Inequalities and Inclusion in Exercise Referral Schemes: A Mixed-Method Multi-Scheme Analysis
Abstract
:1. Introduction
1.1. The Positioning of Physical Activity Prescription with Respect to Inequalities
1.2. Inequalities in Uptake, Adherence, and Outcomes
1.3. The Case for Wider Contextualised Analysis across and between Schemes
1.4. Research Aims
2. Materials and Methods—Phase 1
2.1. Data and Sampling
2.2. Analyses and Data Processing
3. Results—Phase 1
3.1. Inclusion-Related Descriptives
3.2. Model 1: Scheme Uptake
3.3. Model 2: Scheme Completion
3.4. Model 3: Scheme Outcomes
4. Materials and Methods—Phase 2
4.1. Sampling and Recruitment
4.2. Data Collection and Analysis
5. Results—Phase 2
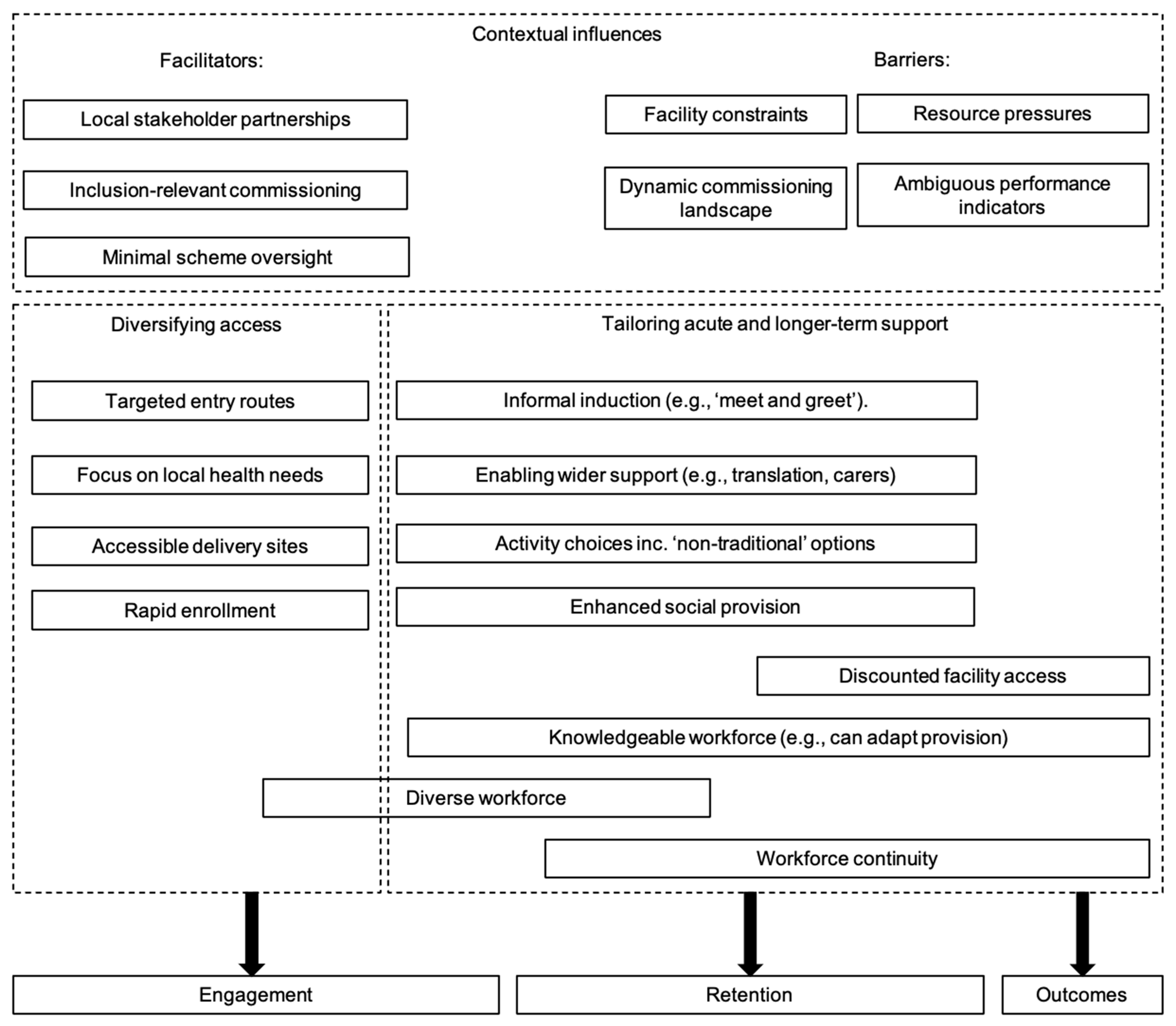
5.1. Diverisfying Access
“My role is to go out and look at different ways to bring referrals in. So I spend a lot of time going off to forums, umm, health task and finishing groups and CCG meetings to see kind of what’s going on out there and try to bring stuff back into the centres.”
5.2. Tailoring Support
5.3. Long-Term Engagement
5.4. Contexutal Challenges
5.5. Contexutal Facilitators
6. Discussion
6.1. Overview of Findings
6.2. Observed Inequalities in Uptake, Completion, and Outcomes
6.3. A Recurrent Issue—Data Quality and Exercise Referral Evaluation
6.4. Learning from Inclusive Practices in Schemes
6.5. Limitations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Global Action Plan on Physical Activity 2018-2030: More Active People for a Healthier World; World Health Organisation: Geneva, Switzerland, 2018. [Google Scholar]
- Althoff, T.; Sosič, R.; Hicks, J.L.; King, A.C.; Delp, S.L.; Leskovec, J. Large-scale physical activity data reveal worldwide activity inequality. Nat. Cell Biol. 2017, 547, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Carey, G.; Crammond, B.; De Leeuw, E. Towards health equity: A framework for the application of proportionate universalism. Int. J. Equity Health 2015, 14, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorenc, T.; Petticrew, M.; Welch, V.; Tugwell, P. What types of interventions generate inequalities? Evidence from systematic reviews. J. Epidemiol. Community Health 2013, 67, 190–193. [Google Scholar] [CrossRef] [Green Version]
- Public Health Guidance [PH54]: Physical Activity: Exercise Referral Schemes. 2014. Available online: https://www.nice.org.uk/guidance/ph54 (accessed on 30 January 2021).
- Kelly, M.C.; Rae, G.C.; Walker, D.; Partington, S.; Dodd-Reynolds, C.J.; Caplan, N. Retrospective cohort study of the South Tyneside Exercise Referral Scheme 2009–14: Predictors of dropout and barriers to adherence. J. Public Health 2016, 39, e257–e264. [Google Scholar] [CrossRef] [Green Version]
- Pavey, T.G.; Taylor, A.H.; Fox, K.R.; Hillsdon, M.; Anokye, N.; Campbell, J.L.; Foster, C.; Green, C.; Moxham, T.; Mutrie, N.; et al. Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: Systematic review and meta-analysis. BMJ 2011, 343, d6462. [Google Scholar] [CrossRef] [Green Version]
- Hanson, C.L.; Ellis, J.G.; Allin, L.J.; Dodd-Reynolds, C.J. An evaluation of the efficacy of the exercise on referral scheme in Northumberland, UK: Association with physical activity and predictors of engagement. A naturalistic observation study. BMJ Open 2013, 3, e002849. [Google Scholar] [CrossRef] [Green Version]
- Tobi, P.; Estacio, E.V.; Yu, G.; Renton, A.; Foster, N. Who stays, who drops out? Biosocial predictors of longer-term adherence in participants attending an exercise referral scheme in the UK. BMC Public Health 2012, 12, 347. [Google Scholar] [CrossRef] [Green Version]
- Shore, C.B.; Hubbard, G.; Gorely, T.; Polson, R.; Hunter, A.; Galloway, S.D. Insufficient Reporting of Factors Associated With Exercise Referral Scheme Uptake, Attendance, and Adherence: A Systematic Review of Reviews. J. Phys. Act. Health 2019, 16, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Tobi, P.; Kemp, P.; Schmidt, E. Cohort differences in exercise adherence among primary care patients referred for mental health versus physical health conditions. Prim. Health Care Res. Dev. 2017, 18, 463–471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgan, K.; Rahman, M.; Moore, G. Patterning in Patient Referral to and Uptake of a National Exercise Referral Scheme (NERS) in Wales from 2008 to 2017: A Data Linkage Study. Int. J. Environ. Res. Public Health 2020, 17, 3942. [Google Scholar] [CrossRef] [PubMed]
- Wade, M.; Mann, S.; Copeland, R.J.; Steele, J. Effect of exercise referral schemes upon health and well-being: Initial observational insights using individual patient data meta-analysis from the National Referral Database. J. Epidemiol. Community Health 2019, 74, 32–41. [Google Scholar] [CrossRef] [Green Version]
- Rowley, N.; Steele, J.; Wade, M.; Copeland, R.J.; Mann, S.; Liguori, G.; Horton, E.; Jimenez, A. Are Exercise Referral Schemes Associated With an Increase in Physical Activity? Observational Findings Using Individual Patient Data Meta-Analysis from the National Referral Database. J. Phys. Act. Health 2020, 17, 621–631. [Google Scholar] [CrossRef]
- Dodd-Reynolds, C.J.; Vallis, D.; Kasim, A.; Akhter, N.; Hanson, C.L. The Northumberland Exercise Referral Scheme as a Universal Community Weight Management Programme: A Mixed Methods Exploration of Outcomes, Expectations and Experiences across a Social Gradient. Int. J. Environ. Res. Public Health 2020, 17, 5297. [Google Scholar] [CrossRef]
- Morgan, F.; Battersby, A.; Weightman, A.L.; Searchfield, L.; Turley, R.; Morgan, H.; Jagroo, J.; Ellis, S. Adherence to exercise referral schemes by participants—What do providers and commissioners need to know? A systematic review of barriers and facilitators. BMC Public Health 2016, 16, 227. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Eynon, M.; Foad, J.; Downey, J.; Bowmer, Y.; Mills, H. Assessing the psychosocial factors associated with adherence to exercise referral schemes: A systematic review. Scand. J. Med. Sci. Sports 2019, 29, 638–650. [Google Scholar] [CrossRef] [PubMed]
- Sowden, S.L.; Breeze, E.; Barber, J.; Raine, R. Do general practices provide equitable access to physical activity interventions? Br. J. Gen. Pr. 2008, 58, e1–e8. [Google Scholar] [CrossRef] [Green Version]
- Hanson, C.L.; Oliver, E.J.; Dodd-Reynolds, C.J.; Allin, L. How do participant experiences and characteristics influences engagement in exercise referral? A qualitative longitudinal study of a scheme in Northumberland, United Kingdom. BMJ Open 2019, 9, e024370. [Google Scholar] [CrossRef] [Green Version]
- Birtwistle, S.B.; Ashcroft, G.; Murphy, R.; Gee, I.; Poole, H.; Watson, P.M. Factors influencing patient uptake of an exercise referral scheme: A qualitative study. Health Educ. Res. 2018, 34, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Pawson, R.; Tilley, N. An Introduction to Scientific Realist Evaluation. In Evaluation for the 21st Century: A Handbook; Chelimsky, E., Shadish, W.R., Eds.; Sage Publications, Inc.: New York, NY, USA, 1997; pp. 405–418. [Google Scholar] [CrossRef]
- Oliver, E.J.; Hanson, C.L.; Lindsey, I.A.; Dodd-Reynolds, C.J. Exercise on referral: Evidence and complexity at the nexus of public health and sport policy. Int. J. Sport Policy Politi. 2016, 8, 731–736. [Google Scholar] [CrossRef] [Green Version]
- Steele, J.; Wade, M.; Polley, M.; Copeland, R.J.; Stokes, S.; Mann, S. The National Referral Database: An initial overview. SportRχiv 2019. [Google Scholar] [CrossRef] [Green Version]
- Oliver, E.J.; Dodd-Reynolds, C.; Kasim, A.; Vallis, D. Community-based exercise prescription: Exploring inequalities in engagement and outcomes using the National Referral Database. Open Sci. Framew. 2019. [Google Scholar]
- UK Government. Indices of Deprivation. 2019. Available online: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed on 30 January 2021).
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Body Mass Index—BMI. 2020. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 30 January 2021).
- Sbaraini, A.; Carter, S.M.; Evans, R.W.; Blinkhorn, A. How to do a grounded theory study: A worked example of a study of dental practices. BMC Med. Res. Methodol. 2011, 11, 128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgan, D.L.; Krueger, R.A. Developing Questions for Focus Groups; Sage Publications Inc.: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Pawluch, D.; Neiterman, E. What Is Grounded Theory and Where Does It Come from. In The SAGE Handbook of Qualitative Methods in Health Research; De Vries, R., Bourgeault, I., Dingwall, R., Eds.; SAGE: London, UK, 2010; pp. 174–192. [Google Scholar]
- Foley, G.; Timonen, V. Using grounded theory method to capture and analyze health care experiences. Health Serv. Res. 2015, 50, 1195–1210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Timonen, V.; Foley, G.; Conlon, C. Challenges when using grounded theory: A pragmatic introduction to doing GT research. Int. J. Qual. Methods 2018, 17, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Public Health England. Local Action on Health Inequalities: Understanding and Reducing Ethnic Inequalities in Health. 2018. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/730917/local_action_on_health_inequalities.pdf (accessed on 30 January 2021).
- Allen, A.; Sesti, F. Health Inequalities and Women—Addressing Unmet Needs. British Medical Association. 2018. Available online: https://www.bma.org.uk/media/2116/bma-womens-health-inequalities-report-aug-2018.pdf (accessed on 30 January 2021).
- Prince, M.; Knapp, M.; Guerchet, M.; McCrone, P.; Prina, M.; Comas-Herrera, A.; Wittenberg, R.; Adelaja, B.; Hu, B.; King, D.; et al. Dementia UK: Update; Alzheimer’s Society: London, UK, 2014. [Google Scholar]
- National Health Service Digital. Statistics on Obesity, Physical Activity and Diet, England. 2020. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2020 (accessed on 30 January 2021).
- Din, N.U.; Moore, G.F.; Murphy, S.; Wilkinson, C.; Williams, N.H. Health professionals’ perspectives on exercise referral and physical activity promotion in primary care: Findings from a process evaluation of the National Exercise Referral Scheme in Wales. Health Educ. J. 2014, 74, 743–757. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sport England. Active Lives Adult May 19–20 Coronavirus Report. 2020. Available online: https://www.sportengland.org/know-your-audience/data/active-lives (accessed on 30 January 2021).
- Hanson, C.L.; Oliver, E.J.; Dodd-Reynolds, C.J.; Pearsons, A.; Kelly, P. A modified Delphi study to gain consensus for a taxonomy to report and classify physical activity referral schemes (PARS). Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1–11. [Google Scholar] [CrossRef]
- Bird, S.M.; Sir David, C.; Farewell, V.T.; Harvey, G.; Tim, H.; Peter, C.S. Performance indicators: Good, bad, and ugly. J. R. Stat. Soc. Ser. A 2004, 168, 11–27. [Google Scholar] [CrossRef]
- Simplican, S.C.; Leader, G.; Kosciulek, J.; Leahy, M. Defining social inclusion of people with intellectual and developmental disabilities: An ecological model of social networks and community participation. Res. Dev. Disabil. 2015, 38, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Gidley, J.; Hampson, G.; Wheeler, L.; Bereded-Samuel, E. From access to success: An integrated approach to quality higher education invormed by social inclusion theory and practice. High. Educ. Policy 2010, 23, 123–147. [Google Scholar] [CrossRef] [Green Version]
- Henderson, H.; Evans, A.B.; Allen-Collinson, J.; Niroshan, A.S. The ‘wild and woolly’ world of exercise referral schemes: Contested interpretations of an exercise as medicine programme. Qual. Res. Sport Exerc. Health 2018, 10, 505–523. [Google Scholar] [CrossRef]
- Glaser, B.G. Constructivist grounded theory? Hist. Soc. Res. Suppl. 2007, 93–105. [Google Scholar]
- Rouhani, S. Intersectionality-informed quantitative research: A primer. Am. J. Public Health 2014, 103, 1082–1089. [Google Scholar]
- Glaser, B.G. Basics of Grounded Theory Analysis: Emergence vs. Forcing; Sociology Press: Mill Valley, CA, USA, 1992. [Google Scholar]
- Benoliel, J.Q. Grounded theory and nursing knowledge. Qual. Health Res. 1996, 6, 406–428. [Google Scholar] [CrossRef]
- Sport England. Uniting the Movement. The Five Big Issues—Connecting with Health and Wellbeing. 2021. Available online: https://www.sportengland.org/why-were-here/uniting-the-movement/what-well-do/connecting-health-and-wellbeing (accessed on 30 January 2021).
| Completer (=1) | Odds Ratio | SD | 2.5% (CI) * | 97.5% (CI) * |
|---|---|---|---|---|
| Constant | −1.18 | 0.22 | −1.62 | −0.77 |
| Female | 0.08 | 0.04 | −0.01 | 0.16 |
| PreSBP | 0.00 | 0.00 | 0.00 | 0.00 |
| PreMetMins | 0.00 | 0.00 | 0.00 | 0.00 |
| Mental | −0.71 | 0.18 | −1.07 | −0.36 |
| Leisure | 0.15 | 0.06 | 0.02 | 0.27 |
| Age | 0.02 | 0.00 | 0.02 | 0.03 |
| IMDde | 0.02 | 0.01 | 0.00 | 0.04 |
| Scheme 5002 | −0.15 | 0.09 | −0.34 | 0.03 |
| Scheme 5144 | −2.71 | 0.79 | −4.41 | −1.37 |
| Scheme 5036 | −0.40 | 0.08 | −0.55 | −0.25 |
| Scheme 5056 | −0.22 | 0.07 | −0.36 | −0.07 |
| Scheme 5063 | 0.37 | 0.15 | 0.07 | 0.67 |
| Scheme 5072 | −0.07 | 0.09 | −0.23 | 0.11 |
| Scheme 5108 | 0.58 | 0.18 | 0.23 | 0.93 |
| Scheme 5156 | 0.13 | 0.38 | −0.62 | 0.88 |
| PreHR | 0.00 | 0.00 | −0.01 | 0.00 |
| EthMinor | −0.03 | 0.04 | −0.10 | 0.05 |
| PreDBP | 0.00 | 0.00 | 0.00 | 0.00 |
| CL1obese | −0.04 | 0.05 | −0.13 | 0.06 |
| CL2obese | −0.08 | 0.06 | −0.19 | 0.03 |
| CL3obese | −0.25 | 0.06 | −0.37 | −0.13 |
| ΔMETMins | Mean | SD | 2.5% (CI) | 97.5% (CI) |
|---|---|---|---|---|
| Constant | 466.64 | 325.75 | −181.06 | 1101.36 |
| Female | −10.82 | 48.03 | −105.29 | 82.51 |
| Age | −5.17 | 1.77 | −8.71 | −1.79 |
| IMDde | 1.50 | 11.65 | −21.25 | 24.15 |
| PreHR | 0.11 | 1.97 | −3.71 | 3.98 |
| EthMinor | 50.89 | 45.90 | −37.27 | 141.41 |
| PreDBP | 0.91 | 1.02 | −1.08 | 2.92 |
| PreBMI | −2.37 | 1.78 | −5.81 | 1.08 |
| PreSBP | 2.61 | 1.36 | −0.03 | 5.29 |
| MentalH | −187.16 | 216.65 | −609.99 | 235.07 |
| Scheme 5144 | −204.57 | 508.87 | −1286.22 | 754.44 |
| Scheme 5002 | 150.90 | 239.42 | −339.79 | 645.42 |
| Scheme 5036 | 53.35 | 235.43 | −420.90 | 544.14 |
| Scheme 5056 | 24.73 | 234.27 | −441.03 | 515.61 |
| Scheme 5063 | −907.51 | 258.06 | −1453.60 | −409.04 |
| Scheme 5072 | 261.42 | 236.12 | −212.49 | 760.54 |
| Scheme 5108 | 13.44 | 260.57 | −491.35 | 545.85 |
| Scheme 5156 | 780.09 | 386.59 | 117.82 | 1608.08 |
| ID | Location | Selection Rationale |
|---|---|---|
| S1 | South East England; rural | Lower overrepresentation of older adults (i.e., relative to other schemes, more younger adults engaged) |
| S2 | London Borough; urban | High completion rates for ethnic minority participants |
| S3 | London Borough; urban | High effectiveness and completion rates across all participants (i.e., less drop-out in high-risk groups). |
| S4 | South West England; rural | Lower overrepresentation of women (i.e., relative to other schemes, more males engaged) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliver, E.J.; Dodd-Reynolds, C.; Kasim, A.; Vallis, D. Inequalities and Inclusion in Exercise Referral Schemes: A Mixed-Method Multi-Scheme Analysis. Int. J. Environ. Res. Public Health 2021, 18, 3033. https://doi.org/10.3390/ijerph18063033
Oliver EJ, Dodd-Reynolds C, Kasim A, Vallis D. Inequalities and Inclusion in Exercise Referral Schemes: A Mixed-Method Multi-Scheme Analysis. International Journal of Environmental Research and Public Health. 2021; 18(6):3033. https://doi.org/10.3390/ijerph18063033
Chicago/Turabian StyleOliver, Emily J., Caroline Dodd-Reynolds, Adetayo Kasim, and Dimitrios Vallis. 2021. "Inequalities and Inclusion in Exercise Referral Schemes: A Mixed-Method Multi-Scheme Analysis" International Journal of Environmental Research and Public Health 18, no. 6: 3033. https://doi.org/10.3390/ijerph18063033






