Lean Six Sigma Approach for Reducing Length of Hospital Stay for Patients with Femur Fracture in a University Hospital
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
- Gender (male/female);
- Age (65 ≤ Age ≤ 75; 75 < Age ≤ 90; >90)
- Date and time of admission;
- Date and time of surgery;
- Date and time of discharge;
- Hypertension (Yes; No);
- Diabetes (Yes; No);
- Cardiovascular diseases (Yes; No);
- Respiratory diseases (Yes; No);
- Kidney diseases (Yes; No);
- Anaemia (Yes; No);
- Bleeding during surgery (Yes; No).
2.2. DMAIC Cycle
2.2.1. Define
- Project title: LSS approach to reduce preoperative LOS through a Diagnostic-Therapeutic-Assistance Path at “San Giovanni di Dio e Ruggi d’Aragona” University Hospital.
- Question: inappropriate prolongation of preoperative LOS.
- CTQ: preoperative LOS, measured in days.
- Target: Realize corrective measures in order to reduce the CTQ increase the percentage of people undergoing surgery within 48 h of admission.
- Deliverables: increase in admissions and decrease in LOS, improvements in patients’ outcome.
- Timeline:
- Define: January–February 2016.
- Measure: March–April 2016.
- Analyze: May–August 2016.
- Improve: September 2016.
- Control: October 2016–June 2020.
- In scope: femur surgery. Complex Operative Unit (C.O.U.) of Orthopedic and Traumatology at the “San Giovanni di Dio e Ruggi d’Aragona” University Hospital of Salerno.
- Out of scope: all other structures and interventions.
- Financial: no funding was provided to chase the target.
- Business need: creation of a pathway making it possible to speed up the surgery process.
- In addition, a SIPOC (Supplier, Input, Process, Output, Customer) scheme was built to clarify the main process characteristics and the scope of the project.
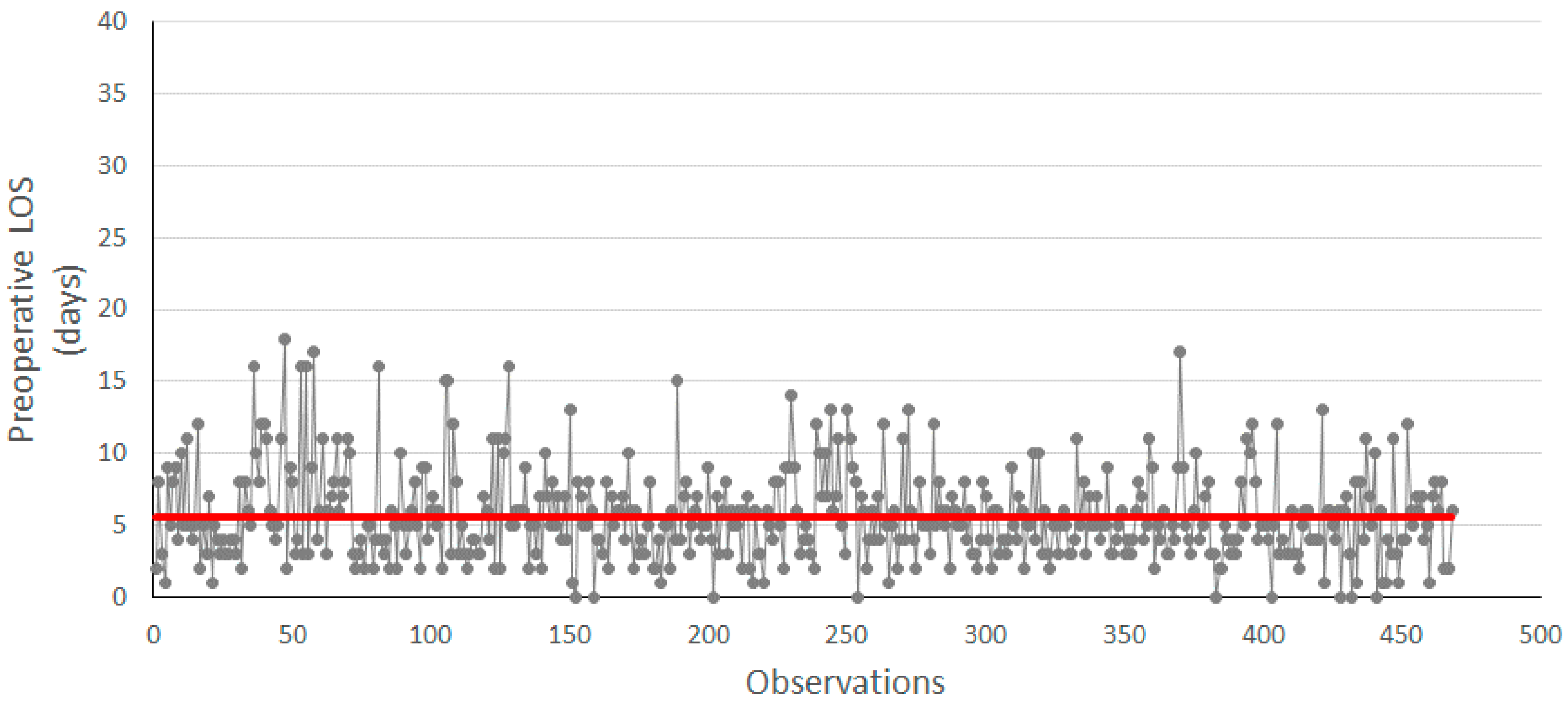
2.2.2. Measure
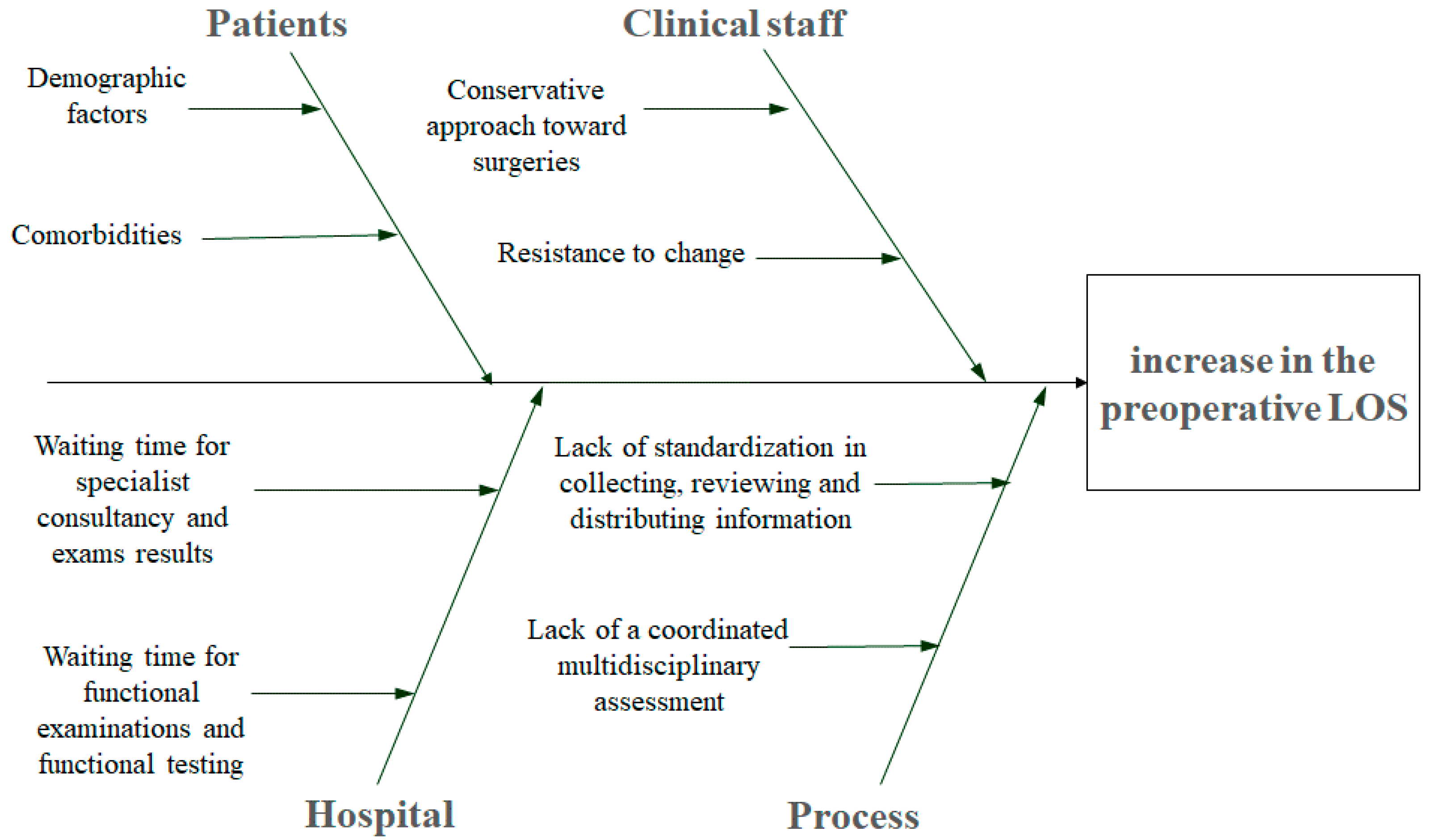
2.2.3. Analyze
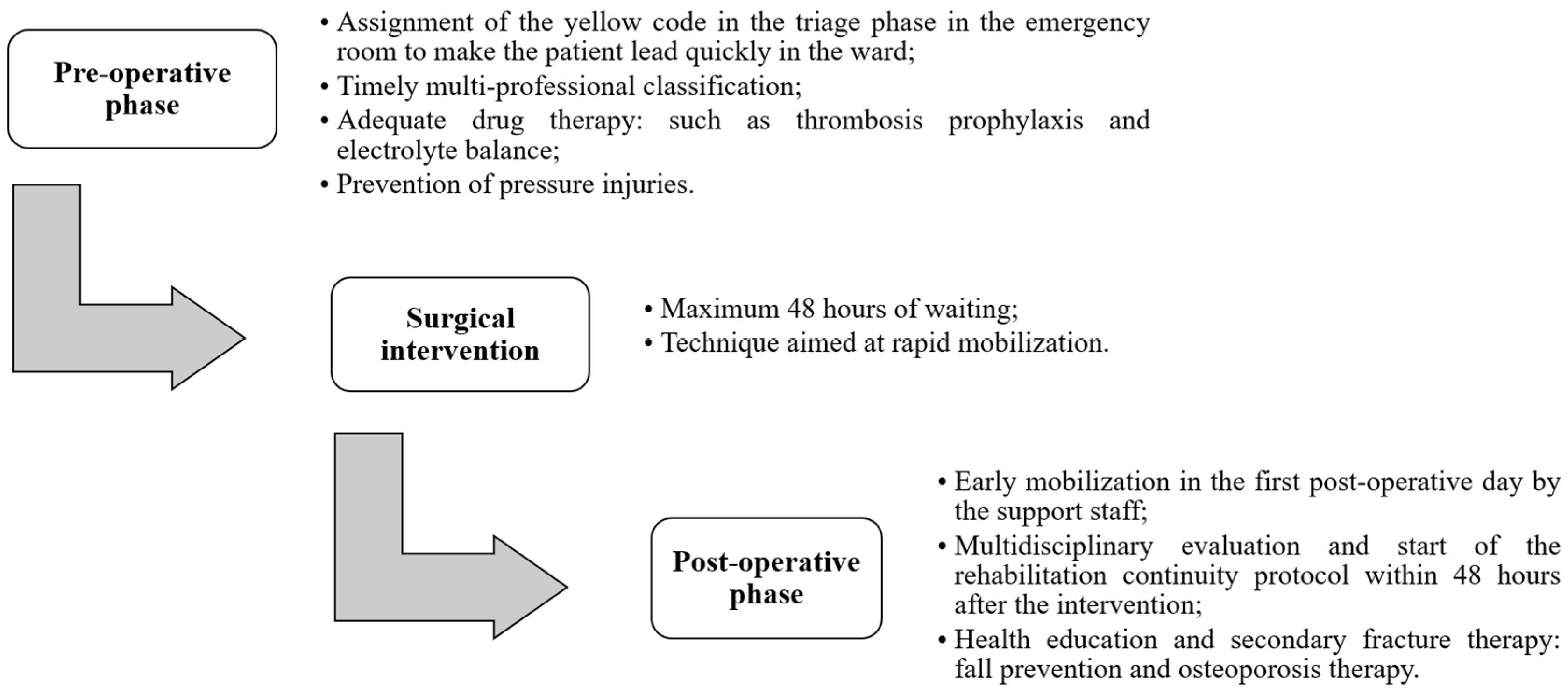
2.2.4. Improve
2.2.5. Control
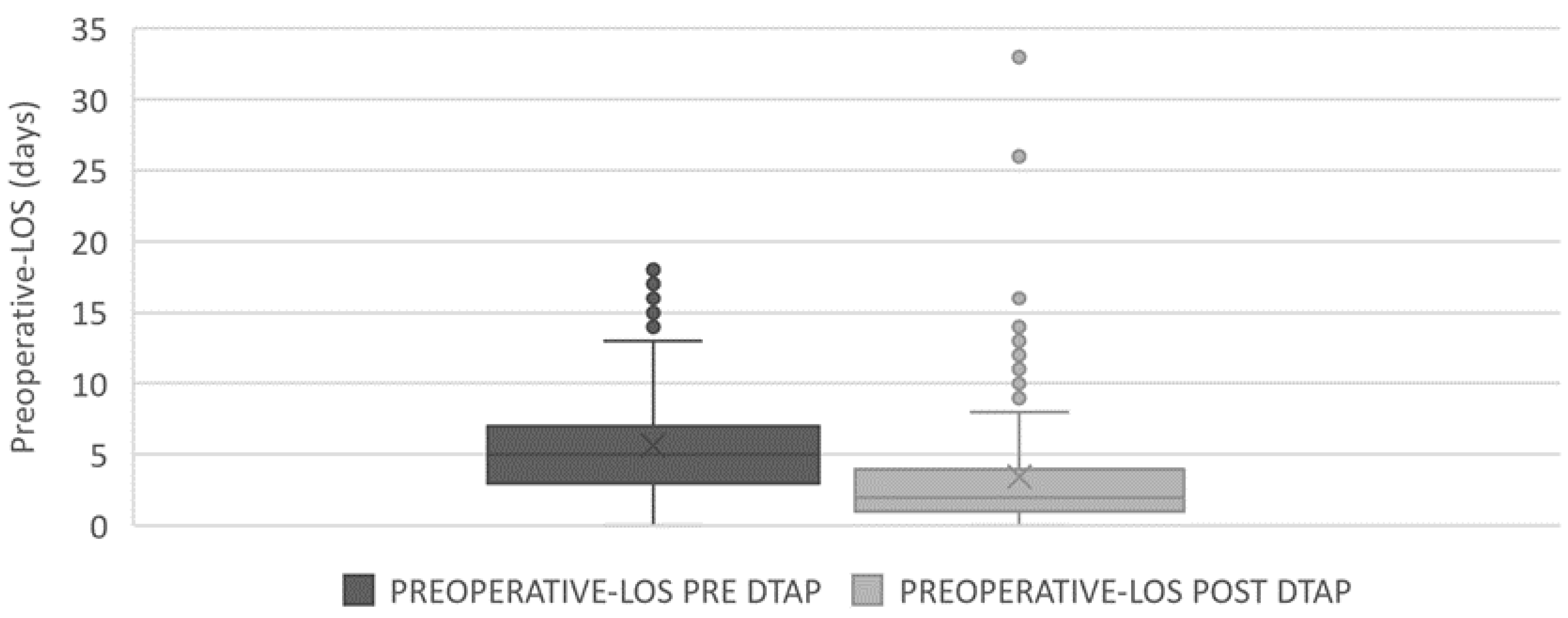
3. Results and Discussion
- Assignment of the yellow code in the triage phase;
- Clinical evaluation and physical examination by the emergency room doctor;
- Execution of instrumental tests as required (X-ray);
- Hospitalization if femur fracture is confirmed;
- Performing routine blood chemistry, CBC (cell blood count), D-dimer, chest, hip and lower limb X-ray, ECG;
- Orthopedic, cardiological, pneumological, geriatric and internist consultancies;
- Execution of additional instrumental tests as required by consultancy;
- Drug therapy, such as thrombosis prophylaxis and electrolyte balance
- Clinical anesthetic evaluation.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rossini, M.; Piscitelli, P.; Fitto, F.; Camboa, P.; Angeli, A.; Guida, G.; Adami, S. Incidence and socioeconomic burden of hip fractures in Italy. Reumatismo 2005, 57, 97–102. [Google Scholar] [CrossRef]
- Kim, S.-M.; Yeom, J.-W.; Song, H.K.; Hwang, K.-T.; Hwang, J.-H.; Yoo, J.-H. Lateral Locked Plating for Distal Femur Fractures by Low-Energy Trauma: What Makes a Difference in Healing? Int. Orthop. 2018, 42, 2907–2914. [Google Scholar] [CrossRef]
- Johnell, O. The Socioeconomic Burden of Fractures: Today and in the 21st Century. Am. J. Med. 1997, 103, S20–S26. [Google Scholar] [CrossRef]
- Lippuner, K.; von Overbeck, J.; Perrelet, R.; Bosshard, H.; Jaeger, P. Incidence and Direct Medical Costs of Hospitalizations Due to Osteoporotic Fractures in Switzerland. Osteoporos. Int. 1997, 7, 414–425. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.-P.; Fu, T.-S.; Lin, Y.-C.; Fan, C.-M. Risk Factors and Quality of Life for the Occurrence of Hip Fracture in Postmenopausal Women. Biomed. J. 2018, 41, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Nyholm, A.M.; Gromov, K.; Palm, H.; Brix, M.; Kallemose, T.; Troelsen, A. Danish Fracture Database Collaborators. Time to Surgery Is Associated with Thirty-Day and Ninety-Day Mortality After Proximal Femoral Fracture: A Retrospective Observational Study on Prospectively Collected Data from the Danish Fracture Database Collaborators. J. Bone Joint Surg. Am. 2015, 97, 1333–1339. [Google Scholar] [CrossRef] [PubMed]
- Italian Ministry of Health. National Agency for Regional Health Services (AGENAS). PNE Programma Nazionale Esiti—Edizione 2020; Italian Ministry of Health: Rome, Italy, 2020.
- Ricciardi, C.; Ponsiglione, A.M.; Converso, G.; Santalucia, I.; Triassi, M.; Improta, G. Implementation and Validation of a New Method to Model Voluntary Departures from Emergency Departments. Math. Biosci. Eng. 2021, 18, 253–273. [Google Scholar] [CrossRef]
- Trunfio, T.A.; Scala, A.; Vecchia, A.D.; Marra, A.; Borrelli, A. Multiple Regression Model to Predict Length of Hospital Stay for Patients Undergoing Femur Fracture Surgery at “San Giovanni Di Dio e Ruggi d’Aragona” University Hospital. In Proceedings of the 8th European Medical and Biological Engineering Conference, 8th European Medical and Biological Engineering Conference, Portorož, Slovenia, 29 November 2020–3 December 2020; Jarm, T., Cvetkoska, A., Mahnič-Kalamiza, S., Miklavcic, D., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 840–847. [Google Scholar]
- Robinson, S.; Radnor, Z.J.; Burgess, N.; Worthington, C. SimLean: Utilising Simulation in the Implementation of Lean in Healthcare. Eur. J. Oper. Res. 2012, 219, 188–197. [Google Scholar] [CrossRef]
- Rutberg, M.H.; Wenczel, S.; Devaney, J.; Goldlust, E.J.; Day, T.E. Incorporating Discrete Event Simulation Into Quality Improvement Efforts in Health Care Systems. Am. J. Med. Qual. 2015, 30, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Simon, R.W.; Canacari, E.G. A Practical Guide to Applying Lean Tools and Management Principles to Health Care Improvement Projects. AORN J. 2012, 95, 85–103. [Google Scholar] [CrossRef]
- Mosadeghrad, A.M. Developing and Validating a Total Quality Management Model for Healthcare Organisations. TQM J. 2015, 27, 544–564. [Google Scholar] [CrossRef]
- Improta, G.; Ponsiglione, A.M.; Parente, G.; Romano, M.; Cesarelli, G.; Rea, T.; Russo, M.; Triassi, M. Evaluation of Medical Training Courses Satisfaction: Qualitative Analysis and Analytic Hierarchy Process. In Proceedings of the 8th European Medical and Biological Engineering Conference, Portorož, Slovenia, 29 November 2020–3 December 2020; Jarm, T., Cvetkoska, A., Mahnič-Kalamiza, S., Miklavcic, D., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 518–526. [Google Scholar]
- Glickman, S.W.; Baggett, K.A.; Krubert, C.G.; Peterson, E.D.; Schulman, K.A. Promoting Quality: The Health-Care Organization from a Management Perspective. Int. J. Qual. Health Care 2007, 19, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Bevan, H. Lean Six Sigma: Some Basic Concepts; NHS Institute for Innovation and Improvement: Coventry, UK, 2006. [Google Scholar]
- Young, T.; McClean, S. Some Challenges Facing Lean Thinking in Healthcare. Int. J. Qual. Health Care 2009, 21, 309–310. [Google Scholar] [CrossRef]
- Joosten, T.; Bongers, I.; Janssen, R. Application of Lean Thinking to Health Care: Issues and Observations. Int. J. Qual. Health Care 2009, 21, 341–347. [Google Scholar] [CrossRef]
- Improta, G.; Guizzi, G.; Ricciardi, C.; Giordano, V.; Ponsiglione, A.M.; Converso, G.; Triassi, M. Agile Six Sigma in Healthcare: Case Study at Santobono Pediatric Hospital. Int. J. Environ. Res. Public. Health 2020, 17, 1052. [Google Scholar] [CrossRef]
- Sorrentino, A.; Scala, A.; Fiorillo, A.; Latessa, I.; Abbate, V.; Dell’Aversana Orabona, G. Six Sigma Approach for a First Evaluation of a Pharmacological Therapy in Tongue Cancer. In Proceedings of the 8th European Medical and Biological Engineering Conference, Portorož, Slovenia, 29 November 2020–3 December 2020; Jarm, T., Cvetkoska, A., Mahnič-Kalamiza, S., Miklavcic, D., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 1028–1037. [Google Scholar]
- Improta, G.; Cesarelli, M.; Montuori, P.; Santillo, L.C.; Triassi, M. Reducing the Risk of Healthcare-Associated Infections through Lean Six Sigma: The Case of the Medicine Areas at the Federico II University Hospital in Naples (Italy). J. Eval. Clin. Pract. 2018, 24, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Trakulsunti, Y.; Antony, J. Can Lean Six Sigma Be Used to Reduce Medication Errors in the Health-Care Sector? Leadersh. Health Serv. 2018, 31, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Antony, J.; Forthun, S.C.; Trakulsunti, Y.; Farrington, T.; McFarlane, J.; Brennan, A.; Dempsey, M. An Exploratory Study into the Use of Lean Six Sigma to Reduce Medication Errors in the Norwegian Public Healthcare Context. Leadersh. Health Serv. Bradf. Engl. 2019, 32, 509–524. [Google Scholar] [CrossRef]
- George, A. Application of Six Sigma DMAIC Methodology to Reduce Medication Errors in a Major Trauma Care Centre in India. Indian J. Pharm. Pract. 2018, 11, 182–187. [Google Scholar] [CrossRef]
- Mahesh, B.P.; Soragaon, B.; Annigeri, A.R. Reduction of Patient Wait Time at a Multi-Specialty Hospital Using DMAIC Methodology and Factor Analysis. Int. J. Eng. Technol. 2018, 7, 309–312. [Google Scholar] [CrossRef]
- Sayeed, Z.; Anoushiravani, A.; El-Othmani, M.; Barinaga, G.; Sayeed, Y.; Cagle, P.; Saleh, K.J. Implementation of a Hip Fracture Care Pathway Using Lean Six Sigma Methodology in a Level I Trauma Center. J. Am. Acad. Orthop. Surg. 2018, 26, 881–893. [Google Scholar] [CrossRef]
- Ricciardi, C.; Balato, G.; Romano, M.; Santalucia, I.; Cesarelli, M.; Improta, G. Fast Track Surgery for Knee Replacement Surgery: A Lean Six Sigma Approach. TQM J. 2020, 32, 461–474. [Google Scholar] [CrossRef]
- Improta, G.; Balato, G.; Romano, M.; Ponsiglione, A.M.; Raiola, E.; Russo, M.A.; Cuccaro, P.; Santillo, L.C.; Cesarelli, M. Improving Performances of the Knee Replacement Surgery Process by Applying DMAIC Principles. J. Eval. Clin. Pract. 2017, 23, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- McNamara, R.; Butler, A.; Baker, C.; Mullen, J.; Lenehan, B.; Grimes, S.; O’Donoghue, H.; Evans, P.; Liston, M.; Cummins, F.; et al. Use of Lean Principals to Improve Flow of Patients with Fractured Neck of Femur--the HOPE Study. Ir. Med. J. 2014, 107, 70–72. [Google Scholar] [PubMed]
- Improta, G.; Ricciardi, C.; Borrelli, A.; D’alessandro, A.; Verdoliva, C.; Cesarelli, M. The Application of Six Sigma to Reduce the Pre-Operative Length of Hospital Stay at the Hospital Antonio Cardarelli. Int. J. Lean Six Sigma 2019, 11, 555–576. [Google Scholar] [CrossRef]
- Ricciardi, C.; Fiorillo, A.; Valente, A.S.; Borrelli, A.; Verdoliva, C.; Triassi, M.; Improta, G. Lean Six Sigma Approach to Reduce LOS through a Diagnostic-Therapeutic-Assistance Path at A.O.R.N. A. Cardarelli. TQM J. 2019, 31, 657–672. [Google Scholar] [CrossRef]
- Scala, A.; Trunfio, T.A.; Vecchia, A.D.; Marra, A.; Borrelli, A. Lean Six Sigma Approach to Implement a Femur Fracture Care Pathway at “San Giovanni Di Dio e Ruggi d’Aragona” University Hospital. In Proceedings of the 8th European Medical and Biological Engineering Conference, Portorož, Slovenia, 29 November 2020–3 December 2020; Jarm, T., Cvetkoska, A., Mahnič-Kalamiza, S., Miklavcic, D., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 740–749. [Google Scholar]
- Rao, N.; Toussaint, N.D. Hip Fractures in Patients with Chronic Kidney Disease Admitted to Victorian Hospitals. Intern. Med. J. 2019, 49, 658–661. [Google Scholar] [CrossRef]
- Frisch, N.B.; Wessell, N.; Jildeh, T.R.; Greenstein, A.; Trent Guthrie, S. Early-Stage Chronic Kidney Disease and Hip Fracture Mortality. J. Surg. Orthop. Adv. 2018, 27, 226–230. [Google Scholar] [PubMed]
- Yoon, B.-H.; Koo, K.-H. Hip Fracture in Chronic Kidney Disease Patients: Necessity of Multidisciplinary Approach. J. Korean Med. Sci. 2017, 32, 1906–1907. [Google Scholar] [CrossRef]
- Dong, C.; Wang, Y.; Wang, Z.; Wang, Y.; Wu, S.; Du, Q.; Wang, A. Damage Control Orthopedics Management as Vital Procedure in Elderly Patients with Femoral Neck Fractures Complicated with Chronic Renal Failure: A Retrospective Cohort Study. PLoS ONE 2016, 11, e0154906. [Google Scholar] [CrossRef]
- Decree of the Italian Ministry of Health (DM 12 Marzo 2019). Nuovo Sistema Di Garanzia per Il Monitoraggio Dell’assistenza Sanitaria; Italian Ministry of Health: Rome, Italy, 2019.
- Vanhaecht, K.; Sermeus, W.; Peers, J.; Lodewijckx, C.; Deneckere, S.; Leigheb, F.; Boonen, S.; Sermon, A.; Boto, P.; Mendes, R.V.; et al. The Impact of Care Pathways for Patients with Proximal Femur Fracture: Rationale and Design of a Cluster-Randomized Controlled Trial. BMC Health Serv. Res. 2012, 12, 124. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, C. Applying Quality Improvement Tools to Quality Planning: Pediatric Femur Fracture Clinical Path Development. J. Healthc. Qual. 1994, 16, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Kosy, J.D.; Blackshaw, R.; Swart, M.; Fordyce, A.; Lofthouse, R.A. Fractured Neck of Femur Patient Care Improved by Simulated Fast-Track System. J. Orthop. Traumatol. 2013, 14, 165–170. [Google Scholar] [CrossRef] [PubMed]

| Supplier | Input | Process | Output | Customer |
|---|---|---|---|---|
| Complex Operative Unit (C.O.U.) of Orthopedic and Traumatology | Surgical and medical services | Care process | Faster time of intervention; | Patients; |
| Improved outcome for patients. | “San Giovanni di Dio e Ruggi d’Aragona” University Hospital of Salerno. |
| Variable | Category | N | Preoperative LOS [Mean ± dev std] | p-Value |
|---|---|---|---|---|
| All | All | 468 | 5.62 ± 3.24 | - |
| Gender | Man | 138 | 5.70 ± 2.86 | 0.281 |
| Women | 330 | 5.59 ± 3.39 | ||
| Age | 65 ≤ Age ≤ 75 | 94 | 6.34 ± 3.93 | 0.293 |
| 75 < Age ≤ 90 | 323 | 5.51 ± 3.00 | ||
| >90 | 51 | 5.000 ± 3.14 | ||
| Hypertension | No | 369 | 5.82 ± 3.34 | 0.021 |
| Yes | 99 | 4.89 ± 2.71 | ||
| Diabetes | No | 399 | 5.65 ± 3.20 | 0.302 |
| Yes | 69 | 5.48 ± 3.48 | ||
| Cardiovascular disease | No | 304 | 5.98 ± 3.31 | 0.0004 |
| Yes | 164 | 4.96 ± 3.00 | ||
| Respiratory disease | No | 428 | 5.63 ± 3.28 | 0.741 |
| Yes | 40 | 5.600 ± 2.77 | ||
| Kidney disease | No | 444 | 5.670 ± 3.26 | 0.219 |
| Yes | 24 | 4.750 ± 2.66 | ||
| Anemia | No | 337 | 5.740 ± 3.34 | 0.395 |
| Yes | 131 | 5.320 ± 2.954 | ||
| Bleeding during surgery | No | 347 | 5.100 ± 2.944 | <0.0001 |
| Yes | 121 | 7.120 ± 3.583 |
| Variable | Category | LOS Pre-DTAP [Mean ± dev std] | LOS Post-DTAP [Mean ± dev std] | Mean Difference [%] | p-Value |
|---|---|---|---|---|---|
| All | All | 5.62 ± 3.24 | 3.45 ± 3.59 | −39% | <0.0001 |
| Gender | Man | 5.70 ± 2.86 | 3.87 ± 4.38 | −32.1% | <0.0001 |
| Women | 5.59 ± 3.39 | 3.32 ± 3.32 | −40.6% | <0.0001 | |
| Age | 65 ≤ Age ≤ 75 | 6.34 ± 3.93 | 4.39 ± 5.51 | −30.8% | <0.0001 |
| 75 < Age ≤ 90 | 5.51 ± 3.00 | 3.31 ± 3.04 | −39.9% | <0.0001 | |
| >90 | 5.00 ± 3.14 | 2.89 ± 2.56 | −42.2% | 0.0002 | |
| Hypertension | No | 5.82 ± 3.34 | 3.78 ± 3.98 | −35.1% | <0.0001 |
| Yes | 4.89 ± 2.71 | 2.94 ± 2.87 | −39.9% | <0.0001 | |
| Diabetes | No | 5.65 ± 3.20 | 3.62 ± 3.84 | −35.9% | <0.0001 |
| Yes | 5.48 ± 3.48 | 2.58 ± 1.75 | −52.9% | <0.0001 | |
| Cardiovascular disease | No | 5.98 ± 3.31 | 3.61 ± 3.51 | −39.6% | <0.0001 |
| Yes | 4.96 ± 3.00 | 3.12 ± 3.78 | −37.1% | <0.0001 | |
| Respiratory disease | No | 5.63 ± 3.28 | 3.47 ± 3.66 | −38.4% | <0.0001 |
| Yes | 5.60 ± 2.77 | 3.24 ± 3.03 | −42.1% | 0.0005 | |
| Kidney disease | No | 5.67 ± 3.26 | 3.40 ± 3.58 | −40% | <0.0001 |
| Yes | 4.75 ± 2.66 | 4.53 ± 3.91 | −4.63% | 0.391 | |
| Anemia | No | 5.74 ± 3.34 | 3.97 ± 4.15 | −30.8% | <0.0001 |
| Yes | 5.32 ± 2.95 | 2.80 ± 2.64 | −47.4% | <0.0001 | |
| Bleeding during surgery | No | 5.10 ± 2.94 | 2.95 ± 3.19 | −42.2% | <0.0001 |
| Yes | 7.12 ± 3.58 | 6.65 ± 4.42 | −6.60% | 0.569 |
| Mean Preoperative LOS before DTAP [Days] | Mean Preoperative LOS after DTAP [days] | Difference in Preoperative LOS [%] | Settings | Reference |
|---|---|---|---|---|
| 5.62 | 3.45 | −39% | University Hospital “San Giovanni di Dio e Ruggi d’Aragona” of Salerno (Italy) | this study |
| 6.90 | 3.15 | −54% | Hospital A.O.R.N. “A. Cardarelli” of Naples (Italy) | [23] |
| not reported | not reported | not reported | British Orthopaedic Association (UK) | [24] |
| 2.00 | 1.00 | −50% | Children’s Hospital, San Diego | [28] |
| 1.87 | 1.22 | −35% | Hospital in South West England (UK) | [29] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scala, A.; Ponsiglione, A.M.; Loperto, I.; Della Vecchia, A.; Borrelli, A.; Russo, G.; Triassi, M.; Improta, G. Lean Six Sigma Approach for Reducing Length of Hospital Stay for Patients with Femur Fracture in a University Hospital. Int. J. Environ. Res. Public Health 2021, 18, 2843. https://doi.org/10.3390/ijerph18062843
Scala A, Ponsiglione AM, Loperto I, Della Vecchia A, Borrelli A, Russo G, Triassi M, Improta G. Lean Six Sigma Approach for Reducing Length of Hospital Stay for Patients with Femur Fracture in a University Hospital. International Journal of Environmental Research and Public Health. 2021; 18(6):2843. https://doi.org/10.3390/ijerph18062843
Chicago/Turabian StyleScala, Arianna, Alfonso Maria Ponsiglione, Ilaria Loperto, Antonio Della Vecchia, Anna Borrelli, Giuseppe Russo, Maria Triassi, and Giovanni Improta. 2021. "Lean Six Sigma Approach for Reducing Length of Hospital Stay for Patients with Femur Fracture in a University Hospital" International Journal of Environmental Research and Public Health 18, no. 6: 2843. https://doi.org/10.3390/ijerph18062843
APA StyleScala, A., Ponsiglione, A. M., Loperto, I., Della Vecchia, A., Borrelli, A., Russo, G., Triassi, M., & Improta, G. (2021). Lean Six Sigma Approach for Reducing Length of Hospital Stay for Patients with Femur Fracture in a University Hospital. International Journal of Environmental Research and Public Health, 18(6), 2843. https://doi.org/10.3390/ijerph18062843









