Melanoma Prevention: Comparison of Different Screening Methods for the Selection of a High Risk Population
Abstract
1. Introduction
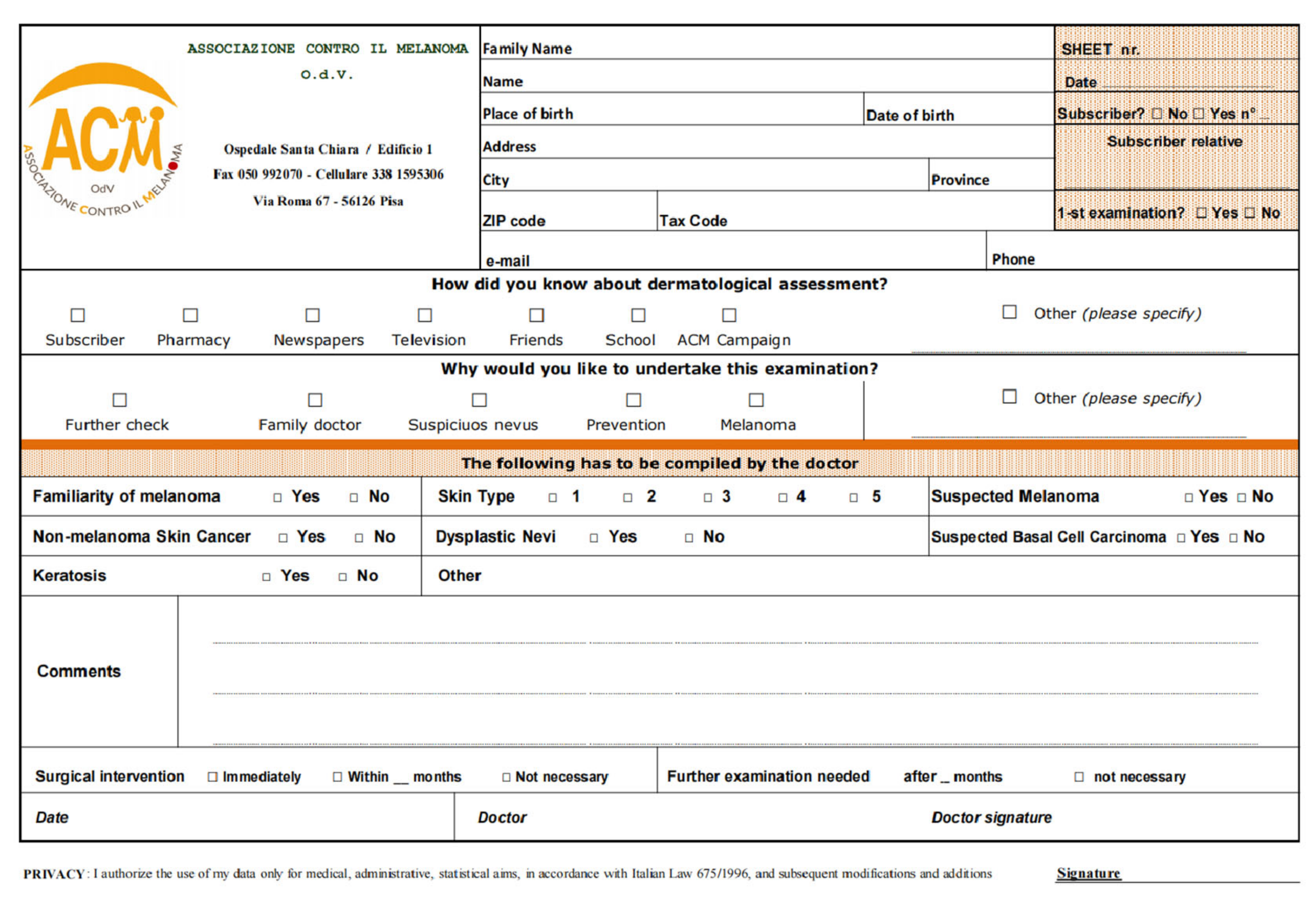
2. Materials and Methods
- Regular skin examinations (RS), conducted all year around primarily within the ACM network, from January 2010 to December 2018;
- Occasional short screening campaigns (OS) lasting 2 weeks every year, from January 2010 to June 2016;
- Selective screening (SS) information campaigns held for 2 weeks yearly where persons were evaluated for the risk of developing melanoma through a quick questionnaire using 10 questions and adapted from the Australian Victorian Melanoma Service Questionnaire [30,31]. Those who fit an intermediate/high risk profile, according to the questionnaire, were recommended to undergo a screening examination from June 2016 to December 2018.
3. Results
Comparison among the Three Recruiting Methods
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Mackie, R.M.; for and on behalf of the Scottish Melanoma Group; Bray, C.; Vestey, J.; Doherty, V.; Evans, A.; Thomson, D.; Nicolson, M. Melanoma incidence and mortality in Scotland 1979–2003. Br. J. Cancer 2007, 96, 1772–1777. [Google Scholar] [CrossRef]
- Ward, E.M.; Sherman, R.L.; Henley, S.J.; Jemal, A.; Siegel, D.A.; Feuer, E.J.; Firth, A.U.; Kohler, B.A.; Scott, S.; Ma, J.; et al. Annual Report to the Nation on the Status of Cancer, Featuring Cancer in Men and Women Age 20–49 Years. JNCI J Natl. Cancer Inst. 2019, 111, djz106. [Google Scholar] [CrossRef]
- American Cancer Society. Facts on Skin Cancer 1993; Document #2049; American Cancer Society: Anchorage, AK, USA, 1993. [Google Scholar]
- Gershenwald, J.E.; Guy, G.P. Stemming the Rising Incidence of Melanoma: Calling Prevention to Action. J. Nat. Cancer Inst. 2016, 108, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gandini, S.; Autier, P.; Boniol, M. Reviews on sun exposure and artificial light and melanoma. Prog. Biophys. Mol. Biol. 2011, 107, 362–366. [Google Scholar] [CrossRef]
- Lasithiotakis, K.; Leiter, U.; Meier, F.; Eigentler, T.; Metzler, G.; Moehrle, M.; Breuninger, H.; Garbe, C. Age and gender are significant independent predictors of survival in primary cuta-neous melanoma. Cancer 2008, 112, 1780–1795. [Google Scholar] [CrossRef] [PubMed]
- Volkovova, K.; Bilanicova, D.; Bartonova, A.; Letašiová, S.; Dusinska, M. Associations between environmental factors and inci-dence of cutaneous melanoma. Rev. Environ. Health 2012, 11 (Suppl. 1), S12. [Google Scholar]
- Titus-Ernstoff, L.; Perry, A.E.; Spencer, S.K.; Gibson, J.; Ding, J.; Cole, B.; Ernstoff, M.S. Multiple primary melanoma: Two-year results from a population-based study. Arch. Dermatol. 2006, 142, 433–438. [Google Scholar] [CrossRef]
- Neale, R.E.; Forman, D.; Murphy, M.F.G.; Whiteman, D.C. Site-specific occurrence of nonmelanoma skin cancers in patients with cutaneous melanoma. Br. J. Cancer 2005, 93, 597–601. [Google Scholar] [CrossRef]
- Farshad, A.; Burg, G.; Panizzon, R.; Dummer, R. A retrospective study of 150 patients with lentigo maligna and lentigo ma-ligna melanoma and the efficacy of radiotherapy using Grenz or soft X-rays. Br. J. Dermatol. 2002, 146, 1042–1046. [Google Scholar] [CrossRef] [PubMed]
- Boniol, M.; Autier, P.; Boyle, P.; Gandini, S. Cutaneous melanoma attributable to sunbed use: Systematic review and me-ta-analysis. BMJ 2012, 345, e4757. [Google Scholar] [CrossRef]
- Cust, A.E.; Armstrong, B.K.; Goumas, C.; Jenkins, M.A.; Schmid, H.; Hopper, J.L.; Kefford, R.F.; Giles, G.G.; Aitken, J.F.; Mann, G.J. Sunbed use during adolescence and early adulthood is associated with increased risk of early-onset melanoma. Int. J. Cancer 2010, 128, 2425–2435. [Google Scholar] [CrossRef]
- Curiel-Lewandrowski, C.; Chen, S.C.; Swetter, S.M.; On behalf of the Melanoma Prevention Working Group-Pigmented Skin Lesion Sub-Committee. Screening and Prevention Measures for Melanoma: Is There a Survival Advantage? Curr. Oncol. Rep. 2012, 14, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.S.; Moore, D.H., II; Mendelsohn, M.L. Screening program reduced melanoma mortality at the Lawrence Livermore National Laboratory, 1984 to 1996. J. Am. Acad. Dermatol. 2008, 58, 741–749. [Google Scholar] [CrossRef][Green Version]
- Whiteman, D.C.; Baade, P.D.; Olsen, C.M. More People Die from Thin Melanomas (≤1 mm) than from Thick Melanomas (>4 mm) in Queensland, Australia. J. Investig. Dermatol. 2015, 135, 1190–1193. [Google Scholar] [CrossRef]
- Geller, A.C.; Elwood, M.; Swetter, S.M.; Brooks, D.R.; Aitken, J.; Youl, P.H.; Demierre, M.-F.; Baade, P.D. Factors related to the presentation of thin and thick nodular melanoma from a popula-tion-based cancer registry in Queensland Australia. Cancer 2009, 115, 1318–1327. [Google Scholar] [CrossRef]
- Swetter, S.M.; Geller, A.C. Perspective: Catch melanoma early. Nat. Cell Biol. 2014, 515, S117. [Google Scholar] [CrossRef] [PubMed]
- Guy, G.P., Jr.; Machlin, S.R.; Ekwueme, D.U.; Yabroff, K.R. Prevalence and costs of skin cancer treatment in the U.S.; 2002–2006 and 2007–2011. Am. J. Prev. Med. 2015, 48, 183–187. [Google Scholar] [CrossRef]
- Rossi, C.R.; Vecchiato, A.; Bezze, G.; Mastrangelo, G.; Montesco, M.C.; Mocellin, S.; Meneghetti, G.; Mazzoleni, F.; Peserico, A.; Lise, M. Early detection of melanoma: An educational campaign in Padova, Italy. Melanoma Res. 2000, 10, 181–187. [Google Scholar] [CrossRef]
- De Rooij, M.J.M.; Rampen, F.H.J.; Schouten, L.J.; Neumann, H.A.M. Total skin examination during screening for malignant mel-anoma does not increase the detection rate. Br. J. Dermatol. 1996, 135, 42–45. [Google Scholar] [CrossRef]
- Stratigos, A.; Nikolaou, V.; Kedicoglou, S.; Antoniou, C.; Stefanaki, I.; Haidemenos, G.; Katsambas, A.D. Melanoma/skin cancer screening in a Mediterranean country: Results of the Eu-romelanoma Screening Day Campaign in Greece. J. Eur. Acad. Dermatol. Venereol. 2007, 21, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Campbell, S.M.; Sroa, N.; Winkelmann, R.R.; Olencki, T.; Bechtel, M. A Global Review of Melanoma Follow-up Guidelines. J. Clin. Aesthetic Dermatol. 2013, 6, 18–26. [Google Scholar]
- MacArthur, K.; Morris, L. Is screening for melanoma effective in primary care? Evid.-Based Pr. 2014, 17, 13. [Google Scholar] [CrossRef]
- Sui, A.; Wiedmann, M.; Guthmann, R. Does screening for melanoma improve mortality rates? Evid. Based Pr. 2020. [Google Scholar] [CrossRef]
- Rat, C.; Grimault, C.; Quereux, G.; Dagorne, M.; Gaultier, A.; Khammari, A.; Dreno, B.; Nguyen, J.-M. Proposal for an annual skin examination by a general practitioner for patients at high risk for melanoma: A French cohort study. BMJ Open 2015, 5, e007471. [Google Scholar] [CrossRef]
- Johansson, M.; Brodersen, J.; Gøtzsche, P.C.; Jørgensen, K.J. Screening for reducing morbidity and mortality in malignant melanoma. Cochrane Database Syst. Rev. 2019, 2019, CD012352. [Google Scholar] [CrossRef]
- Loomans-Kropp, H.A.; Umar, A. Cancer prevention and screening: The next step in the era of precision medicine. NPJ Precis. Oncol. 2019, 3, 1–8. [Google Scholar] [CrossRef]
- Gøtzsche, P.C.; Jørgensen, K.J. Screening for breast cancer with mammography. Cochrane Database Syst. Rev. 2013, 6, CD001877. [Google Scholar] [CrossRef]
- Bretthauer, M.; Fretheim, A.; Odgaard-Jensen, J.; Hoff, G.; Odgaard-Jensen, J. Flexible sigmoidoscopy versus faecal occult blood testing for colorectal cancer screening in asymptomatic individuals. Cochrane Database Syst. Rev. 2013, 9, CD009259. [Google Scholar] [CrossRef]
- Alfred Health Victoria. Melanoma Risk Calculator for the General Public. 2020. Available online: https://www.alfredhealth.org.au/melanoma-risk-calculator/public (accessed on 7 October 2020).
- Alfred Health Victoria. Melanoma Risk Factors. 2020. Available online: https://www.alfredhealth.org.au/services/statewide-services/victorian-melanoma-service/melanoma-risk-factors (accessed on 7 October 2020).
- Piscitelli, P.; Neglia, C.; Falco, A.; Rivezzi, M.; Agnello, N.; Argentiero, A.; Chitano, G.; Distante, C.; Della Rosa, G.; Vinci, G.; et al. Melanoma in the Italian Population and Regional Environmental Influences: A National Retrospective Survey on 2001–2008 Hospitalization Records. Int. J. Environ. Res. Public Health 2015, 12, 9102–9118. [Google Scholar] [CrossRef]
- Victorian Melanoma Service at the Alfred Hospital (Melbourne, Australia). Available online: https://www.alfredhealth.org.au/services/melanoma-service (accessed on 10 October 2020).
- Welch, H.G.; Black, W.C. Overdiagnosis in Cancer. J. Natl. Cancer Inst. 2010, 102, 605–613. [Google Scholar] [CrossRef] [PubMed]
- Michielin, O.; Van Akkooi, A.C.J.; Ascierto, P.A.; Dummer, R.; Keilholz, U.; ESMO Guidelines Committee. Cutaneous melanoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2019, 30, 1884–1901. [Google Scholar] [CrossRef] [PubMed]
- Associazione Contro il Melanoma OdV (ACM) (Pisa, Italy). Available online: https://www.associazionecontromelanoma.it/ (accessed on 10 October 2020).
- Lim, S.Y.; Lee, J.H.; Diefenbach, R.J.; Kefford, R.F.; Rizos, H. Liquid biomarkers in melanoma: Detection and discovery. Mol. Cancer 2018, 17, 1–14. [Google Scholar] [CrossRef] [PubMed]

| Variable | Levels | Counts (%) |
|---|---|---|
| Age (years) | 1–25 | 402 (18.6) |
| 26–45 | 742 (34.3) | |
| 46–65 | 754 (34.9) | |
| 66–85 | 264 (12.2) | |
| NA | 76 (3.4) | |
| Sex | F | 1403 (62.7) |
| M | 835 (37.3) | |
| NA | 0 (0) | |
| Family history | NO | 1903 (85.0) |
| YES | 335 (15.0) | |
| NA | 0 (0) | |
| Skin phototype | III-IV-V | 1009 (45.1) |
| I-II | 1229 (54.9) | |
| NA | 0 (0.0) | |
| Melanoma history | NO | 2165 (96.7) |
| YES | 73 (3.3) | |
| NA | 0 (0.0) | |
| Dysplastic nevi | NO | 2199 (98.3) |
| YES | 39 (1.7) | |
| NA | 0 (0.0) | |
| Seborrheic keratosis | NO | 1787 (79.8) |
| YES | 451 (20.2) | |
| NA | 0 (0.0) | |
| Non-melanoma skin cancer | NO | 2212 (98.8) |
| YES | 26 (1.2) | |
| NA | 0 (0.0) | |
| Recommended follow-up | NO | 1028 (45.9) |
| YES | 1179 (59.7) | |
| NA | 31 (1.4) | |
| Surgery indication | NO | 2007 (89.7) |
| YES | 200 (8.9) | |
| NA | 31 (1.4) | |
| How did people learn about us? | Friends | 303 (13.5) |
| Pharmacists | 77 (3.4) | |
| Media | 133 (5.9) | |
| School | 13 (0.6) | |
| ACM subscribers | 300 (13.5) | |
| ACM campaigns | 160 (7.1) | |
| Other | 404 (18.1) | |
| NA | 848 (37.9) | |
| Reason for skin check | Presence of a Skin lesion | 204 (9.1) |
| Prevention | 1153 (51.5) | |
| Other | 12 (0.5) | |
| NA | 869 (38.8) |
| Variable | Counts (%) | p-Value (Univar.) | p-Value (Multivar.) | ||
|---|---|---|---|---|---|
| RS1094 (48.9) | OS826 (36.9) | SS318 (14.2) | |||
| Age (years) | 6.479 × 10−5 | - | |||
| ≤25 | 218 (19.9) | 139 (16.8) | 45 (14.2) | ||
| 26–45 | 352 (32.2) | 279 (33.9) | 111 (34.9) | ||
| 46–65 | 354 (32.4) | 291 (35.2) | 109 (34.3) | ||
| ≥65 | 133 (12.2) | 78 (9.4) | 53 (16.7) | ||
| NA | 37 (3.4) | 39 (4.7) | 0 (0.0) | ||
| Sex | 0.02093 | - | |||
| F | 668 (60.9) | 549 (66.4) | 190 (59.7) | ||
| M | 428 (39.1) | 277 (33.6) | 128 (40.3) | ||
| NA | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Family history | 0.006994 | 0.0115 | |||
| NO | 921 (84.2) | 725 (87.,8) | 257 (80.8) | ||
| YES | 173 (15.8) | 101 (12.2) | 61 (19.2) | ||
| NA | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Phototype | 5.92 × 10−15 | 1 × 10−5 | |||
| III-IV-V | 438 (40.0) | 462 (55.9) | 109 (34.3) | ||
| I-II | 656 (60.0) | 364 (44.1) | 209 (65.7) | ||
| NA | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Melanoma history | n.s. | n.s. | |||
| NO | 1060 (96.9) | 794 (96.1) | 311 (97.8) | ||
| YES | 34 (3.1) | 32 (3.9) | 7 (2.2) | ||
| NA | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Dysplastic nevi | n.s. | n.s. | |||
| NO | 1078 (98.5) | 810 (98.1) | 311 (97.8) | ||
| YES | 16 (1.5) | 16 (1.9) | 7 (2.2) | ||
| NA | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Seborrheic keratosis | n.s. | - | |||
| NO | 855 (78.2) | 674 (81.6) | 258 (81.1) | ||
| YES | 239 (21.8) | 152 (18.4) | 60 (18.9) | ||
| NA | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Non-melanoma skin cancer | n.s. | - | |||
| NO | 1046 (95.6) | 793 (96.0) | 294 (92.5) | ||
| YES | 48 (4.4) | 33 (4.0) | 24 (7.5) | ||
| NA | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Recommended follow-up | 2.2 × 10−16 | - | |||
| NO | 565 (51.7) | 407 (49.3) | 56 (17.6) | ||
| YES | 507 (46.3) | 413 (50.0) | 259 (81.5) | ||
| NA | 22 (2.0) | 6(0.7) | 3(0.9) | ||
| Advised Surgical Removal | 0.04405 | - | |||
| NO | 985 (90.0) | 747 (90.5) | 275 (86.5) | ||
| YES | 87 (8.0) | 73 (8.8) | 40 (12.6) | ||
| NA | 22 (2.0) | 6(0.7) | 3(0.9) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dubbini, N.; Puddu, A.; Salimbeni, G.; Malloggi, S.; Gandini, D.; Massei, P.; Ferraùto, G.; Rubino, T.; Ricci, L.; Menchini, G.; et al. Melanoma Prevention: Comparison of Different Screening Methods for the Selection of a High Risk Population. Int. J. Environ. Res. Public Health 2021, 18, 1953. https://doi.org/10.3390/ijerph18041953
Dubbini N, Puddu A, Salimbeni G, Malloggi S, Gandini D, Massei P, Ferraùto G, Rubino T, Ricci L, Menchini G, et al. Melanoma Prevention: Comparison of Different Screening Methods for the Selection of a High Risk Population. International Journal of Environmental Research and Public Health. 2021; 18(4):1953. https://doi.org/10.3390/ijerph18041953
Chicago/Turabian StyleDubbini, Nevio, Antonella Puddu, Grazia Salimbeni, Stefano Malloggi, Daniele Gandini, Pietro Massei, Giuseppe Ferraùto, Tommaso Rubino, Laura Ricci, Giovanni Menchini, and et al. 2021. "Melanoma Prevention: Comparison of Different Screening Methods for the Selection of a High Risk Population" International Journal of Environmental Research and Public Health 18, no. 4: 1953. https://doi.org/10.3390/ijerph18041953
APA StyleDubbini, N., Puddu, A., Salimbeni, G., Malloggi, S., Gandini, D., Massei, P., Ferraùto, G., Rubino, T., Ricci, L., Menchini, G., Celli, M., Ghilardi, M., Gianfaldoni, R., Gianfaldoni, S., Nannipieri, A., & Romanini, A. (2021). Melanoma Prevention: Comparison of Different Screening Methods for the Selection of a High Risk Population. International Journal of Environmental Research and Public Health, 18(4), 1953. https://doi.org/10.3390/ijerph18041953






