Access to Healthcare during COVID-19
Abstract
1. Introduction
2. Materials and Methods
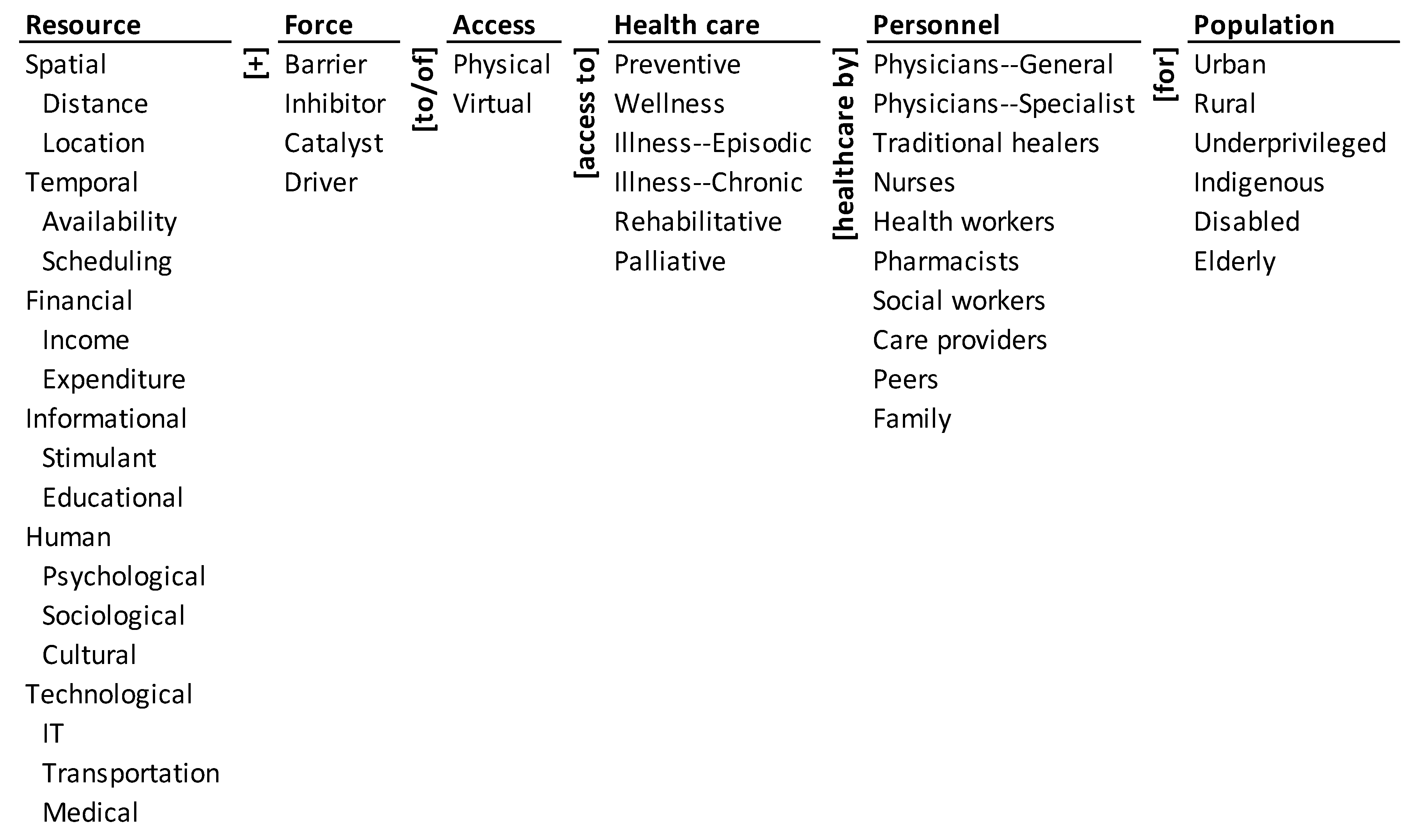
2.1. Ontology of Access to Healthcare during COVID-19
2.2. Method
3. Results
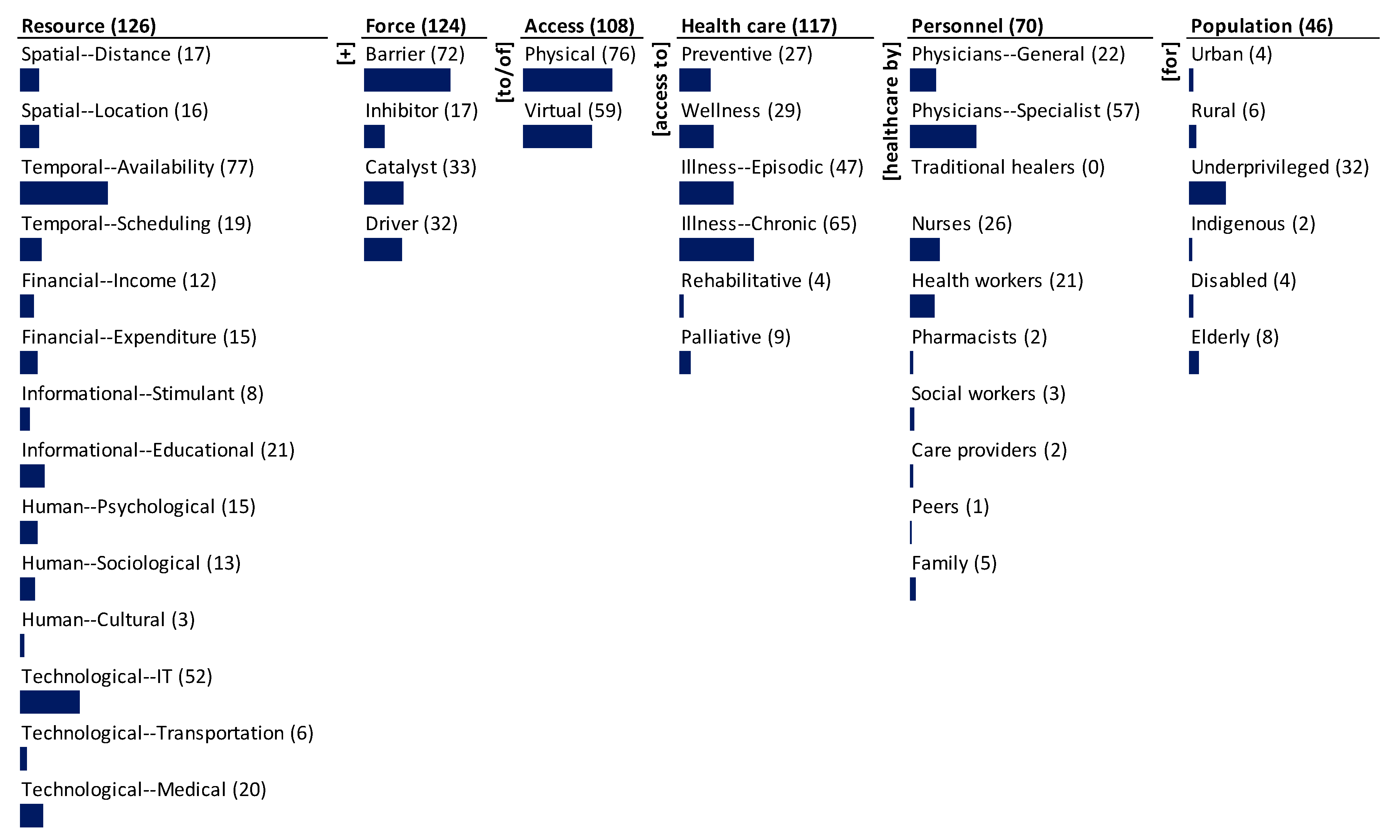
3.1. Monad Map
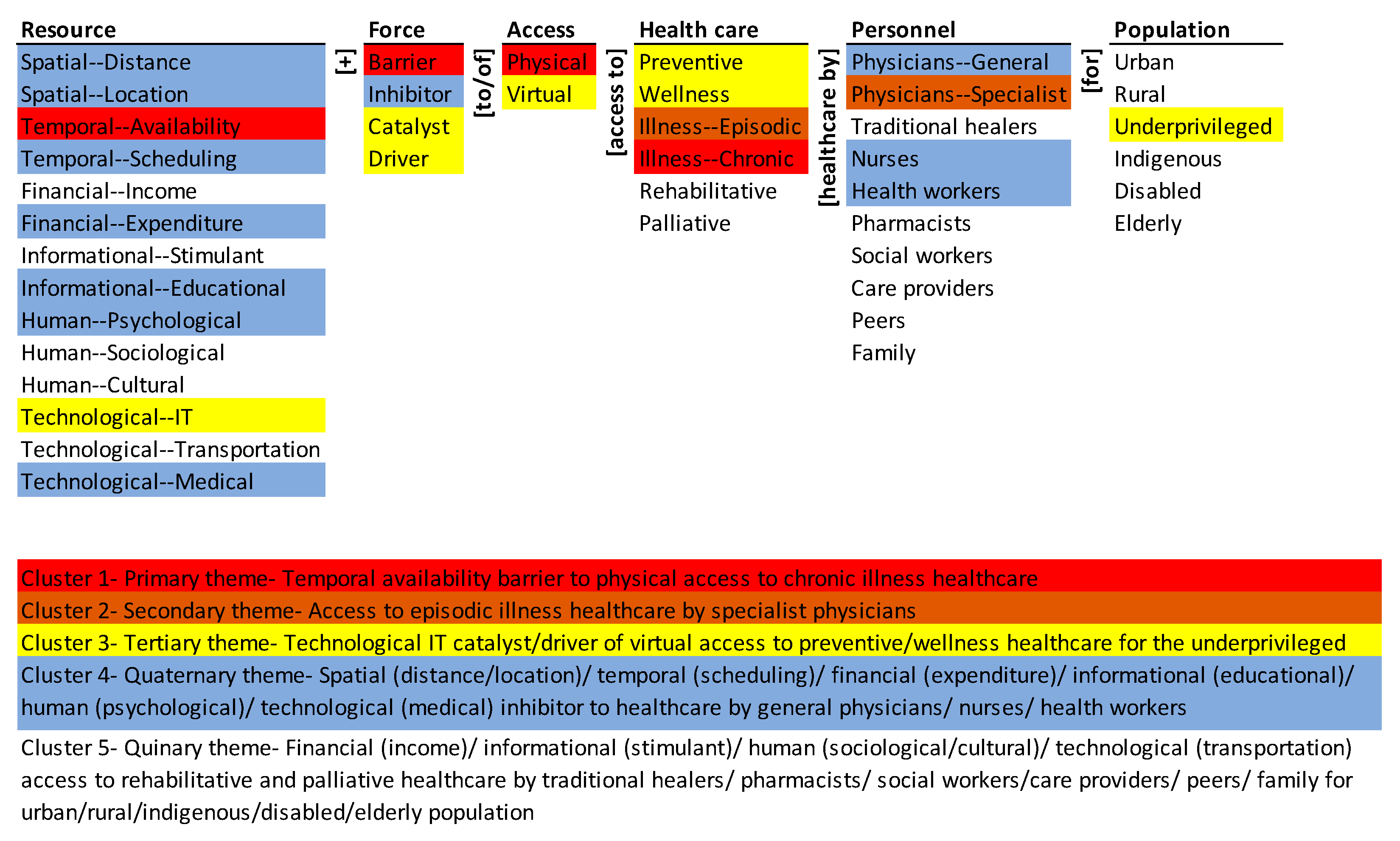
3.2. Theme Map
4. Discussion
- Provide a systemic view of the problem for advancing research and developing guidelines.
- Systematically analyze the emphases and gaps in research and practice and develop a balanced roadmap for both.
- Systematically analyze the gaps between research and practice and develop a strategy for effective translation between the two through feedback and learning.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Daniels, N. Equity of access to health care: Some conceptual and ethical issues. The Milbank Memorial Fund Quarterly. Health Soc. 1982, 60, 51–81. [Google Scholar]
- Whitehead, M. The concepts and principles of equity and health. Int. J. Health Serv. Plan. Adm. Eval. 1992, 22, 429–445. [Google Scholar] [CrossRef]
- Gulliford, M.; Figueroa-Munoz, J.; Morgan, M.; Hughes, D.; Gibson, B.; Beech, R.; Hudson, M. What does ‘access to health care’ mean? J. Health Serv. Res. Policy 2002, 7, 186–188. [Google Scholar] [CrossRef]
- Abedi, V.; Olulana, O.; Avula, V.; Chaudhary, D.; Khan, A.; Shahjouei, S.; Li, J.; Zand, R. Racial, Economic, and Health Inequality and COVID-19 Infection in the United States. J. Racial Ethn. Health Disparities 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Azar, K.M.J.; Shen, Z.; Romanelli, R.J.; Lockhart, S.H.; Smits, K.; Robinson, S.; Brown, S.; Pressman, A.R. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff. (Proj. Hope) 2020, 39, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Maintaining Essential Health Services: Operational Guidance for the COVID-19 Context. World Health Organ. 2020. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-essential-health-services-2020.1 (accessed on 5 December 2020).
- Okereke, M.; Ukor, N.A.; Adebisi, Y.A.; Ogunkola, I.O.; Iyagbaye, E.F.; Owhor, G.A.; Lucero-Prisno, D.E., 3rd. Impact of COVID-19 on access to healthcare in low- and middle-income countries: Current evidence and future recommendations. Int. J. Health Plan. Manag. 2021, 36, 13–17. [Google Scholar] [CrossRef]
- Abuzeineh, M.; Muzaale, A.D.; Crews, D.C.; Avery, R.K.; Brotman, D.J.; Brennan, D.C.; Segev, D.L.; Al Ammary, F. Telemedicine in the care of kidney transplant recipients with Coronavirus Disease 2019: Case reports. Transplant. Proc. 2020, 52, 2620–2625. [Google Scholar] [CrossRef]
- Al-Sofiani, M.E.; Alyusuf, E.Y.; Alharthi, S.; Alguwaihes, A.M.; Al-Khalifah, R.; Alfadda, A. Rapid implementation of a diabetes telemedicine clinic during the Coronavirus Disease 2019 outbreak: Our protocol, experience, and satisfaction reports in Saudi Arabia. J. Diabetes Sci. Technol. 2020, 15, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Aziz, A.; Zork, N.; Aubey, J.J.; Baptiste, C.D.; D’alton, M.E.; Emeruwa, U.N.; Fuchs, K.M.; Goffman, D.; Gyamfi-Bannerman, C.; Haythe, J.H.; et al. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am. J. Perinatol. 2020, 37, 800–808. [Google Scholar] [CrossRef]
- Bourdon, H.; Jaillant, R.; Ballino, A.; El Kaim, P.; Debillon, L.; Bodin, S.; N’Kosi, L. Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: Experience with 500 patients in March and April 2020. J. Fr. D’ophtalmol. 2020, 43, 577–585. [Google Scholar] [CrossRef]
- Burgoyne, N.; Cohn, A.S. Lessons from the transition to relational teletherapy during COVID-19. Fam. Process. 2020, 59, 974–988. [Google Scholar] [CrossRef]
- Lonergan, P.E.; Iii, S.L.W.; Branagan, L.; Gleason, N.; Pruthi, R.S.; Carroll, P.R.; Odisho, A.Y. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID-19: Cross-sectional analysis. J. Med. Internet Res. 2020, 22, e19322. [Google Scholar] [CrossRef]
- Velásquez, J.R.M. Teleconsulta en la pandemia por Coronavirus: Desafíos para la telemedicina pos-COVID-19. Rev. Colomb. De Gastroenterol. 2020, 35 (Suppl. 1), 5–16. [Google Scholar] [CrossRef]
- Hardcastle, L.; Ogbogu, U. Virtual care: Enhancing access or harming care? Healthc. Manag. Forum 2020, 33, 288–292. [Google Scholar] [CrossRef]
- Lau, J.; Knudsen, J.; Jackson, H.; Wallach, A.B.; Bouton, M.; Natsui, S.; Philippou, C.; Karim, E.; Silvestri, D.M.; Avalone, L.; et al. Staying Connected in the COVID-19 pandemic: Telehealth at the largest safety-net system in the United States. Health Aff. (Proj. Hope) 2020, 39, 1437–1442. [Google Scholar] [CrossRef] [PubMed]
- Aragona, M.; Barbato, A.; Cavani, A.; Costanzo, G.; Mirisola, C. Negative impacts of COVID-19 lockdown on mental health service access and follow-up adherence for immigrants and individuals in socio-economic difficulties. Public Health 2020, 186, 52–56. [Google Scholar] [CrossRef]
- Roy, A.; Singh, A.K.; Mishra, S.; Chinnadurai, A.; Mitra, A.; Bakshi, O. Mental health implications of COVID-19 pandemic and its response in India. Int. J. Soc. Psychiatry 2020. [Google Scholar] [CrossRef]
- Javed, B.; Sarwer, A.; Soto, E.B.; Mashwani, Z.U. The coronavirus (COVID-19) pandemic’s impact on mental health. Int. J. Health Plan. Manag. 2020, 35, 993–996. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.E.; Simon, L.; Riedy, C.A.; Barrow, J.R. Modeling the Impact of COVID-19 on Dental Insurance Coverage and Utilization. J. Dent. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Núñez, A.; Ramaprasad, A.; Syn, T.; Lopez, H. An ontological analysis of the barriers to and facilitators of access to health care. J. Public Health 2020, 1–11. [Google Scholar] [CrossRef]
- Ramaprasad, A.; Syn, T. Ontological meta-analysis and synthesis. Commun. Assoc. Inf. Syst. 2015, 37, 138–153. [Google Scholar] [CrossRef]
- Simon, H.A. The Architecture of Complexity. In Proceedings of the American Philosophical Society; American Philosophical Society: Philadelphia, PA, USA, 1962; Volume 106, pp. 467–482. [Google Scholar]
- Cimino, J.J. In defense of the Desiderata. J. Biomed. Inform. 2006, 39, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, B.; Josephson, J.R.; Benjamins, V.R. What are ontologies, and why do we need them? IEEE Intell. Syst. 1999, 14, 20–26. [Google Scholar] [CrossRef]
- Cameron, J.D.; Ramaprasad, A.; Syn, T. An ontology of and roadmap for mHealth research. Int. J. Med. Inform. 2017, 100, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Gruber, T.R. Toward Principles for the design of ontologies used for knowledge sharing. Int. J. Hum. Comput. Stud. 1995, 43, 907–928. [Google Scholar] [CrossRef]
- Gruber, T.R. Ontology. In Encyclopedia of Database Systems; Liu, L., Özsu, M.T., Eds.; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Ramaprasad, A. Cognitive process as a basis for MIS and DSS Design. Manag. Sci. 1987, 33, 139–148. [Google Scholar] [CrossRef]
- Ramaprasad, A.; Mitroff, I.I. On formulating strategic problems. Acad. Manag. Rev. 1984, 9, 597–605. [Google Scholar] [CrossRef]
- Ramaprasad, A.; Poon, E. A computerized interactive technique for mapping influence diagrams (MIND). Strateg. Manag. J. 1985, 6, 377–392. [Google Scholar] [CrossRef]
- Ramaprasad, A. Revolutionary change and strategic management. Behav. Sci. 1982, 27, 387–392. [Google Scholar] [CrossRef]
- Ramaprasad, A. On the definition of feedback. Behav. Sci. 1983, 28, 4–13. [Google Scholar] [CrossRef]
- Quine, W.V.O. From a Logical Point of View (Second, Revised); Harvard University Press: Cambridge, MA, USA, 1961. [Google Scholar]
- Gadicherla, S.; Krishnappa, L.; Madhuri, B.; Mitra, S.G.; Ramaprasad, A.; Seevan, R.; Sreeganga, S.D.; Thodika, N.K.; Mathew, S.; Suresh, V. Envisioning a learning surveillance system for tuberculosis. PLoS ONE 2020, 15, e0243610. [Google Scholar] [CrossRef]
- Núñez, A.; Ramaprasad, A.; Syn, T. National healthcare policies in Chile: An ontological meta-analysis. Stud. Health Technol. Inform. 2015, 216, 1105. [Google Scholar] [CrossRef]
- Ramaprasad, A.; Singai, C.B.; Hasan, T.; Syn, T.; Thirumalai, M. India’s national higher education policy recommendations since independence. J. Educ. Plan. Adm. 2016, 30, 5–24. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Syn, T.; Ramaprasad, A. Megaprojects—symbolic and sublime: An ontological review. Int. J. Manag. Proj. Bus. 2019, 12, 377–399. [Google Scholar] [CrossRef]
- La Paz, A.; Merigó, J.M.; Powell, P.; Ramaprasad, A.; Syn, T. Twenty-five years of the Information Systems Journal: A bibliometric and ontological overview. Inf. Syst. J. 2019, 1–27. [Google Scholar] [CrossRef]
- Mauro, V.; Lorenzo, M.; Paolo, C.; Sergio, H. Treat all COVID 19-positive patients, but do not forget those negative with chronic diseases. Intern. Emerg. Med. 2020, 15, 787–790. [Google Scholar] [CrossRef] [PubMed]
- Chudasama, Y.V.; Gillies, C.L.; Zaccardi, F.; Coles, B.; Davies, M.J.; Seidu, S.; Khunti, K. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 965–967. [Google Scholar] [CrossRef]
- WHO. WHO SAGE Roadmap for Prioritizing Uses of Covid-19 Vaccines in the Context of Limited Supply. World Health Organization. 2020. Available online: https://www.who.int/docs/default-source/immunization/sage/covid/sage-prioritization-roadmap-covid19-vaccines.pdf?Status=Temp&sfvrsn=bf227443_2 (accessed on 10 October 2020).
- Bennardo, F.; Antonelli, A.; Barone, S.; Figliuzzi, M.M.; Fortunato, L.; Giudice, A. Change of outpatient oral surgery during the COVID-19 Pandemic: Experience of an Italian center. Int. J. Dent. 2020, 2020, 1–6. [Google Scholar] [CrossRef]
- Kumar, S.; Chmura, S.; Robinson, C.; Lin, S.H.; Gadgeel, S.M.; Donington, J.; Feliciano, J.; Stinchcombe, T.E.; Werner-Wasik, M.; Edelman, M.J.; et al. Alternative multidisciplinary management options for locally advanced NSCLC during the Coronavirus disease 2019 global pandemic. J. Thorac. Oncol. 2020, 15, 1137–1146. [Google Scholar] [CrossRef]
- Mannelli, C. Whose life to save? Scarce resources allocation in the COVID-19 outbreak. J. Med. Ethics 2020, 46, 364–366. [Google Scholar] [CrossRef]
- Benjamin, G.C. Ensuring health equity during the COVID-19 pandemic: The role of public health infrastructure. Rev. Panam. De Salud Pública 2020, 44, e70. [Google Scholar] [CrossRef]
- Cohen, M.A.; Powell, A.M.; Coleman, J.S.; Keller, J.M.; Livingston, A.; Anderson, J.R. Special ambulatory gynecologic considerations in the era of coronavirus disease 2019 (COVID-19) and implications for future practice. Am. J. Obstet. Gynecol. 2020, 223, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Hao, C. Case-Initiated COVID-19 contact tracing using anonymous notifications. JMIR mHealth uHealth 2020, 8, e20369. [Google Scholar] [CrossRef]
- Jiménez-Rodríguez, D.; García, A.S.; Robles, J.M.; Salvador, M.M.R.; Ronda, F.J.M.; Arrogante, O. Increase in video consultations during the COVID19 pandemic: Healthcare professionals’ perceptions about their implementation and adequate management. Int. J. Environ. Res. Public Health 2020, 17, 5112. [Google Scholar] [CrossRef]
- Andrews, E.E.; Ayers, K.B.; Brown, K.S.; Dunn, D.S.; Pilarski, C.R. No body is expendable: Medical rationing and disability justice during the COVID-19 Pandemic. Am. Psychol. 2020. [Google Scholar] [CrossRef]
- Barroy, H.; Wang, D.; Pescetto, C.; Kutzin, J. How to Budget for COVID-19 Response? A Rapid Scan of Budgetary Mechanisms in Highly Affected Countries. WHO. 2020. Available online: https://www.who.int/docs/default-source/health-financing/how-to-budget-for-covid-19-english.pdf?sfvrsn=356a8077_1 (accessed on 10 October 2020).
- Braithwaite, R.; Warren, R. The African American petri dish. J. Health Care Poor Underserved 2020, 31, 491–502. [Google Scholar] [CrossRef]
- de León-Martínez, L.D.; de la Sierra-de la Vega, L.; Palacios-Ramírez, A.; Rodriguez-Aguilar, M.; Flores-Ramírez, R. Critical review of social, environmental and health risk factors in the Mexican indigenous population and their capacity to respond to the COVID-19. Sci. Total Environ. 2020, 733, 139357. [Google Scholar] [CrossRef] [PubMed]
- Lakhani, A. Which melbourne metropolitan areas are vulnerable to COVID-19 based on age, disability, and access to health services? Using Spatial analysis to identify service gaps and inform delivery. J. Pain Symptom Manag. 2020, 60, e41–e44. [Google Scholar] [CrossRef] [PubMed]
- Kontoangelos, K.; Economou, M.; Papageorgiou, C. Mental health effects of COVID-19 Pandemia: A review of clinical and psychological traits. Psychiatry Investig. 2020, 17, 491–505. [Google Scholar] [CrossRef] [PubMed]
- Ungureanu, B.S.; Vladut, C.; Bende, F.; Sandru, V.; Tocia, V.; Turcu-Stiolica, R.-V.; Groza, A.; Balan, G.G.; Turcu-Stiolica, A. Impact of the COVID-19 pandemic on health-related quality of life, anxiety, and training among young gastroenterologists in Romania. Front. Psychol. 2020, 11, 579177. [Google Scholar] [CrossRef] [PubMed]
- Whaley, P.; Edwards, S.W.; Kraft, A.; Nyhan, K.; Shapiro, A.; Watford, S.; Wattam, S.; Wolffe, T.; Angrish, M. Knowledge organization systems for systematic chemical assessments. Environ. Health Perspect. 2020, 128, 125001. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Núñez, A.; Sreeganga, S.D.; Ramaprasad, A. Access to Healthcare during COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 2980. https://doi.org/10.3390/ijerph18062980
Núñez A, Sreeganga SD, Ramaprasad A. Access to Healthcare during COVID-19. International Journal of Environmental Research and Public Health. 2021; 18(6):2980. https://doi.org/10.3390/ijerph18062980
Chicago/Turabian StyleNúñez, Alicia, S. D. Sreeganga, and Arkalgud Ramaprasad. 2021. "Access to Healthcare during COVID-19" International Journal of Environmental Research and Public Health 18, no. 6: 2980. https://doi.org/10.3390/ijerph18062980
APA StyleNúñez, A., Sreeganga, S. D., & Ramaprasad, A. (2021). Access to Healthcare during COVID-19. International Journal of Environmental Research and Public Health, 18(6), 2980. https://doi.org/10.3390/ijerph18062980







