Racial and Ethnic Disparities in Years of Potential Life Lost Attributable to COVID-19 in the United States: An Analysis of 45 States and the District of Columbia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.2. Estimation Procedure for YPLL-Based Estimands from Administratively Interval Censored Ages at Death
2.3. Procedure Modification to Account for Suppression of Low Death Counts
2.4. Procedure Modification to Further Account for a Subset of Deaths with Unknown Race/Ethnicty
2.5. Computational Savings by Omitting Unnecessary Mortality Datasets
2.6. Complete Monte Carlo Simulation Procedure for Estimation of YPLL-Based Estimands
- Calculate the difference between the total number of deaths as provided by the NCHS Sex Data and the total number of deaths contained in intervals with non-suppressed death counts; this is the number of deaths contained in the union of intervals with suppressed death counts.
- Let denote the total number of MC iterations, and let index the MC iterations. For the task of obtaining a maximum MC point estimate of the estimand of interest that primarily concerns racial/ethnic group r at each MC iteration b, combine the Unknown racial/ethnic group with racial/ethnic group r into a combined r-Unknown racial/ethnic group whose constituents we all assume to be in racial/ethnic group r, combine the remaining racial/ethnic groups that are not included in the definition of the estimand into a single “other” racial/ethnic group, and enumerate all possible mortality datasets, omitting those that would yield a maximum MC point estimate with probability 0. For the task of obtaining a minimum MC point estimate of the estimand of interest, combine all of the racial/ethnic groups not included in the definition of the estimand (including the Unknown racial/ethnic group) and enumerate all possible mortality datasets, omitting those that would yield a minimum MC point estimate with probability 0. Let denote the number of mortality datasets considered for the maximization task in state s, and let denote the number of mortality datasets considered for the minimization task in state s.
- Specify a YPLL upper reference age less than or equal to 85 years. We view age group <1 as equivalent to the singular age 0, and the remaining numeric NCHS age group endpoints represent integer age at last birthday so that there is a 1-year gap between the endpoints of two chronologically consecutive age groups (e.g., 35–44 and 45–54). We treat age as a continuous variable, and as a consequence, we mathematically interpret the <1 age group (age 0) as the right half-open interval , the age group as the half-bounded interval , and the remaining NCHS age groups as right half-open intervals with lower limit equal to the lower endpoint of the corresponding NCHS age group and upper limit equal to the upper endpoint of the corresponding NCHS age group plus one (e.g., age group 5–14 is viewed as ). At each MC iteration b and for each mortality dataset considered for the maximization and minimization tasks, independently simulate an age at death for each individual fatality i corresponding to age interval , where , from the corresponding continuous uniform distribution:Observe that is intentionally and necessarily chosen to be less than or equal to 85 years to obviate the simulation of ages at death corresponding to the 85+ age group, thereby avoiding potential analytic difficulties because each fatality corresponding to the 85+ age group contributes nothing to YPLL.
- At each MC iteration b and for each mortality dataset j, calculate a point estimate of the estimand of interest. In particular, for the estimation of the percentage of total YPLL for racial/ethnic group r, first calculate total YPLL for racial/ethnic group r (which includes the Unknown racial/ethnic group for the maximization task) and the remaining racial/ethnic groups from the simulated ages at death, which are and , respectively. Then, the percentage of total YPLL for racial/ethnic group r, which we denote , is given by:For estimation of the age-adjusted r-to-NH White YPLL RR, first estimate the age-adjusted YPLL rates for racial/ethnic group r and NH Whites, using the 2019 CDC WONDER age distribution estimate of the overall U.S. population as the standard population. The age-adjusted YPLL rate for racial/ethnic group r (which includes the Unknown racial/ethnic group for the maximization task) is calculated using direct age adjustment [54] from the simulated ages at death, which we denote . Since the simulated ages at death are continuous and the CDC WONDER age distribution estimates are defined over integer ages from 0 to 84, we aggregate the corresponding simulated YPLL values with respect the 1-year intervals implied by these integer ages (i.e., age implies age interval ) to calculate the age-specific YPLL rates, which are subsequently applied to the standard population to obtain the age-adjusted YPLL rate for racial/ethnic group r:where denotes aggregate YPLL corresponding to age ; denotes the 2019 CDC WONDER U.S. population estimate for race/ethnicity r, state s, and age ; and denotes the 2019 CDC WONDER U.S. population estimate for age . Then, the age-adjusted r-to-NH White YPLL RR is defined to be the quotient of and :
- At each MC iteration b, store the maximum of the MC point estimates of the estimand of interest calculated from the set of mortality datasets considered for the maximization task, and store the minimum of the MC point estimates calculated from the set of mortality datasets considered for the minimization task.
- A conservative interval estimate of the estimand of interest is given by the quantile of the minimum MC point estimates and the quantile of the maximum MC point estimates.
2.7. Monte Carlo Simulation Procedure for Estimation of Age-Adjusted Mortality Rates and Rate Ratios
2.8. Computation
3. Results
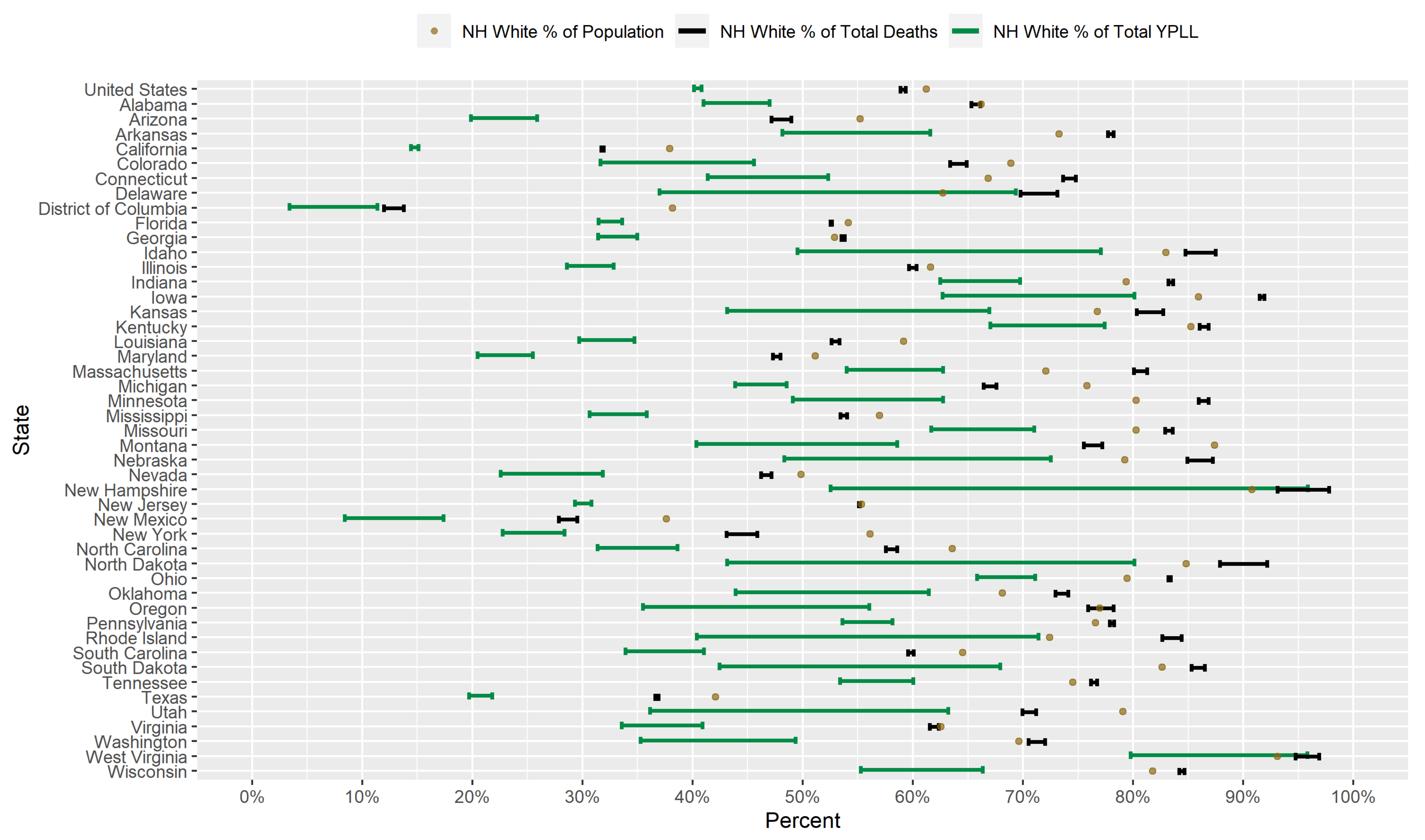
3.1. Results for Non-Hispanic Whites
3.2. Results for Non-Hispanic Blacks
3.3. Results for Hispanics
3.4. Results for Non-Hispanic Asians
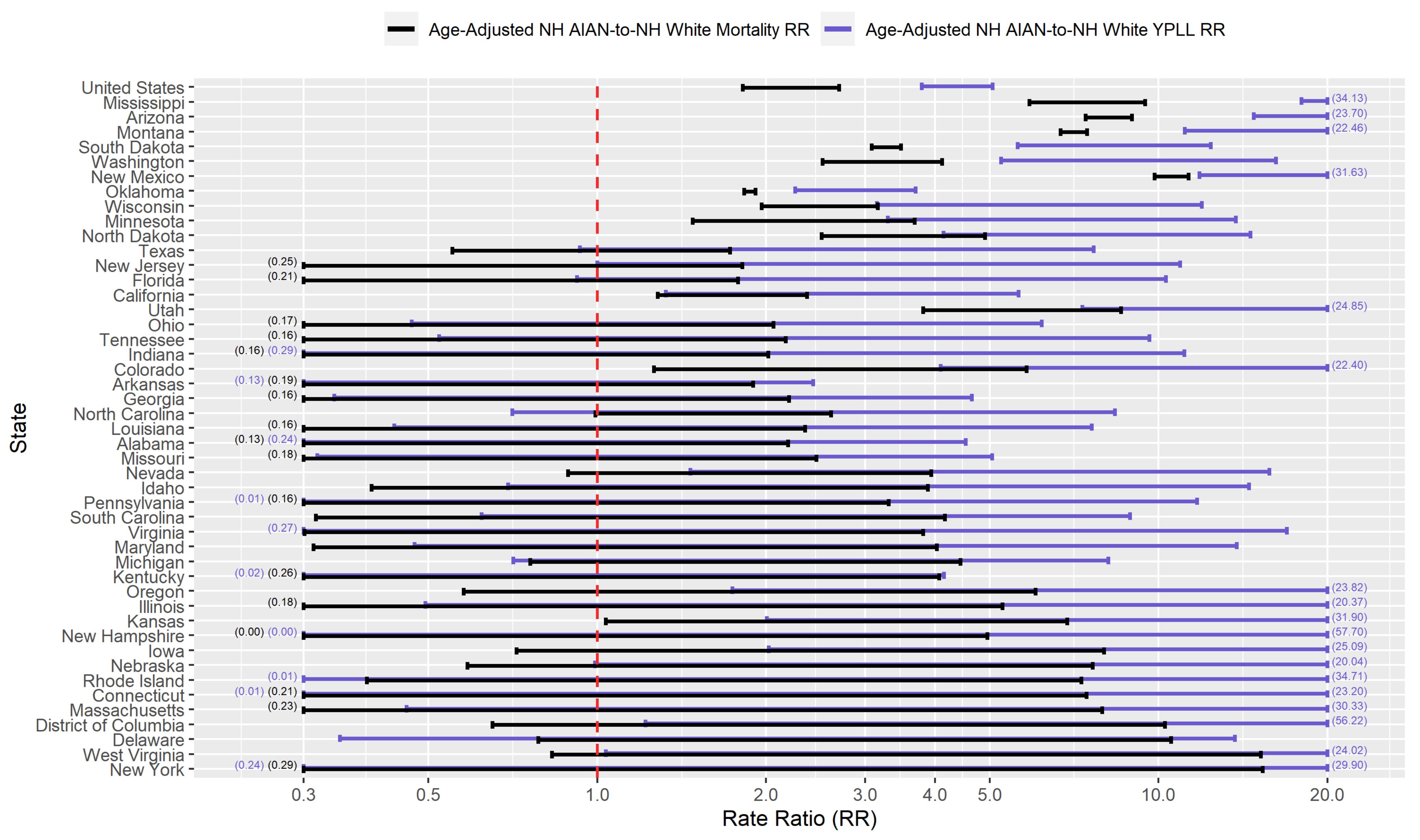
3.5. Results for Non-Hispanic American Indian or Alaska Natives
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CDC | Centers for Disease Control and Prevention |
| COVID-19 | Coronavirus Disease 2019 |
| D.C. | District of Columbia |
| MC | Monte Carlo |
| NCHS | National Center for Health Statistics |
| NH AIAN | Non-Hispanic American Indian or Alaska Native |
| NH Asian | Non-Hispanic Asian |
| NH Black | Non-Hispanic Black |
| NH White | Non-Hispanic White |
| RR | Rate Ratio |
| U.S. | United States |
| YPLL | Years of Potential Life Lost |
References
- Cevik, M.; Kuppalli, K.; Kindrachuk, J.; Peiris, M. Virology, transmission, and pathogenesis of SARS-CoV-2. BMJ 2020, 371. [Google Scholar] [CrossRef] [PubMed]
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- First Patient With Wuhan Coronavirus Is Identified in the U.S. Available online: https://www.nytimes.com/2020/01/21/health/cdc-coronavirus.html (accessed on 15 February 2021).
- Holshue, M.L.; DeBolt, C.; Lindquist, S.; Lofy, K.H.; Wiesman, J.; Bruce, H.; Spitters, C.; Ericson, K.; Wilkerson, S.; Tural, A.; et al. First Case of 2019 Novel Coronavirus in the United States. N. Engl. J. Med. 2020, 382, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Bio Med. 2020, 91, 157–160. [Google Scholar]
- Coronavirus (Covid-19) Data in the United States. Available online: https://github.com/nytimes/covid-19-data (accessed on 15 February 2021).
- Griffith, D.M.; Sharma, G.; Holliday, C.S.; Enyia, O.K.; Valliere, M.; Semlow, A.R.; Stewart, E.C.; Blumenthal, R.S. Men and COVID-19: A Biopsychosocial Approach to Understanding Sex Differences in Mortality and Recommendations for Practice and Policy Interventions. Prev. Chronic Dis. 2020, 17, E63. [Google Scholar] [CrossRef]
- Older Adults: At Greater Risk Of requiring Hospitalization or Dying if Diagnosed with COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html (accessed on 15 February 2021).
- Minority Groups at Risk as States withhold, Provide Partial COVID-19 Racial Data. Available online: https://abcnews.go.com/Politics/states-missing-covid-19-racial-ethnic-data-creates/story?id=70338255 (accessed on 15 February 2021).
- Krieger, N.; Gonsalves, G.; Bassett, M.; Hanage, W.; Krumholz, H. The Fierce Urgency Of Now: Closing Glaring Gaps In US Surveillance Data On COVID-19. Health Aff. Blog 2020. Available online: https://www.healthaffairs.org/do/10.1377/hblog20200414.238084/full/ (accessed on 15 February 2021).
- COVID-19 Hospitalization and Death by Race/Ethnicity. Available online: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (accessed on 15 February 2021).
- Millett, G.A.; Jones, A.T.; Benkeser, D.; Baral, S.; Mercer, L.; Beyrer, C.; Honermann, B.; Lankiewicz, E.; Mena, L.; Crowley, J.S.; et al. Assessing differential impacts of COVID-19 on Black communities. Ann. Epidemiol. 2020, 47, 37–44. [Google Scholar] [CrossRef]
- Karaca-Mandic, P.; Georgiou, A.; Sen, S. Assessment of COVID-19 Hospitalizations by Race/Ethnicity in 12 States. JAMA Intern. Med. 2021, 181, 131–134. [Google Scholar] [CrossRef]
- Holtgrave, D.R.; Barranco, M.A.; Tesoriero, J.M.; Blog, D.S.; Rosenberg, E.S. Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State. Ann. Epidemiol. 2020, 48, 9–14. [Google Scholar] [CrossRef]
- Golestaneh, L.; Neugarten, J.; Fisher, M.; Billett, H.H.; Gil, M.R.; Johns, T.; Yunes, M.; Mokrzycki, M.H.; Coco, M.; Norris, K.C.; et al. The association of race and COVID-19 mortality. EClinicalMedicine 2020, 25, 100455. [Google Scholar] [CrossRef]
- Renelus, B.D.; Khoury, N.C.; Chandrasekaran, K.; Bekele, E.; Briggs, W.M.; Ivanov, A.; Mohanty, S.R.; Jamorabo, D.S. Racial Disparities in COVID-19 Hospitalization and In-hospital Mortality at the Height of the New York City Pandemic. J. Racial Ethn. Health Disparities 2020. [Google Scholar] [CrossRef]
- Lieberman-Cribbin, W.; Tuminello, S.; Flores, R.M.; Taioli, E. Disparities in COVID-19 Testing and Positivity in New York City. Am. J. Prev. Med. 2020, 59, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Diaz, C.E.; Guilamo-Ramos, V.; Mena, L.; Hall, E.; Honermann, B.; Crowley, J.S.; Baral, S.; Prado, G.J.; Marzan-Rodriguez, M.; Beyrer, C.; et al. Risk for COVID-19 infection and death among Latinos in the United States: Examining heterogeneity in transmission dynamics. Ann. Epidemiol. 2020, 52, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Gross, C.P.; Essien, U.R.; Pasha, S.; Gross, J.R.; Wang, S.y.; Nunez-Smith, M. Racial and Ethnic Disparities in Population-Level Covid-19 Mortality. J. Gen. Intern. Med. 2020, 35, 3097–3099. [Google Scholar] [CrossRef] [PubMed]
- Arasteh, K. Prevalence of Comorbidities and Risks Associated with COVID-19 Among Black and Hispanic Populations in New York City: An Examination of the 2018 New York City Community Health Survey. J. Racial Ethn. Health Disparities 2020. [Google Scholar] [CrossRef]
- Abedi, V.; Olulana, O.; Avula, V.; Chaudhary, D.; Khan, A.; Shahjouei, S.; Li, J.; Zand, R. Racial, Economic, and Health Inequality and COVID-19 Infection in the United States. J. Racial Ethn. Health Disparities 2020. [Google Scholar] [CrossRef]
- Thomas, M.D.; Michaels, E.K.; Darling-Hammond, S.; Nguyen, T.T.; Glymour, M.M.; Vittinghoff, E. Whites’ County-Level Racial Bias, COVID-19 Rates, and Racial Inequities in the United States. Int. J. Environ. Res. Public Health 2020, 17, 8695. [Google Scholar] [CrossRef]
- Zelner, J.; Trangucci, R.; Naraharisetti, R.; Cao, A.; Malosh, R.; Broen, K.; Masters, N.; Delamater, P. Racial Disparities in Coronavirus Disease 2019 (COVID-19) Mortality Are Driven by Unequal Infection Risks. Clin. Infect. Dis. 2020, 72, e88–e95. [Google Scholar] [CrossRef]
- Wang, Q.; Berger, N.A.; Xu, R. Analyses of Risk, Racial Disparity, and Outcomes Among US Patients With Cancer and COVID-19 Infection. JAMA Oncol. 2020, 7, 220–227. [Google Scholar] [CrossRef]
- Tirupathi, R.; Muradova, V.; Shekhar, R.; Salim, S.A.; Al-Tawfiq, J.A.; Palabindala, V. COVID-19 disparity among racial and ethnic minorities in the US: A cross sectional analysis. Travel Med. Infect. Dis. 2020, 38, 101904. [Google Scholar] [CrossRef]
- Muñoz-Price, L.S.; Nattinger, A.B.; Rivera, F.; Hanson, R.; Gmehlin, C.G.; Perez, A.; Singh, S.; Buchan, B.W.; Ledeboer, N.A.; Pezzin, L.E. Racial Disparities in Incidence and Outcomes Among Patients With COVID-19. JAMA Netw. Open 2020, 3, e2021892. [Google Scholar] [CrossRef]
- Parcha, V.; Malla, G.; Suri, S.S.; Kalra, R.; Heindl, B.; Berra, L.; Fouad, M.N.; Arora, G.; Arora, P. Geographic Variation in Racial Disparities in Health and Coronavirus Disease-2019 (COVID-19) Mortality. Mayo Clin. Proc. Innov. Qual. Outcomes 2020, 4, 703–716. [Google Scholar] [CrossRef]
- Gu, T.; Mack, J.A.; Salvatore, M.; Sankar, S.P.; Valley, T.S.; Singh, K.; Nallamothu, B.K.; Kheterpal, S.; Lisabeth, L.; Fritsche, L.G.; et al. Characteristics Associated With Racial/Ethnic Disparities in COVID-19 Outcomes in an Academic Health Care System. JAMA Netw. Open 2020, 3, e2025197. [Google Scholar] [CrossRef]
- Vahidy, F.S.; Nicolas, J.C.; Meeks, J.R.; Khan, O.; Pan, A.; Jones, S.L.; Masud, F.; Sostman, H.D.; Phillips, R.; Andrieni, J.D.; et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: Analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open 2020, 10, e039849. [Google Scholar] [CrossRef] [PubMed]
- Ogedegbe, G.; Ravenell, J.; Adhikari, S.; Butler, M.; Cook, T.; Francois, F.; Iturrate, E.; Jean-Louis, G.; Jones, S.A.; Onakomaiya, D.; et al. Assessment of Racial/Ethnic Disparities in Hospitalization and Mortality in Patients With COVID-19 in New York City. JAMA Netw. Open 2020, 3, e2026881. [Google Scholar] [CrossRef] [PubMed]
- Strully, K.; Yang, T.C.; Liu, H. Regional variation in COVID-19 disparities: Connections with immigrant and Latinx communities in US counties. Ann. Epidemiol. 2021, 53, 56–62. [Google Scholar] [CrossRef] [PubMed]
- The Color of Coronavirus: COVID-19 Deaths by Race and Ethnicity in the U.S. Available online: https://www.apmresearchlab.org/covid/deaths-by-race (accessed on 15 February 2021).
- The COVID Racial Data Tracker. Available online: https://covidtracking.com/race (accessed on 15 February 2021).
- Gardner, J.W.; Sanborn, J.S. Years of Potential Life Lost (YPLL)—What Does it Measure? Epidemiology 1990, 1, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Desenclos, J.C.A.; Hahn, R.A. Years of potential life lost before age 65, by race, Hispanic origin, and sex—United States, 1986–1988. Morb. Mortal. Wkly. Rep. CDC Surveill. Summ. 1992, 41, 13–23. [Google Scholar]
- Li, C.; Ekwueme, D.U.; Rim, S.H.; Tangka, F.K. Years of Potential Life Lost and Productivity Losses From Male Urogenital Cancer Deaths—United States, 2004. Urology 2010, 76, 528–535. [Google Scholar] [CrossRef]
- Max, W.; Sung, H.Y.; Shi, Y. Deaths From Secondhand Smoke Exposure in the United States: Economic Implications. Am. J. Public Health 2012, 102, 2173–2180. [Google Scholar] [CrossRef] [PubMed]
- Bassett, M.T.; Chen, J.T.; Krieger, N. Variation in racial/ethnic disparities in COVID-19 mortality by age in the United States: A cross-sectional study. PLoS Med. 2020, 17, e1003402. [Google Scholar] [CrossRef] [PubMed]
- Deaths Involving Coronavirus Disease 2019 (COVID-19) by Race and Hispanic Origin Group and Age, by State. Available online: https://data.cdc.gov/NCHS/Deaths-involving-coronavirus-disease-2019-COVID-19/ks3g-spdg (accessed on 15 February 2021).
- U.S. Deaths Are Up Sharply, Though Covid-19’s Precise Toll Is Murky. Available online: https://www.wsj.com/articles/covid-19s-exact-toll-is-murky-though-u-s-deaths-are-up-sharply-11589555652 (accessed on 15 February 2021).
- Excess Deaths From COVID-19 and Other Causes, March-April 2020, author=Woolf, Steven H and Chapman, Derek A and Sabo, Roy T and Weinberger, Daniel M and Hill, Latoya. JAMA 2020, 324, 510–513. [CrossRef] [PubMed]
- Weinberger, D.M.; Chen, J.; Cohen, T.; Crawford, F.W.; Mostashari, F.; Olson, D.; Pitzer, V.E.; Reich, N.G.; Russi, M.; Simonsen, L.; et al. Estimation of Excess Deaths Associated With the COVID-19 Pandemic in the United States, March to May 2020. JAMA Intern. Med. 2020, 180, 1336–1344. [Google Scholar] [CrossRef] [PubMed]
- Why is NC Delayed in Reporting COVID-19 Death Data? It’s About Death Certificates. Available online: https://www.northcarolinahealthnews.org/2020/09/18/why-is-nc-delayed-in-reporting-covid-19-death-data/ (accessed on 15 February 2021).
- Provisional COVID-19 Death Counts by Sex, Age, and State. Available online: https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku (accessed on 15 February 2021).
- Bridged-Race Population Estimates 1990–2019 Request. Available online: https://wonder.cdc.gov/Bridged-Race-v2019.HTML (accessed on 30 December 2020).
- Rothman, K.J.; Greenland, S.; Lash, T.L. Modern Epidemiology; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- Romeder, J.; McWhinnie, J. Potential Years of Life Lost Between Ages 1 and 70: An Indicator of Premature Mortality for Health Planning. Int. J. Epidemiol. 1977, 6, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Arcà, M.; Di Orio, F.; Forastiere, F.; Tasco, C.; Perucci, C. Years of Potential Life Lost (YPLL) before Age 65 in Italy. Am. J. Public Health 1988, 78, 1202–1205. [Google Scholar] [CrossRef]
- Curran, J.W.; Morgan, W.M.; Hardy, A.M.; Jaffe, H.W.; Darrow, W.W.; Dowdle, W.R. The epidemiology of AIDS: Current status and future prospects. Science 1985, 229, 1352–1357. [Google Scholar] [CrossRef]
- Albert, V.A.; Koh, H.K.; Geller, A.C.; Miller, D.R.; Prout, M.N.; Lew, R.A. Years of potential life lost: Another indicator of the impact of cutaneous malignant melanoma on society. J. Am. Acad. Dermatol. 1990, 23, 308–310. [Google Scholar] [CrossRef]
- Mitra, A.K.; Payton, M.; Kabir, N.; Whitehead, A.; Ragland, K.N.; Brown, A. Potential Years of Life Lost Due to COVID-19 in the United States, Italy, and Germany: An Old Formula with Newer Ideas. Int. J. Environ. Res. Public Health 2020, 17, 4392. [Google Scholar] [CrossRef]
- Xu, J.J.; Belin, T.R.; Ramirez, C.M. Uncertainty Quantification of Years of Potential Life Lost-Based Estimates from Mortality Data Summarized as Death Counts Within Age Intervals. Ann. Epidemiol. 2021, 55, 1–3. [Google Scholar] [CrossRef]
- Bobashev, G.V.; Morris, R.J. Uncertainty and Inference in Agent-based Models. In Proceedings of the 2010 Second International Conference on Advances in System Simulation, Nice, France, 22–27 August 2010; pp. 67–71. [Google Scholar]
- Celentano, D.D.; Szklo, M. Gordis Epidemiology; Elsevier: Philadelphia, PA, USA, 2019. [Google Scholar]
- Racial Data Transparency. Available online: https://coronavirus.jhu.edu/data/racial-data-transparency (accessed on 15 February 2021).
- Table 25. Years of Potential Life Lost before Age 75 for Selected Causes of Death, by Sex, Race, and Hispanic Origin: United States, Selected Years 1980–2007. Available online: https://www.cdc.gov/nchs/data/hus/2010/025.pdf (accessed on 15 February 2021).
- Table 25. Years of Potential Life Lost before age 75 for Selected Causes of Death, by Sex, Race, and Hispanic Origin: United States, Selected Years 1980–2010. Available online: https://www.cdc.gov/nchs/data/hus/2011/025.pdf (accessed on 15 February 2021).
- Table 21. Years of Potential life Lost before Age 75 for Selected Causes of Death, by Sex, Race, and Hispanic Origin: United States, Selected Years 1980–2010. Available online: https://www.cdc.gov/nchs/data/hus/2012/021.pdf (accessed on 15 February 2021).
- Table 21. Years of Potential Life lost Before age 75 For selected Causes of Death, by Sex, Race, and Hispanic Origin: United States, Selected Years 1980–2011. Available online: https://www.cdc.gov/nchs/data/hus/2013/021.pdf (accessed on 15 February 2021).
- Table 19. Years of Potential Life Lost before Age 75 for Selected Causes of Death, by Sex, Race, and Hispanic Origin: United States, Selected Years 1980–2013. Available online: https://www.cdc.gov/nchs/data/hus/2014/019.pdf (accessed on 15 February 2021).
- Table 18 (page 1 of 4). Years of Potential Life Lost before Age 75 for Selected Causes of Death, by Sex, Race, and Hispanic Origin: United States, Selected Years 1980–2014. Available online: https://www.cdc.gov/nchs/data/hus/2015/018.pdf (accessed on 15 February 2021).
- Table 18. Years of Potential Life Lost before Age 75 for Selected Causes of Death, by Sex, Race, and Hispanic Origin: United States, Selected Years 1980–2015. Available online: https://www.cdc.gov/nchs/data/hus/2016/018.pdf (accessed on 15 February 2021).
- Table 18. Years of Potential Life Lost before age 75 for Selected Causes of Death, by Sex, Race, and Hispanic Origin: United States, Selected Years 1980–2016. Available online: https://www.cdc.gov/nchs/data/hus/2017/018.pdf (accessed on 15 February 2021).
- Borse, N.N.; Rudd, R.A.; Dellinger, A.M.; Sleet, D.A. Years of potential life lost from unintentional child and adolescent injuries—United States, 2000–2009. J. Saf. Res. 2013, 45, 127–131. [Google Scholar] [CrossRef]
- Khalil, M.I.; Bimali, M.; Davis, R.; Machado, B.; Kamel, M. MP23-06 Racial Disparities in Years of Potential Life Lost Secondary to Untreated Low and Intermediate Risk Prostate Cancer Deaths. J. Urol. 2020, 203, e339–e340. [Google Scholar] [CrossRef]
- Ekwueme, D.U.; Guy, G.P. Jr.; Li, C.; Rim, S.H.; Parelkar, P.; Chen, S.C. The health burden and economic costs of cutaneous melanoma mortality by race/ethnicity–United States, 2000 to 2006. J. Am. Acad. Dermatol. 2011, 65, S133.e1–S133.e12. [Google Scholar] [CrossRef] [Green Version]
- Ekwueme, D.U.; Guy, G.P. Jr.; Rim, S.H.; White, A.; Hall, I.J.; Fairley, T.L.; Dean, H.D. Health and Economic Impact of Breast Cancer Mortality in Young Women, 1970–2008. Am. J. Prev. Med. 2014, 46, 71–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bucholz, E.M.; Normand, S.L.T.; Wang, Y.; Ma, S.; Lin, H.; Krumholz, H.M. Life Expectancy and Years of Potential Life Lost After Acute Myocardial Infarction by Sex and Race A Cohort-Based Study of Medicare Beneficiaries. J. Am. Coll. Cardiol. 2015, 66, 645–655. [Google Scholar] [CrossRef]
- Iyer, D.G.; Shah, N.S.; Hastings, K.G.; Hu, J.; Rodriguez, F.; Boothroyd, D.B.; Krishnan, A.V.; Falasinnu, T.; Palaniappan, L. Years of Potential Life Lost Because of Cardiovascular Disease in Asian-American Subgroups, 2003–2012. J. Am. Heart Assoc. 2019, 8, e010744. [Google Scholar] [CrossRef] [PubMed]
- Buchanich, J.M.; Doerfler, S.M.; Lann, M.F.; Marsh, G.M.; Burke, D.S. Improvement in racial disparities in years of life lost in the USA since 1990. PLoS ONE 2018, 13, e0194308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- COVID-19 Deaths by Race/Ethnicity. Available online: https://www.kff.org/other/state-indicator/covid-19-deaths-by-race-ethnicity/ (accessed on 15 February 2021).
- Long-Term Effects of COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html (accessed on 15 February 2021).
- Murray, C.J. Quantifying the burden of disease: The technical basis for disability-adjusted life years. Bull. World Health Organ. 1994, 72, 429–445. [Google Scholar]
- Profile: Black/African Americans. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=61 (accessed on 15 February 2021).
- Profile: Hispanic/Latino Americans. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64 (accessed on 15 February 2021).
- People with Certain Medical Conditions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 15 February 2021).
- Giudicessi, J.R.; Roden, D.M.; Wilde, A.A.; Ackerman, M.J. Genetic susceptibility for COVID-19–associated sudden cardiac death in African Americans. Heart Rhythm 2020, 17, 1487–1492. [Google Scholar] [CrossRef]
- Bunyavanich, S.; Grant, C.; Vicencio, A. Racial/Ethnic Variation in Nasal Gene Expression of Transmembrane Serine Protease 2 (TMPRSS2). JAMA 2020, 324, 1567–1568. [Google Scholar] [CrossRef] [PubMed]
- Sarangarajan, R.; Winn, R.; Kiebish, M.A.; Bountra, C.; Granger, E.; Narain, N.R. Ethnic Prevalence of Angiotensin-Converting Enzyme Deletion (D) Polymorphism and COVID-19 Risk: Rationale for Use of Angiotensin-Converting Enzyme Inhibitors/Angiotensin Receptor Blockers. J. Racial Ethn. Health Disparities 2020. [Google Scholar] [CrossRef]
- Social Determinants of Health. Available online: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed on 15 February 2021).
- Abrams, E.M.; Szefler, S.J. COVID-19 and the impact of social determinants of health. Lancet. Respir. Med. 2020, 8, 659–661. [Google Scholar] [CrossRef]
- Shah, G.H.; Shankar, P.; Schwind, J.S.; Sittaramane, V. The Detrimental Impact of the COVID-19 Crisis on Health Equity and Social Determinants of Health. J. Public Health Manag. Pract. 2020, 26, 317–319. [Google Scholar] [CrossRef] [PubMed]
- Rollston, R.; Galea, S. COVID-19 and the Social Determinants of Health. Am. J. Health Promot. 2020, 34, 687–689. [Google Scholar] [CrossRef] [PubMed]
- Hooper, M.W.; Nápoles, A.M.; Pérez-Stable, E.J. COVID-19 and Racial/Ethnic Disparities. JAMA 2020, 323, 2466–2467. [Google Scholar] [CrossRef] [PubMed]
- Maness, S.B.; Merrell, L.; Thompson, E.L.; Griner, S.B.; Kline, N.; Wheldon, C. Social Determinants of Health and Health Disparities: COVID-19 Exposures and Mortality Among African American People in the United States. Public Health Rep. 2021, 136, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Dalsania, A.K.; Fastiggi, M.J.; Kahlam, A.; Shah, R.; Patel, K.; Shiau, S.; Rokicki, S.; DallaPiazza, M. The Relationship Between Social Determinants of Health and Racial Disparities in COVID-19 Mortality. J. Racial Ethn. Health Disparities 2021. [Google Scholar] [CrossRef]
- Changes in Health Coverage by Race and Ethnicity since the ACA, 2010–2018. Available online: https://www.kff.org/racial-equity-and-health-policy/issue-brief/changes-in-health-coverage-by-race-and-ethnicity-since-the-aca-2010-2018/ (accessed on 15 February 2021).
- U.S. Uninsured Rate Steady at 12.2% in Fourth Quarter of 2017. Available online: https://news.gallup.com/poll/225383/uninsured-rate-steady-fourth-quarter-2017.aspx (accessed on 15 February 2021).
- In U.S., 14% With Likely COVID-19 to Avoid Care Due to Cost. Available online: https://news.gallup.com/poll/309224/avoid-care-likely-covid-due-cost.aspx (accessed on 15 February 2021).
- Kutner, M.; Greenburg, E.; Jin, Y.; Paulsen, C. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006-483). Natl. Cent. Educ. Stat. 2006. [Google Scholar]
- Cutilli, C.C.; Bennett, I.M. Understanding the Health Literacy of America Results of the National Assessment of Adult Literacy. Orthop. Nurs. 2009, 28, 27–34. [Google Scholar] [CrossRef] [Green Version]
- Benjamin, R.M. Improving Health by Improving Health Literacy. Public Health Rep. 2010, 125, 784–785. [Google Scholar] [CrossRef] [Green Version]
- Zarocostas, J. How to fight an infodemic. Lancet 2020, 395, 676. [Google Scholar] [CrossRef]
- Managing the COVID-19 Infodemic: Promoting Healthy Behaviours and Mitigating the Harm from Misinformation and Disinformation. Available online: https://www.who.int/news/item/23-09-2020-managing-the-covid-19-infodemic-promoting-healthy-behaviours-and-mitigating-the-harm-from-misinformation-and-disinformation (accessed on 15 February 2021).
- Diseases, T.L.I. The COVID-19 infodemic. Lancet Infect. Dis. 2020, 20, 875. [Google Scholar] [CrossRef]
- Orso, D.; Federici, N.; Copetti, R.; Vetrugno, L.; Bove, T. Infodemic and the spread of fake news in the COVID-19-era. Eur. J. Emerg. Med. 2020, 27, 327–328. [Google Scholar] [CrossRef] [PubMed]
- Cinelli, M.; Quattrociocchi, W.; Galeazzi, A.; Valensise, C.M.; Brugnoli, E.; Schmidt, A.L.; Zola, P.; Zollo, F.; Scala, A. The COVID-19 social media infodemic. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Siebenhaar, K.U.; Köther, A.K.; Alpers, G.W. Dealing With the COVID-19 Infodemic: Distress by Information, Information Avoidance, and Compliance With Preventive Measures. Front. Psychol. 2020, 11, 567905. [Google Scholar] [CrossRef]
- Naeem, S.B.; Bhatti, R. The Covid-19 ‘infodemic’: A new front for information professionals. Health Inf. Libr. J. 2020, 37, 233–239. [Google Scholar] [CrossRef]
- Ahmad, K.; Erqou, S.; Shah, N.; Nazir, U.; Morrison, A.R.; Choudhary, G.; Wu, W.C. Association of poor housing conditions with COVID-19 incidence and mortality across US counties. PLoS ONE 2020, 15, e0241327. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, D.E. Environmental Health Disparities in Housing. Am. J. Public Health 2011, 101, S115–S122. [Google Scholar] [CrossRef]
- Zwickl, K.; Ash, M.; Boyce, J.K. Regional variation in environmental inequality: Industrial air toxics exposure in US cities. Ecol. Econ. 2014, 107, 494–509. [Google Scholar] [CrossRef] [Green Version]
- Wu, X.; Nethery, R.; Sabath, M.; Braun, D.; Dominici, F. Air pollution and COVID-19 mortality in the United States: Strengths and limitations of an ecological regression analysis. Sci. Adv. 2020, 6, eabd4049. [Google Scholar] [CrossRef]
- Pozzer, A.; Dominici, F.; Haines, A.; Witt, C.; Münzel, T.; Lelieveld, J. Regional and global contributions of air pollution to risk of death from COVID-19. Cardiovasc. Res. 2020, 116, 2247–2253. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Priest, N.; Anderson, N.B. Understanding Associations between Race, Socioeconomic Status and Health: Patterns and Prospects. Health Psychol. 2016, 35, 407–411. [Google Scholar] [CrossRef]
- Labor Force Statistics from the Current Population Survey. Household Data. Annual Averages. 18. Employed Persons by Detailed Industry, Sex, Race, and Hispanic or Latino Ethnicity. Available online: https://www.bls.gov/cps/cpsaat18.htm (accessed on 15 February 2021).
- Rogers, T.N.; Rogers, C.R.; VanSant-Webb, E.; Gu, L.Y.; Yan, B.; Qeadan, F. Racial Disparities in COVID-19 Mortality Among Essential Workers in the United States. World Med. Health Policy 2020, 12, 311–327. [Google Scholar] [CrossRef] [PubMed]
- Selden, T.M.; Berdahl, T.A. COVID-19 And Racial/Ethnic Disparities In Health Risk, Employment, And Household Composition. Health Aff. 2020, 39, 1624–1632. [Google Scholar] [CrossRef]
- Singu, S.; Acharya, A.; Challagundla, K.; Byrareddy, S.N. Impact of Social Determinants of Health on the Emerging COVID-19 Pandemic in the United States. Front. Public Health 2020, 8. [Google Scholar] [CrossRef] [PubMed]
- Porta, M. A Dictionary of Epidemiology; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Information about the Pfizer-BioNTech COVID-19 Vaccine. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Pfizer-BioNTech.html (accessed on 15 February 2021).
- Information about the Moderna COVID-19 Vaccine. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Moderna.html (accessed on 15 February 2021).
- People Are Dying. Whom Do We Save First With the Vaccine? Available online: https://www.nytimes.com/2020/12/24/magazine/who-should-get-the-covid-vaccine-next.html (accessed on 15 February 2021).
- The Elderly vs. Essential Workers: Who Should Get the Coronavirus Vaccine First? Available online: https://www.nytimes.com/2020/12/05/health/covid-vaccine-first.html (accessed on 15 February 2021).
- Funk, C.; Tyson, A. Intent to Get a COVID-19 Vaccine Rises to 60% as Confidence in Research and Development Process Increases. Pew Res. Cent. 2020. [Google Scholar]
- LaVeist, T.A.; Nickerson, K.J.; Bowie, J.V. Attitudes about Racism, Medical Mistrust, and Satisfaction with Care among African American and White Cardiac Patients. Med Care Res. Rev. 2000, 57, 146–161. [Google Scholar] [CrossRef]
- Corbie-Smith, G.; Thomas, S.B.; George, D.M.M.S. Distrust, Race, and Research. Arch. Intern. Med. 2002, 162, 2458–2463. [Google Scholar] [CrossRef] [Green Version]
- Boulware, L.E.; Cooper, L.A.; Ratner, L.E.; LaVeist, T.A.; Powe, N.R. Race and Trust in the Health Care System. Public Health Reports Jul-Aug 2003 2003, 118, 358–365. [Google Scholar] [CrossRef]
- Halbert, C.H.; Armstrong, K.; Gandy, O.H.; Shaker, L. Racial Differences in Trust in Health Care Providers. Arch. Intern. Med. 2006, 166, 896–901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kennedy, B.R.; Mathis, C.C.; Woods, A.K. African Americans and Their Distrust of the Health Care System: Healthcare for Diverse Populations. J. Cult. Divers. 2007, 14, 56–60. [Google Scholar] [PubMed]
- Armstrong, K.; McMurphy, S.; Dean, L.T.; Micco, E.; Putt, M.; Halbert, C.H.; Schwartz, J.S.; Sankar, P.; Pyeritz, R.E.; Bernhardt, B.; et al. Differences in the Patterns of Health Care System Distrust Between Blacks and Whites. J. Gen. Intern. Med. 2008, 23, 827–833. [Google Scholar] [CrossRef] [Green Version]
- Musa, D.; Schulz, R.; Harris, R.; Silverman, M.; Thomas, S.B. Trust in the Health Care System and the Use of Preventive Health Services by Older Black and White Adults. Am. J. Public Health 2009, 99, 1293–1299. [Google Scholar] [CrossRef] [PubMed]
- National Survey: Black Adult Perspectives on COVID-19 and Flu Vaccines. Available online: https://www.nfid.org/national-survey-black-adult-perspectives-on-covid-19-and-flu-vaccines/ (accessed on 15 February 2021).
- Bogart, L.M.; Ojikutu, B.O.; Tyagi, K.; Klein, D.J.; Mutchler, M.G.; Dong, L.; Lawrence, S.J.; Thomas, D.R.; Kellman, S. COVID-19 Related Medical Mistrust, Health Impacts, and Potential Vaccine Hesitancy Among Black Americans Living With HIV. J. Acquir. Immune Defic. Syndr. 2021, 86, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Bogart, L.M.; Takada, S.; Cunningham, W.E. Medical Mistrust, Discrimination, and the Domestic HIV Epidemic. In HIV in US Communities of Color; Springer Nature Switzerland AG: Cham, Switzerland, 2021; pp. 207–231. [Google Scholar]
- Medical Mistrust Could Reduce Vaccine Uptake: Q&A with Laura Bogart. Available online: https://www.rand.org/blog/rand-review/2020/12/medical-mistrust-could-reduce-vaccine-uptake-qa-with.html (accessed on 15 February 2021).
- Churches Pair Up with Clinics to Deliver Coronavirus Vaccine to Those Who Need It Most. Available online: https://www.washingtonpost.com/local/churches-coronavirus-vaccine-clinics/2021/02/10/522025f8-6b17-11eb-ba56-d7e2c8defa31_story.html (accessed on 15 February 2021).
- COVID-19 Vaccine: Reaching Black Ohioans with Shots in a Place they Trust—The Church. Available online: https://www.cincinnati.com/story/news/2021/02/10/covid-19-vaccine-black-church-cincinnati/4455725001/ (accessed on 15 February 2021).
- Historic Black Denver Church Opens Doors For COVID Vaccination Event. Available online: https://denver.cbslocal.com/2021/02/07/black-denver-church-covid-vaccination-event-shorter-community-ame/ (accessed on 15 February 2021).
- Jackson is Partnering with Houses of Worship to Vaccinate Members. Is yours on the list? Available online: https://www.miamiherald.com/news/coronavirus/article248477485.html (accessed on 15 February 2021).
- Novant and Churches Partner to help Distribute COVID-19 Vaccine. Available online: https://myfox8.com/news/coronavirus/novant-and-churches-partner-to-help-distribute-covid-19-vaccine/ (accessed on 15 February 2021).
- St. Dominic Hospital Teams Up with Area Churches to Provide COVID vaccine. Available online: https://www.wlbt.com/2021/02/11/st-dominic-hospital-teams-up-with-area-churches-provide-covid-vaccine/ (accessed on 15 February 2021).







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, J.J.; Chen, J.T.; Belin, T.R.; Brookmeyer, R.S.; Suchard, M.A.; Ramirez, C.M. Racial and Ethnic Disparities in Years of Potential Life Lost Attributable to COVID-19 in the United States: An Analysis of 45 States and the District of Columbia. Int. J. Environ. Res. Public Health 2021, 18, 2921. https://doi.org/10.3390/ijerph18062921
Xu JJ, Chen JT, Belin TR, Brookmeyer RS, Suchard MA, Ramirez CM. Racial and Ethnic Disparities in Years of Potential Life Lost Attributable to COVID-19 in the United States: An Analysis of 45 States and the District of Columbia. International Journal of Environmental Research and Public Health. 2021; 18(6):2921. https://doi.org/10.3390/ijerph18062921
Chicago/Turabian StyleXu, Jay J., Jarvis T. Chen, Thomas R. Belin, Ronald S. Brookmeyer, Marc A. Suchard, and Christina M. Ramirez. 2021. "Racial and Ethnic Disparities in Years of Potential Life Lost Attributable to COVID-19 in the United States: An Analysis of 45 States and the District of Columbia" International Journal of Environmental Research and Public Health 18, no. 6: 2921. https://doi.org/10.3390/ijerph18062921
APA StyleXu, J. J., Chen, J. T., Belin, T. R., Brookmeyer, R. S., Suchard, M. A., & Ramirez, C. M. (2021). Racial and Ethnic Disparities in Years of Potential Life Lost Attributable to COVID-19 in the United States: An Analysis of 45 States and the District of Columbia. International Journal of Environmental Research and Public Health, 18(6), 2921. https://doi.org/10.3390/ijerph18062921






