Impact of Service User Video Presentations on Explicit and Implicit Stigma toward Mental Illness among Medical Students in Nepal: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Setting
2.2. Intervention Videos
2.3. Sample and Procedure
2.4. Outcome Measures
2.5. Data Collection and Management
2.6. Ethics and Human Subjects’ Protection
2.7. Data Analysis
3. Results
3.1. Study 1 (Depression only)
3.1.1. Study 1 Sample Description
3.1.2. Study 1 Outcomes
3.1.3. Study 1 Qualitative Findings
3.2. Study 2 (Depression and Psychosis)
3.2.1. Study 2 Sample Description
3.2.2. Study 2 Outcomes
3.3. Comparison between Study 1 (Depression only) and Study 2 (Depression and Psychosis)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Henderson, C.; Noblett, J.; Parke, H.; Clement, S.; Caffrey, A.; Gale-Grant, O.; Schulze, B.; Druss, B.; Thornicroft, G. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry 2014, 1, 467–482. [Google Scholar] [CrossRef]
- Thornicroft, G.; Rose, D.; Kassam, A. Discrimination in health care against people with mental illness. Int. Rev. Psychiatry 2007, 19, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Suwalska, J.; Suwalska, A.; Neumann-Podczaska, A.; Łojko, D. Medical students and stigma of depression. Part I. Stigmatization of patients. Psychiatr. Pol. 2017, 51, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Stefanovics, E.; He, H.; Ofori-Atta, A.; Cavalcanti, M.T.; Neto, H.R.; Makanjuola, V.; Ighodaro, A.; Leddy, M.; Rosenheck, R. Cross-national analysis of beliefs and attitude toward mental illness among medical professionals from five countries. Psychiatr. Q. 2016, 87, 63–73. [Google Scholar] [CrossRef]
- Economou, M.; Peppou, L.; Geroulanou, K.; Kontoangelos, K.; Prokopi, A.; Pantazi, A.; Zervakaki, A.; Stefanis, C. Attitudes of psychology students to depression and its treatment: Implications for clinical practice. Psychiatrike 2017, 28, 46. [Google Scholar] [CrossRef] [Green Version]
- Fernando, S.M.; Deane, F.P.; McLeod, H.J. Sri Lankan doctors’ and medical undergraduates’ attitudes towards mental illness. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 733–739. [Google Scholar] [CrossRef]
- Lyons, Z.; Janca, A. Impact of a psychiatry clerkship on stigma, attitudes towards psychiatry, and psychiatry as a career choice. BMC Med. Educ. 2015, 15, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poreddi, V.; Thimmaiah, R.; Math, S.B. Attitudes toward people with mental illness among medical students. J. Neurosci. Rural Pract. 2015, 6, 349. [Google Scholar]
- Prathaptharyan, T.J.; Annatharyan, D. Attitudes of ’tomorrow’s doctors’ towards psychiatry and mental illness. Natl. Med. J. India 2001, 14, 355–359. [Google Scholar]
- Giasuddin, N.A.; Levav, I.; Gal, G. Mental health stigma and attitudes to psychiatry among bangladeshi medical students. Int. J. Soc. Psychiatry 2015, 61, 137–147. [Google Scholar] [CrossRef]
- Korszun, A.; Dinos, S.; Ahmed, K.; Bhui, K. Medical student attitudes about mental illness: Does medical-school education reduce stigma? Acad. Psychiatry 2012, 36, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Aydin, N.; Yigit, A.; Inandi, T.; Kirpinar, I. Attitudes of hospital staff toward mentally ill patients in a teaching hospital, Turkey. Int. J. Soc. Psychiatry 2003, 49, 17–26. [Google Scholar] [CrossRef]
- Griffiths, K.M.; Carron-Arthur, B.; Parsons, A.; Reid, R. Effectiveness of programs for reducing the stigma associated with mental disorders. A meta-analysis of randomized controlled trials. World Psychiatry 2014, 13, 161–175. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.; Clement, S.; Marcus, E.; Stona, A.-C.; Bezborodovs, N.; Evans-Lacko, S.; Palacios, J.; Docherty, M.; Barley, E.; Rose, D. Evidence for effective interventions to reduce mental health-related stigma and discrimination in the medium and long term: Systematic review. Br. J. Psychiatry 2015, 207, 377–384. [Google Scholar] [CrossRef] [Green Version]
- Corrigan, P.W.; Kerr, A.; Knudsen, L. The stigma of mental illness: Explanatory models and methods for change. Appl. Prev. Psychol. 2005, 11, 179–190. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Morris, S.B.; Michaels, P.J.; Rafacz, J.D.; Rusch, N. Challenging the public stigma of mental illness: A meta-analysis of outcome studies. Psychiatr. Serv. 2012, 63, 963–973. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Wu, S.I.; Biswas, M.; Yate, M.; Aoki, Y.; Barley, E.A.; Thornicroft, G. Effects of short-term interventions to reduce mental health-related stigma in university or college students: A systematic review. J. Nerv. Ment. Dis. 2013, 201, 490–503. [Google Scholar] [CrossRef] [Green Version]
- Pettigrew, T.F.; Tropp, L.R. A meta-analytic test of intergroup contact theory. J. Personal. Soc. Psychol. 2006, 90, 751. [Google Scholar] [CrossRef] [Green Version]
- Clement, S.; van Nieuwenhuizen, A.; Kassam, A.; Flach, C.; Lazarus, A.; de Castro, M.; McCrone, P.; Norman, I.; Thornicroft, G. Filmed v. Live social contact interventions to reduce stigma: Randomised controlled trial. Br. J. Psychiatry 2012, 201, 57–64. [Google Scholar] [CrossRef] [Green Version]
- Reinke, R.R.; Corrigan, P.W.; Leonhard, C.; Lundin, R.K.; Kubiak, M.A. Examining two aspects of contact on the stigma of mental illness. J. Soc. Clin. Psychol. 2004, 23, 377–389. [Google Scholar] [CrossRef]
- Papish, A.; Kassam, A.; Modgill, G.; Vaz, G.; Zanussi, L.; Patten, S. Reducing the stigma of mental illness in undergraduate medical education: A randomized controlled trial. BMC Med. Educ. 2013, 13, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Kassam, A.; Glozier, N.; Leese, M.; Loughran, J.; Thornicroft, G. A controlled trial of mental illness related stigma training for medical students. BMC Med. Educ. 2011, 11, 51. [Google Scholar] [CrossRef] [Green Version]
- Heim, E.; Henderson, C.; Kohrt, B.A.; Koschorke, M.; Milenova, M.; Thornicroft, G. Reducing mental health-related stigma among medical and nursing students in low- and middle-income countries: A systematic review. Epidemiol. Psychiatr. Sci. 2020, 29, e28. [Google Scholar] [CrossRef] [PubMed]
- Iheanacho, T.; Marienfeld, C.; Stefanovics, E.; Rosenheck, R.A. Attitudes toward mental illness and changes associated with a brief educational intervention for medical and nursing students in nigeria. Acad. Psychiatry 2014, 38, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Altindag, A.; Yanik, M.; Ucok, A.; Alptekin, K.; Ozkan, M. Effects of an antistigma program on medical students’ attitudes towards people with schizophrenia. Psychiatry Clin. Neurosci. 2006, 60, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, A.; Tan, K.-A.; Knaak, S.; Chew, B.H.; Ghazali, S.S. Effects of brief psychoeducational program on stigma in malaysian pre-clinical medical students: A randomized controlled trial. Acad. Psychiatry 2016, 40, 905–911. [Google Scholar] [CrossRef]
- Jordans, M.J.D.; Luitel, N.P.; Kohrt, B.A.; Rathod, S.D.; Garman, E.C.; de Silva, M.; Komproe, I.H.; Patel, V.; Lund, C. Community-, facility-, and individual-level outcomes of a district mental healthcare plan in a low-resource setting in Nepal: A population-based evaluation. PLoS Med. 2019, 16, e1002748. [Google Scholar] [CrossRef] [Green Version]
- Gartoulla, P.; Pantha, S.; Pandey, R. Knowledge status on mental health among health professionals of chitwan district, Nepal. J. Inst. Med. 2015, 37, 91–97. [Google Scholar]
- Luitel, N.P.; Jordans, M.J.D.; Kohrt, B.A.; Rathod, S.D.; Komproe, I.H. Treatment gap and barriers for mental health care: A cross-sectional community survey in Nepal. PLoS ONE 2017, 12, e0183223. [Google Scholar] [CrossRef]
- Luitel, N.; Jordans, M.; Adhikari, A.; Upadhaya, N.; Hanlon, C.; Lund, C.; Komproe, I. Mental health care in Nepal: Current situation and challenges for development of a district mental health care plan. Confl. Health 2015, 9, 3. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Mhgap Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings: Mental Health Gap Action Programme (MHGAP)—Version 2.0; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Acharya, B.; Tenpa, J.; Basnet, M.; Hirachan, S.; Rimal, P.; Choudhury, N.; Thapa, P.; Citrin, D.; Halliday, S.; Swar, S. Developing a scalable training model in global mental health: Pilot study of a video-assisted training program for generalist clinicians in rural Nepal. Glob. Ment Health 2017, 4, 41. [Google Scholar] [CrossRef] [Green Version]
- Rai, S.; Gurung, D.; Kaiser, B.N.; Sikkema, K.J.; Dhakal, M.; Bhardwaj, A.; Tergesen, C.; Kohrt, B.A. A service user co-facilitated intervention to reduce mental illness stigma among primary healthcare workers: Utilizing perspectives of family members and caregivers. Fam. Syst. Health 2018, 36, 198–209. [Google Scholar] [CrossRef]
- Kohrt, B.A.; Jordans, M.J.D.; Turner, E.L.; Sikkema, K.J.; Luitel, N.P.; Rai, S.; Singla, D.R.; Lamichhane, J.; Lund, C.; Patel, V. REducing Stigma among Healthcare ProvidErs to improve mental health services (RESHAPE): Protocol for a pilot cluster randomized controlled trial of a stigma reduction intervention for training primary healthcare workers in Nepal. Pilot Feasibility Stud. 2018, 4, 36. [Google Scholar] [CrossRef] [PubMed]
- Kohrt, B.A.; Turner, E.L.; Rai, S.; Bhardwaj, A.; Sikkema, K.J.; Adelekun, A.; Dhakal, M.; Luitel, N.P.; Lund, C.; Patel, V.; et al. Reducing mental illness stigma in healthcare settings: Proof of concept for a social contact intervention to address what matters most for primary care providers. Soc. Sci. Med. 2020, 250, 112852. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, B.N.; Varma, S.; Carpenter-Song, E.; Sareff, R.; Rai, S.; Kohrt, B.A. Eliciting recovery narratives in global mental health: Benefits and potential harms in service user participation. Psychiatr. Rehabil. J. 2020, 43, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Lund, C.; Tomlinson, M.; De Silva, M.; Fekadu, A.; Shidhaye, R.; Jordans, M.; Petersen, I.; Bhana, A.; Kigozi, F.; Prince, M.; et al. Prime: A programme to reduce the treatment gap for mental disorders in five low- and middle-income countries. PLoS Med. 2012, 9, e1001359. [Google Scholar] [CrossRef] [PubMed]
- Jordans, M.J.D.; Luitel, N.P.; Pokhrel, P.; Patel, V. Development and pilot testing of a mental healthcare plan in Nepal. Br. J. Psychiatry 2015, 208, S21–S28. [Google Scholar] [CrossRef] [Green Version]
- Acharya, B.; Basnet, M.; Rimal, P.; Citrin, D.; Hirachan, S.; Swar, S.; Thapa, P.; Pandit, J.; Pokharel, R.; Kohrt, B. Translating mental health diagnostic and symptom terminology to train health workers and engage patients in cross-cultural, non-english speaking populations. Int. J. Ment. Health Syst. 2017, 11, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohrt, B.A.; Hruschka, D.J. Nepali concepts of psychological trauma: The role of idioms of distress, ethnopsychology and ethnophysiology in alleviating suffering and preventing stigma. Cult. Med. Psychiatry 2010, 34, 322–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohrt, B.A.; Harper, I. Navigating diagnoses: Understanding mind-body relations, mental health, and stigma in Nepal. Cult. Med. Psychiatry 2008, 32, 462–491. [Google Scholar] [CrossRef] [Green Version]
- Pescosolido, B.A.; Long, J.S.; Martin, J.K.; Smith, T. Stigma & Mental Illness in Cross-National Perspective: The Sgc-Mhs Interview Schedule Final Revision (Summer 2004); Indiana University: Bloomington, IN, USA, 2004. [Google Scholar]
- Pescosolido, B.A.; Medina, T.R.; Martin, J.K.; Long, J.S. The “backbone” of stigma: Identifying the global core of public prejudice associated with mental illness. Am. J. Public Health 2013, 103, 853–860. [Google Scholar] [CrossRef]
- Bogardus, E.S. Measuring social distance. J. Appl. Sociol. 1925, 9, 299–308. [Google Scholar]
- Van Brakel, W.H.; Cataldo, J.; Grover, S.; Kohrt, B.A.; Nyblade, L.; Stockton, M.; Wouters, E.; Yang, L.H. Out of the silos: Identifying cross-cutting features of health-related stigma to advance measurement and intervention. BMC Med. 2019, 17, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenwald, A.G.; McGhee, D.E.; Schwartz, J.L. Measuring individual differences in implicit cognition: The implicit association test. J. Personal. Soc. Psychol. 1998, 74, 1464. [Google Scholar] [CrossRef]
- Peris, T.S.; Teachman, B.A.; Nosek, B.A. Implicit and explicit stigma of mental illness: Links to clinical care. J. Nerv. Ment. Dis. 2008, 196, 752–760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenwald, A.G.; Nosek, B.A.; Banaji, M.R. Understanding and using the implicit association test: I. An improved scoring algorithm. J. Personal. Soc. Psychol. 2003, 85, 197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jordans, M.J.; Kohrt, B.A.; Luitel, N.P.; Komproe, I.H.; Lund, C. Accuracy of proactive case finding for mental disorders by community informants in Nepal. Br. J. Psychiatry 2015, 207, 501–506. [Google Scholar] [CrossRef]
- Subba, P.; Luitel, N.P.; Kohrt, B.A.; Jordans, M.J.D. Improving detection of mental health problems in community settings in Nepal: Development and pilot testing of the community informant detection tool. Confl. Health 2017, 11, 28. [Google Scholar] [CrossRef]
- StataCorp, L.L.C. Stata Statistical Software: Release 15; StataCorp LP: College Station, TX, USA, 2017. [Google Scholar]
- QSR International. Nvivo Qualitative Data Analysis Software. Version 10; QSR International Pty Ltd.: Doncaster, Australia, 2012. [Google Scholar]
- Jorm, A.F.; Reavley, N.J.; Ross, A.M. Belief in the dangerousness of people with mental disorders: A review. Aust. N. Z. J. Psychiatry 2012, 46, 1029–1045. [Google Scholar] [CrossRef]
- Krendl, A.C.; Freeman, J.B. Are mental illnesses stigmatized for the same reasons? Identifying the stigma-related beliefs underlying common mental illnesses. J. Ment. Health 2019, 28, 267–275. [Google Scholar] [CrossRef]
- Kermode, M.; Bowen, K.; Arole, S.; Pathare, S.; Jorm, A.F. Attitudes to people with mental disorders: A mental health literacy survey in a rural area of maharashtra, India. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 1087–1096. [Google Scholar] [CrossRef]
- Chiles, C.; Stefanovics, E.; Rosenheck, R. Attitudes of students at a us medical school toward mental illness and its causes. Acad. Psychiatry 2017, 41, 320–325. [Google Scholar] [CrossRef]
- Roth, D.; Antony, M.M.; Kerr, K.L.; Downie, F. Attitudes toward mental illness in medical students: Does personal and professional experience with mental illness make a difference? Med. Educ. 2000, 34, 234–236. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Zhang, H.; Yang, G.; Hu, X.; Liu, Z.; Guo, N.; He, H.; Sun, B.; Rosenheck, R. Attitudes towards mental illness among medical students in China: Impact of medical education on stigma. Asia Pac. Psychiatry 2018, 10, e12294. [Google Scholar] [CrossRef]
- Ay, P.; Save, D.; Fidanoglu, O. Does stigma concerning mental disorders differ through medical education? A survey among medical students in istanbul. Soc. Psychiatry Psychiatr. Epidemiol. 2006, 41, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.S.; Johns, R.; Chen, T.F. Pharmacy students’ and graduates’ attitudes towards people with schizophrenia and severe depression. Am. J. Pharm. Educ. 2006, 70, 77. [Google Scholar] [CrossRef] [Green Version]
- Wilkinson, D. The effects of brief psychiatric training on the attitudes of general nursing students to psychiatric patients. J. Adv. Nurs. 1982, 7, 239–253. [Google Scholar] [CrossRef]
- De Vargas, D. The impact of clinical experience with alcoholics on brazilian nursing students’ attitudes toward alcoholism and associated problems. J. Addict. Nurs. 2013, 24, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Esen Danaci, A.; Balikci, K.; Aydin, O.; Cengisiz, C.; Uykur, A.B. The effect of medical education on attitudes towards schizophrenia: A five-year follow-up study. Turk Psikiyatr. Derg. 2016, 27, 176–184. [Google Scholar] [CrossRef] [Green Version]
- Shankar, P.R. Undergraduate medical education in Nepal: One size fits all? J. Educ. Eval. Health Prof. 2011, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Semrau, M.; van Ommeren, M.; Blagescu, M.; Griekspoor, A.; Howard, L.M.; Jordans, M.; Lempp, H.; Marini, A.; Pedersen, J.; Pilotte, I.; et al. The development and psychometric properties of the humanitarian emergency settings perceived needs (hesper) scale. Am. J. Public Health 2012, 102, e55–e63. [Google Scholar] [CrossRef] [PubMed]



| Time 1 (m:ss) | Depression Videos 2 | Psychosis Videos 3 | ||
|---|---|---|---|---|
| Didactic Lecture Video | Service User Testimonial Video | Didactic Lecture Video | Service User Testimonial Video | |
| 0:00–0:59 | Introduction to psychiatrist and mhGAP-IG module for depression | Introduction and family history of the service user living with depression | Introduction to psychiatrist and mhGAP-IG module for psychosis; acute versus chronic psychosis | Introduction to service user living with psychosis; description of symptom onset during pregnancy |
| 1:00–1:59 | Severity and signs of depression; symptoms of depression with examples | Father falling ill precipitating symptoms of depression, which are described in detail affecting daily activities | Continued acute versus chronic psychosis; symptoms of psychosis | Service user’s sister-in-law describes episodes of psychosis; service user describes suicide attempt |
| 2:00–2:59 | Continuation of symptoms; instructions for how to assess and diagnose depression | Service user takes mother to the health clinic, finds a handout with symptoms of depression, and continues to list symptoms of depression | Instructions for how to diagnose psychosis; description of three types of psychosis | Service user seeks medical treatment; reports that visiting a traditional healer did not help her symptoms |
| 3:00–3:59 | Overview of treatments: psychosocial counseling, psychoeducation, and medicine | Health worker speaks about the service user’s diagnosis of depression, comforts her, and referring the service user for counseling | Continued types of psychosis; responding to imminent suicide risk | Counselor describes symptoms of psychosis to make a diagnosis |
| 4:00–4:59 | Detailed explanation of psychosocial counseling and psychoeducation components | Counselor describes psychosocial counseling and psychoeducation skills she used with the service user | Three interventions: family involvement, psychoeducation, and counseling | Counselor describes therapy techniques; service user describes therapeutic activities she practices |
| 5:00–5:59 | Continued explanation of psychosocial counseling and psychoeducation | Service user recalls all of the tools she learned through counseling and psychoeducation | List of medications to treat psychosis; follow-up instructions | Counselor describes three types of psychosis and three types of interventions: family involvement, psychoeducation, and counseling |
| 6:00–6:59 | List of which medications to prescribe and how to prescribe them; follow-up procedures | Service user recovers without medication; she describes what medications are commonly prescribed for depression | Instructions for how to monitor patients with psychosis | List of medications to prescribe; service user describes recovery after she started medication; counselor describes follow-up procedure |
| 7:00–7:45 | Recovery description of how people living with depression can recover and return to normal activities; closing credits | Service user participates in mental health training to educate health workers about depression and sings her own song about mental illness; closing credits | Recovery description of how people living with psychosis can return to normal activities; closing credits | Service user resumes her regular activities at home, such as cooking, cleaning, and gardening; closing credits |
| Variables | Control: No Video (n = 31) | Didactic Video (n = 31) | Service User Video (n = 32) |
|---|---|---|---|
| Age | |||
| Mean (SD) | 21.03 (1.14) | 21.19 (1.11) | 21.00 (1.08) |
| Gender | |||
| Male | 23 (24%) | 25 (27%) | 23 (24%) |
| Female | 8 (8%) | 6 (6%) | 9 (10%) |
| Class Level | |||
| Second Year | 14 (15%) | 15 (16%) | 16 (17%) |
| Third Year | 17 (18%) | 16 (17%) | 16 (17%) |
| Personal experience or has family member/friend with mental illness | |||
| Yes | 18 (19%) | 13 (14%) | 13 (14%) |
| No | 9 (10%) | 14 (15%) | 16 (17%) |
| Don’t Know | 4 (4%) | 4 (4%) | 3 (3%) |
| Previous knowledge about mental illness from schooling | |||
| Yes | 10 (11%) | 10 (11%) | 6 (6%) |
| No | 21 (22%) | 21 (22%) | 26 (28%) |
| Previous knowledge about mental illness outside of schooling | |||
| Yes | 18 (19%) | 21 (22%) | 22 (23%) |
| No | 13 (14%) | 10 (11%) | 10 (11%) |
| Frequent Computer Users | |||
| Yes | 29 (33%) | 28 (32%) | 30 (34%) |
| No | 2 (2%) | 3 (3%) | 2 (2%) |
| Medical specialty interest in psychiatry | 2 (2%) | 1 (1%) | 0 (0%) |
| Outcomes | M (SD) | β coef. | 95% CI | p-Value |
|---|---|---|---|---|
| Explicit Attitude (SDS) | ||||
| Control: no video | 39.10 (11.14) | |||
| Didactic | 33.32 (9.57) | −5.90 | −10.95–−0.86 | 0.02 * |
| Service User | 30.13 (9.16) | −8.85 | −13.85–−3.84 | 0.001 * |
| Implicit Attitude (IAT) † | ||||
| Harmfulness Attribute | ||||
| Control | 0.15 (0.32) | |||
| Didactic | 0.07 (0.33) | −0.02 | −0.11–0.06 | 0.59 |
| Service User | 0.04 (0.36) | −0.13 | −0.30–0.04 | 0.13 |
| Burdensomeness Attribute | ||||
| Control | 0.20 (0.31) | |||
| Didactic | 0.10 (0.34) | −0.05 | −0.13–0.03 | 0.25 |
| Service User | 0.17 (0.29) | −0.03 | −0.19–0.13 | 0.70 |
| Diagnosis Accuracy | ||||
| Control | 0.77 (0.43) | |||
| Didactic | 0.84 (0.37) | 0.21 | −0.43–0.85 | 0.52 |
| Service User | 0.91 (0.30) | 1.04 | −0.42–2.49 | 0.16 |
| Variables | Control: No Video (n = 74) | Didactic Video (n = 70) | Service User (n = 69) |
|---|---|---|---|
| Age | |||
| M (SD) | 19.62 (0.95) | 19.89 (1.21) | 19.81 (1.19) |
| Institution | |||
| TU-IOM | 32 (15%) | 34 (16%) | 36 (17%) |
| KUSMS | 42 (20%) | 35 (16%) | 34 (16%) |
| Gender | |||
| Male | 57 (27%) | 55 (26%) | 53 (25%) |
| Female | 17 (8%) | 15 (7) | 16 (8%) |
| Class Level | |||
| First Year | 40 (19%) | 35 (16%) | 36 (17%) |
| Second Year | 34 (16%) | 35 (16%) | 33 (15%) |
| Personal experience or has family member/friend with mental illness | |||
| Yes | 46 (22%) | 41 (19%) | 38 (18%) |
| No | 22(10%) | 11 (5%) | 20 (9%) |
| Don’t Know | 6 (3%) | 18 (8%) | 11 (5%) |
| Previous knowledge about mental illness from schooling | |||
| Yes | 58 (27%) | 56 (26%) | 49 (23%) |
| No | 16 (8%) | 14 (7%) | 20 (9%) |
| Previous knowledge about mental illness outside of schooling | |||
| Yes | 62 (29%) | 56 (26%) | 48 (23%) |
| No | 12 (6%) | 14 (7%) | 21 (10%) |
| Frequent Computer Users | |||
| Yes | 65 (31%) | 60 (28%) | 60 (28%) |
| No | 9 (4%) | 10 (5%) | 9 (4%) |
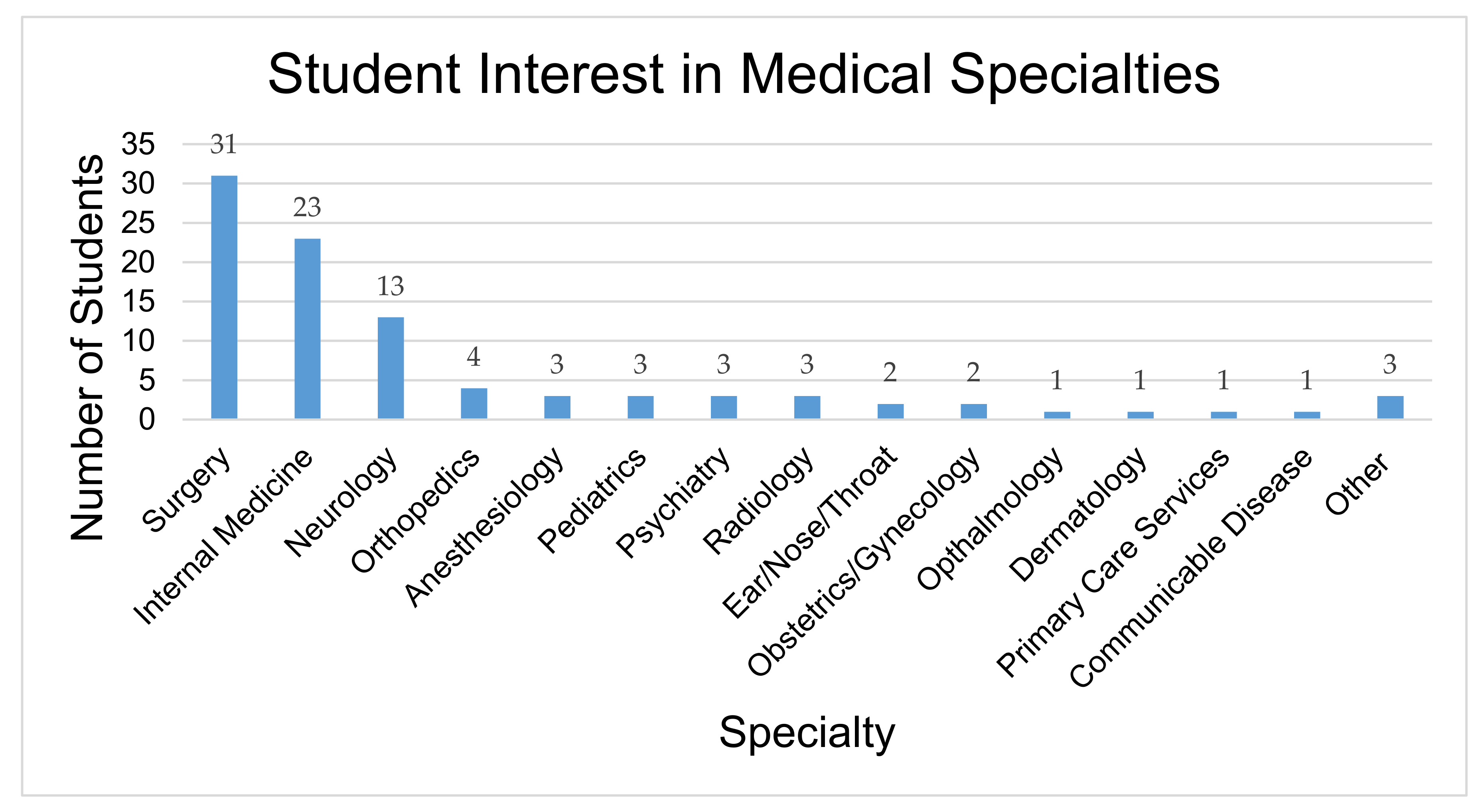
| Medical specialty interest in | |||
| Psychiatry | 3 (1%) | 2 (1%) | 3 (1%) |
| Outcomes | M (SD) | β coef. (95%CI) | p-Value |
|---|---|---|---|
| Explicit Attitude (SDS) | |||
| Control | 41.47 (9.49) | ||
| Didactic | 41.01 (9.43) | −0.45 (−3.74–2.83) | 0.79 |
| Service User | 44.39 (10.97) | 2.74 (−0.55–6.02) | 0.10 |
| Unsafe around people who have mental illness | |||
| Depression Vignette | |||
| Control | 3.59 (1.07) | ||
| Didactic | 3.57 (1.06) | 0.01 (−0.35–0.36) | 0.97 |
| Service User | 3.13 (1.10) | −0.43 (−0.78–(−0.07)) | 0.02 * |
| Psychosis Vignette | |||
| Control | 2.81 (1.02) | ||
| Didactic | 2.74 (1.10) | −0.09 (−0.43–0.26) | 0.61 |
| Service User | 2.52 (1.02) | −0.23 (−0.58–(−0.11)) | 0.18 |
| Potentially violent towards others | |||
| Depression Vignette | |||
| Control | 3.32 (1.06) | ||
| Didactic | 3.21 (1.05) | −0.07 (−0.42–0.27) | 0.67 |
| Service User | 2.81 (1.06) | −0.50 (−0.84–(−0.15)) | 0.005 * |
| Psychosis Vignette | |||
| Control | 2.51 (0.85) | ||
| Didactic | 2.44 (0.91) | −0.10 (−0.39–0.19) | 0.49 |
| Service User | 2.13 (0.84) | −0.33 (−0.62–(−0.05)) | 0.02 △ |
| Implicit Attitude (IAT) ⟐ | |||
| Harmfulness Attribute | |||
| Control | 0.01 (0.31) | ||
| Didactic | −0.004 (0.30) | −0.04 (−0.15–0.08) | 0.54 |
| Service User | 0.02 (0.33) | −0.01 (−0.10–0.13) | 0.81 |
| Burdensomeness Attribute | |||
| Control | 0.06 (0.29) | ||
| Didactic | 0.09 (0.34) | 0.03 (−0.09–0.15) | 0.61 |
| Service User | 0.11 (0.35) | 0.05 (−0.06–0.17) | 0.36 |
| Diagnostic Accuracy of Depression and Psychosis | |||
| Control | 0.36 (0.48) | ||
| Didactic | 0.60 (0.49) | 1.02 (0.34–1.69) | 0.003 * |
| Service User | 0.45 (0.50) | 0.37 (−0.30–1.04) | 0.28 |
| Treatment Accuracy | |||
| Depression Vignette | |||
| Control | 2.03 (1.18) | ||
| Didactic | 2.67 (1.21) | 0.68 (0.29–1.07) | 0.001 * |
| Service User | 2.54 (1.16) | 0.48 (0.09–0.87) | 0.02 * |
| Psychosis Vignette | |||
| Control | 2.26 (1.14) | ||
| Didactic | 2.87 (1.09) | 0.63 (0.25–1.01) | 0.001 * |
| Service User | 2.72 (1.24) | 0.51 (0.14–0.89) | 0.008 * |
| Outcomes | Social Distance Scale (SDS) | Implicit Attitude Test—Harmfulness | Implicit Attitude Test—Burdensomeness |
|---|---|---|---|
| Implicit Attitude (IAT) △: Harmfulness Attribute | r = −0.01 p = 0.86 | ||
| Implicit Attitude (IAT) △: Burdensomeness Attribute | r = 0.09 p = 0.21 | r = 0.27 † p < 0.001 ** | |
| Explicit Attitude (Uncomfortable in public near someone with depression) | r = −0.23 p < 0.001 ** | r < 0.01 p = 0.96 | r = −0.09 p = 0.20 |
| Explicit Attitude (Uncomfortable in public near someone with psychosis) | r = −0.30 p < 0.001 ** | r = −0.03 p = 0.66 | r = −0.19 p = 0.007 * |
| Explicit Attitude (People with depression are violent) | r = −0.10 p = 0.13 | r = −0.08 p = 0.25 | r = −0.05 p = 0.49 |
| Explicit Attitude (People with psychosis are violent) | r = −0.18 p = 0.008 * | r = −0.11 p = 0.13 | r = −0.12 p = 0.11 |
| Knowledge (Accurately diagnosed depression and psychosis) | r = −0.08 p = 0.23 | r = 0.13 p = 0.09 | r = 0.08 p = 0.30 |
| Knowledge (Treatment accuracy for depression) | r = 0.03 p = 0.68 | r = −0.11 p = 0.12 | r = 0.07 p = 0.32 |
| Knowledge (Treatment accuracy for psychosis) | r = −0.06 p = 0.42 | r = −0.04 p = 0.56 | r = 0.01 p = 0.84 |
| Explicit Attitude (SDS) | M (SD) | β Coef. (95%CI) | p-Value |
|---|---|---|---|
| Control | 40.81 (9.11) | -- | -- |
| Didactic | 41.69 (10.19) | 0.19 (−3.38–3.77) | 0.91 |
| Service User | 45.53 (10.68) | 4.44 (1.01–7.87) | 0.01 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tergesen, C.L.; Gurung, D.; Dhungana, S.; Risal, A.; Basel, P.; Tamrakar, D.; Amatya, A.; Park, L.P.; Kohrt, B.A. Impact of Service User Video Presentations on Explicit and Implicit Stigma toward Mental Illness among Medical Students in Nepal: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 2143. https://doi.org/10.3390/ijerph18042143
Tergesen CL, Gurung D, Dhungana S, Risal A, Basel P, Tamrakar D, Amatya A, Park LP, Kohrt BA. Impact of Service User Video Presentations on Explicit and Implicit Stigma toward Mental Illness among Medical Students in Nepal: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(4):2143. https://doi.org/10.3390/ijerph18042143
Chicago/Turabian StyleTergesen, Cori L., Dristy Gurung, Saraswati Dhungana, Ajay Risal, Prem Basel, Dipesh Tamrakar, Archana Amatya, Lawrence P. Park, and Brandon A. Kohrt. 2021. "Impact of Service User Video Presentations on Explicit and Implicit Stigma toward Mental Illness among Medical Students in Nepal: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 4: 2143. https://doi.org/10.3390/ijerph18042143
APA StyleTergesen, C. L., Gurung, D., Dhungana, S., Risal, A., Basel, P., Tamrakar, D., Amatya, A., Park, L. P., & Kohrt, B. A. (2021). Impact of Service User Video Presentations on Explicit and Implicit Stigma toward Mental Illness among Medical Students in Nepal: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(4), 2143. https://doi.org/10.3390/ijerph18042143







