The Impact of Health Policies and Sociodemographic Factors on Doubling Time of the COVID-19 Pandemic in Mexico
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Variables
2.2.1. Outcome Variable: Doubling Time
2.2.2. Independent Variables
2.3. Descriptive Analysis
2.4. Panel Data Model
3. Results
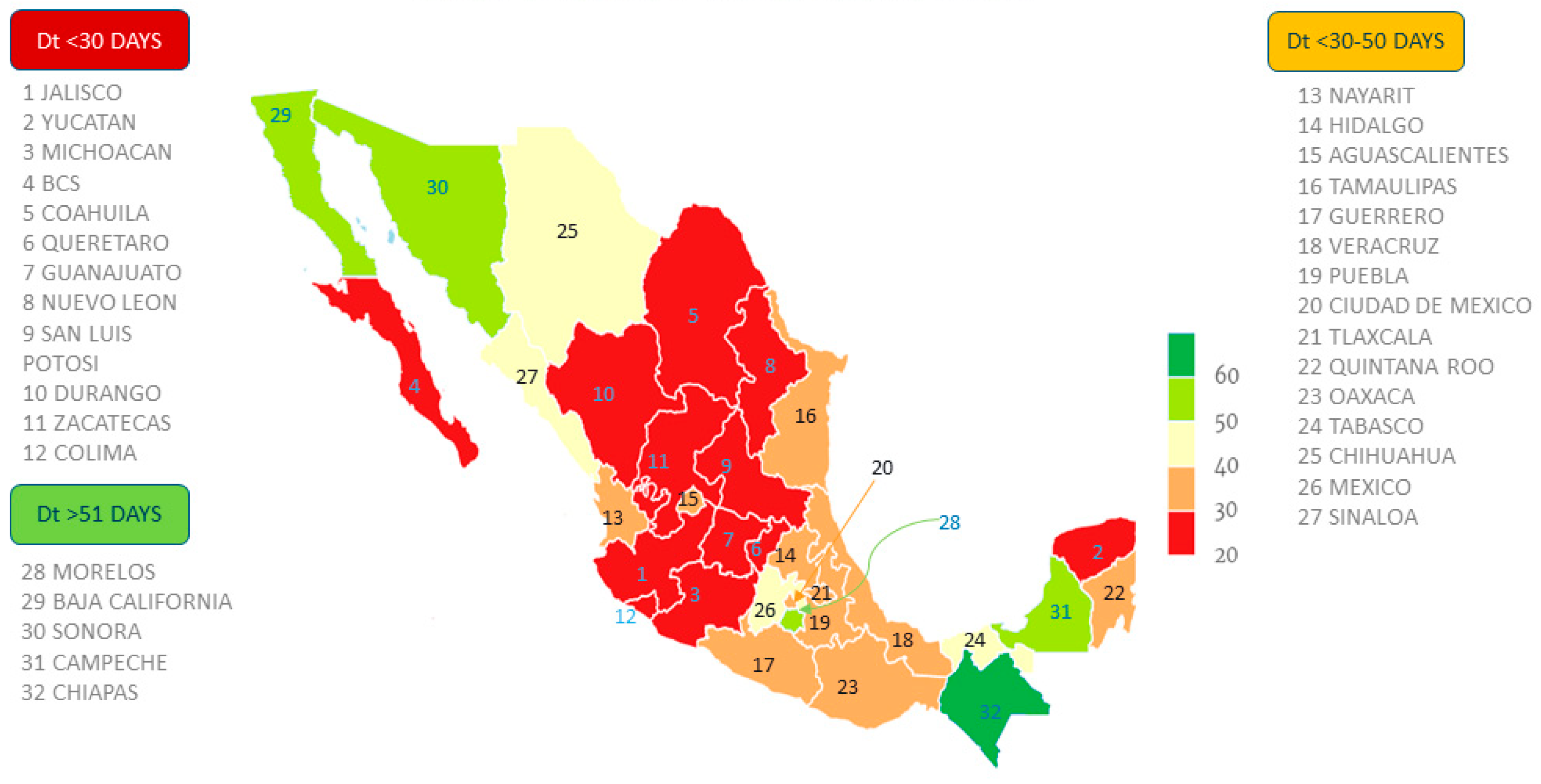
3.1. Descriptive Results
3.2. Categories of Policies Implemented in Response to COVID-19 in Mexico
3.3. Relationship between Policy Index, New Cases and Doubling Time by Epidemiological Week for Each Mexican State
3.4. Panel Data Model
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. COVID 19 Public Health Emergency of International Concern (PHEIC) Global Research and Innovation Forum. Available online: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum (accessed on 30 November 2020).
- Secretaría de Salud. Comunicado Técnico Diario Nuevo Coronavirus en el Mundo (COVID-19) [New Coronavirus in the World (COVID-19) Daily Technical Report]. Available online: https://www.gob.mx/salud/documentos/coronavirus-covid19-comunicados-tecnicos-diarios-diciembre-2020 (accessed on 2 December 2020).
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 2 December 2020).
- World Health Organization. Sanitary Regulation International, 3rd ed.; World Health Organization: Geneva, Switzerland, 2016; pp. 1–84. [Google Scholar]
- Franco, C.J. Diseño de Políticas Públicas, 3rd ed.; IEXE Editorial: Distrito Federal, Mexico, 2016; pp. 1–278. [Google Scholar]
- Cámara de Diputados. Ley General de Salud [General Law of Health]. Available online: http://www.diputados.gob.mx/LeyesBiblio/pdf_mov/Ley_General_de_Salud.pdf (accessed on 4 December 2020).
- Jay, J.; Bor, J.; Nsoesie, E.O.; Lipson, S.K.; Jones, D.K.; Galea, S.; Raifman, J. Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat. Hum. Behav. 2020, 4, 1294–1302. [Google Scholar] [CrossRef]
- Poppe, A. Impact of the Healthcare System, Macro Indicator, General Mandatory Quarantine, and Mask Obligation on COVID-19 Cases and Death in Six Latin American Countries: An Interrupted Time Series Study. Front. Public Health 2020, 8, 607832. [Google Scholar] [CrossRef] [PubMed]
- Golechha, M. COVID-19 Containment in Asia’s Largest Urban Slum Dharavi-Mumbai, India: Lessons for Policymakers Globally. J. Urban Health 2020, 97, 796–801. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.B.; Patel, P. Doubling Time and Its Interpretation for COVID 19 Cases. Nat. J. Community Med. 2020, 11, 141–143. [Google Scholar]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N. Engl. J. Med. 2020, 26, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Muniz-Rodriguez, K.; Chowell, G.; Cheung, C.H.; Jia, D.; Lai, P.Y.; Lee, Y.; Liu, M.; Ofori, S.K.; Roosa, K.M.; Simonsen, L.; et al. Doubling Time of the COVID-19 Epidemic by Chinese Province. Emerg. Infect. Dis. 2020, 26, 1912–1914. [Google Scholar] [CrossRef] [PubMed]
- Jamison, D.T.; Lau, L.J.; Wu, K.B.; Xiong, Y. Country performance against COVID-19: Rankings for 35 countries. BMJ Glob. Health 2020, 5, e003047. [Google Scholar] [CrossRef] [PubMed]
- Hale, T.; Angrist, N.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S. “Variation in Government Responses to COVID-19” Version 5.0. Blavatnik School of Government Working Paper. 2020. Available online: www.bsg.ox.ac.uk/covidtracker (accessed on 18 September 2020).
- Consejo Nacional de Población (CONAPO). Proyecciones de la Población de México y de las Entidades Federativas, 2016–2050 [Projections of the Population of Mexico and the Federal Entities, 2016–2050]. Available online: https://datos.gob.mx/busca/dataset/proyecciones-de-la-poblacion-de-mexico-y-de-las-entidades-federativas-2016-2050 (accessed on 2 September 2020).
- United Nations Development Programme. Human Development Reports 2019. Available online: http://www.hdr.undp.org/en/2019-report (accessed on 18 September 2020).
- Instituto Nacional de Estadística y Geografía (INEGI). Total Quarterly Average Current Income per Household, by State According to Household Deciles, 2016 and 2018. Available online: https://www.inegi.org.mx/app/tabulados/interactivos/default?px=Hogares_10&bd=Hogares (accessed on 2 September 2020).
- Google Maps. Available online: https://www.google.com/covid19/mobility/data_documentation.html?hl=en (accessed on 2 October 2020).
- Wooldridge, J. Econometric Analysis of Cross Section and Panel Data, 1st ed.; The MIT Press: Cambridge, MA, USA, 2002; pp. 247–291. [Google Scholar]
- Constitución Federal de los Estados Unidos Mexicanos. Available online: http://www.ordenjuridico.gob.mx/Constitucion/1824B.pdf (accessed on 10 December 2020).
- Lim, J.M.; Tun, Z.M.; Kumar, V.; Quaye, S.; Offeddu, V.; Cook, A.R.; Lwin, M.O.; Jiang, S.; Tam, C.C. Population anxiety and positive behavior change during the COVID-19 epidemic: Cross-sectional surveys in Singapore, China and Italy. Influ. Other Respir. Viruses 2020, 15, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Bianconi, A.; Marcelli, A.; Campi, G.; Perali, A. Efficiency of COVID-19 mobile contact tracing containment by measuring time-dependent doubling time. Phys. Biol. 2020, 17, 065006. [Google Scholar] [CrossRef]
- Lurie, M.N.; Silva, J.; Yorlets, R.R.; Tao, J.; Chan, P.A. COVID-19 epidemic doubling time in the United States before and during stay-at-home restrictions. J. Infect. Dis. 2020, 222, 1601–1606. [Google Scholar] [CrossRef] [PubMed]
- Vicentini, C.; Bordino, V.; Gardois, P.; Zottien, C.M. Early assessment of the impact of mitigation measures on the COVID-19 outbreak in Italy. Public Health 2020, 185, 99–101. [Google Scholar] [CrossRef]
- Kim, H. The sociopolitical context of the COVID-19 response in South Korea. BMJ Glob. Health 2020, 5, e002714. [Google Scholar] [CrossRef] [PubMed]
- Aquino, E.M.L.; Silveira, I.H.; Pescarini, J.M.; Aquino, R.; Souza-Filho, J.A.; Rocha, A.S.; Ferreira, A.; Victor, A.; Teixeira, C.; Machado, D.B.; et al. Social distancing measures to control the COVID-19 pandemic: Potential impacts and challenges in Brazil. Cienc. Saude Coletiva 2020, 25, 2423–2446. [Google Scholar] [CrossRef] [PubMed]
- Bell, D.; Hansen, K.S.; Kiragga, A.N.; Kambugu, A.; Kissa, J.; Mbonye, A.K. Predicting the Impact of COVID-19 and the Potential Impact of the Public Health Response on Disease Burden in Uganda. Am. J. Trop. Med. Hyg. 2020, 103, 1191–1197. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, S.H.; Bulger, E.L.; Duber, H.C.; Greninger, A.L.; Ong, T.D.; Morris, S.C.; Chew, L.D.; Haffner, T.M.; Sakata, V.L.; Lynch, J.B.; et al. Western Washington State COVID-19 Experience: Keys to Flattening the Curve and Effective Health System Response. J. Am. Coll. Surg. 2020, 231, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Kavaliunas, A.; Ocaya, P.; Mumper, J.; Lindfeldt, I.; Kyhlstedt, M. Swedish policy analysis for Covid-19. Health Policy Technol. 2020, 9, 598–612. [Google Scholar] [CrossRef] [PubMed]
- Benjamin Georges, C. Ensuring health equity during the COVID-19 pandemic: The role of public health infrastructure. Rev. Panam Salud Publica 2020, 44, e70. [Google Scholar] [CrossRef] [PubMed]
- Paul, E.; Brown, G.W.; Ridde, V. COVID-19: Time for paradigm shift in the nexus between local, national and global health. BMJ Glob. Health 2020, 5, e002622. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.A.K.S.; Ajisola, M.; Azeem, K.; Bakibinga, P.; Chen, Y.; Choudhury, N.N.; Fayehun, O.; Griffiths, F.; Harris, B.; Kibe, P.; et al. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: Results of preCOVID and COVID-19 lockdown stakeholder engagements. BMJ Glob. Health 2020, 5, e003042. [Google Scholar] [CrossRef] [PubMed]



| Policy Categories | Policy Value a | Total Policies b |
|---|---|---|
| Closures and containment (C) | ||
| School closing (C1) | 7.56 | 5 |
| Workplace closing (C2) | 5.89 | 664 |
| Cancel public events (C3) | 8.89 | 34 |
| Restrictions on gatherings (C4) | 8.44 | 36 |
| Close public transport (C5) | 4.67 | 1 |
| Stay-at-home requirements (C6) | 7.33 | 1 |
| Restrictions on internal movement (C7) | 7.11 | 96 |
| Restrictions on international movement (C8) | 8.78 | 5 |
| Economic measures (E) | ||
| Income support (E1) | 5.33 | 140 |
| Debt/contract relief for households (E2) | 5.22 | 12 |
| Fiscal measures (E3) | 4.43 | 117 |
| Health measures (H) | ||
| Public information campaigns (H1) | 9.56 | 223 |
| Testing policy (H2) | 8.44 | 10 |
| Contact tracing (H3) | 9.0 | 9 |
| Emergency investment in healthcare (H4) | 9.78 | 61 |
| Mexican State | Population Size | Population Density | Health Index | Income per Capita | Doubling Time Average | New Cases per 100 k Population | Total Cases per 100 k Population |
|---|---|---|---|---|---|---|---|
| Aguascalientes | 1,312,544 | 234 | 0.856 | 2737 | 34 | 19 | 486 |
| Baja California | 3,315,766 | 46 | 0.858 | 2730 | 55 | 22 | 552 |
| Baja California Sur | 712,029 | 10 | 0.857 | 3172 | 28 | 49 | 1220 |
| Campeche | 899,931 | 16 | 0.839 | 2200 | 56 | 26 | 644 |
| Chiapas | 5,217,908 | 71 | 0.83 | 1223 | 118 | 5 | 122 |
| Chihuahua | 3,556,574 | 14 | 0.849 | 2492 | 46 | 10 | 259 |
| Mexico City | 8,918,653 | 5966 | 0.865 | 3648 | 41 | 50 | 1256 |
| Coahuila | 2,954,915 | 19 | 0.853 | 2580 | 29 | 32 | 811 |
| Colima | 711,235 | 126 | 0.849 | 2434 | 22 | 23 | 584 |
| Durango | 1,754,754 | 14 | 0.844 | 2013 | 24 | 17 | 431 |
| Mexico | 5,853,677 | 191 | 0.844 | 2128 | 50 | 18 | 460 |
| Guanajuato | 3,533,251 | 56 | 0.813 | 1353 | 26 | 25 | 622 |
| Guerrero | 2,858,359 | 137 | 0.842 | 1789 | 35 | 19 | 472 |
| Hidalgo | 7,844,830 | 100 | 0.849 | 2792 | 32 | 16 | 400 |
| Jalisco | 16,187,608 | 724 | 0.848 | 2215 | 30 | 12 | 292 |
| Michoacán | 4,584,471 | 78 | 0.838 | 1967 | 29 | 15 | 384 |
| Morelos | 1,903,811 | 390 | 0.844 | 1982 | 55 | 12 | 290 |
| Nayarit | 1,181,050 | 42 | 0.847 | 2221 | 31 | 18 | 458 |
| Nuevo Leon | 5,119,504 | 80 | 0.857 | 3181 | 26 | 26 | 656 |
| Oaxaca | 3,967,889 | 42 | 0.827 | 1457 | 41 | 15 | 374 |
| Puebla | 6,168,883 | 180 | 0.837 | 1798 | 41 | 19 | 472 |
| Queretaro | 2,038,372 | 174 | 0.852 | 2829 | 42 | 29 | 375 |
| Quintana Roo | 1,501,562 | 34 | 0.851 | 2616 | 42 | 29 | 733 |
| San Luis Potosi | 2,717,820 | 44 | 0.839 | 2145 | 26 | 31 | 767 |
| Sinaloa | 2,966,321 | 52 | 0.844 | 2559 | 50 | 23 | 584 |
| Sonora | 2,850,330 | 16 | 0.849 | 2762 | 56 | 33 | 815 |
| Tabasco | 2,395,272 | 97 | 0.843 | 1820 | 45 | 50 | 1250 |
| Tamaulipas | 3,441,698 | 43 | 0.846 | 2267 | 35 | 31 | 784 |
| Tlaxcala | 1,272,847 | 318 | 0.845 | 1859 | 39 | 22 | 548 |
| Veracruz | 8,112,505 | 113 | 0.834 | 1497 | 39 | 15 | 381 |
| Yucatan | 2,097,175 | 53 | 0.837 | 2301 | 30 | 31 | 774 |
| Zacatecas | 1,579,209 | 21 | 0.842 | 1751 | 23 | 16 | 393 |
| Variables | Doubling Time (Model 1) | Doubling Time (Model 2) |
|---|---|---|
| Policy index | 1.378 *** | 0.601 *** |
| (0.163) | (0.168) | |
| Population density | −0.00708 | −0.0120 ** |
| (0.00523) | (0.00528) | |
| Population size (log) | −1.922 * | −1.212 |
| (1.068) | (1.094) | |
| Health index | 1,417 ** | 1134 ** |
| (693.4) | (700.6) | |
| Population poverty (%) | 2.405 *** | 3.290 *** |
| (0.794) | (0.804) | |
| Income per capita (in thousands) | 1.006 | 3.366 *** |
| (0.958) | (0.978) | |
| Mobility in parks | −1.105 *** | |
| (0.389) | ||
| Mobility in transit stations | −0.883 ** | |
| (0.376) | ||
| Mobility in workplaces | 0.821 ** | |
| (0.403) | ||
| Mobility in residential areas | −4.195 *** | |
| (1.460) | ||
| Constant | −1.362 ** | −1.168 * |
| (611.1) | (616.2) | |
| Observations | 739 | 739 |
| Number of states | 31 | 31 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz-Castro, L.; Cabello-Rangel, H.; Hoffman, K. The Impact of Health Policies and Sociodemographic Factors on Doubling Time of the COVID-19 Pandemic in Mexico. Int. J. Environ. Res. Public Health 2021, 18, 2354. https://doi.org/10.3390/ijerph18052354
Díaz-Castro L, Cabello-Rangel H, Hoffman K. The Impact of Health Policies and Sociodemographic Factors on Doubling Time of the COVID-19 Pandemic in Mexico. International Journal of Environmental Research and Public Health. 2021; 18(5):2354. https://doi.org/10.3390/ijerph18052354
Chicago/Turabian StyleDíaz-Castro, Lina, Héctor Cabello-Rangel, and Kurt Hoffman. 2021. "The Impact of Health Policies and Sociodemographic Factors on Doubling Time of the COVID-19 Pandemic in Mexico" International Journal of Environmental Research and Public Health 18, no. 5: 2354. https://doi.org/10.3390/ijerph18052354







