Traditionally, four dominant methods are mentioned in the literature on the organization of nursing care delivery: functional nursing, individual, team nursing, and primary nursing [
4]. The work methods are conceptually organized into two major groups: the task-oriented method and the person-centered methods (
Table 1). These methods are internationally recognized and commonly applied in clinical settings to support the organization in nursing care delivery, reflecting the social values, management ideologies, and resources of a team or organization [
6].
4.1.1. Functional Nursing Method (Task-Oriented)
The functional nursing method became popular during World War II, given the need for nurses to care for many wounded people in hospital settings [
22]. The delivery of nursing care was based on the distribution of standardized tasks by the nurses, who achieved proficiency through the systematic repetition of techniques (such as intravenous drug administration and vital signs monitoring). However, with the end of the war and the sudden increase in birth rates in the following years, this method of care delivery persisted and is still used today in specific clinical contexts [
22], which is considered inappropriate given the associated risks for the quality of care delivery.
Functional nursing, also known as task nursing, focuses on the distribution of work based on the performance of tasks and procedures, where the target of the action is not the patient but rather the task [
23]. The work is thus broken down into tasks performed by different professionals, from a mechanistic perspective [
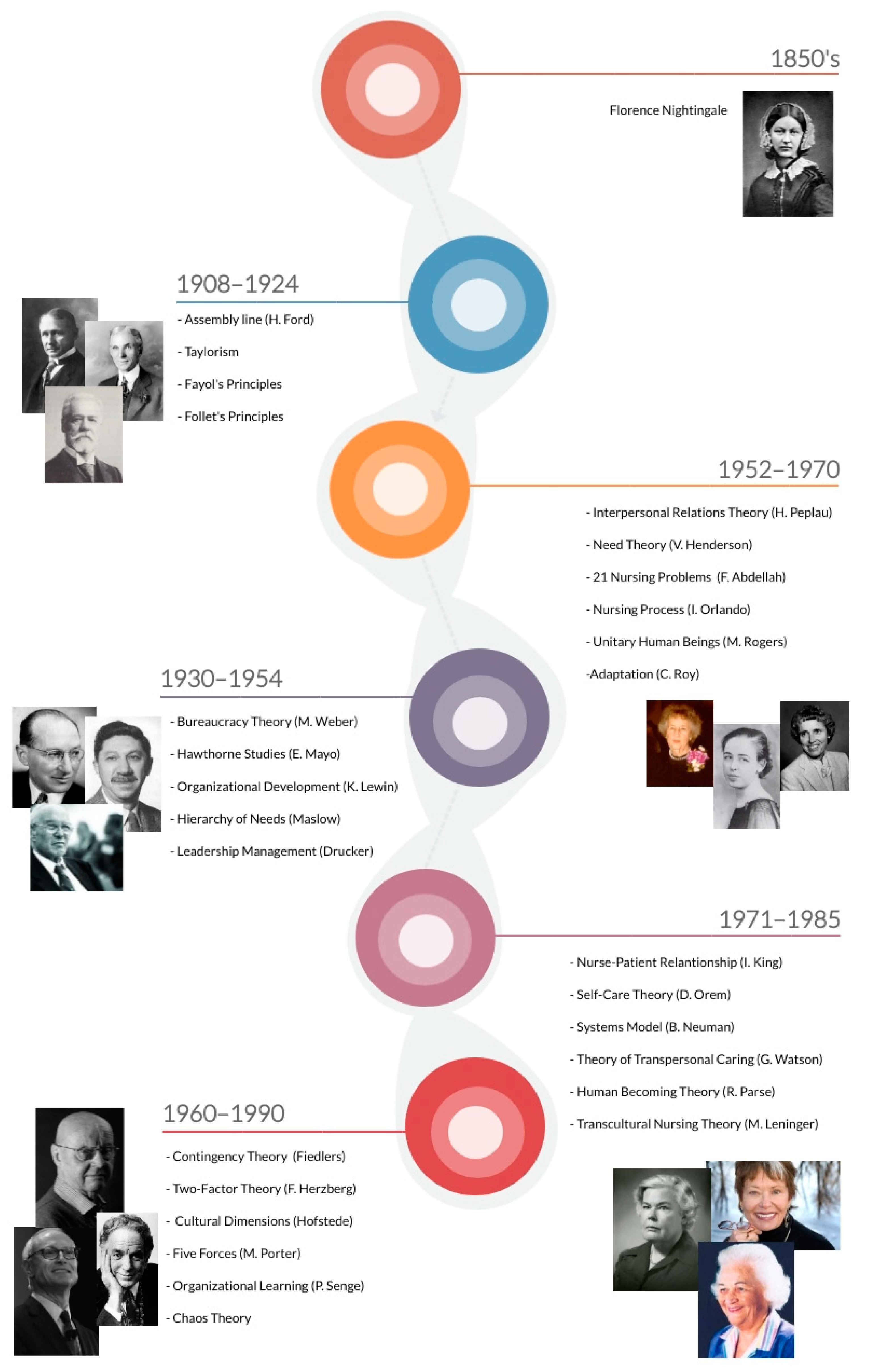
1]. The adoption of this method in care organization is based on Taylor’s principles of the industrial revolution, promoting the maximization of the task in a routine and mechanistic logic. As shown in
Figure 3, this care delivery model is characterized by a lack of coordination between the parts, represented by “piecemeal” interventions in task-oriented care delivery, of an interrelated whole (non-holistic care to the patient). However, a significant number of health managers and administrators believe that “functional” nursing is an economically efficient care delivery method [
22].
This method of classical inspiration in the industrial revolution was used when human resources were scarce because it required a smaller number of professionals [
1] or when it was intended to develop manual dexterity/improve a technique to obtain a better performance. The functional nursing method reduces communication between health team members. The performance of tasks is assumed as the primary purpose in this method, where each nurse “routinizes” the provision of care instead of adopting procedures to provide personalized care to meet each patient’s needs [
4]. This fragmented approach sees the patient as a “place” where nursing care is provided [
1], without significant advantages for the patient. A single advantage for nurses is the increase in manual dexterity when approached as a technique and not as a method. For the organization, the advantages include its immediate efficiency that is translated into an apparent improvement in productivity since it requires fewer nurses, despite the costs derived from the disastrous consequences on quality of care due to safety failures with accident rates and avoidable adverse events [
6].
However, there are several disadvantages. For patients, it does not allow for personalized care, which dehumanizes them, leading to poor quality care and major flaws in patient safety when compared to other methods; it causes more complaining from patients, who are divided by tasks and, consequently, by different professionals, promoting unaccountability; it does not allow the delivery of comprehensive care; it damages the nurse-patient relationship because the patient is not familiar with “his/her” nurse and promotes patient insecurity [
6].
For nurses, it does not allow the application of the nursing process, leading to major difficulties in the identification of patient needs and poor records; it does not promote the continuity of care; it leads to some activities being “forgotten” due to lack of planning; the nurse does not have an overall view of “his/her” patient; it hinders the assessment of care; it increases the risk of healthcare-associated infections (HAIs); it hinders the interaction and the interpersonal relationships between health professionals; it creates poor team spirit and lack of motivation by “routinizing” tasks that are repeatedly performed by the same nurses (Taylorism). Although this method does not currently have a framework in nursing theories, it still seems to be alluded to and practiced based on the classical theories of the industrial revolution. For the organizations, this method results in poor quality and dissatisfied patients.
4.1.2. Person-Centered Care
In person-centered methods, care is delivered according to the scientific method, starting with the identification of the nursing care needs, the definition of priorities, planning, implementation, and evaluation of interventions, providing individualized and personalized care to the patient as an interconnected and integrated whole. It is part of the humanistic perspectives, valuing the relationship and the concern for the other, where the whole is more than the sum of its parts. Thus, it comes closer to the systemic-contingency perspectives.
Individual Method
Known as the case method or total patient care approach, it corresponds to a situation where a single nurse assumes full responsibility for delivering care to a group of patients during a shift [
24]. Although care is not fragmented, its coordination does not prevail between shifts, and changes may occur in the established nursing care plan [
1]. In this method, the overall organization of care to meet the needs identified by the nurse depends on the nurse’s view of his/her role as a professional and may prioritize the patient or the performance of tasks (
Figure 4). In addition, and because the individual method limits the nurses’ action during a shift and the patient(s) to which he/she is allocated, outcome evaluation is based only on circumstantial objectives [
22]. The coordination of the care delivered to all patients in the unit is under the responsibility of a single nurse, usually the head nurse, who supervises and evaluates the delivery of nursing care and makes the most significant decisions throughout the process. However, care delivery in that shift is delegated to the nurse allocated to that shift.
This method has the following advantages for patients: the individualization of care, with satisfaction of their needs; it promotes the nurse-patient relationship; the patient can identify the nurse who provides care in a given shift, resulting in a close, humanized, and personalized care, which also reinforces the confidence in the nurse and the patient’s safety.
For nurses, it promotes the application of the nursing process and the consequent identification and satisfaction of patient needs, with a better ability to make decisions while considering the biopsychosocial totality of human beings; it allows the continuity of care and leads to a reduction of the number of errors and/or omissions, increasing quality; the patient’s deeper knowledge of the nurse leads to greater satisfaction and less effort by establishing an intentional therapeutic relationship; it leads to the development of the nurses’ individual skills and abilities; it promotes greater autonomy in care delivery, responsibility, creativity, knowledge updating, and the evaluation of the quality of care delivery. For the organizations, it translates mainly into higher quality in care delivery [
6].
This method also has some disadvantages/weaknesses. For patients, as each nurse will provide care to different patients in each shift, there is no nurse or figure of reference to whom he can talk to during the hospital stay as “his/her” primary nurse. Due to differences in the individual skills and knowledge of the nurses who provide care, asymmetry can be created in care delivery, leading to heterogeneity in the several shifts related to different levels of care being delivered. For nurses, it has some potential for emotional involvement with the patients and requires a higher level of proficiency from all nurses. For organizations, it requires more staff than the task-oriented method.
Team Nursing Method
This method emerged in the 1950s as a response to low nurse staffing and widespread dissatisfaction among the professionals and patients with the functional nursing method [
24]. It was created to take advantage of the mix of skills of the several members of the nursing teams. This method implements a philosophy where a leader leads a group of people. Thus, it is not considered a procedure. In this philosophy, all team members are familiar with the patient’s needs and/or problems, contributing in a particular way to his/her well-being [
22]. Thus, the team nursing method assumes that the care provided will be of higher quality, efficacy, and safety when planned and provided as a team, due to the individual contributions of each nurse [
7]. Nurses are divided into teams and guided and coordinated by leaders, maximizing the group’s capabilities and the individual qualifications and skills of each nurse [
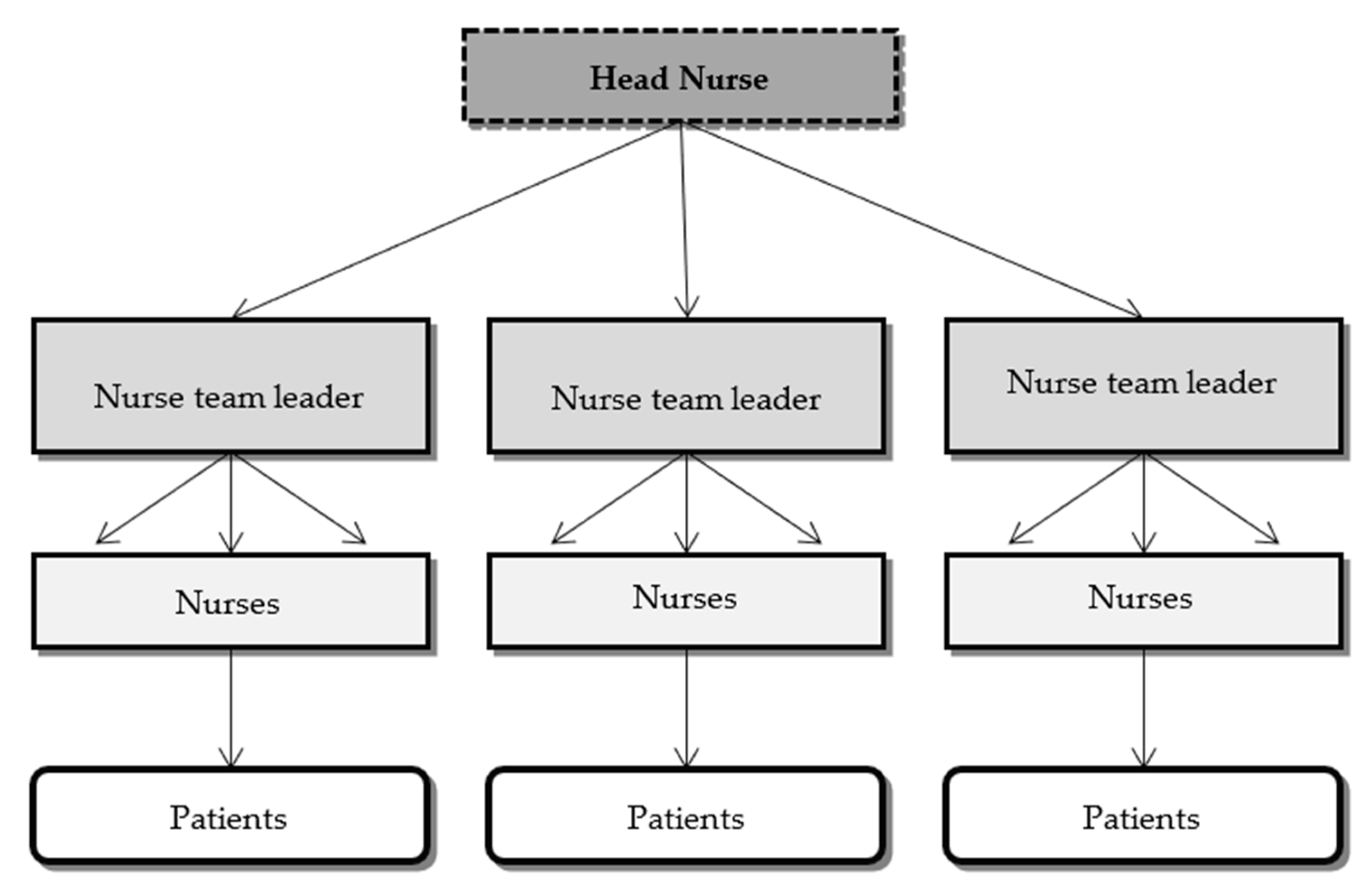
1]. Thus, each team is responsible for the full delivery of care to the patients who are under its responsibility (
Figure 5).
This method is based on two fundamental pillars: (i) leadership in the planning and evaluation of care delivery to each patient; and (ii) effective communication to ensure continuity of care [
7]. According to Kron and Gray [
23], it rests on the principle that all patients can receive better care, provided under the leadership of a nurse who is responsible for: (i) assessing each patient and determining the appropriate nursing intervention; (ii) coordinating planning and intervention; (iii) keeping care plans up to date; and (iv) ensuring that the records of care delivery are made.
In the literature, there are some misconceptions about the team nursing method, which, according to Kron and Gray [
23], are unjustified. According to the authors, the team nursing method does not correspond to the distribution on a functional basis to the various team members or the division of units. Further pointed out as a fragility, it does not refer to the division of responsibilities and patients equally among team members, that is, it does not consist only of cooperation or teamwork. The team nursing method aims to decentralize responsibilities, fighting against the traditional notion of nursing leadership and management concentrated on a single individual. Thus, each nurse recognizes the patients assigned to their team, contributing individually to the satisfaction of their needs. This reality facilitates the consensus among nurses regarding the nursing care provided in the units, laying the foundation for the creation of a school of leaders.
This method has the following advantages/strengths for patients: it promotes a feeling of security as care needs are met by a group of nurses with different levels of skills; it leads to effectiveness in care delivery; and it promotes close and personalized care, increasing patient satisfaction. For nurses, it values and increases communication, teamwork, and leadership; it ensures support from the most experienced and competent (experts) nurses to recent graduates, who are less competent and less experienced; it allows for the development of knowledge and skills through effective work; and it ensures the identification of training needs. For the institutions, it promotes leadership skills, taking advantage of the competencies and skills of all team members; it increases satisfaction; and it facilitates the implementation of new methodologies within the team.
However, its application also has limitations. The patient cannot identify a primary nurse who cares for him/her, which hinders referral. It does not guarantee care delivery in another shift by the same team. For nurses, it can fall into the task method because it requires more effort, dynamism, and quality in interpersonal relationships, and difficulties may arise in interaction and collaboration. Nevertheless, if there is a conceptual awareness of the philosophy underlying this method, this problem will not arise. It may also lead to an unfair distribution or omission of some activities that ought to be performed and even incompetence by some members. It also requires greater knowledge of several patients. For the institutions, it also requires a higher number of nurses than the functional nursing method and the individual method.
Primary Nursing Method
This work method was first called primary nursing, and it was developed in 1968 under the direction of Marie Manthey at the University of Minnesota Hospitals, USA [
25]. The primary nursing method is based on the idea that a nurse is responsible for planning, delivering, and evaluating the care of one or more patients from the moment of admission to discharge [
22].
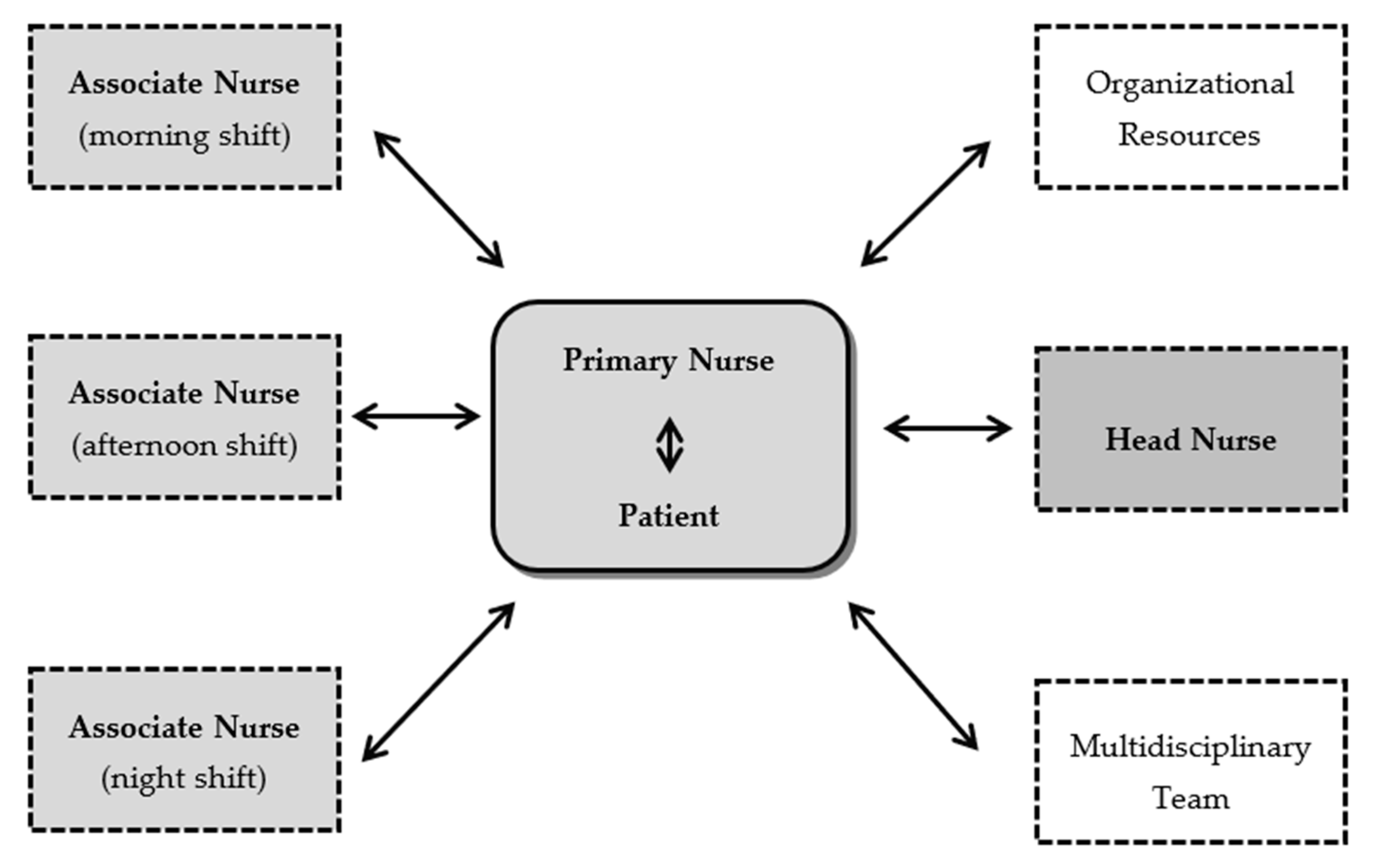
In order to allow continuity of care, each primary nurse is assisted by associate nurses. The delegation of care to associate nurses occurs whenever the primary nurse is not present. Thus, nurses may be simultaneously primary nurses for some patients and associate nurses of other nurses (
Figure 6). However, ultimately, the primary nurse will always be responsible for the coordination of the clinical decisions and supervision during the hospital stay [
1].
This method has several advantages. For the patient, it allows them, better than any other method, to identify who will be the primary nurse during the hospitalization, ensuring continuity of care as no other method [
26], reducing the number of nurses issuing nursing prescriptions/interventions, and reducing the likelihood of errors. The primary nursing method promotes the relationship between nurses and patients, allowing personalized care and increased satisfaction [
27]. For the nurse, it promotes the relationship with the patient, maximizes the identification of needs (due to the deep knowledge of the patient’s status), and the capacity for prescription and evaluation, and allows the identification of the outcomes of their work in terms of health gains, such as a reduction in the number of infections associated with urinary, central, and peripheral catheters [
28]. It also facilitates the communication between nurse/nurse, nurse/patient, nurse/family, nurse/doctor, and nurse/other health professional; it facilitates the training of patients and/or informal caregivers, and promotes a more effective and efficient discharge planning [
29]. Furthermore, it gives greater autonomy to nurses, personalizes responsibility, values nurses’ autonomous interventions, and promotes creativity [
30]. For the institution, this method ensures a higher quality of care, increases patient/family satisfaction, and facilitates the internal mobility of staff and the maximization of their performance [
29].
It also has some disadvantages for the patient, such as the discontinuity in the quality of care that depends on the nurses’ qualifications. In turn, it limits the differentiation and performance of associate nurses, carries a risk of emotional involvement with the patient, and can increase stress [
31]. Given that not all nurses have differentiated training, knowledge, and decision-making capacity, some nurses will not be able to assume the responsibility of coordination [
32,
33]. For the institution, the implementation of this method requires more staff, raises questions regarding the equity of care, requires greater preparation of associate nurses, and requires greater investment in team staffing.
However, according to Kusk and Groenkjaer [
25], although the primary nursing method was widely disseminated more than 50 years ago, only a few studies have been conducted to identify its advantages. In fact, according to the authors, the evidence that supports the superiority of this method over those previously presented “is mainly based on anecdotal or descriptive studies” rather than on quantitative data derived from robust research studies, with genuine control units/institutions, outcomes of interest, and appropriate measurement instruments [
25], despite the results that the research may show.
4.1.3. Critical and Comparative Analysis of Nursing Work Methods
There are four nursing work methods identified: functional nursing, individual, team nursing, and primary nursing. Although conceptually, the task-oriented work methods do not show similarities with the person-centered methods, it is still possible to represent their key aspects in a single table, distinguishing them in terms of complexity of care delivery (
Figure 7).
Thus, the primary nursing method seems to be the one with the most developed key aspects, contrasting with the functional nursing method. In addition, it is the method that most promotes planning, autonomy, responsibility, decision-making skills, and continuity of nursing care.
Sellick and collaborators [
34] compared the functional nursing method and the primary nursing method in two internal medicine units and identified statistically significant differences between the levels of satisfaction of inpatients. In the units under the primary nursing method, the patients reported that the nurses had a more global view of their needs and, consequently, were more concerned with care, communicated more with them and their families, and planned their discharge in a timely and gradual way. From the nurses’ perspective, the primary nursing method increased their satisfaction, enabled them to use all their skills, and made them feel more fulfilled by the profession [
34].
However, Fernandez and collaborators [
35] found contrary results. The adoption of the team nursing method showed a higher level of documentation of care and earlier discharge planning when compared to the primary nursing method. This fact indicates that implementing the primary nursing method in a clinical context is not always a success [
1] because it can be adopted in an inconsistent and unstructured manner, not taking into account the level of competence of the primary element. Huber [
1] tells us about this barrier to more inexperienced nurses, which may culminate in burnout for nurses who are fully responsible for delivering care to a patient without proper preparation. There are limitations in the implementation of this method related to budget and pressure for shorter hospitalizations despite the complexity of care [
36].
A systematic review of the literature conducted by King and collaborators [
7] sought to determine the effectiveness of the team nursing method when compared to the individual method, considering staff well-being (assessed through their satisfaction, absenteeism, stress, and burnout). Although differences were found in specific subdomains of satisfaction, the care organization method in force was not significantly different for nurses. Given their importance for nurses, the authors found that the available human resources, the stability in staffing, the size of the units, the professionals’ skill mix and experience, as well as the ethos of care, should be considered when implementing a care delivery and organization method. However, this process should be based on effective leadership, creating a supportive environment for all professionals [
7].
In a systematic literature review with 2000 participants, Fernandez and collaborators [
35] found that the work methods influenced not only the care provided to the patient and family but also the dynamics of the clinical context and existing professional interrelations. Concerning the delivery of care to patients, the authors did not find consistent results regarding the incidence of falls in services under the teamwork method. However, for the same method, two studies showed that its adoption in the clinical context is statistically associated with lower levels of pain reported by patients and lower incidence of medication errors and adverse outcomes. They also found that the delivery of care using a “hybrid” model, that is, a combination of characteristics of the individual method and the team nursing method, resulted in improved quality of care, especially regarding a reduction in restraint use, but without any impact on the incidence of pressure areas or healthcare-associated infections.
Thus, it is up to nurse managers to recognize the needs and strengths of their nursing team based on their interrelationship with the extended health team and the patients, contextualizing them in a specific sociocultural, geographical, economic, and temporal background. In this line of thought, the discussion of the work method to be used in each clinical context should focus on its dynamics, organization, level of complexity, and required conceptual framework.
One could ask “What is the best response to our patients’ nursing care needs?”. In patient-centered organizations, with a high focus on the promotion of quality of care, more than choosing a crystal-clear model, it is important to ensure the satisfaction of the patient’s nursing needs, preferably with gains for all those involved. In our opinion, supported by the theoretical-conceptual framework of management and nursing and the available studies, this can be achieved through a combination of methods, that is, hybrid methods if they are patient-centered.
Several authors believe that the primary nursing method is the one that best answers the issues of humanization and quality of nursing interventions, with the patient and his/her family at the center of care [
1,
37,
38]. According to Wessel and Manthey [
38], this method is the one that best supports the nurses’ professional practice, focusing on the nurse/patient relationship, facilitating the participation and involvement of the family in care delivery, and enhancing patient outcomes. The primary nursing method focuses on the therapeutic relationship with patients and families, creating the opportunity for nurses to develop their professional role where their technical and relational skills are equally valued and sustained [
38]. The primary nursing method provides a high level of knowledge of the patient and his/her family, promoting in-depth case management. Primary nurses gradually become proficient in decision-making and continuity of care, evidencing advanced skills for the management of complex needs. Thus, nursing teams should have this profile of competencies and be prepared to apply this method to patients with advanced nursing care needs (e.g., patients who are expected to remain dependent on their caregivers after discharge, situations of transition from demanding care, serious chronic diseases, initial stage of the disease/dependence, sudden health transitions, or transitions that are difficult to accept).
Nonetheless, we believe that the work method to be adopted is essentially based on the way care is conceived and planned, its intentionality and awareness, and that it is later reflected in the way nurses organize, deliver, and evaluate this same care. Thus, it is not simply because a nurse collaborates with a shift colleague in a particular activity that we have to consider the functional nursing method or the task-oriented method. After all, if care is designed centered on the patient, it will necessarily and always give priority to the patient and not to the task.