The Association of Nonsuicidal Self-Injury with Quality of Life and Mental Disorders in Clinical Adolescents—A Network Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Subjects
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Sample
3.2. Self-Reported QoL Rating
3.3. Self vs Parents’ Rating of QoL of Adolescents Engaged in NSSI
3.4. Associations between NSSI and QoL Dimensions
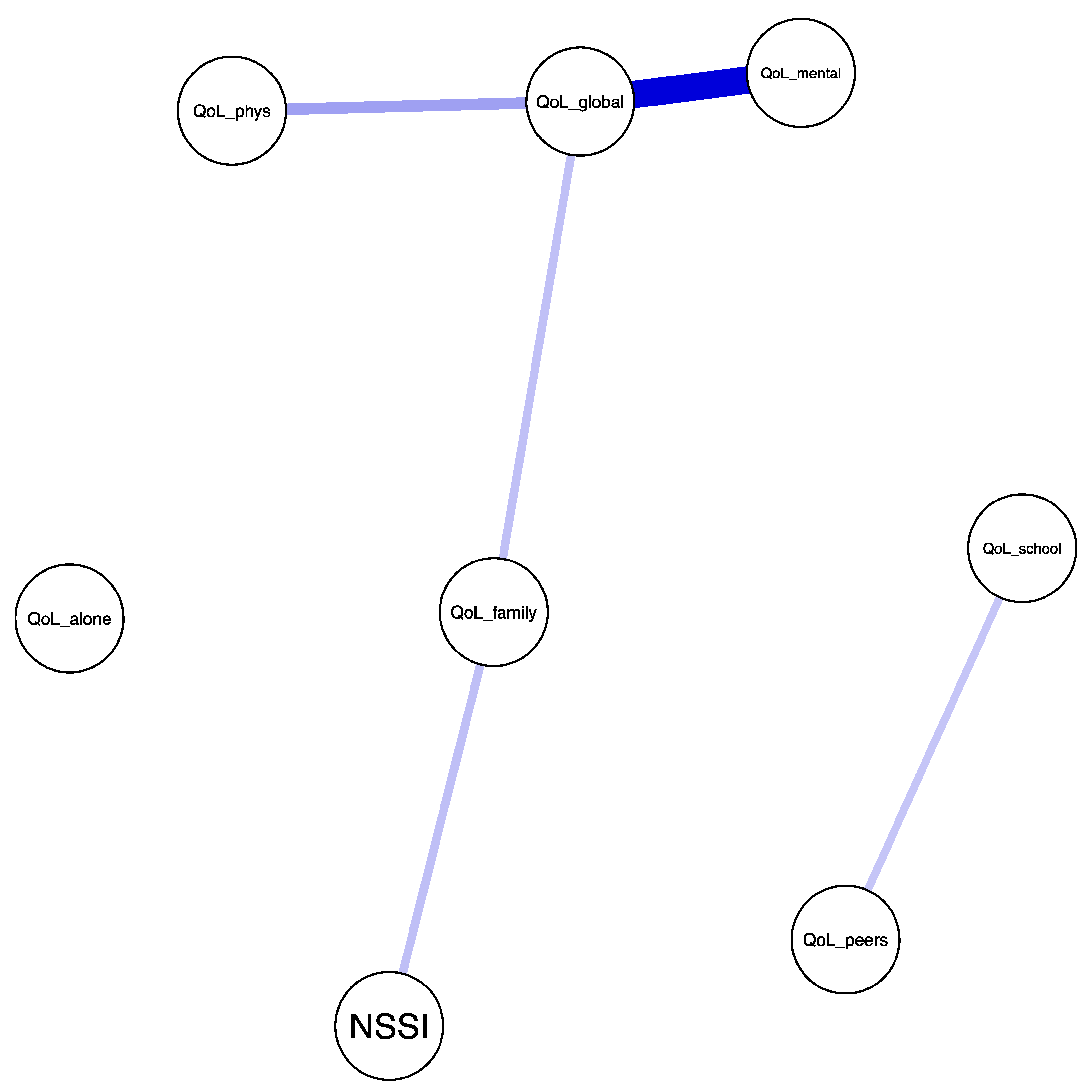
3.5. Associations among NSSI, QoL, and Mental Disorders
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Klonsky, E.D.; Muehlenkamp, J.J. Self-injury: A research review for the practitioner. J. Clin. Psychol. 2007, 63, 1045–1056. [Google Scholar] [CrossRef]
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; APA: Arlington, VA, USA, 2013. [Google Scholar]
- Cipriano, A.; Cella, S.; Cotrufo, P. Nonsuicidal self-injury: A systematic review. Front. Psychol. 2017, 8, 1946. [Google Scholar] [CrossRef]
- Plener, P.L.; Schumacher, T.S.; Munz, L.M.; Groschwitz, R.C. The longitudinal course of non-suicidal self-injury and deliberate self-harm: A systematic review of the literature. Bord. Pers. Disord. Emot. Dysregul. 2015, 2, 2. [Google Scholar] [CrossRef]
- Brunner, R.; Kaess, M.; Parzer, P.; Fischer, G.; Carli, V.; Hoven, C.W.; Wasserman, C.; Sarchiapone, M.; Resch, F.; Apter, A.; et al. Life-time prevalence and psychosocial correlates of adolescent direct self-injurious behavior: A comparative study of findings in 11 European countries. J. Child Psychol. Psychiatry 2014, 55, 337–348. [Google Scholar] [CrossRef]
- Lloyd-Richardson, E.; Perrine, N.; Dierker, L.; Kelley, M.L. Characteristics and functions of non-suicidal self-injury in a community sample of adolescents. Psychol. Med. 2007, 37, 1183–1192. [Google Scholar] [CrossRef] [PubMed]
- Muehlenkamp, J.J.; Claes, L.; Havertape, L.; Plener, P.L. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc. Psychiatry Ment. Health 2012, 6, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Swannell, S.V.; Martin, G.E.; Page, A.; Hasking, P.; St John, N.J. Prevalence of nonsuicidal self-injury in nonclinical samples: Systematic review, meta-analysis and meta-regression. Suicide Life Threat. Behav. 2014, 44, 273–303. [Google Scholar] [CrossRef] [PubMed]
- Kaess, M.; Parzer, P.; Mattern, M.; Plener, P.L.; Bifulco, A.; Resch, F.; Brunner, R. Adverse childhood experiences and their impact on frequency, severity, and the individual function of nonsuicidal self-injury in youth. Psychiatry Res. 2013, 206, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Prinstein, M.J. A Functional approach to the assessment of self-mutilative behavior. J. Consult. Clin. Psychol. 2004, 72, 885–890. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.C.; Plener, P.L. Non-suicidal self-Injury in adolescence. Curr. Psychiatry Rep. 2017, 19, 20. [Google Scholar] [CrossRef]
- Bresin, K.; Schoenleber, M. Gender differences in the prevalence of nonsuicidal self-injury: A meta-analysis. Clin. Psychol. Rev. 2015, 38, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Nitkowski, D.; Petermann, F. Selbstverletzendes Verhalten und komorbide psychische Störungen: Ein Überblick Non-suicidal self-injury and comorbid mental disorders: A review. Fortschr. Neurol. Psychiatr. 2011, 79, 9–20. [Google Scholar] [CrossRef]
- Nock, M.; Joiner, T., Jr.; Gordon, K.; Lloyd-Richardson, E.; Prinstein, M. Non-suicidal self-injury among adolescents: Diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006, 144, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Andover, M.S.; Morris, B.W.; Wren, A.; Bruzzese, M.E. The co-occurrence of non-suicidal self-injury and attempted suicide among adolescents: Distinguishing risk factors and psychosocial correlates. Child Adolesc. Psychiatry Ment. Health 2012, 6, 11. [Google Scholar] [CrossRef]
- Kiekens, G.; Hasking, P.; Boyes, M.; Claes, L.; Mortier, P.; Auerbach, R.P.; Cuijpers, P.; Demyttenaere, K.; Green, J.G.; Kessler, R.C.; et al. The associations between non-suicidal self-injury and first onset suicidal thoughts and behaviors. J. Affect. Disord. 2018, 239, 171–179. [Google Scholar] [CrossRef]
- Klonsky, E.D.; May, A.M.; Glenn, C.R. The relationship between nonsuicidal self-injury and attempted suicide: Converging evidence from four samples. J. Abnorm. Psychol. 2013, 122, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Muehlenkamp, J.J.; Gutierrez, P.M. Risk for suicide attempts among adolescents who engage in non-suicidal self-injury. Arch. Suicide Res. 2007, 11, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Klonsky, E.D. The functions of deliberate self-injury: A review of the evidence. Clin. Psychol. Rev. 2007, 27, 226–239. [Google Scholar] [CrossRef] [PubMed]
- Waals, L.; Baetens, I.; Rober, P.; Lewis, S.; Van Parys, H.; Goethals, E.R.; Whitlock, J. The NSSI Family Distress Cascade Theory. Child Adolesc. Psychiatry Ment. Health 2018, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Bastiaansen, D.; Koot, H.M.; Ferdinand, R.F.; Verhulst, F.C. Quality of life in children with psychiatric disorders: Self-, parent, and clinician report. J. Am. Acad. Child Adolesc. Psychiatry 2004, 43, 221–230. [Google Scholar] [CrossRef]
- Jozefiak, T.; Larsson, B.; Wichstrøm, L.; Wallander, J.; Mattejat, F. Quality of life as reported by children and parents: A comparison between students and child psychiatric outpatients. Health Qual. Life Outcomes 2010, 8, 136. [Google Scholar] [CrossRef]
- The WHOQOL Group. The World Health Organization’s quality of life assessment (WHOQOL): Position paper from the World Health Organisation. Soc. Sci. Med. 1995, 41, 1403–1409. [Google Scholar] [CrossRef]
- Danckaerts, M.; Sonuga-Barke, E.J.S.; Banaschewski, T.; Buitelaar, J.; Döpfner, M.; Hollis, C.; Santosh, P.; Rothenberger, A.; Sergeant, J.; Steinhausen, H.-C.; et al. The quality of life of children with attention deficit/hyperactivity disorder: A systematic review. Eur. Child Adolesc. Psychiatry 2010, 19, 83–105. [Google Scholar] [CrossRef] [PubMed]
- Dallos, G.; Miklosi, M.; Kereszteny, A.; Velo, S.; Szentivanyi, D.; Gadoros, J.; Balazs, J. Self- and parent-rated quality of life of a treatment naïve sample of children with ADHD: The impact of age, gender, type of ADHD, and comorbid psychiatric conditions according to both a categorical and a dimensional approach. J. Atten. Disord. 2014, 21, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Kiss, E.; Kapornai, K.; Baji, I.; Mayer, L.; Vetro, Á. Assessing quality of life: Mother–child agreement in depressed and non-depressed Hungarian. Eur. Child. Adolesc. Psychiatry 2009, 18, 265–273. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wallander, J.L.; Schmitt, M.; Koot, H.M. Quality of life measurement in children and adolescents: Issues, instruments, and applications. J. Clin. Psychol. 2001, 57, 571–585. [Google Scholar] [CrossRef]
- Szentivanyi, D.; Balazs, J. Quality of life in children and adolescents with symptoms or diagnosis of conduct disorder or oppositional defiant disorder. Ment. Health Prev. 2018, 10, 1–8. [Google Scholar] [CrossRef]
- Velo, S.; Kereszteny, A.; Szentivanyi, D.; Balazs, J. Quality of life of patients with attention-deficit/hyperactivity disorder: Systematic review of the past 5 years [Figyelemhiányos hiperaktivitás zavar diagnózisú gyermekek és felnőttek életminősége: Az elmúlt öt év vizsgálatainak szisztematikus áttekintő tanulmánya]. Neuropsychopharmacol. Hung. 2013, 15, 73–82. [Google Scholar]
- Weitkamp, K.; Daniels, J.K.; Romer, G.; Wiegand-Grefe, S. Health-related quality of life of children and adolescents with mental disorders. Health Qual. Life Outcomes 2013, 11, 129. [Google Scholar] [CrossRef]
- Balazs, J.; Miklosi, M.; Halasz, J.; Horváth, L.O.; Szentiványi, D.; Vida, P. Suicidal risk, psychopathology, and quality of life in a clinical population of adolescents. Front. Psychiatry 2018, 9, 17. [Google Scholar] [CrossRef]
- Rönkä, A.R.; Taanila, A.; Koiranen, M.; Sunnari, V.; Rautio, A. Associations of deliberate self-harm with loneliness, self-rated health and life satisfaction in adolescence: Northern Finland Birth Cohort 1986 Study. Int. J. Circumpolar Health 2013, 72, 21085. [Google Scholar] [CrossRef]
- Hawton, K.; Rodham, K.; Evans, E.; Weatherall, R. Deliberate self harm in adolescents: Self report survey in schools in England. BMJ 2002, 325, 1207–1211. [Google Scholar] [CrossRef] [PubMed]
- Zullig, K.J. The Association between deliberate self-harm and college student subjective quality of life. Am. J. Health Behav. 2016, 40, 231–239. [Google Scholar] [CrossRef]
- Kaess, M.; Fischer-Waldschmidt, G.; Resch, F.; Koenig, J. Health related quality of life and psychopathological distress in risk taking and self-harming adolescents with full-syndrome, subthreshold and without borderline personality disorder: Rethinking the clinical cut-off? Bord. Personal. Disord. Emot. Dysregula. 2017, 4, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, S. A farewell to Bonferroni: The problems of low statistical power and publication bias. Behav. Ecol. 2004, 15, 1044–1045. [Google Scholar] [CrossRef]
- McGrath, J.J.; Lim, C.C.W.; Plana-Ripoll, O.; Holtz, Y.; Agerbo, E.; Momen, N.C.; Mortensen, P.B.; Pedersen, C.B.; Abdulmalik, J.; Aguilar-Gaxiola, S.; et al. Comorbidity within mental disorders: A comprehensive analysis based on 145 990 survey respondents from 27 countries. Epidemiol. Psychiatr. Sci. 2020, 29, e153. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Hwang, I.; Sampson, N.A.; Kessler, R.C. Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Mol. Psychiatry 2009, 15, 868–876. [Google Scholar] [CrossRef]
- De Nooy, W.; Mrvar, A.; Batagelj, V. Exploratory Social Network Analysis with Pajek, 2nd ed.; Cambridge University Press: Cambridge, UK, 2011; p. 7. [Google Scholar]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. 2017, 50, 195–212. [Google Scholar] [CrossRef] [PubMed]
- Borsboom, D.; Cramer, A.O.J. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef] [PubMed]
- McNally, R.J.; Robinaugh, D.J.; Wu, G.W.Y.; Wang, L.; Deserno, M.K.; Borsboom, D. Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clin. Psychol. Sci. 2015, 3, 836–849. [Google Scholar] [CrossRef]
- Epskamp, S.; Waldorp, L.J.; Mõttus, R.; Borsboom, D. The Gaussian Graphical Model in Cross-Sectional and Time-Series Data. Multivar. Behav. Res. 2018, 53, 453–480. [Google Scholar] [CrossRef]
- Koller, D.; Friedman, N. Probabilistic Graphical Models: Principles and Techniques; MIT Press: Cambridge, MA, USA, 2009. [Google Scholar]
- Pearl, J. Causality: Models, Reasoning, and Inference; Cambridge University Press: New York, NY, USA, 2000. [Google Scholar]
- Costantini, G.; Epskamp, S.; Borsboom, D.; Perugini, M.; Mõttus, R.; Waldorp, L.; Cramer, A. State of the aRt personality research: A tutorial on network analysis of personality data in R. J. Res. Pers. 2015, 54, 13–29. [Google Scholar] [CrossRef]
- Tibshirani, R. Regression Shrinkage and Selection via the Lasso. J. R. Stat. Soc. Ser. B Stat. Methodol. 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Balázs, J.; Győri, D.; Horváth, L.O.; Mészáros, G.; Szentiványi, D. Attention-deficit hyperactivity disorder and nonsuicidal self-injury in a clinical sample of adolescents: The role of comorbidities and gender. BMC Psychiatry 2018, 18, 34. [Google Scholar] [CrossRef] [PubMed]
- Horváth, L.O.; Győri, D.; Komáromy, D.; Mészáros, G.; Szentiványi, D.; Balázs, J. Nonsuicidal self-injury and suicide: The role of life events in clinical and non-clinical populations of adolescents. Front. Psychiatry 2020, 11, 370. [Google Scholar] [CrossRef] [PubMed]
- Mészáros, G.; Győri, D.; Horváth, L.O.; Szentiványi, D.; Balázs, J. Nonsuicidal self-injury: Its associations with pathological internet use and psychopathology among adolescents. Front. Psychiatry 2020, 11, 814. [Google Scholar] [CrossRef] [PubMed]
- Lecrubier, Y.; Sheehan, D.; Weiller, E.; Amorim, P.; Bonora, I.; Harnett Sheehan, K.; Janavs, J.; Dunbar, G. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Eur. Psychiatry 1997, 12, 224–231. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar] [PubMed]
- Sheehan, D.V.; Sheehan, K.H.; Shytle, R.D.; Janavs, J.; Bannon, Y.; Rogers, J.E.; Milo, K.M.; Stock, S.L.; Wilkinson, B. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J. Clin. Psychiatry 2010, 71, 313–326. [Google Scholar] [CrossRef] [PubMed]
- Balazs, J.; Biro, A.; Dalnoki, D.; Lefkovics, E.; Tamas, Z.; Nagy, P.; Gadoros, J. A Gyermek, M.I.N.I. kérdőív magyar nyelvű változatának ismertetése [Introduction of the Hungarian version of the M.I.N.I. Kid]. Psychiatr. Hung. 2004, 19, 358–364. [Google Scholar]
- Gratz, K.L. Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. J. Psychopathol. Behav. Assess. 2001, 23, 253–263. [Google Scholar] [CrossRef]
- Nock, M.K. Self-Injury. Annu. Rev. Clin. Psychol. 2010, 6, 339–363. [Google Scholar] [CrossRef] [PubMed]
- Bjärehed, J.; Lundh, L.-G. Deliberate self-harm in 14-year-old adolescents: How frequent is it, and how is it associated with psychopathology, relationship variables, and styles of emotional regulation? Cogn. Behav. Ther. 2008, 37, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Kiss, E.; Baji, I.; Mayer, L.; Skulteti, D.; Benak, I.; Vetro, A. Eletminoseg kerdoiv validitasa és pszichometriai jellemzoi magyar gyermekpopulacion [Validity and psychometric properties of a quality of life questionnaire in a Hungarian child and adolescent population]. Psychiatr. Hung. 2007, 22, 33–42. [Google Scholar]
- Mattejat, F.; Jungmann, J.; Meusers, M.; Moik, C.; Schaff, C.; Remschmidt, H. Das Inventar zur Erfassung der Lebensqualität bei psychischgestörten Kindern und Jugendlichen [The assessment of quality of life of children and adolescents with psychiatric disorders]. Z. Für Kinder- Und Jugendpsychiatrie Und Psychother. 1998, 26, 183–196. [Google Scholar]
- Van Borkulo, C.D.; Boschloo, L.; Borsboom, D.; Penninx, B.; Waldorp, L.; Schoevers, R. Association of symptom network structure with the course of depression. JAMA Psychiatry 2015, 72, 1219–1226. [Google Scholar] [CrossRef]
- Deserno, M.K.; Borsboom, D.; Begeer, S.; Geurts, H.M. Multicausal systems ask for multicausal approaches: A network perspective on subjective well-being in individuals with autism spectrum disorder. Autism 2017, 21, 960–971. [Google Scholar] [CrossRef]
- Fried, E.I.; Epskamp, S.; Nesse, R.M.; Tuerlinckx, F.; Borsboom, D. What are “good” depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J. Affect Disord. 2016, 189, 314–320. [Google Scholar] [CrossRef]
- Jaya, E.S.; Hillmann, T.E.; Reininger, K.M.; Gollwitzer, A.; Lincoln, T.M. Loneliness and psychotic symptoms: The mediating role of depression. Cognit. Ther. Res. 2016, 41, 106–116. [Google Scholar] [CrossRef]
- Knefel, M.; Tran, U.S.; Lueger-Schuster, B. The association of posttraumatic stress disorder, complex posttraumatic stress disorder, and borderline personality disorder from a network analytical perspective. J. Anxiety Disord. 2016, 43, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Levine, S.Z.; Leucht, S. Identifying a system of predominant negative symptoms: Network analysis of three randomized clinical trials. Schizophr. Res. 2016, 178, 17–22. [Google Scholar] [CrossRef]
- Isvoranu, A.M.; van Borkulo, C.D.; Boyette, L.-L.; Wigman, J.T.W.; Vinkers, C.H.; Borsboom, D. Group investigators a network approach to psychosis: Pathways between childhood trauma and psychotic symptoms. Schizophr. Bull. 2016, 43, 187–196. [Google Scholar] [CrossRef]
- Isvoranu, A.M.; Borsboom, D.; van Os, J.; Guloksuz, S. A network approach to environmental impact in psychotic disorder: Brief theoretical framework. Schizophr. Bull. 2016, 42, 870–873. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2008, 9, 432–441. [Google Scholar] [CrossRef]
- Barber, R.F.; Drton, M. High-dimensional Ising model selection with Bayesian information criteria. Electron. J. Statist. 2015, 9, 567–607. [Google Scholar] [CrossRef]
- Foygel, R.; Drton, M. Extended Bayesian Information Criteria for Gaussian Graphical Models. Adv. Neural. Inf. Process. Syst. 2010, 23, 2020–2028. [Google Scholar]
- Zhao, P.; Yu, B. On model selection consistency of Lasso. J. Mach. Learn. Res. 2006, 7, 2541–2563. [Google Scholar]
- Chen, J.; Chen, Z. Extended bayesian information criteria for model selection with large model spaces. Biometrika 2008, 95, 759–771. [Google Scholar] [CrossRef]
- Van Borkulo, C.D.; Borsboom, D.; Epskamp, S.; Blanken, T.F.; Boschloo, L.; Schoevers, R.A.; Waldorp, L.J. A new method for constructing networks from binary data. Sci. Rep. 2014, 4, 5918. [Google Scholar] [CrossRef] [PubMed]
- Wagenmakers, E.-J. A practical solution to the pervasive problems ofp values. Psychon. Bull. Rev. 2007, 14, 779–804. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Lafferty, J.; Wasserman, L. The nonparanormal: Semiparametric estimation of high dimensional undirected graphs. J. Mach. Learn. Res. 2009, 10, 2295–2328. [Google Scholar]
- Muthén, B. A general structural equation model with dichotomous, ordered categorical, and continuous latent variable indicators. Psychometrika 1984, 49, 115–132. [Google Scholar] [CrossRef]
- Van Borkulo, C.D.; Epskamp, S. Isingfit: Fitting Ising Models Using the eLasso Method. R Package Version 0.2.0. Available online: https://cran.r-project.org/web/packages/IsingFit/index.html (accessed on 7 September 2016).
- Haslbeck, J.M.B.; Waldorp, L.J. Mgm: Structure Estimation for Time-Varying Mixed Graphical Models in High-Dimensional Data. Available online: http://arxiv.org/abs/1510.06871 (accessed on 26 April 2016).
- Yang, E.; Baker, Y.; Ravikumar, P.; Genevera, I.A.; Liu, Z. Mixed Graphical Models via Exponential Families. J. Mach. Learn. Res. 2014, 33, 1042–1050. [Google Scholar]
- Lauritzen, S.L.; Andersen, A.H.; Edwards, D.; Jöreskog, K.G.; Johansen, S. Mixed Graphical Association Models [with Discussion and Reply]. Scand J. Stat. 1989, 16, 273–306. [Google Scholar]
- Lauritzen, S.L. Graphical Models; Oxford University Press: Oxford, NY, USA, 1996. [Google Scholar]
- Frydenberg, M.; Lauritzen, S.L. Decomposition of Maximum Likelihood in Mixed Graphical Interaction Models. Biometrika 1989, 76, 539–555. [Google Scholar] [CrossRef]
- Loh, P.-L.; Wainwright, M.J. Structure estimation for discrete graphical models: Generalized covariance matrices and their inverses. Ann. Statist. 2013, 41, 3022–3049. [Google Scholar] [CrossRef]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. qgraph: Network visualizations of relationships in psychometric data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- You, J.; Leung, F.; Fu, K. Exploring the reciprocal relations between nonsuicidal self-injury, negative emotions and relationship problems in Chinese adolescents: A longitudinal cross-lag study. J. Abnorm. Child Psychol. 2012, 40, 829–836. [Google Scholar] [CrossRef]
- Baetens, I.; Claes, L.; Martin, G.; Onghena, P.; Grietens, H.; Leeuwen, K.V.; Pieters, C.; Wiersema, J.R.; Griffith, J.W. Is nonsuicidal self-Injury associated with parenting and family factors? J. Early Adolesc. 2013, 34, 387–405. [Google Scholar] [CrossRef]
- Baetens, I.; Andrews, T.; Claes, L.; Martin, G. The association between family functioning and NSSI in adolescence: The mediating role of depressive symptoms. Fam. Sci. 2015, 6, 330–337. [Google Scholar] [CrossRef]
- Bureau, J.-F.; Martin, J.; Freynet, N.; Poirier, A.A.; Lafontaine, M.-F.; Cloutier, P. Perceived dimensions of parenting and non-suicidal self-injury in young adults. J. Youth Adolesc. 2010, 39, 484–494. [Google Scholar] [CrossRef]
- Hilt, L.M.; Nock, M.K.; Lloyd-Richardson, E.E.; Prinstein, M.J. Longitudinal study of nonsuicidal self-injury among young adolescents: Rates, correlates, and preliminary test of an interpersonal model. J. Early Adolesc. 2008, 28, 455–469. [Google Scholar] [CrossRef]
- Adrian, M.; Zeman, J.; Erdley, C.; Lisa, L.; Sim, L. Emotional dysregulation and interpersonal difficulties as risk factors for nonsuicidal self-injury in adolescent girls. J. Abnorm. Child Psychol. 2011, 39, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Fortune, S.; Sinclair, J.; Hawton, K. Adolescents’ views on preventing self-harm. A large community study. Soc. Psychiatry Psychiat. Epidemiol. 2008, 43, 96–104. [Google Scholar] [CrossRef]
- Rissanen, M.-L.; Kylmä, J.; Laukkanen, E. Helping adolescents who self-mutilate: Parental descriptions. J. Clin. Nurs. 2009, 18, 1711–1721. [Google Scholar] [CrossRef]
- Glenn, C.R.; Franklin, J.C.; Nock, M.K. Evidence-based psychosocial treatments for self-injurious thoughts and behaviors in youth. J. Clin. Child Adolesc. Psychol. 2014, 44, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Favazza, A.R. Nonsuicidal self-injury: Definition and classification. In Understanding Nonsuicidal Self-Injury: Origins, Assessment, and Treatment; Nock, M.K., Ed.; American Psychological Association: Washington, DC, USA, 2009; pp. 9–18. [Google Scholar]
- Baetens, I.; Claes, L.; Onghena, P.; Grietens, H.; Van Leeuwen, K.; Pieters, C.; Wiersema, J.R.; Griffith, J.W. The effects of nonsuicidal self-injury on parenting behaviors: A longitudinal analyses of the perspective of the parent. Child Adolesc. Psychiatry Ment. Health 2015, 9, 24. [Google Scholar] [CrossRef]
- Kelada, L.; Whitlock, J.; Hasking, P.; Melvin, G. Parents’ experiences of nonsuicidal self-injury among adolescents and young adults. J. Child Fam. Stud. 2016, 25, 3403–3416. [Google Scholar] [CrossRef]
- Arbuthnott, A.E.; Lewis, S.P. Parents of youth who self-injure: A review of the literature and implications for mental health professionals. Child Adolesc. Psychiatry Ment. Health 2015, 9, 35. [Google Scholar] [CrossRef] [PubMed]
- McDonald, G.; O’Brien, L.; Jackson, D. Guilt and shame: Experiences of parents of self-harming adolescents. J. Child Health Care 2007, 11, 298–310. [Google Scholar] [CrossRef]
- Whitlock, J.; Lloyd-Richardson, E.; Fisseha, F.; Bates, T. Parental secondary stress: The often hidden consequences of nonsuicidal self-injury in youth. J. Clin Psychol. 2018, 74, 178–196. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K. Why Do People Hurt Themselves? New insights into the nature and functions of self-injury. Curr. Dir. Psychol. Sci. 2009, 18, 78–83. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation (WHO). Preventing Suicide: A Global Imperative. Available online: http://apps.who.int/iris/bitstream/10665/131056/1/9789241564779_eng.pdf (accessed on 15 September 2014).
- Grandclerc, S.; Labrouhe, D.D.; Spodenkiewicz, M.; Lachal, J.; Moro, M.-R. Relations between nonsuicidal self-injury and suicidal behavior in adolescence: A systematic review. PLoS ONE 2016, 11, e0153760. [Google Scholar] [CrossRef] [PubMed]
- Chiu, K.; Clark, D.M.; Leigh, E. Prospective associations between peer functioning and social anxiety in adolescents: A systematic review and meta-analysis. J. Affect Disord. 2020, 279, 650–661. [Google Scholar] [CrossRef]
- Vergara, G.A.; Stewart, J.G.; Cosby, E.A.; Lincoln, S.H.; Auerbach, R.P. Non-suicidal self-injury and suicide in depressed adolescents: Impact of peer victimization and bullying. J. Affect. Disord. 2019, 15, 744–749. [Google Scholar] [CrossRef]
- Walter, H.J.; Bukstein, O.G.; Abright, A.R.; Keable, H.; Ramtekkar, U.; Ripperger-Suhler, J.; Rockhill, C. Clinical practice guideline for the assessment and treatment of children and adolescents with anxiety disorders. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1107–1124. [Google Scholar] [CrossRef] [PubMed]
- Verduin, T.; Kendall, P. Differential occurrence of comorbidity within childhood anxiety disorders. J. Clin. Child Adolesc. Psychol. 2003, 32, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Stanley, I.H.; Boffa, J.W.; Rogers, M.L.; Hom, M.A.; Albanese, B.J.; Chu, C.; Capron, D.W.; Schmidt, N.B.; Joiner, T.E. Anxiety sensitivity and suicidal ideation/suicide risk: A meta-analysis. J. Consult. Clin. Psychol. 2018, 86, 946–960. [Google Scholar] [CrossRef]
- Nock, M.K.; Green, J.G.; Hwang, I.; McLaughlin, K.A.; Sampson, N.A.; Zaslavsky, A.M.; Kessler, R.C. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry 2013, 70, 300–310. [Google Scholar] [CrossRef]
- Balazs, J.; Miklosi, M.; Kereszteny, A.; Dallos, G.; Gadoros, J. Attention-deficit hyperactivity disorder and suicidality in a treatment naïve sample of children and adolescents. J. Affect. Disord. 2014, 152–154, 282–287. [Google Scholar] [CrossRef]
- Gothe, N.P.; Ehlers, D.K.; Salerno, E.A.; Fanning, J.; Kramer, A.F.; McAuley, E. Physical activity, sleep and quality of life in older adults: Influence of physical, mental and social well-being. Behav. Sleep Med. 2019, 18, 797–808. [Google Scholar] [CrossRef] [PubMed]
- Alves, V.d.M.; Francisco, L.C.F.d.L.; Belo, F.M.P.; de-Melo-Neto, V.L.; Barros, V.G.; Nardi, A.E. Evaluation of the quality of life and risk of suicide. Clinics 2016, 71, 135–139. [Google Scholar] [CrossRef]
- Bullock, J.G.; Green, D.P.; Ha, S.E. Yes, but what’s the mechanism? (don’t expect an easy answer). J. Pers. Soc. Psychol. 2010, 98, 550–558. [Google Scholar] [CrossRef] [PubMed]
- White-Koning, M.; Arnaud, C.; Dickinson, H.O.; Thyen, U.; Beckung, E.; Fauconnier, J.; McManus, V.; Michelsen, S.I.; Parkes, J.; Parkinson, K.; et al. Determinants of child-parent agreement in quality-of-life reports: A European study of children with cerebral palsy. Pediatrics 2007, 120, e804–e814. [Google Scholar] [CrossRef] [PubMed]
- Vance, Y.H.; Morse, R.C.; Jenney, M.E.; Eiser, C. Issues in measuring quality of life in childhood cancer: Measures, proxies, and parental mental health. J. Child Psychol. Psychiatry 2001, 42, 661–667. [Google Scholar] [CrossRef]
- Slesinger, N.C.; Hayes, N.A.; Washburn, J.J. Understanding predictors of change in a day treatment setting for non-suicidal self-injury. Psychol. Psychother. 2020, 1–19. [Google Scholar] [CrossRef] [PubMed]


| Demographic Variables | Chi/t-Value | p-Value | Corrected p-Value (Bonferroni) | df |
|---|---|---|---|---|
| Father’s education level | 0.770 | 0.680 | 1.000 | 2.000 |
| Mother’s education level | 1.741 | 0.419 | 1.000 | 2.000 |
| Father’s job market status | 7.572 | 0.144 | 1.000 | 5.000 |
| Mother’s job market status | 4.932 | 0.584 | 1.000 | 6.000 |
| Family’s economic situation | 0.534 | 0.581 | 1.000 | 1.000 |
| Family type | 3.665 | 0.641 | 1.000 | 5.000 |
| Adoption status | 2.469 | 0.757 | 1.000 | 4.000 |
| Mental problem in family | 8.912 | 0.059 | 1.000 | 4.000 |
| Suicide in family | 8.043 | 0.097 | 1.000 | 4.000 |
| Number of siblings | 4.686 | 0.802 | 1.000 | 8.000 |
| Number of stepsiblings | 0.553 | 0.512 | 1.000 | 1.000 |
| Twin | 1.205 | 0.818 | 1.000 | 2.000 |
| Pregnancy | 0.000 | 1.000 | 1.000 | 1.000 |
| Birth details (complication) | 0.070 | 0.870 | 1.000 | 1.000 |
| Birth time (too early/late) | 2.799 | 0.280 | 1.000 | 2.000 |
| Early childhood (problems) | 0.196 | 0.816 | 1.000 | 1.000 |
| Left/right-handed | 1.829 | 0.405 | 1.000 | 2.000 |
| Psychological treatment ever | 0.830 | 0.433 | 1.000 | 1.000 |
| Chronic illness | 1.454 | 0.320 | 1.000 | 1.000 |
| Child is taking medication | 0.017 | 1.000 | 1.000 | 1.000 |
| Child was taking medication | 0.197 | 0.719 | 1.000 | 1.000 |
| School (or workplace) type | 3.495 | 0.528 | 1.000 | 4.000 |
| Age (Welch two-sample t-test) | 0.065 | 0.948 | 1.000 | 188.460 |
| Sex | 27.940 | 0.000 | 0.012 * | 1.000 |
| NSSI–Mental Disorders | NSSI | No-NSSI | Chi-Squared Statistics | p-Value | Corrected p-Value (Bonferroni) | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Mood disorders | 0.602 | 0.492 | 0.290 | 0.456 | 38.441 | 0.000 | 0.000 *** |
| Anxiety disorders | 0.796 | 0.405 | 0.591 | 0.494 | 3.660 | 0.056 | 0.334 |
| Att. disr. disorders | 0.480 | 0.502 | 0.280 | 0.451 | 12.392 | 0.000 | 0.002 ** |
| Substance use disorders | 0.235 | 0.426 | 0.118 | 0.325 | 8.497 | 0.004 | 0.022 * |
| Psychotic disorders | 0.265 | 0.444 | 0.065 | 0.247 | 7.260 | 0.007 | 0.042 * |
| Suicidality | 0.684 | 0.467 | 0.226 | 0.420 | 17.494 | 0.000 | 0.000 *** |
| Domains of Quality of Life (QoL) | Mean (NSSI) | Mean (No-NSSI) | t-Value | df | p-Value | Corrected p-Value (Bonferroni) |
|---|---|---|---|---|---|---|
| School | 3.286 | 2.957 | −1.895 | 184.315 | 0.060 | 0.418 |
| Family | 2.704 | 2.032 | −4.517 | 186.371 | 0.000 | 0.000 *** |
| Peer relations | 2.429 | 2.172 | −1.517 | 188.569 | 0.131 | 0.917 |
| Alone activity | 2.143 | 1.796 | −2.310 | 188.017 | 0.022 | 0.154 |
| Physical health | 2.714 | 2.194 | −3.400 | 188.809 | 0.001 | 0.006 ** |
| Mental health | 3.796 | 3.151 | −3.972 | 188.063 | 0.000 | 0.001 ** |
| Global well-being | 3.378 | 2.667 | −4.508 | 188.203 | 0.000 | 0.000 *** |
| Domains of Quality of Life | NSSI | No-NSSI | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (Self-Rating) | Mean (Parent Rating) | t-Value | df | p-Value | Corrected p-Value (Bonferroni) | Mean (Self- Rating) | Mean (Parent Rating) | t-Value | df | p-Value | Corrected p-Value (Bonferroni) | |
| School | 3.286 | 3.337 | −0.416 | 97.000 | 0.678 | 1.000 | 2.957 | 3.226 | −2.056 | 92.000 | 0.043 | 0.298 |
| Family | 2.704 | 2.602 | 0.799 | 97.000 | 0.426 | 1.000 | 2.032 | 2.215 | −1.727 | 92.000 | 0.088 | 0.613 |
| Peer relations | 2.429 | 2.622 | −1.271 | 97.000 | 0.207 | 1.000 | 2.172 | 2.527 | −3.169 | 92.000 | 0.002 | 0.015 * |
| Alone activity | 2.143 | 2.071 | 0.487 | 97.000 | 0.627 | 1.000 | 1.796 | 2.043 | −1.885 | 92.000 | 0.063 | 0.438 |
| Physical health | 2.714 | 2.378 | 2.737 | 97.000 | 0.007 | 0.052 | 2.194 | 2.172 | 0.188 | 92.000 | 0.851 | 1.000 |
| Mental health | 3.796 | 3.949 | −1.315 | 97.000 | 0.191 | 1.000 | 3.151 | 3.688 | −4.247 | 92.000 | 0.000 | 0.000 *** |
| Global well-being | 3.378 | 3.673 | −2.608 | 97.000 | 0.011 | 0.074 | 2.667 | 3.419 | −6.850 | 92.000 | 0.000 | 0.000 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gyori, D.; Farkas, B.F.; Horvath, L.O.; Komaromy, D.; Meszaros, G.; Szentivanyi, D.; Balazs, J. The Association of Nonsuicidal Self-Injury with Quality of Life and Mental Disorders in Clinical Adolescents—A Network Approach. Int. J. Environ. Res. Public Health 2021, 18, 1840. https://doi.org/10.3390/ijerph18041840
Gyori D, Farkas BF, Horvath LO, Komaromy D, Meszaros G, Szentivanyi D, Balazs J. The Association of Nonsuicidal Self-Injury with Quality of Life and Mental Disorders in Clinical Adolescents—A Network Approach. International Journal of Environmental Research and Public Health. 2021; 18(4):1840. https://doi.org/10.3390/ijerph18041840
Chicago/Turabian StyleGyori, Dora, Bernadett Frida Farkas, Lili Olga Horvath, Daniel Komaromy, Gergely Meszaros, Dora Szentivanyi, and Judit Balazs. 2021. "The Association of Nonsuicidal Self-Injury with Quality of Life and Mental Disorders in Clinical Adolescents—A Network Approach" International Journal of Environmental Research and Public Health 18, no. 4: 1840. https://doi.org/10.3390/ijerph18041840
APA StyleGyori, D., Farkas, B. F., Horvath, L. O., Komaromy, D., Meszaros, G., Szentivanyi, D., & Balazs, J. (2021). The Association of Nonsuicidal Self-Injury with Quality of Life and Mental Disorders in Clinical Adolescents—A Network Approach. International Journal of Environmental Research and Public Health, 18(4), 1840. https://doi.org/10.3390/ijerph18041840







