Tobacco Use Changes and Perceived Health Risks among Current Tobacco Users during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Procedures
2.3. Data Analysis
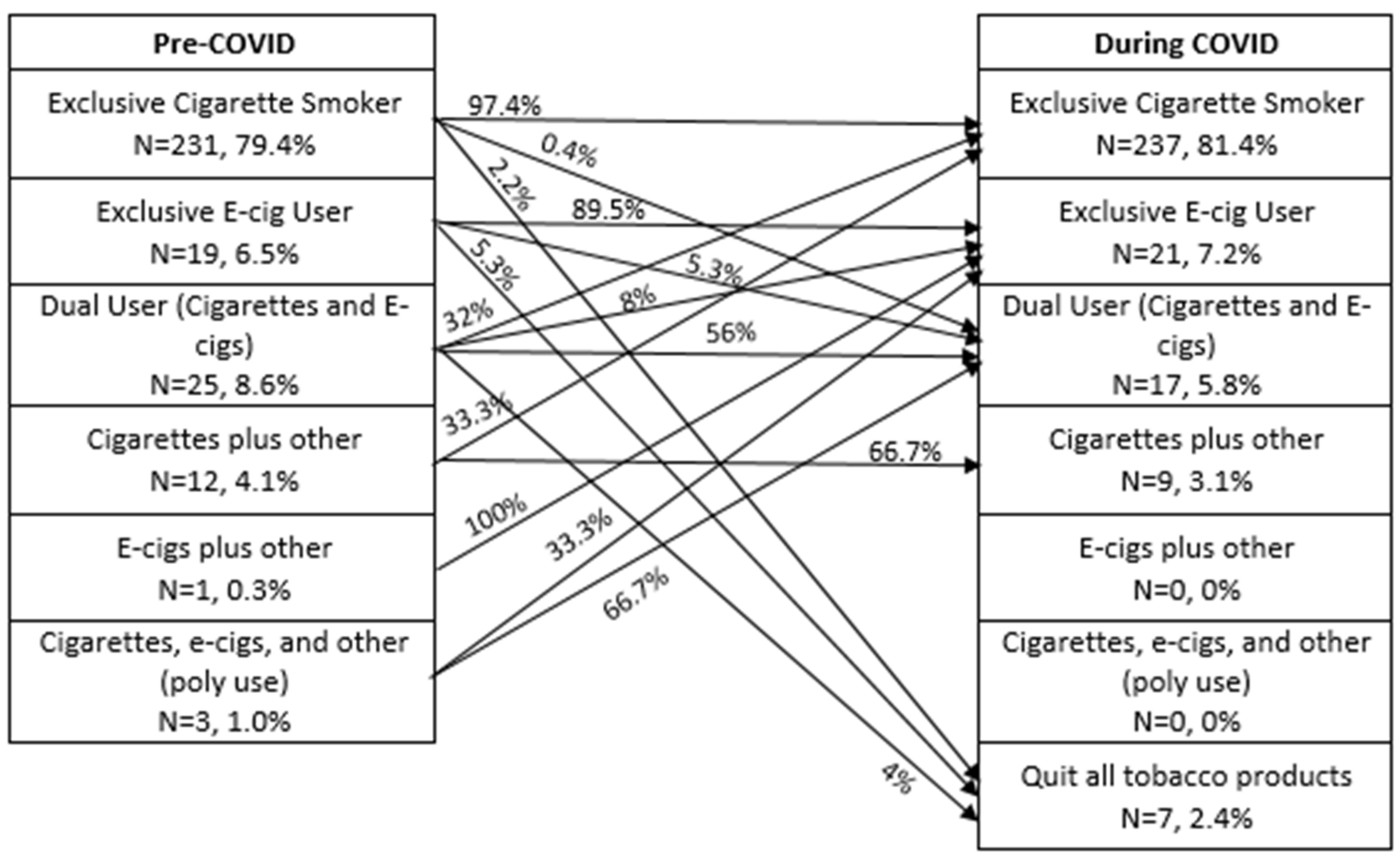
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patel, A.; Jernigan, D.B. Initial Public Health Response and Interim Clinical Guidance for the 2019 Novel Coronavirus Outbreak United States, December 31, 2019–February 4, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 140–146. [Google Scholar] [CrossRef]
- Coronavirus Resource Center, Johns Hopkins University. Available online: https://coronavirus.jhu.edu/ (accessed on 28 December 2020).
- Office of the Surgeon General (US). Office on Smoking and Health (US). The Health Consequences of Smoking: A Report of the Surgeon General; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2004. [Google Scholar]
- Alqahtani, J.S.; Oyelade, T.; Aldhahir, A.M.; Alghamdi, S.M.; Almehmadi, M.; Alqahtani, A.S.; Quaderi, S.; Mandal, S.; Hurst, J.R. Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0233147. [Google Scholar] [CrossRef] [PubMed]
- Simons, D.; Shahab, L.; Brown, J.; Perski, O. The association of smoking status with SARS-CoV-2 infection, hospitalisation and mortality from COVID-19: A living rapid evidence review with Bayesian meta-analyses (version 9). Qeios 2020. [Google Scholar] [CrossRef]
- Farsalinos, K.; Barbouni, A.; Poulas, K.; Polosa, R.; Caponnetto, P.; Niaura, R. Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: A systematic review and meta-analysis. Ther. Adv. Chronic. Dis. 2020, 11. [Google Scholar] [CrossRef]
- Paleiron, N.; Mayet, A.; Marbac, V.; Perisse, A.; Barazzutti, H.; Brocq, F.X.; Janvier, F.; Bertrand, D.; Bylicki, O. Impact of Tobacco Smoking on the risk of COVID-19.A large scale retrospective cohort study. Nicotine Tob. Res. 2021. [Google Scholar] [CrossRef]
- Kim, L.; Garg, S.; O’Halloran, A.; Whitaker, M.; Pham, H.; Anderson, E.J.; Armistead, I.; Bennett, N.M.; Billing, L.; Como-Sabetti, K.; et al. Risk Factors for Intensive Care Unit Admission and In-hospital Mortality among Hospitalized Adults Identified through the U.S. Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.Y.; Danielson, M.L.; Town, M.; Derado, G.; Greenlund, K.J.; Daily Kirley, P.; Alden, N.B.; Yousey-Hindes, K.; Anderson, E.J.; Ryan, P.A.; et al. Risk Factors for COVID-19-associated hospitalization: COVID-19-Associated Hospitalization Surveillance Network and Behavioral Risk Factor Surveillance System. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Paredes, M.R.; Apaolaza, V.; Fernandez-Robin, C.; Hartmann, P.; Yañez-Martinez, D. The impact of the COVID-19 pandemic on subjective mental well-being: The interplay of perceived threat, future anxiety and resilience. Pers. Individ. Differ. 2021, 170, 110455. [Google Scholar] [CrossRef] [PubMed]
- Cullen, W.; Gulati, G.; Kelly, B.D. Mental health in the COVID-19 pandemic. QJM 2020, 113, 311–312. [Google Scholar] [CrossRef] [PubMed]
- Kassel, J.D.; Stroud, L.R.; Paronis, C.A. Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychol. Bull. 2003, 129, 270–304. [Google Scholar] [CrossRef] [PubMed]
- Russell, M.A.H.; Peto, J.; Patel, U.A. The classification of smoking by factorial structure of motives. J. R. Stat. Soc. Ser. A 1974, 137, 313–333. [Google Scholar] [CrossRef]
- McKennell, A.C. Smoking Motivation Factors. Br. J. Soc. Clin. Psychol. 1970, 9, 8–22. [Google Scholar] [CrossRef] [PubMed]
- Frazer, K.; Callinan, J.E.; McHugh, J.; van Baarsel, S.; Clarke, A.; Doherty, K.; Kelleher, C. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2016, 2, Cd005992. [Google Scholar] [CrossRef]
- Keller, P.A.; D’Silva, J.; Lien, R.K.; Boyle, R.G.; Kingsbury, J.; O’Gara, E. Perceived harm of menthol cigarettes and quitting behaviors among menthol smokers in Minnesota. Prev. Med. Rep. 2020, 20, 101269. [Google Scholar] [CrossRef]
- Costello, M.J.; Logel, C.; Fong, G.T.; Zanna, M.P.; McDonald, P.W. Perceived risk and quitting behaviors: Results from the ITC 4-country survey. Am. J. Heal. Behav. 2012, 36, 681–692. [Google Scholar] [CrossRef] [PubMed]
- Parslow, R.A.; Jorm, A.F. Tobacco use after experiencing a major natural disaster: Analysis of a longitudinal study of 2063 young adults. Addiction 2006, 101, 1044–1050. [Google Scholar] [CrossRef]
- Osaki, Y.; Maesato, H.; Minobe, R.; Kinjo, A.; Kuwabara, Y.; Imamoto, A.; Myoga, Y.; Matsushita, S.; Higuchi, S. Changes in smoking behavior among victims after the great East Japan earthquake and tsunami. Environ. Heal. Prev. Med. 2020, 25, 19. [Google Scholar] [CrossRef]
- Vlahov, D.; Galea, S.; Ahern, J.; Resnick, H.; Kilpatrick, D. Sustained increased consumption of cigarettes, alcohol, and marijuana among Manhattan residents after September 11, 2001. Am. J. Publ. Health 2004, 94, 253–254. [Google Scholar] [CrossRef]
- Lanctot, J.Q.; Stockton, M.B.; Mzayek, F.; Read, M.; McDevitt-Murphy, M.; Ward, K. Effects of Disasters on Smoking and Relapse: An Exploratory Study of Hurricane Katrina Victims. Am. J. Health Educ. 2008, 39, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Klemperer, E.M.; West, J.C.; Peasley-Miklus, C.; Villanti, A.C. Change in Tobacco and Electronic Cigarette Use and Motivation to Quit in Response to COVID-19. Nicotine Tob. Res. 2020, 22, 1662–1663. [Google Scholar] [CrossRef] [PubMed]
- Sokolovsky, A.W.; Hertel, A.W.; Micalizzi, L.; White, H.R.; Hayes, K.L.; Jackson, K.M. Preliminary impact of the COVID-19 pandemic on smoking and vaping in college students. Addict. Behav. 2020, 115, 106783. [Google Scholar] [CrossRef]
- Yach, D. Tobacco Use Patterns in Five Countries During the COVID-19 Lockdown. Nicotine Tob. Res. 2020, 22, 1671–1672. [Google Scholar] [CrossRef] [PubMed]
- Galstyan, E.; Galimov, A.; Sussman, S. Commentary: The Emergence of Pod Mods at Vape Shops. Eval. Health Prof. 2018, 42, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Rolland, B.; Haesebaert, F.; Zante, E.; Benyamina, A.; Haesebaert, J.; Franck, N. Global Changes and Factors of Increase in Caloric/Salty Food Intake, Screen Use, and Substance Use During the Early COVID-19 Containment Phase in the General Population in France: Survey Study. JMIR Publ. Health Surveill. 2020, 6, e19630. [Google Scholar] [CrossRef]
- Malta, D.C.; Szwarcwald, C.L.; Barros, M.B.A.; Gomes, C.S.; Machado, Í.E.; Souza Júnior, P.R.B.; Romero, D.E.; Lima, M.G.; Damacena, G.N.; Pina, M.F.; et al. The COVID-19 Pandemic and changes in adult Brazilian lifestyles: A cross-sectional study, 2020. Epidemiologia Serv. Saude Rev. Sist. Unico Saude Bras. 2020, 29, e2020407. [Google Scholar] [CrossRef]
- Cancello, R.; Soranna, D.; Zambra, G.; Zambon, A.; Invitti, C. Determinants of the Lifestyle Changes during COVID-19 Pandemic in the Residents of Northern Italy. Int. J. Environ. Res. Publ. Health 2020, 17, 6287. [Google Scholar] [CrossRef] [PubMed]
- Oliver, J.A.; Foulds, J. Association Between Cigarette Smoking Frequency and Tobacco Use Disorder in U.S. Adults. Am. J. Prev. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Bommele, J.; Hopman, P.; Walters, B.H.; Geboers, C.; Croes, E.; Fong, G.T.; Quah, A.C.K.; Willemsen, M. The double-edged relationship between COVID-19 stress and smoking: Implications for smoking cessation. Tob. Induc. Dis. 2020, 18, 63. [Google Scholar] [CrossRef]
- Soule, E.K.; Mayne, S.; Snipes, W.; Guy, M.C.; Breland, A.; Fagan, P. Impacts of COVID-19 on Electronic Cigarette Purchasing, Use and Related Behaviors. Int. J. Environ. Res. Publ. Health 2020, 17, 6762. [Google Scholar] [CrossRef]
- United States Public Health Service Office of the Surgeon General; National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health. Publications and Reports of the Surgeon General. In Smoking Cessation: A Report of the Surgeon General; US Department of Health and Human Services: Washington, DC, USA, 2020. [Google Scholar]
- Czeisler, M.E.; Marynak, K.; Clarke, K.E.N.; Salah, Z.; Shakya, I.; Thierry, J.M.; Ali, N.; McMillan, H.; Wiley, J.F.; Weaver, M.D.; et al. Delay or Avoidance of Medical Care Because of COVID-19-Related Concerns—United States, June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1250–1257. [Google Scholar] [CrossRef]
- Matkin, W.; Ordóñez-Mena, J.M.; Hartmann-Boyce, J. Telephone counselling for smoking cessation. Cochrane Database Syst. Rev. 2019, 5, Cd002850. [Google Scholar] [CrossRef]
- Rosoff-Verbit, Z.; Logue-Chamberlain, E.; Fishman, J.; Audrain-McGovern, J.; Hawk, L.; Mahoney, M.; Mazur, A.; Ashare, R. The Perceived Impact of COVID-19 among Treatment-Seeking Smokers: A Mixed Methods Approach. Int. J. Environ. Res. Publ. Health 2021, 18. [Google Scholar] [CrossRef]
- Pettigrew, S.; Jun, M.; Roberts, I.; Bullen, C.; Nallaiah, K.; Rodgers, A. Preferences for Tobacco Cessation Information and Support During Covid-19. J. Addict. Med. 2020, 14, e362–e365. [Google Scholar] [CrossRef] [PubMed]
- Smokefree Action Coalition. Smoking and COVID-Quit for COVID. Available online: https://smokefreeaction.org.uk/quitforcovid/ (accessed on 23 December 2020).
- American Lung Association. Telehealth as a Vehicle to Support Tobacco Cessation. Available online: https://www.lung.org/getmedia/0df40b1c-cca4-4f8d-b17f-1c0ef19052a1/telehealth-tobacco-cessation.pdf (accessed on 23 December 2020).
- Rosenstock, I.M. The Health Belief Model and Preventive Health Behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Champion, V.L.; Skinner, C.S. The health belief model. Health Behav. Health Educ. Theory Res. Pract. 2008, 4, 45–65. [Google Scholar]
- Cummings, K.M.; Jette, A.M.; Brock, B.M.; Haefner, D.P. Psychosocial determinants of immunization behavior in a swine influenza campaign. Med. Care 1979, 17, 639. [Google Scholar] [CrossRef] [PubMed]
- Guidry, J.P.D.; Carlyle, K.E.; LaRose, J.G.; Perrin, P.; Messner, M.; Ryan, M. Using the Health Belief Model to Analyze Instagram Posts about Zika for Public Health Communications. Emerg. Infect. Dis. 2019, 25, 179–180. [Google Scholar] [CrossRef]
- Azizi, N.; Karimy, M.; Salahshour, V.N. Determinants of adherence to tuberculosis treatment in Iranian patients: Application of health belief model. J. Infect. Develop. Ctries. 2018, 12, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Guidry, J.P.D.; Austin, L.L.; O’Donnell, N.H.; Coman, I.A.; Lovari, A.; Messner, M. Tweeting the #flushot: Beliefs, Barriers, and Threats During Different Periods of the 2018 to 2019 Flu Season. J. Prim. Care Community Health 2020, 11. [Google Scholar] [CrossRef]
- Saghafi-Asl, M.; Aliasgharzadeh, S.; Asghari-Jafarabadi, M. Factors influencing weight management behavior among college students: An application of the Health Belief Model. PLoS ONE 2020, 15, e0228058. [Google Scholar] [CrossRef]
- Didarloo, A.; Nabilou, B.; Khalkhali, H.R. Psychosocial predictors of breast self-examination behavior among female students: An application of the health belief model using logistic regression. BMC Publ. Health 2017, 17, 861. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.; Skinner, C.S.; Hui, S.; Monahan, P.; Juliar, B.; Daggy, J.; Menon, U. The effect of telephone versus print tailoring for mammography adherence. Patient Educ. Couns. 2007, 65, 416–423. [Google Scholar] [CrossRef] [PubMed]
- Skinner, C.S.; Strecher, V.J.; Hospers, H. Physicians’ recommendations for mammography: Do tailored messages make a difference? Am. J. Publ. Health 1994, 84, 43–49. [Google Scholar] [CrossRef] [PubMed]
| Pre- COVID-19 | During COVID-19 | p Value | |
|---|---|---|---|
| Cigarette smoker % (n) | 93.1 (271/291) | 90.4 (263/291) | <0.01 |
| Cigarettes per day Mean (SD) (n) | 15.4 (7.7) (258) | 16.3 (8.4) (253) | <0.01 |
| E-cigarette user % (n) | 16.2 (47/291) | 13.1 (38/291) | <0.01 |
| Times used per day Mean (SD) (n) | 13.1 (14.8) (32) | 16.4 (16.3) (37) | 0.01 |
| Qualitative Response Themes | Sub-Themes | Response Example |
|---|---|---|
| Increase smoking | ||
| Boredom | “I smoke more than I used [to] because I’m stuck in the house and because I feel bored” “Since I’m stuck in the house, I have smoked more...probably out of boredom. I hate it.” | |
| Stress/anxiety | “The stress of going to work and coming home and possibly affecting my family. Every time going to the grocery store to get food and having to come home and wash everything so there is no chance of catching it. Stress of not being able to pay my bills on time or at all.” | |
| Working from home | “I smoke more, as I am working from home. I can easily walk outside in between work functions. And with trying to be a teacher, mom, employee and everything else- it can make for a stressful day.” “Working at home allows me to smoke at will rather than being in a smoke free environment for 8 hours per day.” | |
| Decreased smoking | ||
| Health reasons | “I am trying not to smoke as much due to the fact of my hands and fingers being in close contact with my face, especially mouth.” “It has caused me to cut back, just in case I would contract the virus.” | |
| More time at home | “Smoke less because I am home more.” “Being stuck in the house with my girlfriend has resulted in her taking notice to my habit more often. That has then affected how many times she says “you smoke too much” in a day. For the record, its increased. THAT in return has reduced the amount of times I go outside for a cigarette.” | |
| No change | “The COVID-19 pandemic has not affected my tobacco products use at all. I still purchase, while wearing a mask.” “It has not affected the number of cigarettes I smoke each day; however, since this coronavirus pandemic, I tend to feel as though I might be being judged (by strangers passing by) more than usual.” | |
| Desire to quit/reduce | “I talked to my physician about quitting smoking and got the nicotine patch from pharmacy. I haven’t used it yet. I smoke when I’m stressed and anxious so I don’t want to go through even more stress, anxiety from withdrawal at this time.” “I quit as soon as I came down with a fever and cough. Clearly I am aware of how detrimental smoking is to my health; however, I did not consider how it could make me more vulnerable to COVID-19 and its effects. I was terrified and quit immediately.” “I was in the process of quitting and this scare was enough to make me quit. Although as this drags on I find myself having the urge to smoke a cigarette again.” | |
| Changes in obtaining nicotine products | “It has made it more difficult to get as this is a non- essential business. Luckily though they were able to go online.” “I just buy them in bulk now” |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yingst, J.M.; Krebs, N.M.; Bordner, C.R.; Hobkirk, A.L.; Allen, S.I.; Foulds, J. Tobacco Use Changes and Perceived Health Risks among Current Tobacco Users during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 1795. https://doi.org/10.3390/ijerph18041795
Yingst JM, Krebs NM, Bordner CR, Hobkirk AL, Allen SI, Foulds J. Tobacco Use Changes and Perceived Health Risks among Current Tobacco Users during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(4):1795. https://doi.org/10.3390/ijerph18041795
Chicago/Turabian StyleYingst, Jessica M., Nicolle M. Krebs, Candace R. Bordner, Andrea L. Hobkirk, Sophia I. Allen, and Jonathan Foulds. 2021. "Tobacco Use Changes and Perceived Health Risks among Current Tobacco Users during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 4: 1795. https://doi.org/10.3390/ijerph18041795
APA StyleYingst, J. M., Krebs, N. M., Bordner, C. R., Hobkirk, A. L., Allen, S. I., & Foulds, J. (2021). Tobacco Use Changes and Perceived Health Risks among Current Tobacco Users during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(4), 1795. https://doi.org/10.3390/ijerph18041795








