Relationship between Neuromuscular Mechanosensitivity and Chronic Neck Pain in Guitarists: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Subjects
2.3. Sample Size
2.4. Measurements
2.4.1. Pain and Disability
2.4.2. Pressure Pain Threshold
2.4.3. Upper Limb Neural Test One
2.5. Statistical Analysis
3. Results
3.1. Pressure Pain Threshold
3.2. Upper Limb Neural Tension Test One
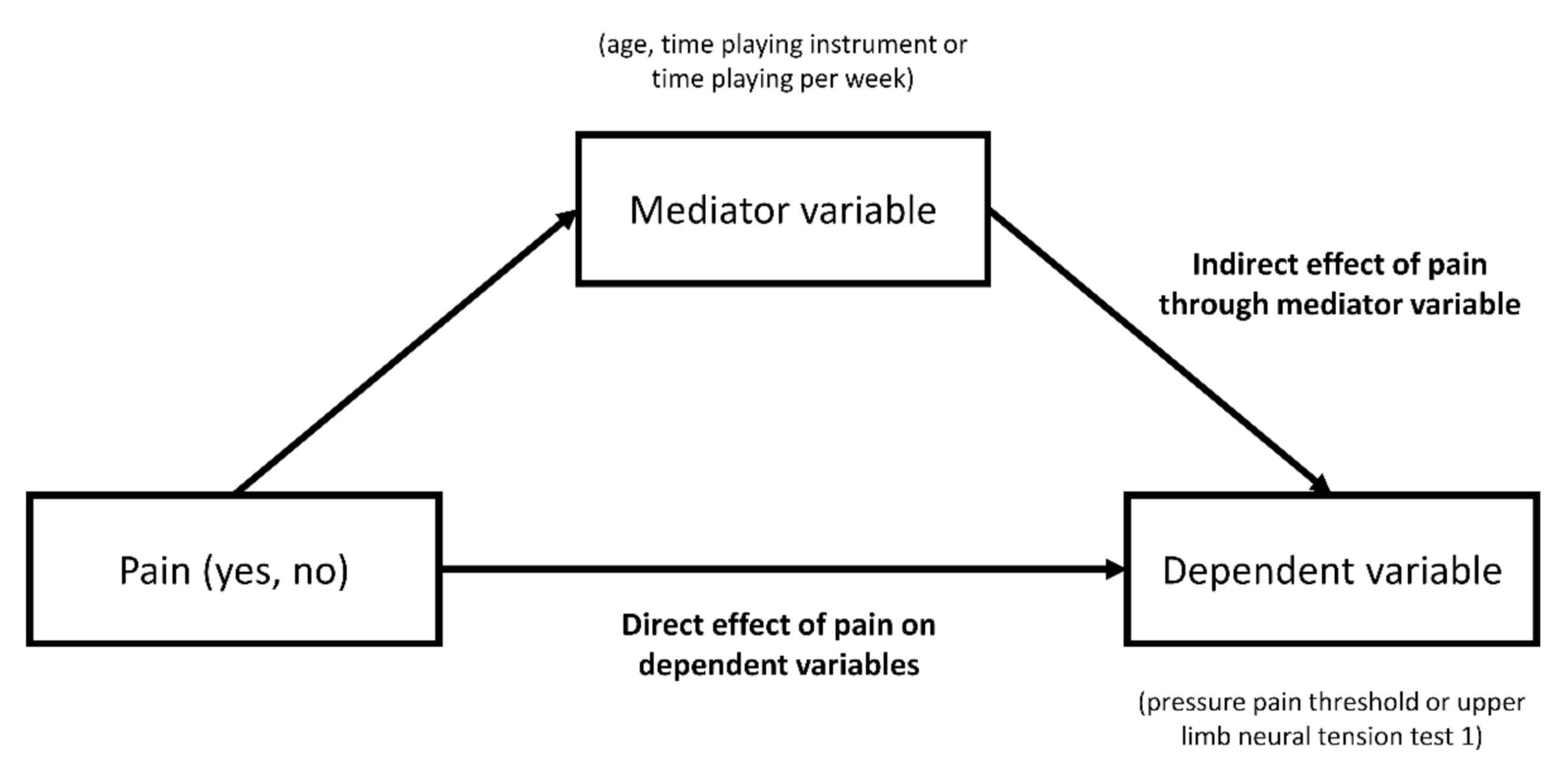
3.3. Simple Mediation Analyses
3.4. Multiple Regression Analyses for Tissue Mechanosensitivity
3.5. Relationship between Pain and Disability
3.6. Relationship between Pressure Pain Threshold and Upper Limb Neural Tension Test One
4. Discussion
4.1. Pressure Pain Threshold
4.2. Upper Limb Neural Tension Test One
4.3. Simple Mediation Analyses
4.4. Multiple Regression Analyses for Tissue Mechanosensitivity
4.5. Relationship between Pain and Disability
4.6. Relationship between Pressure Pain Threshold and Upper Limb Neural Tension Test One
4.7. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hansen, P.A.; Reed, K. Common Musculoskeletal Problems in the Performing Artist. Phys. Med. Rehabil. Clin. N. Am. 2006, 17, 789–801. [Google Scholar] [CrossRef]
- Rickert, D.L.; Barrett, M.S.; Ackermann, B.J. Injury and the orchestral environment: Part I. The role of work organisation and psychosocial factors in injury risk. Med. Probl. Perform. Art. 2013, 28, 219–229. [Google Scholar] [PubMed]
- Silva, A.G.; Lã, F.M.B.; Afreixo, V. Pain Prevalence in Instrumental Musicians: A Systematic Review. Med. Probl. Perform. Art. 2015, 30, 8–19. [Google Scholar] [CrossRef]
- Kok, L.M.; Huisstede, B.M.A.; Voorn, V.M.A.; Schoones, J.W.; Nelissen, R.G.H.H. The occurrence of musculoskeletal complaints among professional musicians: A systematic review. Int. Arch. Occup. Environ. Health 2016, 89, 373–396. [Google Scholar] [CrossRef] [PubMed]
- Zaza, C. Playing-related musculoskeletal disorders in musicians: A systematic review of incidence and prevalence. CMAJ 1998, 158, 1019–1025. [Google Scholar]
- Kok, L.M.; Vlieland, T.P.V.; Fiocco, M.; Nelissen, R.G. A comparative study on the prevalence of musculoskeletal complaints among musicians and non-musicians. BMC Musculoskelet. Disord. 2013, 14, 9. [Google Scholar] [CrossRef] [PubMed]
- Baadjou, V.A.E.; Roussel, N.A.; Verbunt, J.A.M.C.F.; Smeets, R.J.E.M.; de Bie, R.A. Systematic review: Risk factors for musculoskeletal disorders in musicians. Occup. Med. 2016, 66, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Fejer, R.; Kyvik, K.O.; Hartvigsen, J. The prevalence of neck pain in the world population: A systematic critical review of the literature. Eur. Spine J. 2006, 15, 834–848. [Google Scholar] [CrossRef] [PubMed]
- Côté, P.; Cassidy, J.D.; Carroll, L.J.; Kristman, V. The annual incidence and course of neck pain in the general population: A population-based cohort study. Pain 2004, 112, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Dieleman, J.L.; Baral, R.; Birger, M.; Bui, A.L.; Bulchis, A.; Chapin, A.; Hamavid, H.; Horst, C.; Johnson, E.K.; Joseph, J.; et al. US Spending on Personal Health Care and Public Health, 1996–2013. JAMA 2016, 316, 2627. [Google Scholar] [CrossRef]
- Côté, P.; Wong, J.J.; Sutton, D.; Shearer, H.M.; Mior, S.; Randhawa, K.; Ameis, A.; Carroll, L.J.; Nordin, M.; Yu, H.; et al. Management of neck pain and associated disorders: A clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur. Spine J. 2016, 25, 2000–2022. [Google Scholar] [CrossRef]
- López-de-Uralde-Villanueva, I.; Beltran-Alacreu, H.; Fernández-Carnero, J.; Gil-Martínez, A.; La Touche, R. Differences in Neural Mechanosensitivity between Patients with Chronic Nonspecific Neck Pain With and Without Neuropathic Features. A Descriptive Cross-Sectional Study. Pain Med. 2015, 17, 136–148. [Google Scholar] [CrossRef][Green Version]
- Martinez-Merinero, P.; Nuñez-Nagy, S.; Achalandabaso-Ochoa, A.; Fernandez-Matias, R.; Pecos-Martin, D.; Gallego-Izquierdo, T. Relationship between Forward Head Posture and Tissue Mechanosensitivity: A Cross-Sectional Study. J. Clin. Med. 2020, 9, 634. [Google Scholar] [CrossRef] [PubMed]
- Sanchis-Alfonso, V.; Roselló-Sastre, E. Hypothesis: Anterior knee pain in the young patient-what causes the pain? ”Neural model”. Acta Orthop. Scand. 2003, 74, 697–703. [Google Scholar] [CrossRef]
- McDougall, J.J. Arthritis and pain. Neurogenic origin of joint pain. Arthritis Res. Ther. 2006, 8, 220. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, J.; Raimundo, J.; Santos, F.; Ferreira, M.; Lopes, T.; Ramos, L.; Silva, A.G. Forward head posture is associated with pressure pain threshold and neck pain duration in university students with subclinical neck pain. Somatosens. Mot. Res. 2018, 35, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Dhrithi, M.A.; Agrawal, P.R.; Aju, K. Prevalence of playing-related musculoskeletal disorder (PRMSD) among amateur young guitar players. J. Musculoskelet. Res. 2013, 16, 1–6. [Google Scholar] [CrossRef]
- Silva, F.M.; Brismée, J.-M.; Sizer, P.S.; Hooper, T.L.; Robinson, G.E.; Diamond, A.B. Musicians injuries: Upper quarter motor control deficits in musicians with prolonged symptoms—A case-control study. Musculoskelet. Sci. Pract. 2018, 36, 54–60. [Google Scholar] [CrossRef]
- Overton, M.; Du Plessis, H.; Sole, G. Electromyography of neck and shoulder muscles in instrumental musicians with musculoskeletal pain compared to asymptomatic controls: A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2018, 36, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; Blettner, M.; et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF36–BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar] [CrossRef]
- Kahl, C.; Cleland, J.A. Visual analogue scale, numeric pain rating scale and the McGill pain Questionnaire: An overview of psychometric properties. Phys. Ther. Rev. 2005, 10, 123–128. [Google Scholar] [CrossRef]
- Andrade Ortega, J.A.; Delgado Martínez, A.D.; Ruiz, R.A. Validation of the Spanish Version of the Neck Disability Index. Spine 2010, 35, E114–E118. [Google Scholar] [CrossRef]
- Teresa Hervás, M.; Navarro Collado, M.J.; Peiró, S.; Rodrigo Pérez, J.L.; López Matéu, P.; Martínez Tello, I. Versión española del cuestionario DASH. Adaptación transcultural, fiabilidad, validez y sensibilidad a los cambios. Med. Clin. 2006, 127, 441–447. [Google Scholar] [CrossRef]
- Ylinen, J.; Nykänen, M.; Kautiainen, H.; Häkkinen, A. Evaluation of repeatability of pressure algometry on the neck muscles for clinical use. Man. Ther. 2007, 12, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Sterling, M.; Treleaven, J.; Edwards, S.; Jull, G. Pressure pain thresholds of upper limb peripheral nerve trunks in asymptomatic subjects. Physiother. Res. Int. 2000, 5, 220–229. [Google Scholar] [CrossRef]
- Martínez-Merinero, P.; Lluch, E.; Gallezo-Izquierdo, T.; Pecos-Martín, D.; Plaza-Manzano, G.; Nuñez-Nagy, S.; Falla, D. The influence of a depressed scapular alignment on upper limb neural tissue mechanosensitivity and local pressure pain sensitivity. Musculoskelet. Sci. Pract. 2017, 29, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Oliver, G.S.; Rushton, A. A study to explore the reliability and precision of intra and inter-rater measures of ULNT1 on an asymptomatic population. Man. Ther. 2011, 16, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Field, A.P. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; SAGE Publications Ltd.: London, UK, 2018. [Google Scholar]
- Hayes, A.F.; Rockwood, N.J. Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behav. Res. Ther. 2017, 98, 39–57. [Google Scholar] [CrossRef]
- Kok, L.M.; Groenewegen, K.A.; Huisstede, B.M.A.; Nelissen, R.G.H.H.; Rietveld, A.B.M.; Haitjema, S. The high prevalence of playing-related musculoskeletal disorders (PRMDs) and its associated factors in amateur musicians playing in student orchestras: A cross-sectional study. PLoS ONE 2018, 13, e0191772. [Google Scholar] [CrossRef]
- Quaghebeur, J.; Wyndaele, J.-J.; De Wachter, S. Pain areas and mechanosensitivity in patients with chronic pelvic pain syndrome: A controlled clinical investigation. Scand. J. Urol. 2017, 51, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Arnstein, P.; Caudill, M.; Mandle, C.L.; Norris, A.; Beasley, R. Self efficacy as a mediator of the relationship between pain intensity, disability and depression in chronic pain patients. Pain 1999, 80, 483–491. [Google Scholar] [CrossRef]
- Moraska, A.F.; Hickner, R.C.; Kohrt, W.M.; Brewer, A. Changes in Blood Flow and Cellular Metabolism at a Myofascial Trigger Point With Trigger Point Release (Ischemic Compression): A Proof-of-Principle Pilot Study. Arch. Phys. Med. Rehabil. 2013, 94, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Al-Shatti, T.; Barr, A.E.; Safadi, F.F.; Amin, M.; Barbe, M.F. Increase in inflammatory cytokines in median nerves in a rat model of repetitive motion injury. J. Neuroimmunol. 2005, 167, 13–22. [Google Scholar] [CrossRef][Green Version]
- Yılmaz, S.; Taş, S.; Tunca Yılmaz, Ö. Comparison of Median Nerve Mechanosensitivity and Pressure Pain Threshold in Patients With Nonspecific Neck Pain and Asymptomatic Individuals. J. Manip. Physiol. Ther. 2018, 41, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Chacur, M.; Milligan, E.D.; Gazda, L.S.; Armstrong, C.; Wang, H.; Tracey, K.J.; Maier, S.F.; Watkins, L.R. A new model of sciatic inflammatory neuritis (SIN): Induction of unilateral and bilateral mechanical allodynia following acute unilateral peri-sciatic immune activation in rats. Pain 2001, 94, 231–244. [Google Scholar] [CrossRef]
- McLean, S.M.; Moffett, J.K.; Sharp, D.M.; Gardiner, E. An investigation to determine the association between neck pain and upper limb disability for patients with non-specific neck pain: A secondary analysis. Man. Ther. 2011, 16, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Nee, R.J.; Yang, C.-H.; Liang, C.-C.; Tseng, G.-F.; Coppieters, M.W. Impact of order of movement on nerve strain and longitudinal excursion:A biomechanical study with implications for neurodynamic test sequencing. Man. Ther. 2010, 15, 376–381. [Google Scholar] [CrossRef]
| Characteristic * | Healthy (n = 70) | Neck Pain (n = 70) | p-Value |
|---|---|---|---|
| Age, years | 25.46 (10.01) | 32.99 (10.25) | < 0.01 |
| Weight, kg | 69.10 (11.92) | 69.60 (8.85) | 0.78 |
| Height, cm | 164.24 (7.13) | 165.63 (5.23) | 0.19 |
| BMI, kg/m2 | 25.63 (4.11) | 25.38 (3.09) | 0.66 |
| Time sleeping, hours | 6.60 (1.27) | 6.27 (1.08) | 0.10 |
| Time playing instrument, years | 7.11 (7.15) | 15.26 (9.28) | < 0.01 |
| Time playing per week, hours | 10.63 (6.42) | 20.18 (7.80) | < 0.01 |
| Time with pain, months | - | 19.23 (16.60) | |
| VAS pain, cm | - | 3.94 (1.61) | |
| DASH | - | 52.01 (10.57) | |
| DASH, sport activities | - | 5.69 (2.18) | |
| NDI | - | 27.31 (8.75) | |
| Sex women, n (%) | 12 (17.1) | 12 (17.1) | 1.00 |
| Dominant side R, n (%) | 68 (97.1) | 64 (91.4) | 0.28 |
| Physical exercise #, n (%) | 14 (20) | 10 (14.3) | 0.37 |
| Location of Measurement * | Healthy (n = 70) | Neck Pain (n = 70) | Between-Group Differences, Mean (95% CI) | Effect Size (95% CI) |
|---|---|---|---|---|
| Upper trapezius, dominant side | 4.65 (1.82) | 3.19 (1.28) | −1.46 ‡ (−1.99, −0.93) | 0.93 (0.57, 1.28) |
| Upper trapezius, non-dominant side | 4.35 (1.71) | 3.12 (1.06) | −1.23 ‡ (−1.71, −0.76) | 0.87 (0.52, 1.22) |
| Median nerve, dominant side | 4.00 (1.52) | 2.79 (1.44) | −1.21 ‡ (−1.70, −0.71) | 0.82 (0.47, 1.16) |
| Median nerve, non-dominant side | 4.08 (1.73) | 2.83 (1.52) | −1.25 ‡ (−1.79, −0.70) | 0.77 (0.42, 1.11) |
| ULNT1 * | Healthy (n = 70) | Neck Pain (n = 70) | Between-Group Differences, Mean (95% CI) | Effect Size (95% CI) |
|---|---|---|---|---|
| Dominant side | −18.21 (6.75) | −22.84 (11.14) | 4.63 ‡ (1.55, 7.71) | 0.50 (0.16, 0.84) |
| Non-dominant side | −17.79 (4.45) | −22.55 (10.77) | 4.76 ‡ (2.01, 7.52) | 0.58 (0.24, 0.92) |
| Variable * | Age | Time Playing Instrument | Time Playing Per Week |
|---|---|---|---|
| PPT UT dominant side | 0.06 (−0.13, 0.47) | 0.10 (−0.33, 0.45) | −0.05 (−0.34, 0.32) |
| PPT UT non-dominant side | −0.03 (−0.23, 0.24) | 0.17 (−0.17, 0.54) | 0.03 (−0.23, 0.41) |
| PPT MN dominant side | −0.05 (-0.30, 0.23) | 0.11 (−0.24, 0.44) | −0.07 (−0.38, 0.34) |
| PPT MN non-dominant side | −0.06 (−0.20, 0.50) | −0.03 (−0.53, 0.40) | −0.05 (−0.40, 0.43) |
| ULNT1 dominant side | 0.01 (−0.17, 0.18) | −0.09 (−0.33, 0.12) | −0.15 (−0.41, 0.03) |
| ULNT1 non-dominant side | 0.37 (−0.89, 2.05) | −1.17 (−3.19, 0.38) | −0.76 (−2.69, 0.71) |
| Model R2 | Step 2 R2 Change | p-Value | |
|---|---|---|---|
| Pressure pain threshold, median nerve (predicted) | |||
| Step 1 | 0.15 | ||
| Step 2 | 0.22 | 0.07 | 0.50 |
| Pressure pain threshold, upper trapezius (predicted) | |||
| Step 1 | 0.17 | ||
| Step 2 | 0.28 | 0.11 | 0.21 |
| Upper limb neural test 1 (predicted) | |||
| Step 1 | 0.09 | ||
| Step 2 | 0.16 | 0.07 | 0.56 |
| Model R2 | Step 2 R2 Change | p-Value | |
|---|---|---|---|
| VAS predicted by NDI and DASH | |||
| Step 1 | 0.08 | ||
| Step 2 | 0.22 | 0.14 | < 0.01 |
| NDI predicted by DASH | |||
| Step 1 | 0.13 | ||
| Step 2 | 0.14 | 0.01 | 0.87 |
| ULNT1 predicted by PPT-UT and PPT-MN | |||
| Step 1 | 0.07 | ||
| Step 2 | 0.10 | 0.03 | 0.12 |
| PPT-UT predicted by PPT-MN | |||
| Step 1 | 0.09 | ||
| Step 2 | 0.55 | 0.46 | < 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rojas, V.E.A.; Pluma, A.F.; Pecos-Martín, D.; Achalandabaso-Ochoa, A.; Fernández-Matías, R.; Martinez-Merinero, P.; Nuñez-Nagy, S.; Gallego-Izquierdo, T. Relationship between Neuromuscular Mechanosensitivity and Chronic Neck Pain in Guitarists: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 2673. https://doi.org/10.3390/ijerph18052673
Rojas VEA, Pluma AF, Pecos-Martín D, Achalandabaso-Ochoa A, Fernández-Matías R, Martinez-Merinero P, Nuñez-Nagy S, Gallego-Izquierdo T. Relationship between Neuromuscular Mechanosensitivity and Chronic Neck Pain in Guitarists: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(5):2673. https://doi.org/10.3390/ijerph18052673
Chicago/Turabian StyleRojas, Valeria Estefanía Aguilar, Arisandy Flores Pluma, Daniel Pecos-Martín, Alexander Achalandabaso-Ochoa, Rubén Fernández-Matías, Patricia Martinez-Merinero, Susana Nuñez-Nagy, and Tomás Gallego-Izquierdo. 2021. "Relationship between Neuromuscular Mechanosensitivity and Chronic Neck Pain in Guitarists: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 5: 2673. https://doi.org/10.3390/ijerph18052673
APA StyleRojas, V. E. A., Pluma, A. F., Pecos-Martín, D., Achalandabaso-Ochoa, A., Fernández-Matías, R., Martinez-Merinero, P., Nuñez-Nagy, S., & Gallego-Izquierdo, T. (2021). Relationship between Neuromuscular Mechanosensitivity and Chronic Neck Pain in Guitarists: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(5), 2673. https://doi.org/10.3390/ijerph18052673







