Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification
Abstract
1. Should Post-COVID Symptoms Be Considered a New “Syndrome”?
2. How Should Post-COVID Symptoms Be Defined?
- Confirmed (positive diagnosis of SARS-CoV-2 with real-time reverse transcription-polymerase chain reaction [RT/PCR] and/or positive SARS-CoV-2 antibodies testing);
- Probable (symptoms consistent with COVID-19, with negative RT-PCR and/or antibody test, with or without positive radiological signs but WITH contact with a confirmed/suspected case of COVID-19 the previous 2 weeks before the symptom onset);
- Possible (symptoms consistent with COVID-19, with negative RT-PCR and/or antibody tests, with/without radiological signs but WITHOUT contact with a confirmed or suspected case of COVID-19 the previous 2 weeks before the onset of the symptoms) [18].
3. Is There a Timeframe for Defining Post-COVID Symptoms?
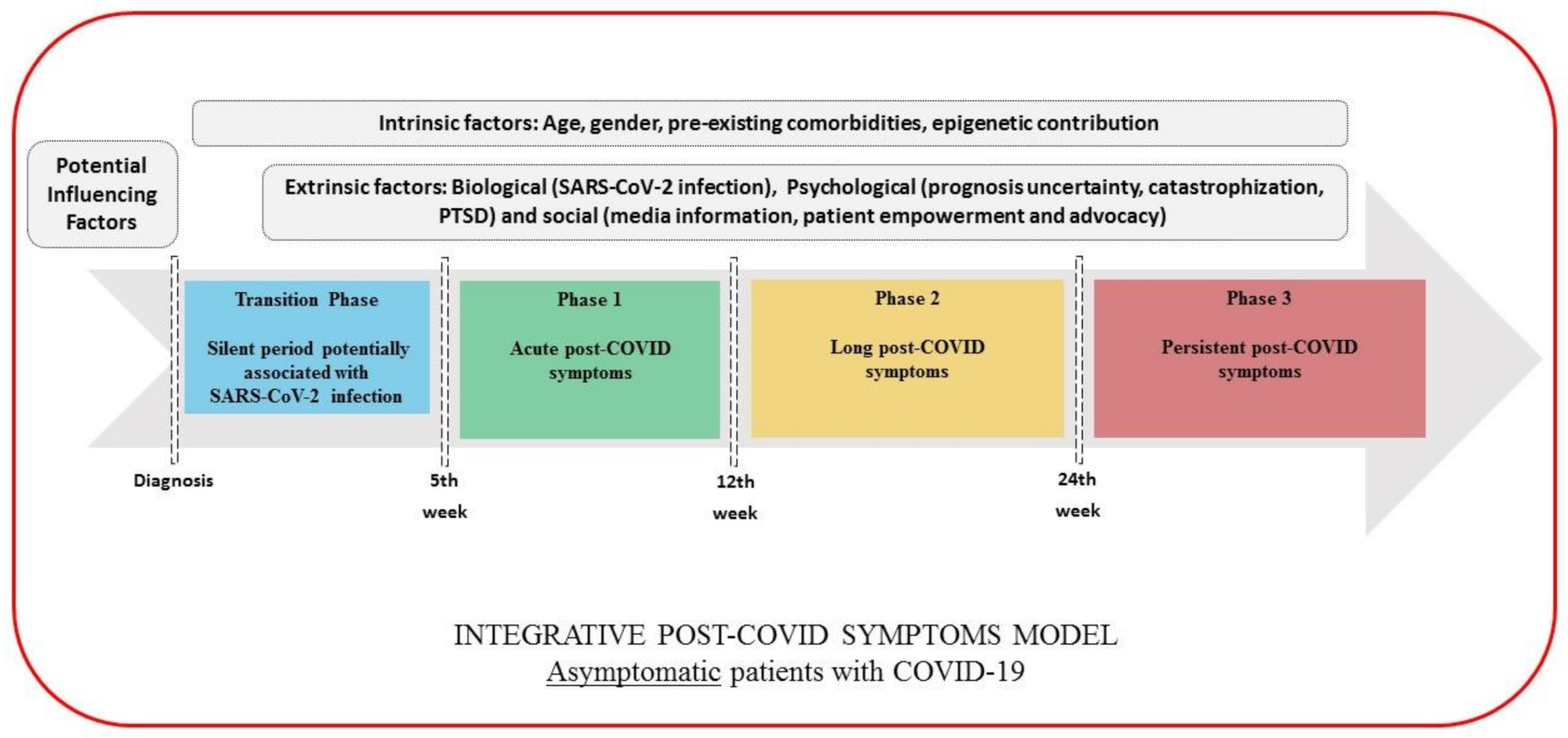
4. Integrative Classification for Defining Post-COVID Symptoms
- Transition Phase: Symptoms potentially associated with acute COVID-19: symptoms up to 4–5 weeks;
- Phase 1: Acute post-COVID symptoms: symptoms from week 5 to week 12;
- Phase 2: Long post-COVID symptoms: symptoms from week 12 to week 24;
- Phase 3: Persistent post-COVID symptoms: symptoms lasting more than 24 weeks.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marshall, M. The lasting misery of coronavirus long-haulers. Nature 2020, 585, 339–341. [Google Scholar] [CrossRef]
- Rubin, R. As their numbers grow, COVID-19 “Long Haulers” stump experts. JAMA 2020. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- No authors listed. Long COVID: Let patients help define long-lasting COVID symptoms. Nature 2020, 586, 170. [Google Scholar] [CrossRef]
- Callard, F.; Perego, E. How and why patients made Long Covid. Soc. Sci. Med. 2021, 268, 113426. [Google Scholar] [CrossRef] [PubMed]
- The Lancet. Facing up to long COVID. Lancet 2020, 396, 1861. [Google Scholar] [CrossRef]
- Carfì, A.; Bernabei, R.; Landi, F.; Gemelli against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients after Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef]
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef]
- Carvalho-Schneider, C.; Laurent, E.; Lemaignen, A.; Beaufils, E.; Bourbao-Tournois, C.; Laribi, S.; Flament, T.; Ferreira-Maldent, N.; Bruyère, F.; Stefic, K.; et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin. Microbiol. Infect. 2021, 27, 258–263. [Google Scholar] [CrossRef]
- Arnold, D.T.; Hamilton, F.W.; Milne, A.; Morley, A.J.; Viner, J.; Attwood, M.; Noel, A.; Gunning, S.; Hatrick, J.; Hamilton, S.; et al. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: Results from a prospective UK cohort. Thorax 2020. online ahead of print. [Google Scholar] [CrossRef]
- Mandal, S.; Barnett, J.; Brill, S.E.; Brown, J.S.; Denneny, E.K.; Hare, S.S.; Heightman, M.; Hillman, T.E.; Jacob, J.; Jarvis, H.C.; et al. ‘Long-COVID’: A cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax 2020. online ahead of print. [Google Scholar] [CrossRef]
- Nehme, M.; Braillard, O.; Alcoba, G.; Aebischer-Perone, S.; Courvoisier, D.; Chappuis, F.; Guessous, I. COVID-19 symptoms: Longitudinal evolution and persistence in outpatient settings. Ann. Intern. Med. 2020, M20-5926, 1–4. [Google Scholar] [CrossRef]
- Tenforde, M.W.; Kim, S.S.; Lindsell, C.J.; Rose, E.B.; Shapiro, N.I.; Files, D.C.; Gibbs, K.W.; Erickson, H.L.; Steingrub, J.S.; Smithline, H.A.; et al. Symptom duration and risk factors for delayed return to usual health among outpatients with Covid-19 in a multistate health care systems network-United States, March–June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 993–998. [Google Scholar] [CrossRef] [PubMed]
- Stavem, K.; Ghanima, W.; Olsen, M.K.; Gilboe, H.M.; Einvik, G. Persistent symptoms 1.5–6 months after COVID-19 in non-hospitalised subjects: A population-based cohort study. Thorax 2020. online ahead of print. [Google Scholar] [CrossRef]
- Page, M. The British Medical Association Illustrated Medical Dictionary, 4th ed.; Dorling Kindersley: London, UK, 2018; pp. 177–536. [Google Scholar]
- Mahase, E. COVID-19: What do we know about “long COVID”? BMJ 2020, 370, m2815. [Google Scholar] [CrossRef] [PubMed]
- Nabavi, N. Long COVID: How to define it and how to manage it. BMJ 2020, 370, m3489. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (NICE), Royal College of General Practitioners, Healthcare Improvement Scotland SIGN. COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19; National Institute for Health and Care Excellence: London, UK, 2020; Available online: www.nice.org.uk/guidance/ng188 (accessed on 30 December 2020).
- Raveendran, A. Long COVID-19: Challenges in the diagnosis and proposed diagnostic criteria. Diabetes Metab. Syndr. 2020, 15, 145–146. [Google Scholar] [CrossRef]
- Oran, D.P.; Topol, E.J. Prevalence of asymptomatic SARS-CoV-2 Infection: A narrative review. Ann. Intern. Med. 2020, 173, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Alimohamadi, Y.; Sepandi, M.; Taghdir, M.; Hosamirudsari, H. Determine the most common clinical symptoms in COVID-19 patients: A systematic review and meta-analysis. J. Prev. Med. Hyg. 2020, 61, E304–E312. [Google Scholar] [CrossRef]
- Ticona, J.H.; Zaccone, V.M.; McFarlane, I.M. Community-acquired pneumonia: A focused review. Am. J. Med. Case Rep. 2021, 9, 45–52. [Google Scholar] [CrossRef]
- Tostmann, A.; Bradley, J.; Bousema, T.; Yiek, W.-K.; Holwerda, M.; Bleeker-Rovers, C.; Oever, J.T.; Meijer, C.; Rahamat-Langendoen, J.; Hopman, J.; et al. Strong associations and moderate predictive value of early symptoms for SARS-CoV-2 test positivity among healthcare workers, the Netherlands, March 2020. Eurosurveillance 2020, 25, 2000508. [Google Scholar] [CrossRef]
- Magnavita, N.; Tripepi, G.; Di Prinzio, R.R. Symptoms in health care workers during the COVID-19 epidemic. A cross-sectional survey. Int. J. Environ. Res. Public Health 2020, 17, 5218. [Google Scholar] [CrossRef]
- Yelin, D.; Margalit, I.; Yahav, D.; Runold, M.; Bruchfeld, J. Long COVID-19-it’s not over until? Clin. Microbiol. Infect. 2020. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Mair, M.D.D.; Hussain, M.; Siddiqui, S.; Das, S.; Baker, A.; Conboy, P.; Valsamakis, T.; Uddin, J.; Rea, P. A systematic review and meta-analysis comparing the diagnostic accuracy of initial RT-PCR and CT scan in suspected COVID-19 patients. Br. J. Radiol. 2021, 94, 20201039, online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Dinnes, J.; Takwoingi, Y.; Davenport, C.; Spijker, R.; Taylor-Phillips, S.; Adriano, A.; Beese, S.; Dretzke, J.; Di Ruffano, L.F.; et al. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst. Rev. 2020, 6, CD013652. [Google Scholar] [CrossRef] [PubMed]
- Baig, A.M. Chronic COVID Syndrome: Need for an appropriate medical terminology for Long-COVID and COVID Long-Haulers. J. Med. Virol 2020. online ahead of print. [Google Scholar] [CrossRef]
- Halpin, S.; O’Connor, R.; Sivan, M. Long COVID and chronic COVID syndromes. J. Med. Virol 2020. online ahead of print. [Google Scholar] [CrossRef]
- Sivan, M.; Taylor, S. NICE guideline on long covid. BMJ 2020, 371, m4938. [Google Scholar] [CrossRef] [PubMed]
- Lauer, S.A.; Grantz, K.H.; Bi, Q.; Jones, F.K.; Zheng, Q.; Meredith, H.R.; Azman, A.S.; Reich, N.G.; Lessler, J. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann. Intern. Med. 2020, 172, 577–582. [Google Scholar] [CrossRef]
- Ikegami, S.; Benirschke, R.; Flanagan, T.; Tanna, N.; Klein, T.; Elue, R.; Debosz, P.; Mallek, J.; Wright, G.; Guariglia, P.; et al. Persistence of SARS-CoV-2 nasopharyngeal swab PCR positivity in COVID-19 convalescent plasma donors. Transfusion 2020, 60, 2962–2968. [Google Scholar] [CrossRef]
- Magnavita, N.; Soave, P.M.; Ricciardi, W.; Antonelli, M. Occupational stress and mental health of anesthetists during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 8245. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Di Prinzio, R.R.; Chirico, F.; Sacco, A.; Quintavalle, G. COVID-19 and staff mental health: Is there an evidence? An Italian field study. Eur. J. Public Health 2020, 30, ckaa165.565. [Google Scholar] [CrossRef]
- Alanzi, T. A Review of mobile applications available in the app and google play stores used during the COVID-19 outbreak. J. Multidiscip. Healthc. 2021, 14, 45–57. [Google Scholar] [CrossRef]
- NIHR. Living with Covid-19. A Dynamic Review of the Evidence around Ongoing COVID-19 SYMPTOMS (Often Called Long COVID). Available online: https://evidence.nihr.ac.uk/themedreview/living-with-covid19 (accessed on 15 October 2020).
- Mahase, E. Long COVID Could Be Four Different Syndromes, Review Suggests. BMJ 2020, 371, m3981. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-de-las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Cuadrado, M.L.; Florencio, L.L. Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification. Int. J. Environ. Res. Public Health 2021, 18, 2621. https://doi.org/10.3390/ijerph18052621
Fernández-de-las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Cuadrado ML, Florencio LL. Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification. International Journal of Environmental Research and Public Health. 2021; 18(5):2621. https://doi.org/10.3390/ijerph18052621
Chicago/Turabian StyleFernández-de-las-Peñas, César, Domingo Palacios-Ceña, Víctor Gómez-Mayordomo, María L. Cuadrado, and Lidiane L. Florencio. 2021. "Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification" International Journal of Environmental Research and Public Health 18, no. 5: 2621. https://doi.org/10.3390/ijerph18052621
APA StyleFernández-de-las-Peñas, C., Palacios-Ceña, D., Gómez-Mayordomo, V., Cuadrado, M. L., & Florencio, L. L. (2021). Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification. International Journal of Environmental Research and Public Health, 18(5), 2621. https://doi.org/10.3390/ijerph18052621







