The Association between Blood Pressure Trajectories and Risk of Cardiovascular Diseases among Non-Hypertensive Chinese Population: A Population-Based Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
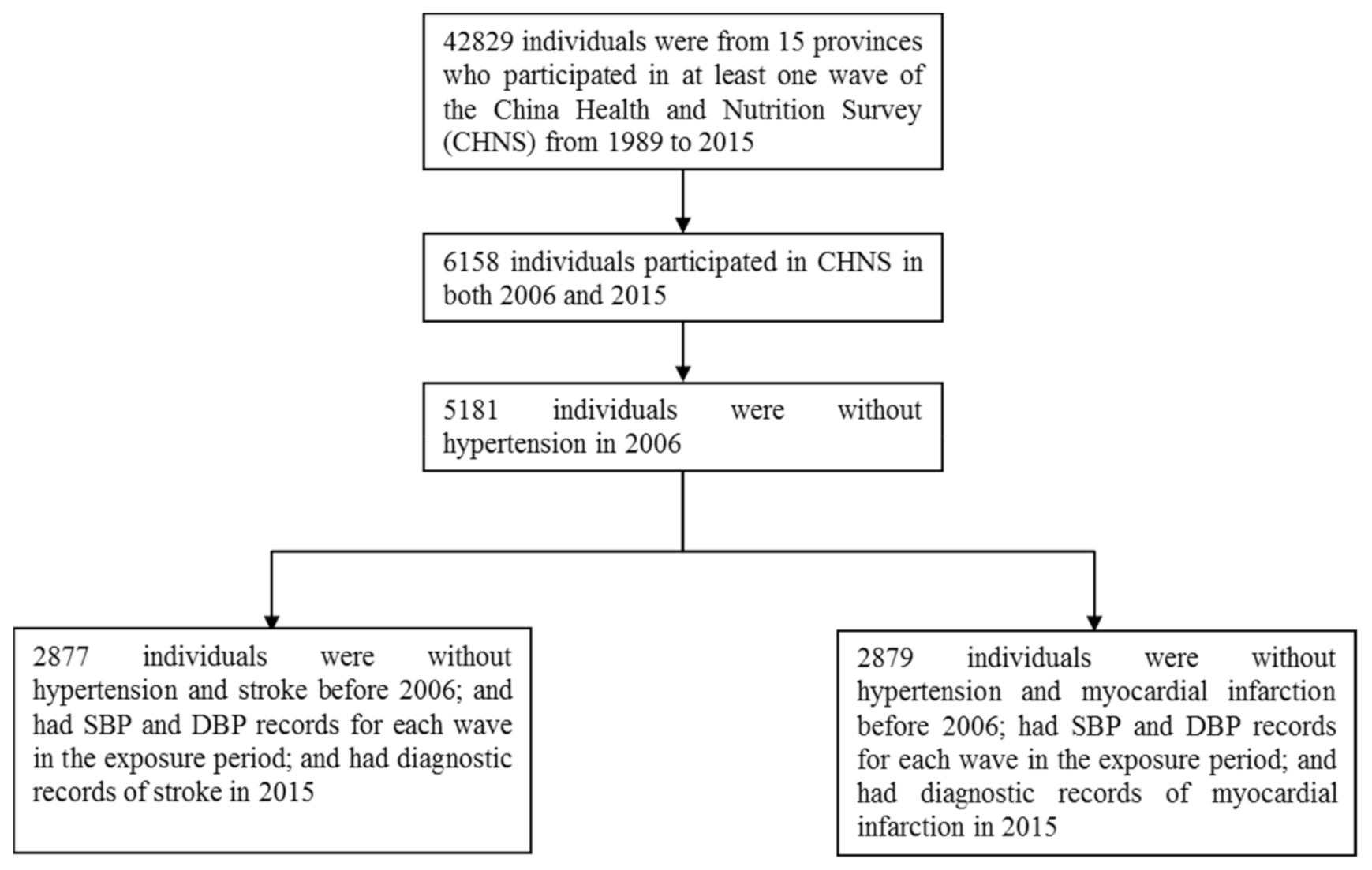
2.1. Study Design and Population
2.2. Ethical Approval
2.3. Data Collection
2.3.1. Main Outcomes
2.3.2. Covariates
2.4. Statistical Analyses
2.5. Sensitivity Analyses
3. Results
3.1. Descriptive Analysis
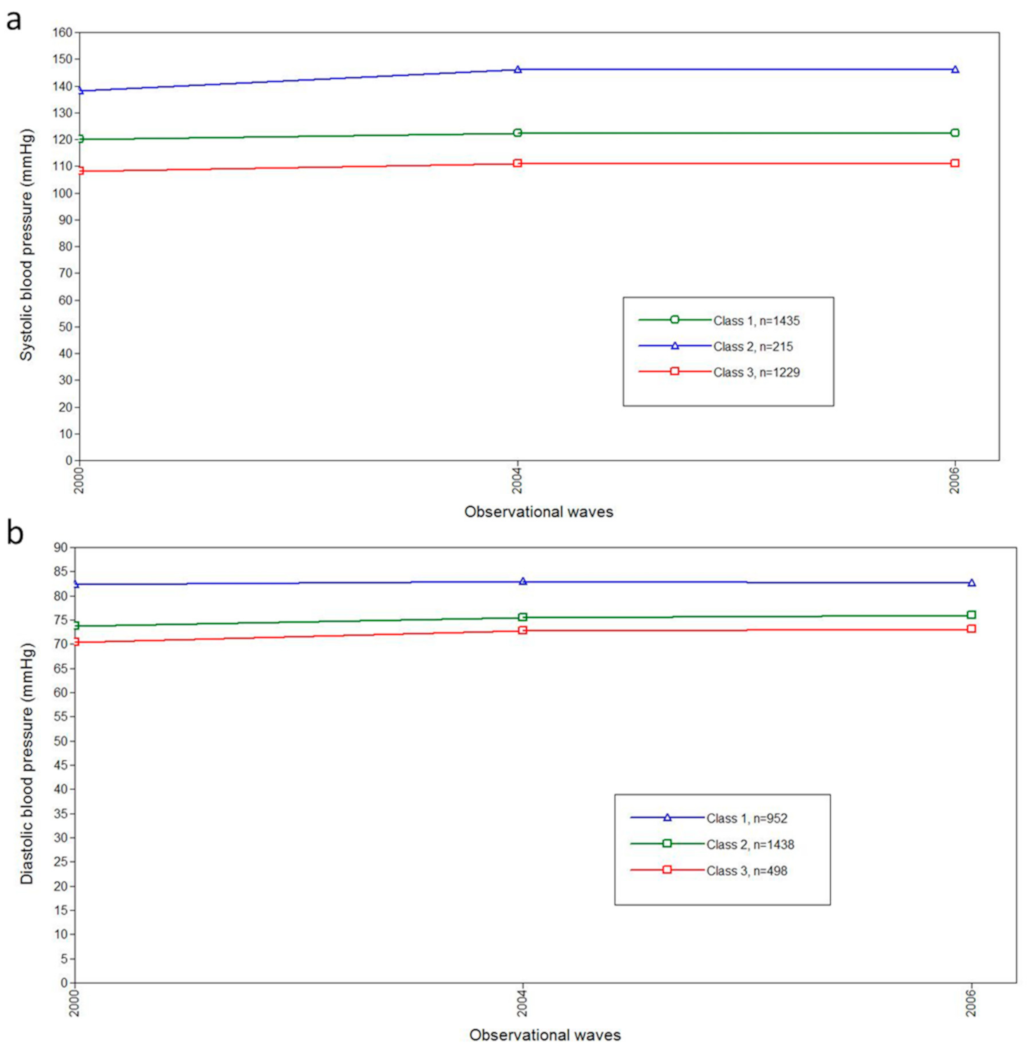
3.2. GMM for Blood Pressure
3.3. Characteristics across Trajectory Groups
3.4. Cox Regression Analyses for Stroke and MI
3.5. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wendelboe, A.M.; Raskob, G.E. Global Burden of Thrombosis: Epidemiologic Aspects. Circ. Res. 2016, 118, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Collaborators, G.S. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar]
- Noncommunicable Diseases. Available online: https://www.who.int/health-topics/noncommunicable-diseases#tab=tab_1 (accessed on 9 November 2020).
- Gippsland Disabiltiy Advocacy Inc. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef] [Green Version]
- Yu, D.; Huang, J.; Hu, D.; Chen, J.; Cao, J.; Li, J.; Gu, D. Prevalence and risk factors of prehypertension among Chinese adults. J. Cardiovasc. Pharm. 2008, 52, 363–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erbel, R.; Lehmann, N.; Möhlenkamp, S.; Churzidse, S.; Bauer, M.; Kälsch, H.; Schmermund, A.; Moebus, S.; Stang, A.; Roggenbuck, U.; et al. Subclinical coronary atherosclerosis predicts cardiovascular risk in different stages of hypertension: Result of the Heinz Nixdorf Recall Study. Hypertension 2012, 59, 44–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukuhara, M.; Arima, H.; Ninomiya, T.; Hata, J.; Yonemoto, K.; Doi, Y.; Hirakawa, Y.; Matsumura, K.; Kitazono, T.; Kiyohara, Y. Impact of lower range of prehypertension on cardiovascular events in a general population: The Hisayama Study. J. Hypertens. 2012, 30, 893–900. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.M.; Park, H.S.; Han, J.H.; Lee, J.S.; Lee, J.; Ryu, O.H.; Lee, K.W.; Cho, K.H.; Yoon, D.; Baik, S.H.; et al. Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J. Hypertens. 2006, 24, 1515–1521. [Google Scholar] [CrossRef] [PubMed]
- Janghorbani, M.; Amini, M.; Gouya, M.M.; Delavari, A.; Alikhani, S.; Mahdavi, A. Nationwide survey of prevalence and risk factors of prehypertension and hypertension in Iranian adults. J. Hypertens. 2008, 26, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Wu, Z.; Liu, J.; Wang, W.; Zhao, D.; Ceng, Z.; Wang, W.; Liu, J.; Qin, L.; Liu, S. Impact of high-normal blood pressure on risk of cardiocerebrovascular disease in 11 provinces in China. Zhonghua Yi Xue Za Zhi 2002, 82, 1083–1085. [Google Scholar]
- Gu, D.; Chen, J.; Wu, X.; Duan, X.; Jones, D.W.; Huang, J.F.; Chen, C.S.; Chen, J.C.; Kelly, T.N.; Whelton, P.K.; et al. Prehypertension and risk of cardiovascular disease in Chinese adults. J. Hypertens. 2009, 27, 721–729. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, Z.; Zhang, L.; Wang, X.; Hao, G.; Zhang, Z.; Shao, L.; Tian, Y.; Dong, Y.; Zheng, C.; et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation 2018, 137, 2344–2356. [Google Scholar] [CrossRef]
- Vasan, R.S.; Larson, M.G.; Leip, E.P.; Kannel, W.B.; Levy, D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: A cohort study. Lancet 2001, 358, 1682–1686. [Google Scholar] [CrossRef]
- Egan, B.M.; Stevens-Fabry, S. Prehypertension--prevalence, health risks, and management strategies. Nat. Rev. Cardiol. 2015, 12, 289–300. [Google Scholar] [CrossRef] [PubMed]
- Vasan, R.S.; Larson, M.G.; Leip, E.P.; Evans, J.C.; O’Donnell, C.J.; Kannel, W.B.; Levy, D. Impact of high-normal blood pressure on the risk of cardiovascular disease. N. Engl. J. Med. 2001, 345, 1291–1297. [Google Scholar] [CrossRef]
- Han, M.; Li, Q.; Liu, L.; Zhang, D.; Ren, Y.; Zhao, Y.; Liu, D.; Liu, F.; Chen, X.; Cheng, C.; et al. Prehypertension and risk of cardiovascular diseases: A meta-analysis of 47 cohort studies. J. Hypertens. 2019, 37, 2325–2332. [Google Scholar] [CrossRef] [PubMed]
- Kalaitzidis, R.G.; Bakris, G.L. Prehypertension is it relevant for nephrologists? Kidney Int. 2010, 77, 194–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, K.H.; Henderson, V.W.; Stolwyk, R.J.; Dennerstein, L.; Szoeke, C. Prehypertension in midlife is associated with worse cognition a decade later in middle-aged and older women. Age Ageing 2015, 44, 439–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Menezes, S.T.; Giatti, L.; Brant, L.; Griep, R.H.; Schmidt, M.I.; Duncan, B.B.; Suemoto, C.K.; Ribeiro, A.; Barreto, S.M. Hypertension, Prehypertension, and Hypertension Control: Association With Decline in Cognitive Performance in the ELSA-Brasil Cohort. Hypertension 2021, 77, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Derakhshan, A.; Bagherzadeh-Khiabani, F.; Arshi, B.; Ramezankhani, A.; Azizi, F.; Hadaegh, F. Different Combinations of Glucose Tolerance and Blood Pressure Status and Incident Diabetes, Hypertension, and Chronic Kidney Disease. J. Am. Heart Assoc. 2016, 5, e003917. [Google Scholar] [CrossRef] [Green Version]
- Law, M.R.; Morris, J.K.; Wald, N.J. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009, 338, b1665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Das, S.; John, K.D.; Bokka, S.K.; Remmel, K.; Akça, O. Blood Pressure Management Following Large Vessel Occlusion Strokes: A Narrative Review. Balk. Med. J. 2020, 37, 253–259. [Google Scholar] [CrossRef]
- Li, C.; Zhang, Y.; Xu, T.; Peng, H.; Wang, D.; Xu, T.; Sun, Y.; Bu, X.; Chen, C.S.; Wang, A.; et al. Systolic Blood Pressure Trajectories in the Acute Phase and Clinical Outcomes in 2-Year Follow-up Among Patients With Ischemic Stroke. Am. J. Hypertens. 2019, 32, 317–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smitson, C.C.; Scherzer, R.; Shlipak, M.G.; Psaty, B.M.; Newman, A.B.; Sarnak, M.J.; Odden, M.C.; Peralta, C.A. Association of Blood Pressure Trajectory With Mortality, Incident Cardiovascular Disease, and Heart Failure in the Cardiovascular Health Study. Am. J. Hypertens. 2017, 30, 587–593. [Google Scholar] [CrossRef] [Green Version]
- Portegies, M.L.; Mirza, S.S.; Verlinden, V.J.; Hofman, A.; Koudstaal, P.J.; Swanson, S.A.; Ikram, M.A. Mid- to Late-Life Trajectories of Blood Pressure and the Risk of Stroke: The Rotterdam Study. Hypertension 2016, 67, 1126–1132. [Google Scholar] [CrossRef] [Green Version]
- Maddox, T.M.; Ross, C.; Tavel, H.M.; Lyons, E.E.; Tillquist, M.; Ho, P.M.; Rumsfeld, J.S.; Margolis, K.L.; O’Connor, P.J.; Selby, J.V.; et al. Blood pressure trajectories and associations with treatment intensification, medication adherence, and outcomes among newly diagnosed coronary artery disease patients. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 347–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fan, J.H.; Wang, J.B.; Wang, S.M.; Abnet, C.C.; Qiao, Y.L.; Taylor, P.R. Longitudinal change in blood pressure is associated with cardiovascular disease mortality in a Chinese cohort. Heart 2018, 104, 1764–1771. [Google Scholar] [CrossRef]
- Xu, Y.; Möller, J.; Wang, R.; Liang, Y. Life-course blood pressure trajectories and cardiovascular diseases: A population-based cohort study in China. PLoS ONE 2020, 15, e0240804. [Google Scholar] [CrossRef] [PubMed]
- China Health and Nutrition Survey. Available online: https://www.cpc.unc.edu/projects/china (accessed on 21 October 2020).
- Du, S.; Batis, C.; Wang, H.; Zhang, B.; Zhang, J.; Popkin, B.M. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am. J. Clin. Nutr. 2014, 99, 334–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, L. 2018 Chinese guidelines for the management of hypertension. Chin. J. Cardiovasc. Med. 2019, 24, 24–56. [Google Scholar]
- Working Group on Obesity in China. Guidelines on prevention and Control of Overweight and Obesity in Chinese Adults (Excerpts). Acta Nutr. Sin. 2004, 24, 1–4. [Google Scholar]
- Zhao, J.; Su, C.; Wang, H.; Wang, Z.; Wang, Y.; Zhang, B. Secular Trends in Energy and Macronutrient Intakes and Distribution among Adult Females (1991–2015): Results from the China Health and Nutrition Survey. Nutrients 2018, 10, 115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.J.; Carlin, J.B. Multiple imputation for missing data: Fully conditional specification versus multivariate normal imputation. Am. J. Epidemiol. 2010, 171, 624–632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spratt, M.; Carpenter, J.; Sterne, J.A.; Carlin, J.B.; Heron, J.; Henderson, J.; Tilling, K. Strategies for multiple imputation in longitudinal studies. Am. J. Epidemiol. 2010, 172, 478–487. [Google Scholar] [CrossRef]
- Dempster, A.P.; Laird, N.M.; Rubin, D.B. Maximum Likelihood from Incomplete Data via the EM Algorithm. J. R. Stat. Soc. Ser. B Methodol. 1977, 39, 1–38. [Google Scholar]
- Wu, S.; An, S.; Li, W.; Lichtenstein, A.H.; Gao, J.; Kris-Etherton, P.M.; Wu, Y.; Jin, C.; Huang, S.; Hu, F.B.; et al. Association of Trajectory of Cardiovascular Health Score and Incident Cardiovascular Disease. JAMA Netw. Open 2019, 2, e194758. [Google Scholar] [CrossRef] [Green Version]
- Hess, K.R. Graphical methods for assessing violations of the proportional hazards assumption in Cox regression. Stat. Med. 1995, 14, 1707–1723. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Jin, C.; Vaidya, A.; Wu, Y.; Rexrode, K.; Zheng, X.; Gurol, M.E.; Ma, C.; Wu, S.; Gao, X. Blood Pressure Trajectories and the Risk of Intracerebral Hemorrhage and Cerebral Infarction: A Prospective Study. Hypertension 2017, 70, 508–514. [Google Scholar] [CrossRef]
- Mattsson, M.; Maher, G.M.; Boland, F.; Fitzgerald, A.P.; Murray, D.M.; Biesma, R. Group-based trajectory modelling for BMI trajectories in childhood: A systematic review. Obes. Rev. 2019, 20, 998–1015. [Google Scholar] [CrossRef]
- Ames, M.E.; Wintre, M.G. Growth Mixture Modeling of Adolescent Body Mass Index Development: Longitudinal Patterns of Internalizing Symptoms and Physical Activity. J. Res. Adolesc. 2016, 26, 889–901. [Google Scholar] [CrossRef]
- Xian, H.; Scherrer, J.F.; Madden, P.A.; Lyons, M.J.; Tsuang, M.; True, W.R.; Eisen, S.A. Latent class typology of nicotine withdrawal: Genetic contributions and association with failed smoking cessation and psychiatric disorders. Psychol. Med. 2005, 35, 409–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lubke, G.; Muthén, B.O. Performance of Factor Mixture Models as a Function of Model Size, Covariate Effects, and Class-Specific Parameters. Struct. Equ. Modeling A Multidiscip. J. 2007, 14, 26–47. [Google Scholar] [CrossRef]
- Lo, Y.; Mendell, N.R.; Rubin, D.B. Testing the number of components in a normal mixture. Biometrika 2001, 88, 767–778. [Google Scholar] [CrossRef]
- Van der Nest, G.; Passos, V.L.; Candel, M.J.J.M.; van Breukelen, G.J.P. An overview of mixture modelling for latent evolutions in longitudinal data: Modelling approaches, fit statistics and software. Adv. Life Course Res. 2020, 43, 100323. [Google Scholar] [CrossRef]
- Gurven, M.; Blackwell, A.D.; Rodríguez, D.E.; Stieglitz, J.; Kaplan, H. Does blood pressure inevitably rise with age?: Longitudinal evidence among forager-horticulturalists. Hypertension 2012, 60, 25–33. [Google Scholar] [CrossRef] [Green Version]
- Wolf-Maier, K.; Cooper, R.S.; Banegas, J.R.; Giampaoli, S.; Hense, H.W.; Joffres, M.; Kastarinen, M.; Poulter, N.; Primatesta, P.; Rodríguez-Artalejo, F.; et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA 2003, 289, 2363–2369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franklin, S.S.; Gustin, W.T.; Wong, N.D.; Larson, M.G.; Weber, M.A.; Kannel, W.B.; Levy, D. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation 1997, 96, 308–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, L.; Hardy, R.; Kuh, D.; Power, C. Life-course body mass index trajectories and blood pressure in mid life in two British birth cohorts: Stronger associations in the later-born generation. Int. J. Epidemiol. 2015, 44, 1018–1026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.J.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.J.; et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA 2003, 289, 2560–2572. [Google Scholar] [CrossRef]
- Vidt, D.G. Angiotensin-receptor blockers for prehypertension. Curr. Hypertens. Rep. 2006, 8, 361–362. [Google Scholar] [CrossRef]
- Williams, S.A.; Michelson, E.L.; Cain, V.A.; Yang, M.; Nesbitt, S.D.; Egan, B.M.; Julius, S. An evaluation of the effects of an angiotensin receptor blocker on health-related quality of life in patients with high-normal blood pressure (prehypertension) in the Trial of Preventing Hypertension (TROPHY). J. Clin. Hypertens. Greenwich 2008, 10, 436–442. [Google Scholar] [CrossRef] [Green Version]
- Julius, S.; Nesbitt, S.D.; Egan, B.M.; Weber, M.A.; Michelson, E.L.; Kaciroti, N.; Black, H.R.; Grimm, R.J.; Messerli, F.H.; Oparil, S.; et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N. Engl. J. Med. 2006, 354, 1685–1697. [Google Scholar] [CrossRef]
- Shimizu, Y.; Kato, H.; Lin, C.H.; Kodama, K.; Peterson, A.V.; Prentice, R.L. Relationship between longitudinal changes in blood pressure and stroke incidence. Stroke 1984, 15, 839–846. [Google Scholar] [CrossRef] [Green Version]

| Variables | Dataset of Stroke (n = 2877) | Dataset of MI (n = 2879) | ||
|---|---|---|---|---|
| N | % | N | % | |
| Age group in 2006 | ||||
| ≤40 | 640 | 22.2 | 642 | 22.3 |
| 41–50 | 874 | 30.4 | 873 | 30.3 |
| 51–60 | 815 | 28.3 | 811 | 28.2 |
| ≥61 | 548 | 19.0 | 553 | 19.2 |
| Location | ||||
| Urban | 731 | 25.4 | 730 | 25.4 |
| Rural | 2146 | 74.6 | 2149 | 74.6 |
| Ethnic | ||||
| Majority (Han) | 2451 | 85.2 | 2454 | 85.2 |
| Minority | 426 | 14.8 | 425 | 14.8 |
| Gender | ||||
| Male | 1282 | 44.6 | 1283 | 44.6 |
| Female | 1595 | 55.4 | 1596 | 55.4 |
| Education level | ||||
| Illiteracy | 829 | 28.8 | 821 | 28.5 |
| Primary school | 595 | 20.7 | 603 | 20.9 |
| Middle school degree | 1259 | 43.8 | 1257 | 43.7 |
| Technical or vocational degree and higher | 194 | 6.7 | 198 | 6.9 |
| Smoking in 2006 | ||||
| Never | 1992 | 69.2 | 1994 | 69.3 |
| Ever | 885 | 30.8 | 885 | 30.7 |
| Still smoking in 2006 | ||||
| No | 2087 | 72.5 | 2090 | 72.6 |
| Yes | 790 | 27.5 | 789 | 27.4 |
| Drinking in 2006 | ||||
| Never | 1942 | 67.5 | 1942 | 67.5 |
| Ever | 935 | 32.5 | 937 | 32.5 |
| BMI category in 2006 (kg/m2) | ||||
| Underweight | 160 | 5.6 | 159 | 5.5 |
| Normal | 1681 | 58.4 | 1687 | 58.6 |
| Overweight | 818 | 28.4 | 816 | 28.3 |
| Obese | 218 | 7.6 | 217 | 7.5 |
| Energy intake in 2006 a | 2226.01 ± 670.73 | 2225.37 ± 671.33 | ||
| Activity level in 2006 | ||||
| Light | 1043 | 36.3 | 1043 | 36.2 |
| Middle | 417 | 14.5 | 424 | 14.7 |
| Heavy | 1408 | 48.9 | 1404 | 48.8 |
| No working ability | 9 | 0.3 | 8 | 0.3 |
| Variable | Systolic Blood Pressure | Diastolic Blood Pressure | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Class 1 (n = 277) | Class 2 (n = 1713) | Class 3 (n = 887) | P | Class 1 (n = 1035) | Class 2 (n = 1793) | Class 3 (n = 49) | P | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |||
| Event | 15 | 5.4% | 26 | 1.5% | 3 | 0.3% | <0.001 b | 6 | 0.6% | 38 | 2.1% | 0 | 0.0% | 0.004 b |
| Age group in 2006 | ||||||||||||||
| ≤40 | 1 | 0.4% | 242 | 14.1% | 397 | 44.8% | <0.001 | 380 | 36.7% | 257 | 14.3% | 3 | 6.1% | <0.001 |
| 41–50 | 29 | 10.5% | 483 | 28.2% | 362 | 40.8% | 443 | 42.8% | 420 | 23.4% | 11 | 22.4% | ||
| 51–60 | 82 | 29.6% | 610 | 35.6% | 123 | 13.9% | 205 | 19.8% | 595 | 33.2% | 15 | 30.6% | ||
| ≥61 | 165 | 59.6% | 378 | 22.1% | 5 | 0.6% | 7 | 0.7% | 521 | 29.1% | 20 | 40.8% | ||
| Location | ||||||||||||||
| Urban | 59 | 21.3% | 442 | 25.8% | 230 | 25.9% | 0.255 | 273 | 26.4% | 447 | 24.9% | 11 | 22.4% | 0.620 |
| Rural | 218 | 78.7% | 1271 | 74.2% | 657 | 74.1% | 762 | 73.6% | 1346 | 75.1% | 38 | 77.6% | ||
| Ethnicity | ||||||||||||||
| Majority (Han) | 240 | 86.6% | 1447 | 84.5% | 764 | 86.1% | 0.409 | 896 | 86.6% | 1515 | 84.5% | 40 | 81.6% | 0.254 |
| Minority | 37 | 13.4% | 266 | 15.5% | 123 | 13.9% | 139 | 13.4% | 278 | 15.5% | 9 | 18.4% | ||
| Gender | ||||||||||||||
| Male | 125 | 45.1% | 1094 | 63.9% | 63 | 7.1% | <0.001 | 38 | 3.7% | 1209 | 67.4% | 35 | 71.4% | <0.001 |
| Female | 152 | 54.9% | 619 | 36.1% | 824 | 92.9% | 997 | 96.3% | 584 | 32.6% | 14 | 28.6% | ||
| Education level | ||||||||||||||
| Illiteracy | 137 | 49.5% | 493 | 28.8% | 199 | 22.4% | <0.001 | 253 | 24.4% | 554 | 30.9% | 22 | 44.9% | 0.001 b |
| Primary school | 64 | 23.1% | 353 | 20.6% | 178 | 20.1% | 215 | 20.8% | 370 | 20.6% | 10 | 20.4% | ||
| Middle school | 61 | 22.0% | 749 | 43.7% | 449 | 50.6% | 498 | 48.1% | 745 | 41.6% | 16 | 32.7% | ||
| Technical or vocational degree and higher | 15 | 5.4% | 118 | 6.9% | 61 | 6.9% | 69 | 6.7% | 124 | 6.9% | 1 | 2.0% | ||
| Smoking in 2006 | ||||||||||||||
| Never | 193 | 69.7% | 963 | 56.2% | 836 | 94.3% | <0.001 | 995 | 96.1% | 971 | 54.2% | 26 | 53.1% | <0.001 |
| Ever | 84 | 30.3% | 750 | 43.8% | 51 | 5.7% | 40 | 3.9% | 822 | 45.8% | 23 | 46.9% | ||
| Still smoking in 2006 | ||||||||||||||
| No | 208 | 75.1% | 1039 | 60.7% | 840 | 94.7% | <0.001 | 998 | 96.4% | 1063 | 59.3% | 26 | 53.1% | <0.001 |
| Yes | 69 | 24.9% | 674 | 39.3% | 47 | 5.3% | 37 | 3.6% | 730 | 40.7% | 23 | 46.9% | ||
| Drinking in 2006 | ||||||||||||||
| Never | 190 | 68.6% | 973 | 56.8% | 779 | 87.8% | <0.001 | 928 | 89.7% | 996 | 55.5% | 18 | 36.7% | <0.001 |
| Ever | 87 | 31.4% | 740 | 43.2% | 108 | 12.2% | 107 | 10.3% | 797 | 44.5% | 31 | 63.3% | ||
| BMI category in 2006 (kg/m2) | ||||||||||||||
| Underweight | 24 | 8.7% | 96 | 5.6% | 40 | 4.5% | <0.001 | 47 | 4.5% | 109 | 6.1% | 4 | 8.2% | 0.036 b |
| Normal | 154 | 55.6% | 996 | 58.1% | 531 | 59.9% | 608 | 58.7% | 1047 | 58.4% | 26 | 53.1% | ||
| Overweight | 63 | 22.7% | 510 | 29.8% | 245 | 27.6% | 289 | 27.9% | 518 | 28.9% | 11 | 22.4% | ||
| Obese | 36 | 13.0% | 111 | 6.5% | 71 | 8.0% | 91 | 8.8% | 119 | 6.6% | 8 | 16.3% | ||
| Energy intake in 2006 a | 2067.19 ± 686.13 | 2311.11 ± 684.61 | 2111.26 ± 610.69 | <0.001 c | 2110.90 ± 608.47 | 2291.07 ± 694.00 | 2277.09 ± 743.05 | <0.001 c | ||||||
| Activity level in 2006 | ||||||||||||||
| Light | 135 | 48.7% | 594 | 34.7% | 314 | 35.4% | <0.001 b | 365 | 35.3% | 662 | 36.9% | 16 | 32.7% | 0.405 b |
| Middle | 27 | 9.7% | 253 | 14.8% | 137 | 15.4% | 153 | 14.8% | 260 | 14.5% | 4 | 8.2% | ||
| Heavy | 112 | 40.4% | 861 | 50.3% | 435 | 49.0% | 516 | 49.9% | 863 | 48.1% | 29 | 59.2% | ||
| No working ability | 3 | 1.1% | 5 | 0.3% | 1 | 0.1% | 1 | 0.1% | 8 | 0.4% | 0 | 0.0% | ||
| Variable | Systolic Blood Pressure | Diastolic Blood Pressure | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Class 1 (n = 1435) | Class 2 (n = 215) | Class 3 (n = 1229) | P | Class 1 (n = 952) | Class 2 (n = 1438) | Class 3 (n = 498) | P | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |||
| Event | 28 | 2.0% | 9 | 4.2% | 4 | 0.3% | <0.001 b | 25 | 2.6% | 15 | 1.0% | 1 | 0.2% | 0.000 b |
| Age group in 2006 | ||||||||||||||
| ≤40 | 128 | 8.9% | 2 | 0.9% | 512 | 41.7% | <0.001 | 95 | 10.0% | 217 | 15.1% | 330 | 67.5% | <0.001 |
| 41–50 | 415 | 28.9% | 26 | 12.1% | 432 | 35.2% | 269 | 28.3% | 449 | 31.2% | 155 | 31.7% | ||
| 51–60 | 518 | 36.1% | 69 | 32.1% | 224 | 18.2% | 321 | 33.7% | 486 | 33.8% | 4 | 0.8% | ||
| ≥61 | 374 | 26.1% | 118 | 54.9% | 61 | 5.0% | 267 | 28.0% | 286 | 19.9% | 0 | 0.0% | ||
| Location | ||||||||||||||
| Urban | 367 | 25.6% | 49 | 22.8% | 314 | 25.5% | 0.668 | 270 | 28.4% | 341 | 23.7% | 119 | 24.3% | 0.620 |
| Rural | 1068 | 74.4% | 166 | 77.2% | 915 | 74.5% | 682 | 71.6% | 1097 | 76.3% | 370 | 75.7% | ||
| Ethnicity | ||||||||||||||
| Majority (Han) | 1237 | 86.2% | 187 | 87.0% | 1030 | 83.8% | 0.167 | 845 | 88.8% | 1182 | 82.2% | 427 | 87.3% | <0.001 |
| Minority | 198 | 13.8% | 28 | 13.0% | 199 | 16.2% | 107 | 11.2% | 256 | 17.8% | 62 | 12.7% | ||
| Gender | ||||||||||||||
| Male | 854 | 59.5% | 95 | 44.2% | 334 | 27.2% | <0.001 | 598 | 62.8% | 659 | 45.8% | 26 | 5.3% | <0.001 |
| Female | 581 | 40.5% | 120 | 55.8% | 895 | 72.8% | 354 | 37.2% | 779 | 54.2% | 463 | 94.7% | ||
| Education level | ||||||||||||||
| Illiteracy | 426 | 29.7% | 100 | 46.5% | 295 | 24.0% | <0.001 | 272 | 28.6% | 481 | 33.4% | 68 | 13.9% | <0.001 |
| Primary school | 328 | 22.9% | 49 | 22.8% | 226 | 18.4% | 205 | 21.5% | 293 | 20.4% | 105 | 21.5% | ||
| Middle school | 588 | 41.0% | 53 | 24.7% | 616 | 50.1% | 405 | 42.5% | 580 | 40.3% | 272 | 55.6% | ||
| Technical or vocational degree and higher | 93 | 6.5% | 13 | 6.0% | 92 | 7.5% | 70 | 7.4% | 84 | 5.8% | 44 | 9.0% | ||
| Smoking in 2006 | ||||||||||||||
| Never | 848 | 59.1% | 153 | 71.2% | 993 | 80.8% | <0.001 | 564 | 59.2% | 957 | 66.6% | 473 | 96.7% | <0.001 |
| Ever | 587 | 40.9% | 62 | 28.8% | 236 | 19.2% | 388 | 40.8% | 481 | 33.4% | 16 | 3.3% | ||
| Still smoking in 2006 | ||||||||||||||
| No | 920 | 64.1% | 161 | 74.9% | 1009 | 82.1% | <0.001 | 617 | 64.8% | 999 | 69.5% | 474 | 96.9% | <0.001 |
| Yes | 515 | 35.9% | 54 | 25.1% | 220 | 17.9% | 335 | 35.2% | 439 | 30.5% | 15 | 3.1% | ||
| Drinking in 2006 | ||||||||||||||
| Never | 869 | 60.6% | 145 | 67.4% | 928 | 75.5% | <0.001 | 549 | 57.7% | 955 | 66.4% | 438 | 89.6% | <0.001 |
| Ever | 566 | 39.4% | 70 | 32.6% | 301 | 24.5% | 403 | 42.3% | 483 | 33.6% | 51 | 10.4% | ||
| BMI category in 2006 (kg/m2) | ||||||||||||||
| Underweight | 50 | 3.5% | 7 | 3.3% | 102 | 8.3% | <0.001 | 4 | 0.4% | 117 | 8.1% | 38 | 4 | <0.001 |
| Normal | 738 | 51.4% | 74 | 34.4% | 875 | 71.2% | 329 | 34.6% | 998 | 69.4% | 360 | 329 | ||
| Overweight | 511 | 35.6% | 76 | 35.3% | 229 | 18.6% | 433 | 45.5% | 302 | 21.0% | 81 | 433 | ||
| Obese | 136 | 9.5% | 58 | 27.0% | 23 | 1.9% | 186 | 19.5% | 21 | 1.5% | 10 | 186 | ||
| Energy intake in 2006 a | 2290.27 ± 687.03 | 2060.53 ± 635.23 | 2178.43 ± 650.28 | <0.001 | 2288.77 ± 689.68 | 2225.48 ± 672.58 | 2101.64 ± 612.98 | <0.001 c | ||||||
| Activity level in 2006 | ||||||||||||||
| Light | 544 | 37.9% | 110 | 51.2% | 389 | 31.7% | <0.001 b | 420 | 44.1% | 463 | 32.2% | 160 | 32.7% | <0.001 b |
| Middle | 207 | 14.4% | 20 | 9.3% | 197 | 16.0% | 136 | 14.3% | 201 | 14.0% | 87 | 17.8% | ||
| Heavy | 678 | 47.2% | 84 | 39.1% | 642 | 52.2% | 394 | 41.4% | 769 | 53.5% | 241 | 49.3% | ||
| No working ability | 6 | 0.4% | 1 | 0.5% | 1 | 0.1% | 2 | 0.2% | 5 | 0.3% | 1 | 0.2% | ||
| Outcomes | Classes of Trajectories | Event | n | Incidence Density a | Crude Model | Adjusted Model 1 b | Adjusted Model 2 c | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | ||||||
| Stroke | SBP | Class 3 | 3 | 887 | 0.063 | Ref. | Ref. | Ref. | ||||||
| Class 1 | 15 | 277 | 1.015 | 16.400 | 4.748–56.648 | <0.001 | 3.837 | 0.911–16.167 | 0.067 | 3.837 | 0.911–16.167 | 0.067 | ||
| Class 2 | 26 | 1713 | 0.282 | 4.513 | 1.366–14.910 | 0.013 | 1.369 | 0.357–5.248 | 0.647 | 1.369 | 0.357–5.248 | 0.647 | ||
| DBP | Class 1 | 6 | 1035 | 0.107 | Ref. | - | - | - | - | - | - | |||
| Class 2 | 38 | 1793 | 0.395 | 3.685 | 1.558–8.718 | 0.003 | - | - | - | - | - | - | ||
| Class 3 | 0 | 49 | 0 | - | - | - | - | - | - | - | - | - | ||
| MI | SBP | Class 3 | 4 | 1229 | 0.060 | Ref. | Ref. | Ref. | ||||||
| Class 1 | 28 | 1435 | 0.362 | 6.047 | 2.121–17.239 | 0.001 | 6.047 | 2.121–17.239 | 0.001 | 6.047 | 2.121–17.239 | 0.001 | ||
| Class 2 | 9 | 215 | 0.778 | 13.017 | 4.009–42.470 | <0.001 | 13.017 | 4.009–42.270 | <0.001 | 13.017 | 4.009–42.270 | <0.001 | ||
| DBP | Class 3 | 1 | 498 | 0.038 | Ref. | Ref. | - | - | - | |||||
| Class 1 | 25 | 952 | 0.488 | 12.996 | 1.761–95.913 | 0.012 | 2.821 | 0.323–24.665 | 0.349 | - | - | - | ||
| Class 2 | 15 | 1438 | 0.193 | 5.118 | 0.676–38.742 | 0.114 | 1.312 | 0.150–11.494 | 0.806 | - | - | - | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, F.; Lin, Q.; Li, M.; Chen, L.; Li, Y. The Association between Blood Pressure Trajectories and Risk of Cardiovascular Diseases among Non-Hypertensive Chinese Population: A Population-Based Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 2909. https://doi.org/10.3390/ijerph18062909
Li F, Lin Q, Li M, Chen L, Li Y. The Association between Blood Pressure Trajectories and Risk of Cardiovascular Diseases among Non-Hypertensive Chinese Population: A Population-Based Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(6):2909. https://doi.org/10.3390/ijerph18062909
Chicago/Turabian StyleLi, Fang, Qian Lin, Mingshu Li, Lizhang Chen, and Yingjun Li. 2021. "The Association between Blood Pressure Trajectories and Risk of Cardiovascular Diseases among Non-Hypertensive Chinese Population: A Population-Based Cohort Study" International Journal of Environmental Research and Public Health 18, no. 6: 2909. https://doi.org/10.3390/ijerph18062909
APA StyleLi, F., Lin, Q., Li, M., Chen, L., & Li, Y. (2021). The Association between Blood Pressure Trajectories and Risk of Cardiovascular Diseases among Non-Hypertensive Chinese Population: A Population-Based Cohort Study. International Journal of Environmental Research and Public Health, 18(6), 2909. https://doi.org/10.3390/ijerph18062909







