) | 1 (1.9) | ||
| learning knowledge | 6.75 (1.55) | 6.62 (1.44) | 0.43 (0.127) | |
| self-confidence | 4.48 (2.50) | 4.72 (2.26) | 0.51 (0.612) | |
| learner satisfaction | 102.08 (11.06) | 100.51 (11.32) | 0.72 (0.475) | |
| critical thinking | 105.92 (11.56) | 102.81 (10.84) | 1.42 (0.158) | |
| r (p) | |||
|---|---|---|---|
| Self-Confidence | Learner Satisfaction | Critical Thinking | |
| self-confidence | 1 | 0.361 (<0.001) ** | 0.208 (0.033) * |
| learner satisfaction | 1 | 0.622 (<0.001) ** | |
| critical thinking | 1 | ||
| Characteristics | Mean (SD 3) | |||||
|---|---|---|---|---|---|---|
| Exp. 1 (n = 52) | Cont. 2 (n = 53) | |||||
| Pre-Test | Post-Test | t/p | Pre-Test | Post-Test | t/p | |
| self-confidence | 4.48 (2.50) | 7.94 (1.59) | 10.52 (<0.001) ** | 4.72 (2.26) | 7.15 (1.63) | 10.84 (<0.001) ** |
| learner satisfaction | 102.08 (11.06) | 114.58 (7.18) | 9.50 (<0.001) ** | 100.51 (11.32) | 108.68 (10.05) | 6.58 (<0.001) ** |
| critical thinking | 105.92 (11.56) | 111.37 (12.67) | 5.09 (<0.001) ** | 102.81 (10.84) | 106.45 (11.67) | 4.36 (<0.001) ** |
| Characteristics | Exp. 1 (n = 52) | Cont. 2 (n = 53) | t/p |
|---|---|---|---|
| Mean (SD 3) | Mean (SD) | ||
| self-confidence | 7.94 (1.59) | 7.15 (1.63) | 2.52 (0.013) * |
| learner satisfaction | 114.58 (7.18) | 108.68 (10.05) | 3.47 (0.001) ** |
| critical thinking | 111.37 (12.67) | 106.45 (11.67) | 2.07 (0.041) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Son, H.K. Comparison of Learning Transfer Using Simulation Problem-Based Learning and Demonstration: An Application of Papanicolaou Smear Nursing Education. Int. J. Environ. Res. Public Health 2021, 18, 1765. https://doi.org/10.3390/ijerph18041765
Lee J, Son HK. Comparison of Learning Transfer Using Simulation Problem-Based Learning and Demonstration: An Application of Papanicolaou Smear Nursing Education. International Journal of Environmental Research and Public Health. 2021; 18(4):1765. https://doi.org/10.3390/ijerph18041765
Chicago/Turabian StyleLee, Jeongim, and Hae Kyoung Son. 2021. "Comparison of Learning Transfer Using Simulation Problem-Based Learning and Demonstration: An Application of Papanicolaou Smear Nursing Education" International Journal of Environmental Research and Public Health 18, no. 4: 1765. https://doi.org/10.3390/ijerph18041765
APA StyleLee, J., & Son, H. K. (2021). Comparison of Learning Transfer Using Simulation Problem-Based Learning and Demonstration: An Application of Papanicolaou Smear Nursing Education. International Journal of Environmental Research and Public Health, 18(4), 1765. https://doi.org/10.3390/ijerph18041765






