Towards Standardization in the Diagnostic Evaluation of ACL Injuries in Skeletally Immature Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Delphi Panel
2.2. Delphi Structure and Data Collection
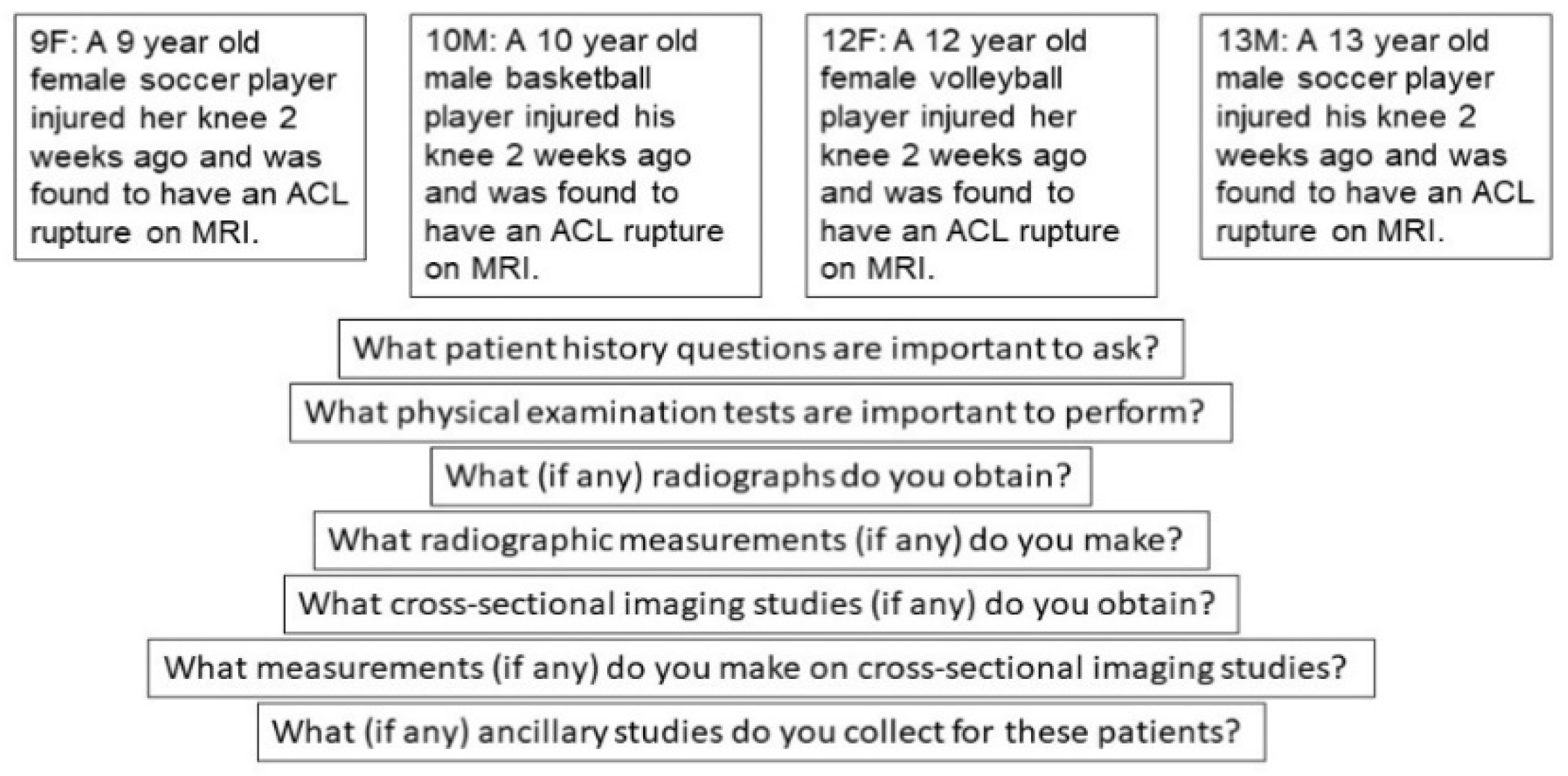
- What patient history questions are important to ask?
- What physical examination tests are important to perform?
- What (if any) radiographs do you obtain?
- What radiographic measurements (if any) do you make?
- What cross-sectional imaging studies (if any) do you obtain?
- What measurements (if any) do you make on cross-sectional imaging studies?
- What (if any) ancillary studies do you collect for these patients?
3. Results
3.1. Delphi Panelists
3.2. Consensus and Disagreement
3.2.1. Historical Factors
3.2.2. Physical Examination Factors
3.2.3. Radiographic Sequences
3.2.4. Radiographic Measurements
3.2.5. Cross-Sectional Imaging
3.2.6. Cross-Sectional Measurements
3.2.7. Ancillary Diagnostics
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dodwell, E.R.; Lamont, L.E.; Green, D.W.; Pan, T.J.; Marx, R.G.; Lyman, S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am. J. Sports Med. 2014, 42, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Gornitzky, A.L.; Lott, A.; Yellin, J.L.; Fabricant, P.D.; Lawrence, J.T.; Ganley, T.J. Sport-Specific Yearly Risk and Incidence of Anterior Cruciate Ligament Tears in High School Athletes: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2016, 44, 2716–2723. [Google Scholar] [CrossRef] [PubMed]
- Jayanthi, N.A.; LaBella, C.R.; Fischer, D.; Pasulka, J.; Dugas, L.R. Sports-specialized intensive training and the risk of injury in young athletes: A clinical case-control study. Am. J. Sports Med. 2015, 43, 794–801. [Google Scholar] [CrossRef]
- Shea, K.G.; Grimm, N.L.; Ewing, C.K.; Aoki, S.K. Youth sports anterior cruciate ligament and knee injury epidemiology: Who is getting injured? In what sports? When? Clin. Sports Med. 2011, 30, 691–706. [Google Scholar] [CrossRef] [PubMed]
- Shaw, L.; Finch, C.F. Trends in Pediatric and Adolescent Anterior Cruciate Ligament Injuries in Victoria, Australia 2005–2015. Int. J. Environ. Res. Public Health 2017, 14, 599. [Google Scholar] [CrossRef] [Green Version]
- Beck, N.A.; Lawrence, J.T.R.; Nordin, J.D.; DeFor, T.A.; Tompkins, M. ACL Tears in School-Aged Children and Adolescents Over 20 Years. Pediatrics 2017, 139. [Google Scholar] [CrossRef] [Green Version]
- Vavken, P.; Murray, M.M. Treating anterior cruciate ligament tears in skeletally immature patients. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2011, 27, 704–716. [Google Scholar] [CrossRef] [Green Version]
- Vavken, P.; Tepolt, F.A.; Kocher, M.S. Concurrent Meniscal and Chondral Injuries in Pediatric and Adolescent Patients Undergoing ACL Reconstruction. J. Pediatric Orthop. 2018, 38, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Millett, P.J.; Willis, A.A.; Warren, R.F. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: Does a delay in treatment increase the risk of meniscal tear? Arthroscopy 2002, 18, 955–959. [Google Scholar] [CrossRef] [Green Version]
- Lawrence, J.T.; Argawal, N.; Ganley, T.J. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: Is there harm in delay of treatment? Am. J. Sports Med. 2011, 39, 2582–2587. [Google Scholar] [CrossRef]
- Magnussen, R.A.; Pedroza, A.D.; Donaldson, C.T.; Flanigan, D.C.; Kaeding, C.C. Time from ACL injury to reconstruction and the prevalence of additional intra-articular pathology: Is patient age an important factor? Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2029–2034. [Google Scholar] [CrossRef]
- Kocher, M.S.; Saxon, H.S.; Hovis, W.D.; Hawkins, R.J. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: Survey of the Herodicus Society and The ACL Study Group. J. Pediatric Orthop. 2002, 22, 452–457. [Google Scholar] [CrossRef]
- Anderson, A.F. Transepiphyseal replacement of the anterior cruciate ligament in skeletally immature patients. A preliminary report. J. Bone Jt. Surg. Am. 2003, 85, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Calvo, R.; Figueroa, D.; Gili, F.; Vaisman, A.; Mocoçain, P.; Espinosa, M.; León, A.; Arellano, S. Transphyseal anterior cruciate ligament reconstruction in patients with open physes: 10-year follow-up study. Am. J. Sports Med. 2015, 43, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.S.; Garg, S.; Micheli, L.J. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J. Bone Jt. Surg. Am. Vol. 2005, 87, 2371–2379. [Google Scholar]
- Cohen, M.; Ferretti, M.; Quarteiro, M.; Marcondes, F.B.; De Hollanda, J.P.; Amaro, J.T.; Abdalla, R.J. Transphyseal Anterior Cruciate Ligament Reconstruction in Patients With Open Physes. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 831–838. [Google Scholar] [CrossRef] [PubMed]
- Cruz, A.I.; Lakomkin, N.; Fabricant, P.D.; Lawrence, J.T. Transphyseal ACL Reconstruction in Skeletally Immature Patients: Does Independent Femoral Tunnel Drilling Place the Physis at Greater Risk Compared With Transtibial Drilling? Orthop. J. Sports Med. 2016, 4. [Google Scholar] [CrossRef] [Green Version]
- American Academy of Orthopaedic Surgeons. Management of Anterior Cruciate Ligament Injuries: Evidence-based Clinical Practice Guideline. JAAOS 2014.
- Murry, J.W.; Hammons, J.O. Delphi: A Versatile Methodology for Conducting Qualitative Research. Rev. High. Educ. 1995, 18, 423–436. [Google Scholar] [CrossRef]
- Von der Gracht, H.A. Consensus measurement in Delphi studies: Review and implications for future quality assurance. Technol. Forecast. Soc. Chang. 2012, 79, 1525–1536. [Google Scholar] [CrossRef]
- Micheli, L.J.; Rask, B.; Gerberg, L. Anterior cruciate ligament reconstruction in patients who are prepubescent. Clin. Orthop. Relat. Res. 1999, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Garcia, S.; Pandya, N.K. Anterior Cruciate Ligament Re-tear and Revision Reconstruction in the Skeletally Immature Athlete. Curr. Rev. Musculoskelet. Med. 2020, 13, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef] [Green Version]
- Guzzanti, V.; Falciglia, F.; Stanitski, C.L. Preoperative evaluation and anterior cruciate ligament reconstruction technique for skeletally immature patients in Tanner stages 2 and 3. Am. J. Sports Med. 2003, 31, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Heyworth, B.E.; Osei, D.A.; Fabricant, P.D.; Schneider, R.; Doyle, S.M.; Green, D.W.; Widmann, R.F.; Lyman, S.; Burke, S.W.; Scher, D.M.; et al. The shorthand bone age assessment: A simpler alternative to current methods. J. Pediatric Orthop. 2013, 33, 569–574. [Google Scholar] [CrossRef] [PubMed]
| Vignette | Modal Response | Agreement | Consensus | Disagreement Sources |
|---|---|---|---|---|
| 9F | Injury History | 100 | 67% | |
| Family History | 92 | |||
| Sports Participation | 92 | |||
| Current Symptoms | 100 | |||
| 10M | Injury History | 100 | 83% | |
| Family History | 92 | |||
| Sports Participation | 92 | |||
| Current Symptoms | 100 | |||
| 12F | Injury History | 100 | 83% | Family History |
| Sports Participation | 92 | |||
| Current Symptoms | 100 | |||
| Menarche | 100 | |||
| 13M | Family History | 92 | 83% | |
| Sports Participation | 92 | |||
| Current Symptoms | 100 | |||
| Injury History | 100 |
| Vignette | Modal Response | Agreement | Consensus | Disagreement Sources |
|---|---|---|---|---|
| 9F | Lachmann | 100 | 67% | |
| Pivot-shift | 100 | |||
| Collateral exam | 100 | |||
| Meniscal Exam | 100 | |||
| ROM | 100 | |||
| Ligamentous Laxity | 100 | |||
| Effusion | 100 | |||
| 10M | Lachmann | 100 | 53% | |
| Pivot-shift | 100 | |||
| Collateral exam | 100 | |||
| Meniscal Exam | 100 | |||
| ROM | 100 | |||
| Ligamentous Laxity | 100 | |||
| Effusion | 100 | |||
| 12F | Lachmann | 100 | 75% | |
| Pivot-shift | 100 | |||
| Collateral exam | 100 | |||
| Meniscal Exam | 100 | |||
| ROM | 100 | |||
| Ligamentous Laxity | 100 | |||
| Effusion | 100 | |||
| 13M | Lachmann | 100 | 67% | Effusion |
| Pivot-shift | 100 | |||
| Collateral exam | 100 | |||
| Meniscal Exam | 100 | |||
| ROM | 100 | |||
| Ligamentous Laxity | 100 |
| Vignette | Modal Response | Agreement | Consensus | Disagreement Sources |
|---|---|---|---|---|
| (a) | ||||
| 9F | Flexion | 83 | 67% | |
| Standing AP | 100 | |||
| Lateral | 100 | |||
| Long-leg Alignment | 92 | |||
| Bone Age Wrist Films | 83 | |||
| 10M | Flexion | 83 | 67% | |
| Standing AP | 100 | |||
| Lateral | 100 | |||
| Long-leg Alignment | 92 | |||
| Bone Age Wrist Films | 83 | |||
| 12F | Flexion | 93 | 67% | |
| Standing AP | 100 | |||
| Lateral | 100 | |||
| Long-leg Alignment | 92 | |||
| Bone Age Wrist Films | 92 | |||
| 13M | Flexion | 83 | 67% | |
| Standing AP | 100 | |||
| Lateral | 100 | |||
| Long-leg Alignment | 92 | |||
| Bone Age Wrist Films | 92 | |||
| (b) | ||||
| 9F | Tibial Slope | 100 | 67% | |
| 10M | Tibial Slope | 100 | 67% | Mechanical Axis Alignment |
| Physeal Status | 100 | |||
| 12F | Tibial Slope | 100 | 75% | |
| 13M | Tibial Slope | 100 | 67% | Mechanical Axis Alignment |
| Physeal Status | 100 | |||
| Diagnostic Evaluation Technique | 9F | 10M | 12F | 13M | All |
|---|---|---|---|---|---|
| Patient History | |||||
| Injury History | * | * | * | * | * |
| Family History | * | * | # | * | * |
| Sports Participation | * | * | * | * | * |
| Current Symptoms | * | * | * | * | * |
| Menarche | * | * | |||
| Physical Exam | |||||
| Lachmann | * | * | * | * | * |
| Pivot-shift | * | * | * | * | * |
| Collateral Exam | * | * | * | * | * |
| Meniscal Exam | * | * | * | * | * |
| ROM | * | * | * | * | * |
| Ligamentous Laxity | * | * | * | * | * |
| Effusion | * | * | * | * | |
| Radiographic Sequence | |||||
| Flexion | * | * | * | * | * |
| Standing AP | * | * | * | * | * |
| Lateral | * | * | * | * | * |
| Long-leg Alignment | * | * | * | * | * |
| Bone Age Wrist Films | * | * | * | * | * |
| Radiographic Interpretation | |||||
| Tibial Slope | * | * | * | * | * |
| Physeal Status | * | * | * | ||
| Mechanical alignment/leg lengths | # | # | # | # | * |
| Skeletal age | # | # | # | # | * |
| Cross-Sectional Imaging | |||||
| MRI | * | * | * | * | * |
| Cross-Sectional Measurement | |||||
| None | * | * | * | * | * |
| Ancillary Studies | |||||
| None | * | * | * | * | * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seabol, L.; Boden, S.; Herman, M.; Ruh, E.; Kocher, M.; McClincy, M. Towards Standardization in the Diagnostic Evaluation of ACL Injuries in Skeletally Immature Patients. Int. J. Environ. Res. Public Health 2021, 18, 2684. https://doi.org/10.3390/ijerph18052684
Seabol L, Boden S, Herman M, Ruh E, Kocher M, McClincy M. Towards Standardization in the Diagnostic Evaluation of ACL Injuries in Skeletally Immature Patients. International Journal of Environmental Research and Public Health. 2021; 18(5):2684. https://doi.org/10.3390/ijerph18052684
Chicago/Turabian StyleSeabol, Liliana, Stephanie Boden, Max Herman, Ethan Ruh, Mininder Kocher, and Michael McClincy. 2021. "Towards Standardization in the Diagnostic Evaluation of ACL Injuries in Skeletally Immature Patients" International Journal of Environmental Research and Public Health 18, no. 5: 2684. https://doi.org/10.3390/ijerph18052684






